ORIGINAL ARTICLE
Four-year randomized clinical trial of oxalic acid pretreatment
in restorations of non-carious cervical lesions
Nadine Luísa Guimarães Albuquerque1&André Mattos Brito de Souza1,2&
Maria Denise Rodrigues de Moraes1,2&Juliano Sartori Mendonça1&
Lidiany Karla Azevedo Rodrigues1&Sérgio Lima Santiago1
Received: 2 December 2014 / Accepted: 30 June 2015 / Published online: 15 July 2015
#Springer-Verlag Berlin Heidelberg 2015
Abstract
Objective The aim of this study was to evaluate the efficiency of oxalic acid (BisBlock) on restorations of non-carious cer-vical lesions.
Materials and methodsOne operator placed 90 restorations randomly divided into two groups in 20 patients under cotton rolls isolation: Control Group—two-step etch-and-rinse adhe-sive technique; and Experimental Group—two-step etch-and-rinse adhesive technique with oxalic acid pretreatment after acid-etched dentin. The restorative adhesive system used was XP Bond/Durafill. The restorations were directly assessed by two independent examiners, using the modified United States Public Health Service (USPHS) criteria at the baseline and 4 years. Data were statistically analyzed using the Fisher and McNemar tests (p< 0.05).
ResultsFifteen patients (75 %) were available for recall after 4 years. The McNemar test detected significant differences within the Experimental Group between the baseline and 4-year evaluations for retention (p < 0.05). For the Control Group, there was no significant difference (p> 0.05) between the periods. The Fisher test showed no statistically significant difference between the groups for all other criteria (p> 0.05).
Conclusion After 4 years of service, the use of oxalic acid did not influence the clinical performance of restorations when it was used under composite resin restorations.
Keywords Adhesive . Clinical trial . Dentin hypersensitivity . Oxalates
Clinical relevance
Dentin pretreatment with oxalic acid means an additional step in the etch-and-rinse adhesive technique and although being effective in reducing dentinal hypersensitivity may impair the retention of adhesive restorations over time.
Introduction
Non-carious cervical lesions (NCCLs) are related to many factors including erosion, abrasion, gingival recession, peri-odontal surgery, and abfraction [1,2]. These lesions are sig-nificantly more prevalent in older people, with premolars be-ing the most affected teeth [3], and are usually associated with dentin hypersensitivity due to the exposure of dentin in the oral environment [4,5]. When loss of enamel and/or cement occurs, the dentinal tubules are exposed to the oral environ-ment and the presence of certain stimuli causes the displace-ment of fluids within the tubules, indirectly stimulating the pulp nerve endings and causing the sensation of pain. The hydrodynamic theory is the most widely accepted hypothesis to explain how stimuli applied on the dentin surface influence nerve fibers [6]. Therefore, dentin hypersensitivity being a painful oral condition affecting the quality of life for many people [7] and to a correct diagnosis a patient’s history * Sérgio Lima Santiago
sergiosantiago@ufc.br
1 Department of Operative Dentistry, Faculty of Pharmacy, Dentistry
and Nursing, Federal University of Ceará, Fortaleza, Ceará, Brazil
2
School of Dentistry, University of Fortaleza, Fortaleza, Ceará, Brazil
3
Rua Monsenhor Furtado s/n, Rodolfo Teófilo, Fortaleza, CE 60430-355, Brazil
screening and a brief clinical examination is necessary in order to avoid false diagnosis [8].
In an attempt to reduce this discomfort, several desensitizing agents such as calcium hydroxide, stannous fluoride, arginine, glutaraldehyde, and oxalates have been used [5, 9–16]. These agents promote the occlusion of the dentinal tubules, thereby reducing the movement of the fluids within the tubules and, consequently, reducing dentin sensi-tivity [5,9].
Oxalate-based desensitizing agents, derived from oxalic acid, were introduced as an option treatment for dentin hypersensitivity in the 1980s. These agents are being increasingly used because they act not only by obliterating the dentin tubules, with the precipitation of calcium oxalate crystals on the surface and inside the dentin tubules, but also by depolarizating the nerve end-ings [10, 11, 17], preventing the conduction of current which leads to pain. Thus, these products have satisfac-tory efficacy for neural and physical action [18]. A re-cent study about dental practice suggests the use of oxalate in the treatment of dentinal hypersensitivity in 40 % of the cases [19].
