Reconstruction of pelviperineal injuries with
perforator laps: clinical experience with 22 cases
Reconstruções pelveperineais com uso de retalhos cutâneos baseados em
vasos perfurantes: experiência clínica com 22 casos
ABSTRACT
Introduction: Plastic surgery consultation is commonly sought for the treatment of pel viperineal injuries in general hospitals. The objective of this study was to present the
experience acquired in the treatment of perineal, sacral, and hip injuries with the use of perforator laps. Methods: Patients referred to the Plastic Surgery Division of the Clinical Hospital of Medicine College of Universidade de São Paulo for evaluation of pelviperi
neal and hip wounds from February to May 2009 were retrospectively evaluated. A total of 22 patients underwent reconstruction with skin and fasciocutaneous laps based on the perforator vessels, according to the inclusion criteria. The average follow-up period was
6 months. Results: Pelviperineal injuries consisted of pressure ulcers in 20 cases (91%),
deep infection in 1 case (45%), and perineal hidradenitis in 1 case (4.5%). The choice of lap for reconstruction was dependent on the local wound: 15 cases (68.2%) of sacral ul
cers were repaired with a superior gluteal artery perforator lap; 3 cases (13.6%) of ischial ulcers were repaired with an inferior gluteal artery perforator lap; and 2 cases (9.1%) of
trochanteric ulcers were repaired using a tensor fascia lata perforator lap. A fasciocutaneous
gluteofemoral lap was selected for reconstruction of post Fournier’ syndrome in 1 patient and was used after resection of perineal hidradenitis in 1 patient. A new suture for late primary closure was necessary in 3 (13.6%) cases in which the suture line dehiscence was < 10% of the injury perimeter during the irst 15 post-operative days. There were no cases of > 3% necrosis of the lap surface. These results were maintained during the follow-up
evaluation period. Conclusions: The results of the study were satisfactory, and the utility
of surgical laps without the incorporation of muscle for pelviperineal reconstruction was
demonstrated. This treatment alternative decreases donor site morbidity and preserves the muscular tissue for future interventions.
Keywords: Perineum. Wounds and injuries. Pressure ulcer. Surgical laps. Plastic surgery.
RESUMO
Introdução: As lesões pelveperineais representam grande parcela das interconsultas para o
cirurgião plástico em hospitais gerais. O objetivo do presente trabalho é apresentar a expe
riência obtida no tratamento de pacientes com lesões perineais, sacrais e de quadril com o
uso de retalhos com vasos perfurantes. Método: Foram estudados, retrospectivamente, os
pacientes submetidos a avaliação pela equipe da Divisão de Cirurgia Plástica do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, nos meses de fevereiro a
Study conducted at the Plastic Surgery Division of the Clinical Hospital of the College of Medicine of
Universidade de São Paulo, São Paulo, SP, Brazil. Paper submitted to SGP (Sistema
de Gestão de Publicações/ Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery). Study presented at the Brazilian
Congress of Plastic Surgery held
in São Paulo, SP, Brazil, 2009. Paper received: July 23, 2011 Paper accepted: October 28, 2011
1. Plastic surgeon, physician preceptor at the Plastic Surgery Division of the Clinical Hospital of the College of Medicine of the Universidade de São Paulo (HCFMUSP), São Paulo, SP, Brazil.
2. Resident physician of Plastic Surgery of HCFMUSP, São Paulo, SP, Brazil.
3. Master in Plastic Surgery, assistant physician of the Plastic Surgery Division of HCFMUSP, São Paulo, SP, Brazil.
4. Plastic surgeon, assistant physician of the Instituto do Câncer do Estado de São Paulo (Institute of Cancer of São Paulo State), São Paulo, SP, Brazil. 5. PhD in Plastic Surgery, assistant physician of the Plastic Surgery Division of HCFMUSP, São Paulo, SP, Brazil.
6. Titular professor of Plastic Surgery Discipline at Medicine College of Universidade de São Paulo, chief of Plastic Surgery Division of HCFMUSP, São Paulo, SP, Brazil.
