www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
SPECIAL
ARTICLE
First
Clinical
Consensus
and
National
Recommendations
on
Tracheostomized
Children
of
the
Brazilian
Academy
of
Pediatric
Otorhinolaryngology
(ABOPe)
and
Brazilian
Society
of
Pediatrics
(SBP)
夽
,
夽夽
Melissa
A.G.
Avelino
a,b,c,d,∗,
Rebecca
Maunsell
e,
Fabiana
Cardoso
Pereira
Valera
f,
José
Faibes
Lubianca
Neto
g,h,
Cláudia
Schweiger
i,j,
Carolina
Sponchiado
Miura
k,
Vitor
Guo
Chen
a,l,
Dayse
Manrique
a,m,
Raquel
Oliveira
n,
Fabiano
Gavazzoni
o,
Isabela
Furtado
de
Mendonc
¸a
Picinin
p,q,r,
Paulo
Bittencourt
p,
Paulo
Camargos
r,
Fernanda
Peixoto
s,
Marcelo
Barciela
Brandão
t,
Tania
Maria
Sih
u,v,
Wilma
Terezinha
Anselmo-Lima
waUniversidadeFederaldeSãoPaulo(UNIFESP),EscolaPaulistadeMedicina(EPM),SãoPaulo,SP,Brazil bUniversidadeFederaldeGoiás(UFG),Goiânia,GO,Brazil
cPontifíciaUniversidadeCatólicadeGoiás(PUC-GO),Goiânia,GO,Brazil
dUniversidadeFederaldeGoiás(UFG),HospitaldasClínicas,UnidadedeCabec¸aePescoc¸o,Goiânia,GO,Brazil eUniversidadeEstadualdeCampinas(UNICAMP),FaculdadedeCiênciasMédicas,Departamentode
Oftalmo/Otorrinolaringologia,Campinas,SP,Brazil
fUniversidadeSãoPaulo(USP),FaculdadedeMedicinadeRibeirãoPreto,DepartamentodeOftalmologia,Otorrinolaringologiae CirurgiadeCabec¸aePescoc¸o,RibeirãoPreto,SP,Brazil
gUniversidadeFederaldeCiênciasdaSaúdedePortoAlegre(UFCSPA),PortoAlegre,RS,Brazil
hHospitaldaCrianc¸aSantoAntônio,Servic¸odeOtorrinolaringologiaPediátrica,PortoAlegre,RS,Brazil
iUniversidadeFederaldoRioGrandedoSul(UFRGS),ProgramadePós-graduac¸ãoemSaúdedaCrianc¸aedoAdolescente, PortoAlegre,RS,Brazil
jHospitaldeClínicasdePortoAlegre,PortoAlegre,RS,Brazil
kUniversidadeSãoPaulo(USP),HospitaldasClínicasdaFaculdadedeMedicinadeRibeirãoPreto,RibeirãoPreto,SP,Brazil lUniversidadeFederaldeSãoPaulo(UNIFESP),EscolaPaulistadeMedicina(EPM),DepartamentodeOtorrinolaringologiae CirurgiadeCabec¸aePescoc¸o,SãoPaulo,SP,Brazil
mAssociac¸ãodeAssistênciaaCrianc¸aDeficiente(AACD),ClínicadeOtorrinolaringologia,SãoPaulo,SP,Brazil nUniversidadeFederaldoCeará(UFC),Fortaleza,CE,Brazil
oHospitalPequenoPríncipe,Curitiba,PR,Brazil
pServic¸odeAssistênciaIntegralàCrianc¸aTraqueostomizada(SAIT),BeloHorizonte,MG,Brazil
夽
Pleasecitethisarticleas:AvelinoMA,MaunsellR,ValeraFC,LubiancaNetoJF,SchweigerC,MiuraCS,etal.FirstClinicalConsensusand NationalRecommendationsonTracheostomizedChildrenoftheBrazilianAcademyofPediatricOtorhinolaryngology(ABOPe)andBrazilian SocietyofPediatrics(SBP).BrazJOtorhinolaryngol.2017;83:498---506.
夽夽ThisarticleisaConsensusmadebyspecialistsonthesubject,andthus,approvalbytheResearchEthicsCommittees(REC)doesnot
apply.
∗Correspondingauthor.
E-mail:melissa.avelino@uol.com.br(M.A.Avelino).