Furthermore, oxalate-based desensitizing agents are al-so being studied in laboratorial studies as an alternative for inclusion in restorative procedures with the additional effect of improving resin-dentin bonds over time [20]. When applied on acid-etched dentin, calcium oxalate crystals tend to form only in the dentin tubules, leaving the dentin surface unobstructed and available for bonding with dental adhesives [21,22]. The use of oxalate during bonding procedures could enhance solvent evaporation by decreasing the amount of water entrapped within these adhesives, allowing for better control of the adequate wet and facilitating the penetration of adhesives into wet demineralized dentin [14,22,23]. However, the stability of this bond needs to be evaluated in long-term clinical trials. Taking into consideration the lack of long-term studies that assess the clinical performance of restorative procedures associated with oxalate-based desensitizing agents, the aim of this study was to evaluate the longevity and clinical success of restorations in non-carious cervical lesions with or without the application of oxalic acid. The null hypothesis tested was that both technics have similar effectiveness after 4 years of clinical service.
Methods and materials
Study design
The study was reported following the CONSORT statement [24]. This is a controlled, blind, and randomized clinical trial. The local Ethics Committee on Investigations Involving
Human Subjects reviewed and approved the protocol and con-sent form for this study (protocol #224/08).
Sample size calculation
The following parameters were set for sample size calculation: expected proportion was 0.85, relative standard error of 10 %; the power of the test was calculated to be 80 % (beta error); and the two-tailed alpha error to be 5 %. Based on this, a sample size of 18 subjects was found to be necessary. Taking into consideration possible loss during the study, a 10 % in-crease in sample size was set.
Inclusion and exclusion criteria
Twenty volunteer patients of both sexes (16 female, 4 male), ranging in age from 24 to 55 years old, were examined to determine if they met the inclusion and exclusion criteria. Anamnesis, photographs, and radiographic examinations were performed, followed by the clinical evaluations, using a mouth mirror, an explorer, and a periodontal probe. All selected patients were properly instructed about the condition and objectives of the study and signed an informed consent and authorization form in order to participate in this investigation.
The following were the criteria for inclusion of a patient in this study: appropriate oral hygiene; absence of caries and periodontal disease; bruxism and traumatic occlusion; no wear facets; presence of at least two non-carious cervical lesions with a depth equal or greater than 1 mm, independently of their location in the dental arcade to be restored. Patients with extremely poor oral hygiene, severe or chronic periodontitis, or heavy bruxism habits were excluded from the study.
The degree of hypersensitivity was determined according to the Verbal Rating Scale (VRS) from 0 to 3, in which: 0 = no discomfort; 1 = minimum discomfort; 2 = mild discomfort; and 3 = intense discomfort. Each tooth received air blast stim-uli with an air syringe for 1 s at a distance of 1 cm from the tooth surface, and the presence of sensitivity was used to en-roll in the study.
Restorative procedure
A total of 90 restorations in 20 patients were performed by one operator, and 45 of these had a prior treatment with oxalic acid (Bisblock-BISCO Inc. Schaumburg, IL, USA) after etch-ing. The remaining 45 were used as control. The treatment used for each tooth was randomly set using a table created in the Excel system (Microsoft, NM, USA).
Initially, the operator anesthetized the teeth (Mepiadre® 100, Nova DFL, Rio de Janeiro, RJ, Brazil) and cleaned all lesions with pumice and water in a rubber cup (KG Sorensen, Barueri, SP, Brazil). This step was followed by rinsing and drying.