Guilherme Cardinali Barreiro1
linColn Saito millan2
huGo nakamoto3
eduardo montaG4
Paulo tuma Jr.5
maio de 2009, que apresentavam feridas em região pelveperineal e no quadril. No total, 22 pacientes foram submetidos a reconstrução com retalhos cutâneos e fasciocutâneos baseados em vasos perfurantes, de acordo com os critérios de inclusão. O período de seguimento médio
foi de 6 meses. Resultados: A lesão pelveperineal foi úlcera por pressão em 20 (91%) casos,
infecção profunda em 1 (4,5%), e hidradenite perineal em 1 (4,5%). A opção dos retalhos foi previamente estabelecida, dependendo do local da ferida: úlceras sacrais, retalho baseado nas perfurantes da artéria glútea superior em 15 (68,2%) casos; úlceras isquiáticas, retalho baseado nos vasos perfurantes da artéria glútea inferior em 3 (13,6%) casos; e úlceras tro
cantéricas, retalho tensor da fascia lata perfurante em 2 (9,1%) casos. Retalho fasciocutâneo inervado gluteofemoral foi a opção para a reconstrução póssíndrome de Fournier em um paciente e após ressecção de hidradenite perineal em outro. Houve necessidade de nova sutura
para fechamento primário tardio em deiscência < 10% do perímetro da lesão em 3 (13,6%) casos, durante os primeiros 15 dias de pós-operatório. Não houve casos de necrose > 3%
da superfície do retalho. Os resultados foram mantidos no período de seguimento avaliado. Conclusões: Os resultados obtidos no presente estudo foram satisfatórios e icou demons
trada a utilidade de retalhos cirúrgicos sem incorporação de músculo para reconstruções pelveperineais. Essa alternativa para tratamento é menos mórbida para as áreas doadoras e
preserva o tecido muscular para possível intervenção futura.
Descritores: Períneo. Ferimentos e lesões. Úlcera de pressão. Retalhos cirúrgicos. Cirurgia plástica.
INTRODUCTION
Plastic surgery consultation is commonly sought for the treatment of pelviperineal and hip injuries in general hospi tals. The majority of these wounds are caused by pressure
ulcers, although other etiologies are common, including peri
neal hidradenitis, deep infections, trauma, burns sequelae, neo plasias, and surgical trauma. The treatment usually con -sists of local care, surgical debridement, proper dressing, frequent position changes, and nutritional support1.
Certain patients with pelviperineal and hip wounds re
quire reconstructive plastic surgery2. Primary closure, der
-moepidermal grafts, and fasciocutaneous or musculocuta
neous laps are the best options for reconstruction with the objective of illing, covering, and protecting the laps3. The
use of myocutaneous laps is very common, as described by
Costa et al.4, who reported on a series of cases of pelviperineal
reconstruction of pressure ulcers using myocutaneous laps. In the Plastic Surgery Division of the Clinical Hospital
of the College of Medicine of Universidade de São Paulo
(HCFMUSP), the use of perforator laps is common prac
tice. In 2004, Munhoz5 used a transverse abdominal skin
lap based on the supericial epigastric artery perforator for breast reconstructions. Improved topographic localization of
dominant perforator vessels in the pelvis and hip enabled the establishment of a protocol for pelviperineal reconstruction
using cutaneous perforator laps.
The objective of this study was to describe our experience with the use of perforator laps for the treatment of perineal, sacral, and hip injuries.
METHODS
A total of 22 patients with perineal, sacral, and hip inju ries were evaluated and followed up at the Plastic Surgery
Di vision of HCFMUSP from February to May 2009. The
Wound Group was formed by interconsultation with inpa tients in other clinics of HCFMUSP.
Demographic data was collected, and an epidemiological inventory of each patient was created, including age, gender,
and cause of injury. The indication criteria for surgical interven tion were favorable clinical conditions, proper nutritional state,
possibility of home care, prognosis, and underlying disease. During the period included in the study, 22 patients un -derwent pelviperineal and hip reconstruction with local laps, including 13 (59.1%) men and 9 (40.9%) women. The patients ranged in age from 17 to 46 years, and the average age was 32.6 years. The cause of perineal injury was pressure ulcers in 20 cases (91%; level III or IV ulcers in paraplegic or quadri
plegic patients), deep infection in 1 (4.5%) case, and perineal hidradenitis in 1 case (4.5%).