PeerReviewundertheresponsibilityofAssociac¸ãoBrasileiradeOtorrinolaringologiaeCirurgiaCérvico-Facial.
http://dx.doi.org/10.1016/j.bjorl.2017.06.002
qUniversidadeJosédoRosárioVellano(UNIFENAS),CursodeMedicina,BeloHorizonte,MG,Brazil
rUniversidadeFederaldeMinasGerais(UFMG),HospitaldasClínicas(HC),PneumologiaPediátrica,BeloHorizonte,MG,Brazil sUniversidadeFederaldeGoiás(UFG),UnidadedeTerapiaIntensiva,Goiânia,GO,Brazil
tUniversidadeEstadualdeCampinas(UNICAMP),FaculdadedeCiênciasMédicas,DepartamentodePediatria,Campinas,SP,Brazil uUniversidadedeSãoPaulo(FMUSP),FaculdadedeMedicina,SãoPaulo,SP,Brazil
vInternationalSocietyforOtitisMedia(ISOM),SãoPaulo,SP,Brazil
wUniversidadeSãoPaulo(USP),FaculdadedeMedicinadeRibeirãoPreto,RibeirãoPreto,SP,Brazil
Received31May2017;accepted6June2017 Availableonline27June2017
KEYWORDS Tracheostomy; Child;
Guidelines; Consensus
Abstract
Introduction:Tracheostomyisaprocedurethatcanbeperformedinanyagegroup,including childrenunder1yearofage.UnfortunatelyhealthprofessionalsinBrazilhavegreatdifficulty dealingwiththisconditionduetothelackofstandardcareorientation.
Objective: Thisclinical consensus by Academia Brasileira deOtorrinolaringologia Pediátrica (ABOPe)andSociedadeBrasileiradePediatria(SBP)aimstogeneratenationalrecommendations onthecareconcerningtracheostomizedchildren.
Methods:A group ofexperts experiencedinpediatric tracheostomy(otorhinolaryngologists, intensivecarepediatricians,endoscopists,andpediatricpulmonologists)wereselected,taking intoaccountthedifferentregionsofBrazilandfollowinginclusionandexclusioncriteria. Results:Theresultsgeneratedfromthisdocumentwerebasedontheagreementofthemajority ofparticipantsregardingtheindications,typeofcannula,surgicaltechniques,care,andgeneral guidelinesanddecannulation.
Conclusion: Theseguidelinescanbeusedasdirectivesforawiderangeofhealthprofessionals acrossthecountrythatdealwithtracheostomizedchildren.
© 2017 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Published by Elsevier Editora Ltda. This is an open access article under the CC BY license (http:// creativecommons.org/licenses/by/4.0/).
PALAVRAS-CHAVE Traqueostomia; Crianc¸a; Diretrizes; Consenso
PrimeiroConsensoClínicoeRecomendac¸õesNacionaisemCrianc¸as
TraqueostomizadasdaAcademiaBrasileiradeOtorrinolaringologiaPediátrica(ABOPe)
eSociedadeBrasileiradePediatria(SBP)
Resumo
Introduc¸ão: A traqueostomiaé umprocedimento quepodeser realizado em qualquerfaixa etária, inclusive em crianc¸as abaixo de um ano. Infelizmenteno Brasil existeuma enorme dificuldadedosprofissionaisdesaúdeemlidarcomestacondic¸ãoeumafaltadepadronizac¸ão doscuidados.
Objetivo: Este consenso clínico realizado pela Academia Brasileira de Otorrinolaringolo-gia Pediátrica (ABOPe) e Sociedade Brasileira de Pediatria (SBP) tem como objetivo gerar recomendac¸õesnacionaissobreoscuidadosecondutasdiantedascrianc¸astraqueostomizadas. Método: Foramselecionadosumgrupodeespecialistascomexperiênciaemtraqueostomiana infância(otorrinolaringologistas,pediatrasintensivistas,endoscopistas,pneumopediatras)que tivessemcomprovadaatuac¸ãopráticanoassunto,equetambémcontemplassemasdiversas regiõesdoBrasil,deacordocomoscritériosdeinclusãoeexclusão.
Resultados: Osresultadosgeradosnestedocumentoforamapartirdaconcordânciadamaioria dos participantes em relac¸ãoas indicac¸ões,tipo decânula, técnicascirúrgicas, cuidadose orientac¸õesgeraisedecanulac¸ão.