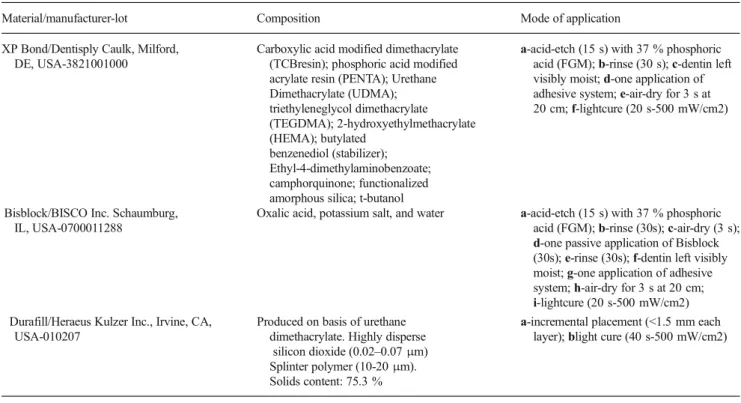
The restorative technique and the materials used are de-scribed in Table1. Resin composite increments were inserted and light-cured for 40 s using a calibrated light-curing unit (Vip Junior, Bisco Inc., Schaumburg, IL, USA) at 500 mW/ cm2with a curing radiometer (Demetron/Kerr, Orange, CA, USA). Composite excess was immediately removed using a #12 scalpel blade. Finishing and polishing was performed using 12-fluted tungsten carbide burs (FG Bur, KG Sorensen, São Paulo, Brazil), abrasive cups (Enhance, Dentsply-DeTrey GmbHD Konstanz, Germany), and disks (Sof-Lex polishing disks, 3 M ESPE, Seefeld, Germany).
Clinical evaluation
The restorations were evaluated at baseline and 4 years by two experienced and calibrated examiners other than the operator.
The clinical evaluation was performed using a mirror and a double-ended probe after tooth prophylaxis with water and pumice in a low-speed hand piece. For training purposes, the examiner observed 10 photographs that were representative of each score for each criterion. In cases where the two exam-iners disagreed on a rating, both re-examined the restoration and arrived at a final joint decision in order to obtain only one score for each restored tooth. The intra-examiner Cohen’s Kappa statistic was 0.9.
Modified United States Public Health Service criteria [25] were used to evaluate retention, marginal integrity, marginal discoloration, postoperative sensitivity, anatomic form, and caries (Table2) at the baseline and 4-year periods. Alfa and Bravo scores were classified as clinically acceptable. The baseline rating was carried out 1 week after restoration, im-mediately after the finishing and polishing procedures.
Statistical analysis
The statistical analysis compared the ratings of each criterion between groups in the different periods using the Fisher’s exact test. Intragroup comparisons between the baseline and 4 years with the same technique were performed by the McNemar test. Statistical procedures were performed using the Statistical Package for Social Sciences (SPSS 17.0) for Windows. The significance level for all statistical evaluations was set at 5 %.
Table 1 Materials, composition, and mode of the application of the materials
Material/manufacturer-lot Composition Mode of application XP Bond/Dentisply Caulk, Milford,
DE, USA-3821001000
Carboxylic acid modified dimethacrylate (TCBresin); phosphoric acid modified acrylate resin (PENTA); Urethane Dimethacrylate (UDMA); triethyleneglycol dimethacrylate (TEGDMA); 2-hydroxyethylmethacrylate (HEMA); butylated
benzenediol (stabilizer); Ethyl-4-dimethylaminobenzoate; camphorquinone; functionalized amorphous silica; t-butanol
a-acid-etch (15 s) with 37 % phosphoric acid (FGM);b-rinse (30 s);c-dentin left visibly moist;d-one application of adhesive system;e-air-dry for 3 s at 20 cm;f-lightcure (20 s-500 mW/cm2)
Bisblock/BISCO Inc. Schaumburg, IL, USA-0700011288
Oxalic acid, potassium salt, and water a-acid-etch (15 s) with 37 % phosphoric acid (FGM);b-rinse (30s);c-air-dry (3 s);
d-one passive application of Bisblock (30s);e-rinse (30s);f-dentin left visibly moist;g-one application of adhesive system;h-air-dry for 3 s at 20 cm;
i-lightcure (20 s-500 mW/cm2) Durafill/Heraeus Kulzer Inc., Irvine, CA,
USA-010207
Produced on basis of urethane dimethacrylate. Highly disperse
silicon dioxide (0.02–0.07μm)
Splinter polymer (10-20μm).