The general procedure consisted of surgical debridement
and installation of a vacuum therapy device for 1 to 2 weeks. The reconstruction was carried out with local laps, especially those based on perforator vessels. The laps were planned and
the isolation and dissection of the perforators were based on the anatomic repairs described6. In sacral ulcers (15 cases, 62.2%), a superior gluteal artery perforator lap was used7;
ischial ulcers (3 cases, 13.6%) were repaired using an inferior gluteal artery perforator lap8 with V-Y advancement laps;
skin lap based on the transverse branch of the lateral femoral
circumlex artery9. The gluteofemoral fasciocutaneous lap10 based on the descending branch of the inferior gluteal artery was the choice for reconstruction in a patient with a perineal
injury associated with Fournier syndrome and in 1 patient after resection of perineal hidradenitis (Table 1).
The post-operative follow-up period ranged from 4 to 9 months, with an average follow-up period of 6 months. The patients were evaluated after discharge in weekly outpatient consultations during the irst month and subsequently every
two months. The operated areas were evaluated and eventual
necrosis, relapses, dehiscence, or infections were recorded. Other areas were also examined to detect possible new pres sure ulcers.
RESULTS
All complications were considered to be minor. Total loss of the lap due to necrosis was not observed. A new suture for late primary closure was necessary in 3 (13.6%) cases in which the suture line dehiscence was <10% of the injury perimeter during the irst 15 post-operative days. In these 3 cases, < 3% of the total lap surface showed necrosis, and the
treatment involved debridement and direct suture without the development of new dehiscence.
All wounds showed complete closure. The laps remai ned viable in all patients, without signs of relapse at the 2-month
outpatient consultation. Patients were provided with instruc tions on recumbent positioning and appropriate maneuvers
for position changes. Out of 15 patients with sacral ulcers, 3 (20%) presented level II11 ischial ulcers during the followup
period, and the ulcers were treated conservatively.
Figures 1 to 3 illustrate some of the cases described in the
present study.
DISCUSSION
Pelviperineal injuries represent a great challenge for the
plastic surgeon. New pressure ulcers are common in general
hospitals and are mostly caused by poor compliance with
guidelines for position changes, mainly affecting intensive
care patients. Flap reconstruction is often postponed until favorable clinical and local conditions are achieved. The initial treatment includes dressing changes and surgical
debridement of the devitalized tissues in addition to orien
tation regarding posture, which is the responsibility of the
nursing team in charge.
Surgical reconstruction is indicated in patients who were discharged from intensive therapy and have shown functional
recovery, as well as in spinal cord trauma or stroke patients. The treatment of paralyzed patients involves the education of
both, the patient and third parties in charge of patient care. In these patients, it is important to control neurogenic bladder
spasticity and ensure regular position changes12.
To accelerate the preparation of the wound bed, our insti
tution routinely uses the negative pressure (vacuum) method,
which has been found to improve the results of surgery and prevent the need for multiple surgical interventions. During
the reconstruction itself, the plastic surgeon should explore all the options for laps whose dissection is based on anatomic repairs.
Musculocutaneous gluteus maximus laps are commonly
used for the repair of sacral and ischial pressure ulcers13.
Hamstring muscle laps have also been successfully applied
for the treatment of ischial pressure ulcers14. Tensor fasciae
latae muscle laps are the treatment of choice for the repair
of trochanteric pressure ulcers15. All these alternatives use
Table 1 – Location of the injuries and laps used for reconstruction.
Lesion site Flap used for reconstruction
Number of cases
Sacral pressure ulcer RFCBPAGS 15
Ischial pressure ulcer RFCBPAGI 3
Trochanteric pressure ulcer RCBPRTACFL 2
Perineal injury RFCIGF 2
RCBPRTACFL = skin lap based on the perforator of the transverse branch of the lateral femoral circumlex artery; RFCBPAGI = fasciocutaneous lap based on the inferior gluteal artery perforator; RFCBPAGS = fasciocutaneous lap based on the superior gluteal artery perforator; RFCIGF = gluteofemoral fasciocutaneous lap.