Introduction
The internationalliterature traditionally reportsthe need fortracheostomyinapproximately0.5---2%ofchildren under-going intubation and mechanical ventilation in intensive care units. In the last 60 years, changes in the epidemi-ologyof infectious diseases and the evolution of medical techniqueshavechangedtheindicationsfortracheostomy. Tracheostomy can be performed in children of any age group,includinginfantsunder1-yearof age.Theincrease in the use of tracheostomy in this age group has been attributed tothe greater survival of preterm infants and those requiring prolonged ventilation.1 This procedure, when performed in children and especially infants and newborns,hasbeen associatedwithgreatermorbidityand mortalitywhencomparedtoadults.2,3
Regardingtheindicationsoftracheostomyinchildhood, wehaveseensignificantchangesinrecentyears.4,5
It can be currently observed that in Brazil huge diffi-cultyforhealthprofessionalstodealwiththisconditionis apparent,aswellasthelackofcarestandardization.Atthe worldwidelevel,thisproblemhasbeenattenuatedinother countriesinrecentyears,throughthediscussionand sugges-tionofconsensuses amongprofessionalswhohave contact withtracheostomizedchildren.6---9
Thecreationofspecificcareteamsforthesechildrenhas showntooptimizecareandcanpotentiallyreducenotonly the hospitalcosts but alsothe suffering of the child and thefamilyinvolved,promotingimprovedcarewithresolute perspectives.10Somestudiesintheliteraturehavedepicted thedifficultiesandthenegativeimpactfor thechild, par-entsand/orcaregivers inthepresenceoftracheostomyin childhood.11,12
In a review paper published in 2016 on tracheostomy complications,13comparedthelast3decades,thepresence of granuloma, infection and cannula obstruction are still amongthemost frequentproblems,thatis, theonesthat dependoncareandguidelines.Unfortunately,thereareyet nolinesofcareforthatmatterinourcountry.
Themortalityratesrelatedtotracheostomyinchildren rangefrom0% to5.9% in the international literature.13 A BrazilianstudycarriedoutinPortoAlegrein2009reported amortalityrateof4%.14
In Brazil, this lack of care standardization is due to thelack of national guidelinestoguidethe Brazilian Uni-fiedHealthSystem(SUS---Servic¸oÚnicodeSaúde)andthe NationalHealthAgency(ANS---AgênciaNacionaldeSaúde), which is reflected in the lack of availability of material needed to care for these patients, such astracheostomy cannulasin themedicalcare services,aswellasthe lack oftrainingofthemedicalandnon-medicalteamsthattreat theseyoungpatients. Withoutpropertraining forcannula replacement, these children are maintained in the Ter-tiary System for these procedures, without assistance or basicguidelines.Unfortunately,eveninthemajorcenters andTertiaryHospitals,thesebasicmaterials(tracheostomy tubesforregularchange)arenotavailable,sothesechildren belongtothesystem,buttherearenocodesinSUSthat con-templateperformingthisprocedure,whichisessentialfor thechildnottodevelopemergencysituations,suchas air-wayobstructionorhospitaladmissionduetolunginfections. Therefore,afterbeingtracheostomized,thesechildrenare
often lost in the public system, as there is no adequate flowofreferralandfollow-up,asitoccurswithother life-threateningdiseases.
In 2016, the Brazilian Academy of Pediatric Otorhino-laryngology (ABOPe --- Academia Brasileira de Otorrino-laringologiaPediátrica)duringitsmostimportantnational scientificevent,launchedtheprojecttocarryoutaNational Consensus for recommendations in tracheostomized chil-dren.Thus,theaimofthisConsensusistoobtaintheopinion ofagroupofexpertsintracheostomizedchildren,aimingto establishnationalguidelinesformedicalconductsandcare, allowing in thenear futurethe creationof ‘‘standards of care’’andthecreationofaflowchartforthereferraland treatmentofthesechildrenintheUnifiedHealthSystem.
Methods
During a meeting, we requested colleagues from differ-entregionsofthecountrytocreateagroupof expertson the subject. We alsorequested the opinion of colleagues whowerenotpresent,butwhohadacknowledgedpractical experienceinthisareaandwereinterestedinparticipating inthisproject.
Two initial coordinators, with proven practical experi-enceinPediatricAirwaysinNationalUniversityInstitutions, in additiontoscientificactivities in thesubject, received indicationsfortheselectionofthegrouptobecreated.The BrazilianSociety ofPediatricswasapproachedandinvited toprovidesupportandpartnershipinthiswork,andit indi-catedmemberswhowerepediatriciansandexperiencedin thecareof tracheostomizedchildrentoparticipateinthe consensus.
Inclusioncriteriaforselectionoftheexpertgroup
- DeclaredinterestinparticipatingintheConsensus; - Otorhinolaryngologists with proven experience in
pedi-atric airways, either through consistent publications on the subject, or by practicing in referral services in the country;
- Otorhinolaryngologistswhowerenotpresentatthe meet-ing, but who the coordinators considered important regardingtheirperformanceintheareainourcountry; - GroupofpediatriciansdesignatedbytheBrazilianSociety
of Pediatrics: intensivists, bronchoscopists, pulmonolo-gists with proven experience in the management of tracheostomizedchildren.