Solids content: 75.3 %
Results
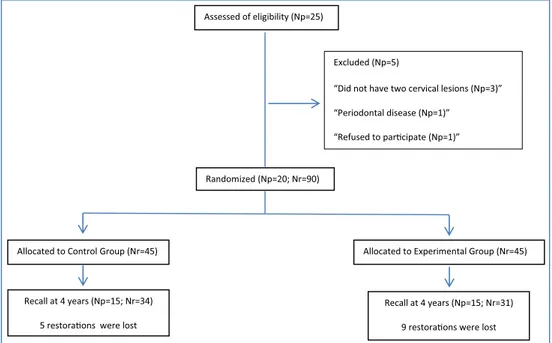
Five out of the 25 participants initially screened were excluded from the study because they did not fulfill the inclusion criteria. Thus, a total of 20 subjects with a mean age of 45 years were enrolled. Ninety restorations were placed, 45 for each group. All information regarding the number of research sub-jects who attended and the amount of restorations evaluated after 4 years are presented in Fig.1.
Table3 summarizes the clinical performance findings as frequency of Alfa, Bravo, and Charlie scores in two periods: baseline and 4-year recall. At the recall, five restorations from
the control group and nine from the experimental group were lost. Therefore, in regards to the retention rate, the control group was 85.3 % (%A + B) and 70.9 % (%A + B) for the experimental group. There was no statistically significant dif-ference between the groups (p= 0.2288). For all other evalu-ated criteria, the rate (%A + B) was 100 % in both groups. There was no statistically significant difference in each crite-rion (p= 1.000).
Regarding retention rate, the intragroup comparisons dem-onstrated no statistically significant difference between the baseline and 4-year recall in the control group (p = 0.06), while there was a statistically significant difference in the
Table 2 Modified USPHS direct evaluation system
Category Criteria
Retention A = Retained
C = Mobile or missing Marginal integrity A = Undetectable
B = Visible evidence of a crevice along the margin, dentin not exposed
C = Explorer penetrates into crevice, dentin is exposed Marginal discoloration A = No discoloration at margins
B = Shallow discoloration C = Deep discoloration Postoperative sensitivity A = Absent; clinically acceptable
C = Present; clinically unacceptable
Caries A = Absent
C = Present
Anatomic form A = Restoration is continuous
B = Discontinuous, but dentin is not exposed C = Material is missing, dentin is exposed
A= Alfa andB= Bravo (clinically acceptable);C= Charlie (clinically unacceptable)
Assessed of eligibility (Np=25)
Excluded (Np=5)
“Did not have two cervical lesions (Np=3)”
“Periodontal disease (Np=1)”
“Refused to parƟcipate (Np=1)”
Randomized (Np=20; Nr=90)
Allocated to Control Group (Nr=45) Allocated to Experimental Group (Nr=45)
Recall at 4 years (Np=15; Nr=34)
5 restoraƟons were lost
Recall at 4 years (Np=15; Nr=31)
9 restoraƟons were lost Fig. 1 Flow diagram.Npnumber
experimental group (p= 0.003). For all other evaluated criteria in both groups, no statistically significant difference was found (p= 1.000).
Discussion
Desensitizing agents, particularly oxalates, have been used as dentin pretreatment in cases of dentin hypersensitivity [13,16,
26,27]. Although there are clinical studies using BisBlock as a desensitizing agent [16,26,27], there are few clinical trials [13,27, 28] of this substances under restorations in non-carious cervical lesions with a long-term evaluation, making this study relevant to complement and confront some laboratorial and clinical findings.
This study investigated the clinical performance of a two-step etch-and-rinse adhesive with and without oxalic acid pre-treatment in non-carious cervical lesions. The observed results showed that both techniques presented similar clinical perfor-mance after 4 years of service. This leads the authors failed to reject the null hypothesis.
The influence of the oxalic acid on etched dentin before use of an adhesive system is unclear, and there is no consensus in the literature. Shafiei & Memarpour [29] in an in vitro study concluded that the oxalate desensitizer adversely influenced the sealing ability. They attributed this effect to a possible
intervention of calcium oxalate crystals on the dentinal and enamel surfaces and tubule orifices with the bonding procedure, thereby inhibiting the formation of a sufficient hybrid layer.
According to Al Qahtani [30], the formation of calcium oxalate crystals into the dentin occurs after the application of oxalate-based solutions. The coverage of the dentin surface with an acid-resistant layer of oxalate crystals may interfere with the formation of a sufficient hybrid layer, decreasing the bond strength to dentin [30]. In addition, they also believe that although the oxalate solution has been thoroughly rinsed be-fore the adhesives’application, residual oxalic acid may have remained and reacted with calcium, causing crystal precipita-tion on the dentin surface, which, in turn, could disturb poly-merization of the adhesives and, ultimately, compromise their bonding performance [30,31].