A
C D
B
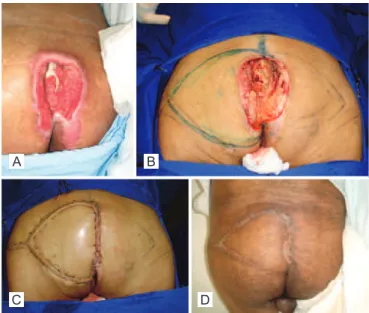
Figure 1 – Patient with sacral pressure ulcer. In A, pre-operative aspect. In B, pressure ulcer after debridement and marking of
the fasciocutaneous lap based on the superior gluteal artery
A B C
D E
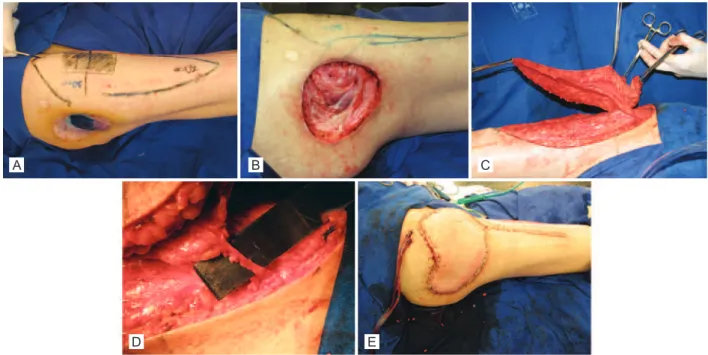
Figure 2 – Patient with trochanteric pressure ulcer. In A, pre-operative aspect. In B, pressure ulcer after debridement of the devitalized tissue. In C, skin lap based on the perforator of the transverse branch of the lateral femoral circumlex artery
(tensor fascia lata perforator lap). In D, characteristics of the preserved perforator laps. In E, immediate post-operative aspect.
A B
C D
Figure 3 – Patient with perineal wound resulting from Fournier’s
syndrome. In A, pre-operative aspect. In B, appearance after
debridement and marking of the lap. In C, dissected gluteofemoral
fasciocutaneous lap. In D, immediate post-operative aspect.
the muscle as a vector for skin lap perfusion, compromising
the donor site for future interventions. To diminish this type
of morbidity, our institution began to use perforator laps for
cutaneous repairs, and these laps do not require the inclusion of an underlying muscle.
Perforator laps, which are based on the angiosome con
-cept16, usually require more advanced knowledge of anatomy and surgical ability. Koshima et al.17 and Ao et al.18 were
the pioneers in the use of perforator laps based on gluteal, lumbar, and intercostal arteries for the repair of lumbosacral
defects in the early 90’s. In the present study, the laps were
designed to receive their blood supply through the recons
titution of well known vascular pedicles. Careful dissection keeping the perforator vessel anatomy in mind enabled the
isolation of the perforators and the elevation of the fasciocu
taneous laps, including enough tissue to cover the injuries
and allow primary closure of the donor areas.
The advantages of this type of lap are countless: it pre -serves the muscle, allows the inclusion of multiple compo
nents in the lap, and reduces pain and functional deicits at
the donor site7,18. In comparison, musculocutaneous laps
are thick and well vascularized. Nevertheless, the muscular tissue is more sensitive to ischemia, and the removal of
muscles from the donor area has greater functional morbi dity19. The potential disadvantage of fasciocutaneous laps
based on perforator vessels is their reduced thickness, which limits their use to the reconstruction of wounds requiring greater illing7. In the patients included in this study, there was no need for volume addition besides that provided by
Approximately 80% of patients with paralysis are prone
to recurrence of pressure ulcers or the development of new
ones, depending on the source and follow-up period19. Even
in these patients, in which the donor site functionality is not a priority, the use of perforator laps preserves the underlying tissues, such as the muscle itself, which can be used as an alternative source in cases of relapse. Among the patients included in this study, there were no cases of relapse within a 6-month follow-up period, although 3 patients presented
with new ulcers at other sites. These patients were paraplegic and had sacral pressure ulcers that were diagnosed and trea
ted during their hospitalization for spinal cord trauma. Upon discharge, these patients used a wheelchair for mobility and developed level II11 ischial ulcers that were treated with re gular dressings.
In the present study, no complications related to the viabi
lity of the laps that could compromise the closure of lesions were observed, with the exception of 3 cases of partial dehis
cence that were treated with debridement and direct suture. In patients with paralysis that present with pressure ulcers, the
tendency towards recurrence or development of new wounds is common19,20, which emphasizes the importance of using
laps that enable the reuse of the donor site and local tissues.
