w w w . r b o . o r g . b r
Original
Article
Functional
results
from
reconstruction
of
the
anterior
cruciate
ligament
using
the
central
third
of
the
patellar
ligament
and
flexor
tendons
夽
Marcos
George
de
Souza
Leao
∗,
Abelardo
Gautama
Moreira
Pampolha,
Nilton
Orlando
Junior
Fundac¸ãoHospitalAdrianoJorge,Manaus,AM,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received11September2014 Accepted23October2014 Availableonline17October2015
Keywords:
Anteriorcruciateligament Knee
Treatment
a
b
s
t
r
a
c
t
Objectives: Toevaluatekneefunctioninpatientsundergoingreconstructionoftheanterior
cruciateligament(ACL)usingthecentralthirdofthepatellarligamentorthemedialflexor tendonsoftheknee,i.e.quadrupleligamentsfromthesemitendinosusandgracilis(ST-G), bymeansoftheKneeSocietyScore(KSS)andtheLysholmscale.
Methods:Thiswasarandomizedprospectivelongitudinalstudyon40patientswho
under-wentarthroscopicACLreconstructionbetweenSeptember 2013andAugust2014. They comprised37malesandthreefemales,withagesrangingfrom16to52years.Thepatients werenumberedrandomlyfrom1to40:theevennumbersunderwentsurgicalcorrection usingtheST-Gtendonsandtheoddnumbers,usingthepatellartendon.Functional evalua-tionsweremadeusingtheKSSandLysholmscale,appliedintheeveningbeforethesurgical procedureandsixmonthsaftertheoperation.
Results:Fromthestatisticalanalysis,itcouldbeseenthatthepatients’functionalcapacity
wassignificantlygreateraftertheoperationthanbeforetheoperation.Therewasstrong evidencethatthetwoformsoftherapyhadsimilarresults(p=>0.05),inallthecomparisons.
Conclusions: TheresultsfromtheACLreconstructionsweresimilarwithregardtofunctional
recoveryofthekneeandimprovementofqualityoflife,independentofthetypeofgraft. Itwasnotpossibletoidentifythebestmethodofsurgicaltreatment.Thesurgeon’sclinical andtechnicalexperienceandthepatientarethefactorsthatdeterminethechoiceofgraft typeforuseinACLsurgery.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
夽
WorkperformedattheFundac¸ãoHospitalAdrianoJorge,Manaus,AM,Brazil.
∗ Correspondingauthor.
E-mail:mgsleao@uol.com.br(M.G.deSouzaLeao).
http://dx.doi.org/10.1016/j.rboe.2015.10.002
Resultados
funcionais
da
reconstruc¸ão
do
ligamento
cruzado
anterior
com
o
terc¸o
central
do
ligamento
patelar
e
os
tendões
flexores
Palavras-chave:
Ligamentocruzadoanterior Joelho
Tratamento
r
e
s
u
m
o
Objetivos: Avaliarafunc¸ãodosjoelhosempacientessubmetidosàreconstruc¸ãodo
liga-mentocruzadoanterior(LCA),comoterc¸ocentraldoligamentodapatela(TP)ouostendões flexoresmediaisdojoelho(semitendíneoegrácilquádruplos:ST-G)ipsilaterais,pormeio doKneeSocietyScore(KSS)edaescaladeLysholm.
Métodos: Estudolongitudinal,prospectivoerandomizado,com40pacientessubmetidosà
reconstruc¸ãodoLCAporviaartroscópica,desetembrode2013aagostode2014,dosquais 37eramdosexomasculinoetrêsdofeminino,comde16a52anos,enumeradosdeforma aleatóriade1a40.Osnúmerosparesforamsubmetidosàcorrec¸ãocirúrgicacomostendões doST-GeosnúmerosimparescomoTP.Foramaplicadosparaaavaliac¸ãofuncionaloKSS eaescaladeLysholmnanoiteanterioraoprocedimentocirúrgicoecomseismesesde pós-operatório.
Resultados: Emanáliseestatísticafoipossívelobservarquenopós-operatórioacapacidade
funcionaldospacientesfoisignificativamentemaiordoquenopré-operatório.Háfortes evidênciasdequeambasasterapêuticassejamsimilaresemseusresultados(p=>0,05),em todasascomparac¸ões.