The study of Aranha et al. [32] reported gap formation between oxalate-treated dentin and the restoration in SEM analysis. In 2012, Yousry [33] also observed the morphology of the Boxalate-hybrid complex layer^ in the SEM image, showing adhesive failure within the resin-dentin interface jeopardizing the bonding process.
Silva et al. [21] also evaluated whether the effect of the combined application of oxalate with etch-and-rinse adhesives interferes with the durability of resin-dentin bonds when using two- and three-step etch-and-rinse adhesives. They used the microtensile method in the laboratory and showed that,
Table 3 Evaluation of the materials at baseline and after 4 years
Category Material Baseline 4 years
Scores Scores
A B C % A + B A B C % A + B McNemar’s Test Retention Control 45 0 0 100 % 29 0 5 83.5 % p= 0.0625
Bisblock 45 0 0 100 % 22 0 9 70.9 % p= 0.0039 Fisher;p= 1.000 Fisher;p= 0.2288
Marginal integrity Control 40 5 0 100 % 14 15 0 100 % p= 1.000 Bisblock 39 6 0 100 % 7 15 0 100 % p= 1.000
Fisher;p= 1.000 Fisher;p= 1.000
Marginal discoloration Control 45 0 0 100 % 26 3 0 100 % p= 1.000 Bisblock 45 0 0 100 % 18 4 0 100 % p= 1.000
Fisher;p= 1.000 Fisher;p= 1.000
Postoperative sensitivy Control 45 0 0 100 % 29 0 0 100 % p= 1.000 Bisblock 45 0 0 100 % 22 0 0 100 % p= 1.000
Fisher;p= 1.000 Fisher;p= 1.000
Caries Control 45 0 0 100 % 29 0 0 100 % p= 1.000 Bisblock 45 0 0 100 % 22 0 0 100 % p= 1.000
Fisher;p= 1.000 Fisher;p= 1.000
Anatomic form Control 44 1 0 100 % 26 3 0 100 % p= 1.000 Bisblock 38 7 0 100 % 20 2 0 100 % p= 1.000
despite oxalate desensitizer being shown to contribute to the reduction of resin-dentin bond degradation over time, it com-promised the baseline bond strength to the teeth that received potassium oxalate after acid etching. After 2 years, they also showed that the potassium oxalate may adversely affect the baseline hardness of etch-and-rinse adhesives [34]. Therefore, in accordance with these previous studies [21,29–34], it can speculate that crystal precipitation on the etched dentin surface impaired the adequate hybrid layer formation.
On the other hand, the results of the present clinical trial are in agreement with in vitro studies conducted by Pashley et al. [23] and Tay et al. [22] where demonstrated that po-tassium oxalate does not interfere with the bond strength. SEM images showed that the application of potassium oxa-late gel on etched dentin resulted in the formation of crystals inside the tubules rather than on the surface. An examination of the bonded interfaces demonstrated that the crystal for-mation inside the tubules did not compromise the forfor-mation of a typical hybrid layer on the top of dentin surfaces. Resin monomers penetrated into the tubules filling the spaces around the crystals forming resin tags with a jagged-like feature [23]. Two-step etch-and-rinse adhesives are consid-ered full-permeable membranes that allow flow of liquids that comes both the external environment as dentinal tu-bules. This permeability is primarily responsible for the hy-drolytic degradation of hybrid layer [35]. The association of adhesive restorations and oxalate-based agents could mini-mize contact of adhesives with the dentinal fluid, thereby reducing hydrolytic degradation and improving the clinical success rate of restorations [23]. The application of potassi-um oxalate salts on dentin surface after acid etching shows similar immediate bond strength to dentin when compared to a no pretreatment with desensitizing agents, not interfering in the process of bond strength [22].
Silva et al. [21] also concluded that potassium oxalate played an important role in decelerating the long-term degra-dation of the resin-dentin bonds. They argue that the presence of calcium oxalate crystals partially blocking the fluid transu-dation improves the resin-dentin bond strength due to the de-creased dilution of the adhesive by dentin fluids, mainly in deep dentin. This result corroborates with the clinical findings of Sartori et al. [13], where they concluded that potassium oxalate did not interfere in the clinical performance of com-posite resin restorations in non-carious cervical lesions during the 18-month clinical trial and De Souza et al. [36] where the use of oxalic acid as an agent of dentin pretreatment did not influence the clinical performance of restorations in non-carious cervical lesions after 1 year.