CONCLUSIONS
The results obtained in this study were satisfactory, and the beneits of using surgical laps that do not require the
inclusion of an underlying muscle for pelviperineal recons truction were demonstrated. This treatment alternative is asso ciated with lower donor site morbidity and preserves the muscular tissue for future interventions.
REFERENCES
1. Conway H, Grifith BH. Plastic surgery for closure of decubitus ulcers in patients with paraplegia, based on experience with 1,000 cases. Am J Surg. 1956;91(6):946-75.
2. Sørensen JL, Jørgensen B, Gottrup F. Surgical treatment of pressure ulcers. Am J Surg. 2004;188(1A Suppl):42-51.
3. Rosen JM, Mo ST, Liu A. Experience with the island inferior gluteal
thigh lap compared with other local laps for the reconstruction of the pelvic area. Ann Plast Surg. 1990;24(6):498-509.
4. Costa MP, Sturtz G, Costa FPP, Ferreira MC, Barros Filho TEP Epide
miologia e tratamento das úlceras de pressão: experiência de 77 casos. Acta Ortop Bras. 2005;13(3):124-33.
5. Munhoz AM. Estudo crítico da anatomia arterial do retalho vascula
rizado pela artéria perfurante muscular da artéria epigástrica inferior [dissertação de mestrado]. São Paulo: Faculdade de Medicina da Uni
versidade de São Paulo; 2004.
6. Hallock GG. A primer of schematics to facilitate the design of the prefer
red muscle perforator laps. Plast Reconstr Surg. 2009;123(3):1107-15. 7. Coşkunirat OK, Ozgentaş HE. Gluteal perforator laps for coverage of
pressure sores at various locations. Plast Reconstr Surg. 2004;113(7): 2012-7.
8. Higgins JP, Orlando GS, Blondeel PN. Ischial pressure sore reconstruc
tion using an inferior gluteal artery perforator (IGAP) lap. Br J Plast Surg. 2002;55(1):83-5.
9. Ishida LH, Munhoz AM, Montag E, Alves HR, Saito FL, Nakamoto HA, et al. Tensor fasciae latae perforator lap: minimizing donor-site
morbidity in the treatment of trochanteric pressure sores. Plast Reconstr
Surg. 2005;116(5):1346-52.
10. Hurwitz DJ, Swartz WM, Mathes SJ. The gluteal thigh lap: a reliable, sensate lap for the closure of buttock and perineal wounds. Plast Re
constr Surg. 1981;68(4):521-32.
11. Shea JD. Pressure sores: classiication and management. Clin Orthop Relat Res. 1975;(112):89-100.
12. Bauer JD, Mancoll JS, Phillips LG. Pressure sores. In: Thorne CH, ed. Grabb & Smith’s plastic surgery. 6a ed. New York: Lippincott Williams & Wilkins; 2007. p. 722-9.
13. Baek SM, Williams GD, McElhinney AJ, Simon BE. The gluteus maxi
mus myocutaneous lap in the management of pressure sores. Ann Plast Surg. 1980;5(6):471-6.
14. James JH, Moir IH. The biceps femoris musculocutaneous lap in the
repair of pressure sores around the hip. Plast Reconstr Surg. 1980;
66(5):736-9.
15. Nahai F, Silverton JS, Hill HL, Vasconez LO. The tensor fascia lata musculocutaneous lap. Ann Plast Surg. 1978;1(4):372-9.
16. Taylor GI, Palmer JH. The vascular territories (angiosomes) of the body: experimental study and clinical applications. Br J Plast Surg. 1987;40(2):113-41.
17. Koshima I, Moriguchi T, Soeda S, Kawata S, Ohta S, Ikeda A. The gluteal
perforatorbased lap for repair of sacral pressure sores. Plast Reconstr
Surg. 1993;91(4):678-83.
18. Ao M, Mae O, Namba Y, Asagoe K. Perforator-based lap for coverage of lumbosacral defects. Plast Reconstr Surg. 1998;101(4):987-91. 19. Bauer J, Phillips LG. MOC-PSSM CME article: Pressure sores. Plast
Reconstr Surg. 2008;121(1 Suppl):1-10.
20. Seyhan T, Ertas NM, Bahar T, Borman H. Simpliied and versatile use of gluteal perforator laps for pressure sores. Ann Plast Surg. 2008; 60(6):673-8.
Correspondence to: Guilherme Cardinali Barreiro