Exclusioncriteria
- Nothavingexpressedaninterestinparticipatingafterthe invitation;
- Anotherrepresentativefromthesameservicewasalready participatingintheConsensus;
- Not having broad performance or continuous clinical practicewithtracheostomizedchildren.
43 multiple-choice questions was discussed. Those ques-tionsfor whichtherewasanagreementofmorethan50% ofparticipantsregardingtheanswer wereconsideredasa consensus.Whennoneoftheanswersobtaineda50% agree-ment, the results were presented for each question and theconsiderationswerediscussedbythegroup.Participants wereaskedtoanswerbasedonwhattheyconsideredideal, eventhoughtheymightnotnecessarilybeabletopractice thatintheirservicesduetofinancialandlogistical limita-tions.Questionsonsurgicaltechniqueswereansweredonly byparticipatingsurgeons.
The questions were divided into topics: tracheostomy indications,typeofcannula,surgicaltechnique,care, guid-ance,anddecannulation.
During the consensus, the need to create guidelines relatedto daily practiceconcerning phonatoryvalve use, complications, speechtherapy indication,andattendance atschoolactivitiesoratdaycarecenterswasalsoraised.
Results
Indications
Itwastheconsensusamongthemembersthattracheostomy in children shouldbe performed in a surgical center. The Consensus members considered it essential to perform a preoperativeendoscopicairwayevaluation(EAE)beforethe tracheostomy toassess the causes of respiratory obstruc-tionandbasedonthe findingsandthefuturetherapeutic proposal, decide the best location for the tracheostomy. In cases where it is impossible to perform this examina-tion prior to the tracheostomy, it is suggested that it be performedaftertheproceduretoverifytheadequate tra-cheostomypositioning,for thefollow-upofthetreatment ofairwaypathologies,toguidefuturetreatments,aswell as to report the presence of a patent airway above the tracheostomy.Airwayendoscopyisunderstoodasthe exam-inationfromthenasalcavitiestothemainbronchi,making it possible to evaluate all possible points of upper air-way obstruction. The examination with flexible and rigid
endoscopesshouldbeperformedwheneverpossible.Ideally, airwayendoscopy should be performed in a surgical cen-terunderanesthesiainspontaneousventilation,forgreater safetyandopportunitytoaddresseventualpathologies dur-ingthesameexamination.
Iftheendoscopicevaluationisnotpossibleat thetime ofthetracheostomy,theconsensusmembersconsideredit shouldbeindicatedasearlyaspossible,ideallyupto15days afterthetracheostomy,andnolaterthan30daysafterthe procedure.Thisindicationisabsolute,consideringthatthe effectontheinflammatory processinitsacutephasecan modify the prognosis, particularly in the case of stenotic lesionswithscarringofthelarynx.
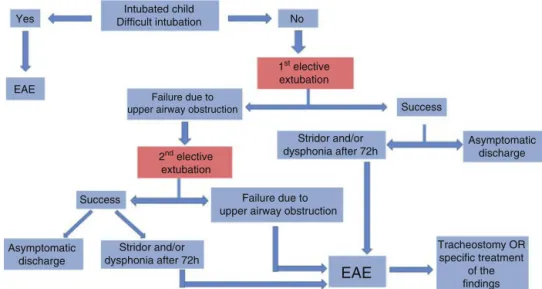
Inthecaseofchildreninanintensivecareunit(ICU)with extubationfailureduetohighrespiratoryobstruction,the membersconsideredtheindicationofairwayendoscopyto beabsoluteinthefollowingsituations:
- afterthesecondelectiveextubationfailureand/or; - in the persistence of stridor or dysphonia after 72h of
extubation.
Inthecaseofchildrenwithahistoryofdifficult intuba-tion,airwayendoscopyissuggestedbeforethefirstelective extubation(Fig.1).
The tracheostomy indications shouldguide thetype of cannulaandventilatorysupportrequired,aswellas follow-upand therapeutic anddecannulation planning. Allthese variablesandperspectivesshouldbediscussedwiththe fam-ilysincetheindicationofthetracheostomy.