Analyzing marginal integrity, marginal discoloration, post-operative sensitivity, caries, and anatomic form, the authors had 100 % of success at the 4-year recall, in agreement with other clinical trials [37–40]. There were no statistically signif-icant differences between treatments, and both were
significantly important in reducing dentin hypersensitivity. However, the retention rate of the oxalic acid group was in-fluenced over time. Therefore, the use of oxalic acid as a pretreatment agent in the etch-and-rinse technique must be considered as an additional step that may impair the longevity of adhesive restorations in non-carious cervical lesions.
Conclusions
Within the limits of the current study, it may be concluded that, despite oxalate being shown to contribute to the reduc-tion of dentin hypersensitive, dentin pretreatment with oxalic acid meant an additional step in the etch-and-rinse adhesive technique.
Conflict of interest The authors declare that they have no conflict of interest.
References
1. Scherman A, Jacobsen PL (2002) Managing dentin hypersensitiv-ity: what treatment to recommend to patients. J Am Dent Assoc 123:57–61
2. Coleman TA, Grippo JO, Kinderknecht KE (2000) Cervical dentin hypersensitivity. Part 2: associations with abfractive lesions. Quintessence Int 31:466–473
3. Wood I, Jawad Z, Paisley C, Brunton P (2008) Noncarious cervical tooth surface loss: a literature review. J Dent 36:759–766 4. Veitz-Keenan A, Barna JA, Strober B, et al (2013) Treatments for
hypersensitive noncarious cervical lesions: a practitioners engaged in applied research and learning (PEARL) network randomized clinical effectiveness study. J Am Dent Assoc 144:495–506 5. Camilotti V, Zilly J, Busato PMR, et al (2012) Desensitizing
treat-ments for dentin hypersensitivity: a randomized, split-mouth clini-cal trial. Braz Oral Res 26:263–268
6. Brännström M, Linden LA, Aström A (1967) The hydrodynamics of the dental tubule and pulp fluid: a discussion of its significance in relation to dentinal sensitivity. Caries Res 1:310–317
7. West NX, Sanz M, Lussi A, et al (2013) Prevalence of dentine hypersensitivity and study of associated factors: a European popu-lation based cross-sectional study. J Dent 41:841–851
8. Gernhardt CR (2013) How valid and applicable are current diag-nostic criteria and assessment methods for dentin hypersensitivity? An overview. Clin Oral Investig. 2013 17:31-40.
9. Assis JA, Rodrigues LKA, Fonteles CSR, et al (2011) Dentin hy-persensitivity after treatment with desensitizing agents: a random-ized, double-blind, split-mouth clinical trial. Braz Dent J 22:157–
161
10. Gillam DG, Newman HN, Davies EH, et al (2004) Clinical evalu-ation of ferric oxalate in relieving dentine hypersensitivity. J Oral Rehabil 31:245–250
11. Barrientos C, Xaus G, Leighton C, et al (2011) Oxalic acid under adhesive restorations as a mean to reduce dentin sensitivity: a four-month clinical trial. Oper Dent 36:126–132
13. Sartori N, Lopes GC, Vieira LC (2012) Clinical performance of cervical restorations with desensitizing agents: 18-month clinical trial. J Adhes Dent 14:183–189
14. Ding YJ, Yao H, Wang GH, et al (2014) A randomized double-blind placebo-controlled study of the efficacy of Clinpro XT var-nish and Gluma dentin desensitizer on dentin hypersensitivity. Am J Dent 27:79–83
15. West NX, Seong J, Davies M (2015) Management of dentine hy-persensitivity: efficacy of professionally and self-administered agents. J Clin Periodontol 42(Suppl. 16):S256–S302. doi:10.1111/ jcpe.12336
16. Vora J, Mehta D, Meena N, et al (2012) Effects of two topical desensitizing agents and placebo on dentin hypersensitivity. Am J Dent 25:293–298