Cannulatypes
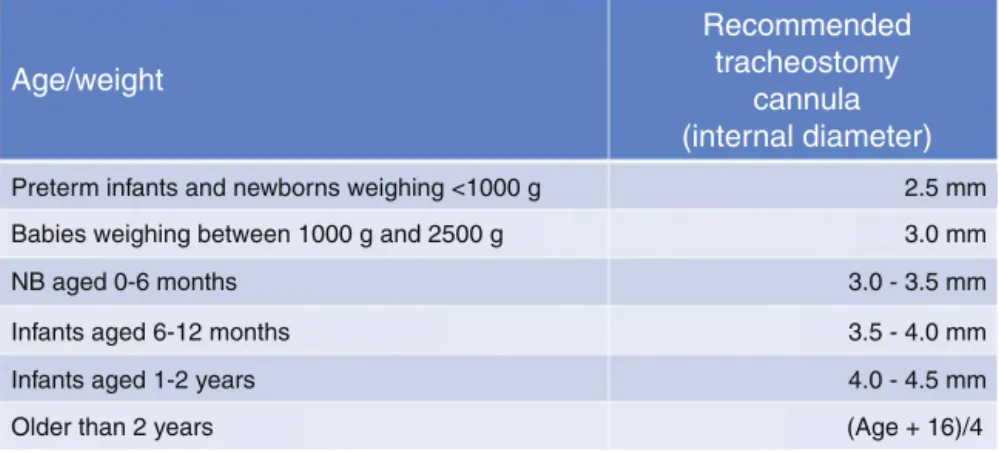
Thesizesofthecannulashouldbeadequateforthechild’s weightandage(Fig.2---cannulasizes),andtheuseofcuffs isindicatedonlytooptimizeventilationandtotemporarily reducetheimpactofaspiration,whenpresent.
Whenindicated,theuseofcuffpressureshouldbe mea-suredandmaintainedatthemaximumupto20cmH20or 15mmHg.
Yes No
Success
Success
Asymptomatic discharge EAE
EAE
Intubated child Difficult intubation
Failure due to upper airway obstruction
Stridor and/or dysphonia after 72h
Stridor and/or dysphonia after 72h
Failure due to upper airway obstruction
Asymptomatic discharge
Tracheostomy OR specific treatment
of the findings 1st elective
extubation
2nd elective extubation
Age/weight
Preterm infants and newborns weighing <1000 g 2.5 mm
3.0 mm
3.0 - 3.5 mm
3.5 - 4.0 mm
4.0 - 4.5 mm
(Age + 16)/4 Babies weighing between 1000 g and 2500 g
NB aged 0-6 months
Infants aged 6-12 months
Infants aged 1-2 years
Older than 2 years
Recommended
tracheostomy
cannula
(internal diameter)
Figure2 Diameteroftracheostomycannulaappropriateforage/weight.Thenumberofthetracheostomycannulacorresponds totheinternaldiameterinmillimeters(mm).NB,newborn;g,grams.
Table1 Descriptionofthetracheostomycannulasmostfrequentlyfoundinthenationalmarketwithcompositionmaterialand durabilityindicatedinthepackageinsertbythemanufacturer.
Canulla/brands Material Durability
SHILEY SiliconizedPVC 28days---cleansingandreusearenotrecommended.
PORTEX PVC 29days---cleansingandreusearenotrecommended.
BIVONA Silicone 9monthswithcleansingevery30days
TRACHOE SiliconizedPVC 120days
COMPERa PVC 30days
aAttentionregardingthedimensionsofthiscannula,ofwhichlengthisonaverage7mmlongerthantheothers.
The use of biocompatible siliconized or plastic tra-cheostomycannulas(Table1)isrecommended.Theuseof metalcannulasisnotrecommendedinchildrenduetotheir lowbiocompatibility,lackofmalleabilityandgreaterriskof trachealinjury,sincechildren,unlikeadults,donotrestrict theircervicalandbodymovementswhentheysubmittedtoa tracheostomy.Theadaptationofcannulaswithinadequate lengthsisnot recommendedeither.The easy cleansingof theinternalmandrelcreatesafalsesenseoflow obstruc-tionrisk,whichhasnotbeendemonstratedbyevidence,and candelaytheexchangeofthecannulas.Furthermore,itis necessarytoconsiderthattheinternalmandrelreducesthe cannulalumenand canleadtorespiratory failuredespite thesupposedlyadequatesizefortheage.
Surgicaltechnique
Thesurgicaltechniqueusedbysurgeonsshouldvary accord-ingto theage group and thepathology. Even considering these variables, all surgeons use nonabsorbable repair suturesorstomamaturationwithabsorbablesuturesfixing thetracheatotheskindependingonthepatient’sageand characteristics,orthecharacteristics andrequirementsof the intensive care unit. Another variablediscussion point according to the patient’s pathology is the height of the tracheostomy,whichwilldepend onthediagnosisandthe futuretreatmentfordecannulation.
Itwasaconsensusamongtheauthorsthatthefirstchange should occur after one week of the tracheostomy, when thenonabsorbablesutures shouldalsoberemoved to pre-ventexacerbationofthelocalinflammatoryprocesses.The
use ofantibioticprophylaxis is recommended,anda first-generationcephalosporinisusuallyused.Theindicationof chestX-rayaftertracheostomyshouldbeconsideredin chil-dren under one year of age, to certify that the cannula is well-positioned in relation to the carina if there is no intraoperative endoscopy confirmation. In older children, thepostoperativechestX-raymaybestandardizedinsome intensivecareunits,butitisnotroutinelyrecommendedby thegroup.
There was no consensus on the need to fix the tra-cheostomy cannula to the skin; however, 44.4% of the participatingsurgeonsreportedusingthisfixation.Inturn, 33.3%ofsurgeonsfixthetracheostomycannulatotheskinin thefirstweekonlyinspecialcircumstances;andtheothers donotthinkitnecessarytoperformthisfixation,usingonly thecord.
Careandrecommendations
Aspiration
Adviceonaspirationtechnique,needforhumidification,and regularcannulachangesbeforedischargeisalways recom-mended. It is imperative that surgeons who perform the tracheostomyprovidetheserecommendationsthemselves, evenifthereisamultiprofessionalteamcapableoftraining thecaregivers.
DATA OF PATIENT WITH TRACHEOSTOMY
NAME OF THE PATIENT:
Hospital:
Attending physician:
Size of cannula
External diameter
Internal diameter
Presence of cuff
Aspiration Length
Size of catheter: Depth of
catheter: cm
Applicable considerations:
CRITICAL ALERT: AIRWAY PATENCY ABOVE THE CANNULA YES NO
Cuff insufflation: no yes
If yes: water air volume: ____ mL
Date of last change: ______/______/___________
Form filled out by:
Figure3 IDcardofthetracheostomizedchild(CICT).
materials available at home should include: non-sterile gloves, single-use disposable aspiration catheters, and a tracheostomy cannula half-size smaller than the one being used. A modified clean technique, as defined by the American Thoracic Society (ATS) is recommended for cannula handling, aspiration and change of dressing and cord:non-sterilegloves,butsterileaspirationcatheters.
Theaspirationtechniquecanshowslightvariations,but ingeneral,itshouldbegentleyetefficient.Attentionshould begivento:
- choiceofcathetersize,notexceedingtwo-thirdsof the sizeofthecannula;
- depthofaspirationtopreventtraumatothetracheadistal tothecannulatip;
- aspirationtimetopreventhypoxia,pneumothorax,vagal reflexes.
Regarding thetypeofcannulafixation,thereisno evi-dence to recommend any preference between cord and Velcro. Therewasaconsensusamongtheexperts thatno specifictypeofaspiratorhasprovensuperiorefficiency.
It is recommended that the services provide a tra-cheostomizedchildwithanidentification cardatthetime ofhospitaldischarge(Fig.3),whichshouldincludethe fol-lowinginformation(cardtemplate):
- nameandageofthechildanddateoftracheostomy; - criticalalertspecifyingwhethertheairwayabovethe
tra-cheostomyispatentornot;
- sizeofthecannulabeingusedandrecommended aspira-tioncatheternumber;
- recommendedaspirationdepth;
- identificationofthehospitalorreferralservicethat fol-lowsthechildandtheattendingphysician.
List of suggested materials per month:
120 Units of urethral catheters (discriminate caliber)
120 ampoule units (10mL vials) of 0.9% saline solution
60 packs of sterile gauze dressings (packs with 5 units)
3 boxes of procedure gloves
1 unit of Micropore™ Surgical Tape 25mmX10
1 unit of fixation cord (every 3 months)
1 150mL container of alcohol
Optional (reque
sted by
the assisting
team)
1 ambu for children (Silicone Face Mask) without reservoir
Permanent material for emergencies:
1 tracheostomy cannula half-size smaller than the one being used
Xylocaine gel or other lubricant to facilitate passage of the cannula
Figure4 Monthlylistofmaterials.
In case of accidental decannulation, a cannula of the same size or a smaller one should be used for replace-ment.Iftheseareunavailable,werecommend theuseof a half-smaller size tracheal tube, followed by the imme-diate referral of the child to the reference service for tracheostomycannularepositioning.Thegroupalso empha-sizes the importance of teaching parents about the risk of decannulation, and of demonstrating the child’s posi-tion(cervicalhyperextension)forthisrepositioning,aswell as stoma exposure, by moving away the skin from the region.