17. Mehta D, Gowda VS, Santosh A, et al (2014) Randomized con-trolled clinical trial on the efficacy of dentin desensitizing agents. Acta Odontol Scand 9:1–6
18. Pereira JC, Segala AD, Gillam DG (2005) Effect of desensitizing agents on the hydraulic conductance of human dentin subjected to different surface pre-treatments—an in vitro study. Dent Mater 21: 129–138
19. Vieira AHM, Passos VF, Assis JS, et al (2009) Clinical evaluation of a 3 % potassium oxalate gel and a GaAIAs laser for the treatment of dentinal hypersensitivity. Photomed Laser Surg 27:807–812 20. Cunha-Cruz J, Wataha J, Zhou L, et al (2010) Dentin
hypersensi-tivity: choice of treatments by dentists of the northwest PREC EDENT network. J Am Dent Assoc 141:1097–1105
21. Silva SMA, Malcarne-Zanon J, Carvalho RM, et al (2010) Effect of oxalate desensitizer on the durability of resin-bonded interfaces. Oper Dent 35:610–617
22. Tay FR, Pashley DH, Mak YF, et al (2003) Integrating oxalate desensitizers with total-etch two-step adhesive. J Dent Res 82: 703–707
23. Pashley DH, Carvalho MR, Pereira JC, et al (2001) The use of oxalate to reduce permeability under adhesive restorations. Am J Dent 14:89–94
24. de Andrade e Silva SM, Marquezini Jr L, Manso AP, et al (2007) Effects of a combined application of potassium oxalate gel/adhesive agent on dentin permeability in vitro. J Adhes Dent 9:505–512 25. Schulz KF, Altman DG, Moher D, CONSORT Group (2011)
CONSORT 2010 statement: updated guidelines for reporting par-allel group randomised trials. Int J Surg 9:672–677
26. Ryge G (1980) Clinical criteria. Int Dent J 30:347–358
27. Pamir T, Dalgar H, Onal B (2007) Clinical evaluation of three desensitizing agents in relieving dentin hypersensitivity. Oper Dent 32:544–548
28. Erdemir U, Yildiz E, Kilic I, et al (2010) The efficacy of three desensitizing agents used to treat dentin hypersensitivity. J Am Dent Assoc 141:285–296
29. Shafiei F, Memarpour M (2013) Effect of surface pretreatment with two desensitizer techniques on the microleakage of resin composite restorations. Lasers Med Sci 28:247–251
30. Al Qahtani MQ, Platt JA, Moore BK, et al (2003) The effect on shear bond strength of rewetting dry dentin with two desensitizers. Oper Dent 28:287–296
31. Shafiei F, Motamedi M, Alavi AA, et al (2010) The effect of oxalate desensitizers on the microleakage of resin composite restorations bonded by etch and rinse adhesive systems. Oper Dent 35:682–688 32. Aranha AC, Junior A de S S, Cavalcante LM, et al (2006) Microtensile bond strengths of composite to dentin treated with desensitizer products. J Adhes Dent 8:85–90
33. Yousry MM (2012) Effect of re-etching oxalate-occluded dentin and enamel on bonding effectiveness of etch-and-rinse adhesives. J Adhes Dent 14:31–38
34. Silva SMA, Malacarne-Zanon J, Carvalho RM, et al (2012) Effects of potassium oxalate on Knoop hardness of etch-and-rinse adhe-sives. Oper Dent 37:356–362
35. De Munck J, Van Landuyt K, Peumans M, et al (2005) A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res 84:118–132
36. De Souza AM, Colares RC, Mendonça JS, et al (2014) Effect of oxalic acid pre-treatment in restorations of non-carious cervical lesions: a randomized clinical trial. J Conserv Dent 17:427–431 37. Santiago SL, Franco EB, Mendonca JS, et al (2003) One-year
clin-ical evaluation of tooth-colored materials in Non-carious cervclin-ical lesions. J Appl Oral Sci 11:175–180
38. Reis A, Loguercio AD (2009) A 36-month clinical evaluation of ethanol/water and acetone-based etch-and-rinse adhesives in non-carious cervical lesions. Oper Dent 34:384–391
39. Reis A, Loguercio AD (2006) A 24-month follow-up of flowable resin composite as an intermediate layer in Non-carious cervical lesions. Oper Dent 31:523–529