Stomahygieneoncedailyisrecommended,ormore fre-quently,dependingontheclimaticconditionsandthechild’s generalhealth status,presence ofexcessivesecretions or localcomplications.Theroutineuseofointmentsisnot rec-ommended,exceptinthepresenceofsignsofinflammation oftheperistomalskin.Inthecaseofointmentuse,itshould alwaysfollowmedicalprescription. Theuseofgauzepads betweenthecannulaandtheskinoftheneckisalso debat-able,anditisa consensusthat themostimportanteffort wouldbe topreventthe accumulation of moisturein the peristomalskinregion.Sometimestheuseofgauzepadscan promotetheaccumulationandretentionofsecretionsand peristomalmoisture,andthus, ifused,gauzepadsshould bechangedwhenevertheyaresoiled.
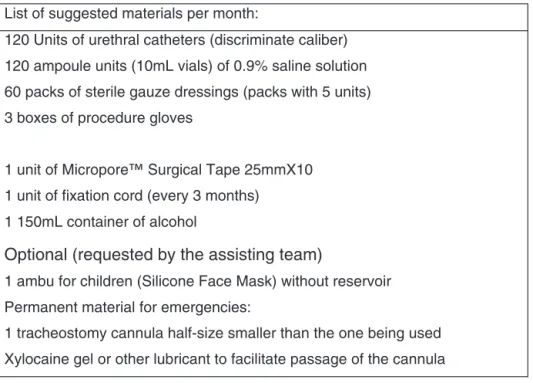
Establishingstandardizedprotocolswouldreducetherisk of complications, particularly thoserelated tothe occur-rence of peristomal inflammatory processes. Creating an emergencychecklistcouldreducetheriskofthemostfeared complicationofall,i.e.,accidentaldecannulation(Fig.4). Inhalation, nebulization,and humidification. The use of inhalation and nebulization should follow medical guide-lines, and the practice of inhalation with physiological solutionsand itsbenefitaimingat humidifyingtheairway isnotwellestablished.Aimingtokeeptheairwayhydrated andhumidified,itis alwaysnecessary torecommendthat
the child maintainan adequate water intake,considering thegreaterfluidlossduetothetracheostomy.
The useof hydroscopic filters or ‘‘false nose’’may be usefulinmostcasesandtheirindicationshouldbe individ-ualizedineachcase,dependingontheamountofsecretion and,especially,thechild’slungfunction.
Secretionculture. Thetracheostomyisanareacolonized by microorganisms. The collection of tracheal secretions would be indicated only in cases of tracheitis with hos-pitalization indication or in the preoperative period of laryngotracheal reconstruction surgeries to guide intra-venousantibiotictherapy.Itisworthrememberingthatthe diagnosisoftracheitisisbasedonclinicalcriteria:increase and/or alteration in trachealsecretions associated or not withfever,worseningofthegeneralhealthstatusand tachy-cardiainthepresenceofanormalchestX-ray.Thecultureof trachealsecretionisindicatedtoguidetheantibiotic ther-apyinseverecases,forwhichhospitalizationisrequired. Phonatory valves. The use of phonatory valves is rec-ommended both to facilitate communication and speech development,andperhapsmainlytoreducetheriskof bron-choaspiration,promotingthereturnofsubglotticpressure. Theuseofphonatoryvalvesiscontraindicatedincasesof:
- Severeairwaystenosis;
- Needtousecannulawithaninsufflatedcuff; - Severetracheomalacia;
- Restrictivepulmonarydisease;
- Severeneurologicaldisorderorcomatosepatient.
Complications
Persistent trachea-cutaneous fistulas after decannulation are considered minor complications of tracheostomies. If theypersistafterthreemonths,medicalevaluationfor sur-gicalclosureshouldbeindicated.
Granulomas are quite frequent complications of tra-cheostomies and may occur externally in the stoma, or internallyinthetrachea.Forexternalgranulomas,in addi-tiontothe use oftopical medications,thereinforcement in local care is indicated. Internal granulomas should be approached when obstructive, and especially during the decannulationprocess,evenwhenthereispartial obstruc-tion.
Speechtherapyandaudiologicalevaluation
Speechtherapyandaudiologicalevaluationhavebeen rec-ommended in tracheostomized children in the prelingual periodforcommunicationdevelopmentandincasesof dys-phagia.
Decannulation
The followingwereconsidered factorsthatcontraindicate decannulation:
- AbsenceofEAE;
- Dependence on mechanical ventilation in the last 3 months;
- Dependenceontracheostomyforpulmonarytoilet.
After detailed and complete evaluation of the airway while the childis awake andunder anesthesiaon sponta-neousventilation, the followingdecannulation protocol is suggestedforchildrenolderthan2years:
- Progressivereductionincannulasize; - Cannulaocclusionduringthedayathome;
- 68.75% of the authors believe that nocturnal occlusion of the cannulashould be carried out only in a hospital environment;
- Decannulation of patients with comorbidities should be carriedoutattheintensivecareunitinthefirst24h; - Observationinhospitalenvironmentforatleast48hafter
decannulation.
Forchildrenunder2yearstherecommendedprotocolis:
- Thecannulaocclusionperiodpriortodecannulationisnot necessary;
- Observationduringthefirst24hafterdecannulationinthe ICUregardlessofcomorbidities;
- Observationinhospitalenvironmentforatleast72hafter decannulation.
Performingapolysomnographywithanoccludedcannula, although recommendedbysome services,wasnot recom-mendedbythegroup.Theperformanceofairwayendoscopy whilethechildisunderinducedsleepandobservationofthe respiratorypatternduringtheexaminationandalsointhe
hospitalwasconsideredsufficienttoruleoutthepresence ofobstructionthatpreventsdecannulation.
Accesstoschool
Thepresenceoftracheostomyaloneshouldnotpreventthe childfromattendingschool.However,itisnecessarythata qualifiedpersonprovidethenecessarycare,including can-nulaaspirationandclearing,ifnecessary.
Final
considerations
This consensus was created aiming to generate national guidelinesbyspecialistsinrelationtothemedicalpractices andcareoftracheostomizedchildren,butitisnoteworthy toemphasizethatitdoesnotmeantheymustbefollowed exactlyastheywereportrayedhere.Weacknowledgethe diversityand limitations of ourvast country, but we also deem it extremelyimportant that our publicentities pay specialattentiontothisgroupofchildren,who,astheyhave atracheostomy,becomesovulnerable.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.CorbettHJ,MannKS,MitraI,JesudasonEC,LostyPD,Clarke RW.Tracheostomy---a10yearexperiencefromaUKpediatric surgicalcenter.JPediatrSurg.2007;42:1251---4.
2.PereiraKD,MacGregorAR,MitchellRB.Complicationsof neona-taltracheostomy:a5-yearreview.OtolaryngolHeadNeckSurg. 2004;131:810---3.
3.Ruggiero FP, Carr MM. Infant tracheotomy: results ofa sur-vey regardingtechnique. Arch Otolaryngol Head Neck Surg. 2008;134:263---7.
4.ButnaruCS,ColreavyMP,AyariS,FroehlichP.Tracheotomyin children:evolutioninindications.IntJPediatr Otorhinolaryn-gol.2006;70:115---9.
5.HadfieldPJ,Lloyd-FaulconbridgeRV,AlmeydaJ,AlbertDM, Bai-leyCM.Thechangingindicationsforpaediatrictracheostomy. IntJPediatrOtorhinolaryngol.2003;67:7---10.
6.BestPracticeStatement:Caringforthechild/youngpersonwith atracheostomyScotland.www.nhshealthquality.org.Set2008. 7.MitchellRB,HusseyHM,SetzenG,JacobsIN,NussenbaumB, DawsonC,etal.Clinicalconsensusstatement:tracheostomy care.OtolaryngolHeadNeckSurg.2013;148:6---20.
8.UrrestarazuP,VarónJ,RodríguezA,Ton V,VilaF,CiprianiS, etal.Consensosobreelcuidadodelni˜nocontraqueostomía. ArchArgentPediatr.2016;114:89---95.
9.Strychowsk JE, Albert D, Chan K, Cheng A, Daniel SJ, De Alarcon A, et al. International Pediatric Otolaryngology Group(IPOG)consensusrecommendations:routine periopera-tivepediatrictracheotomycare.IntJPediatrOtorhinolaryngol. 2016;86:250---5.
10.Abode KA, Drake AF, Zdanski CJ, Retsch-Bogart GZ, Gee AB, Noah TL. A multidisciplinary children’s airway center: impactonthecareofpatientswithtracheostomy.Pediatrics. 2016;137:e20150455.
12.HartnickC,BisselC,ParsonsSK.Theimpactofpediatric tra-cheotomyonparentalcaregiverburdenandhealthstatus.Arch OtolaryngolHeadNeckSurg.2003;129:1065---9.
13.Dal’AstraAP,QuirinoAV,CaixêtaJA,AvelinoMA.Tracheostomy in childhood: review ofthe literature on complications and
mortalityoverthelastthreedecades.BrazJOtorhinolaryngol. 2017;83:207---14.