Conclusões: Osresultadosdareconstruc¸ãodoLCA,independentementedotipodeenxerto,
sãosimilaresnarecuperac¸ãofuncionaldojoelhoenamelhoriadaqualidadedevida.Nãofoi possívelidentificarmelhormétododetratamentocirúrgico.Aexperiênciaclínica,atécnica docirurgiãoeopacientesãoquemditamaescolhadotipodeenxertoquedeveráserusado paraacirurgiadoLCA.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Todososdireitosreservados.
Introduction
Anteriorcruciateligament(ACL)injuriesarethecommonest ligamentinjuriesoftheknee.Consideringthattearsofthis ligamentmainlyaffectyoungindividualswhopracticesports, thetreatmentinstitutedneedstoprovidethesepatientswith theconditionsforthemtoreturntotheirsport.1
Withtheaimofachievingthisobjective,manytechniques havebeen developedforreconstructingthe ACL,especially over the last 30 years, using autografts, allografts or syn-thetic grafts, including through advances in arthroscopic techniques.2 Today, the two options most commonly used
forACL reconstructionusing autograftsinvolve use ofthe medialhamstring muscles, quadruple semitendinosusand gracilis(ST-G)and thecentralthirdofthe patellaligament (PT).3
Recently,manysystems havebeen developedfor evalu-ating the pre and postoperativeresults from patients who undergosurgicalproceduresontheknee.4Useofthesescales
servesasanevaluationparameterandthusmakesit possi-blemeasurementstobestandardizedandmadeuniformand reproducible,inrelationtotreatmentproposals.
The Knee Society Score (KSS) combines subjective and objectiveinformation;separatesthekneescore(pain,stability, rangeofmotion,etc.)frompatients’functionalscores(ability towalkandgoupanddownstairs);andassessesthe clini-calconditionwithregardtopainintensity,rangeofmotion, anteroposteriorandmediolateralstability,contractures dur-ingflexion,deformitiesandmisalignment.5
TheLysholmscaleisoneofthequestionnairesmostused forevaluatingkneesymptoms.Itiscomposedofeight ques-tions,withclosedalternativesfortheresponses,andthefinal resultisexpressedbothinwordsandinnumbers:“excellent”, from95to100points;“good”,from84to94points;“fair”,from 65to83points;and“poor”,whenthevaluesarelessthanor equalto64points.6
Thepresentstudyhadtheaimofevaluatingpatientswho underwentsurgicaltreatmentforarthroscopicreconstruction oftheACLusinganautograftfromtheST-GorPT.Toachieve thisobjective,theKSSandLysholmscalesneededtobeused, appliedduringtheimmediatepreoperativeperiodandafter sixmonthsoffollow-up, inordertoascertainwhetherone techniquemightsuperiortotheother(ST-GversusPT).
Materials
and
methods
Between September 2013 and August 2014, a randomized prospectivelongitudinalstudywasconductedamongpatients for whom surgical treatment for ACL injuries had been indicated, becauseofcomplaintsofinstabilityand positive physicalandcomplementaryexaminations.Theseoperations wereperformedusinganipsilateralautografteitherfromthe centralthirdofthepatellarligament(PT)orfromthemedial flexortendonsoftheknee,i.e.thesemitendinosusandgracilis (ST-G).
outpatientclinic,withaconfirmed diagnosis ofACLinjury alone, with anauthorization for hospitalization requested, andwithanoperationperformedonlybytheprincipal inves-tigator. The criteria considered for exclusions comprised situationsofcomplexkneeinjuries(involvingmultiple liga-ments,osteoarthritisandmeniscalinjuries),revisionsurgery, inflammatory pathological conditions, obesity (body mass index>30),withdrawalofthepatient,operationsperformed byothersurgeonsandrefusaltosignthefreeandinformed consentstatement. Patients were only counted withinthe methodologyandwithinthestatisticalanalysisontheresults iftheymetalloftheinclusioncriteria.
Forty authorizations for hospitalization were gathered from the appropriate sectorof our institution. From these documents,fortypatientswhohadbeenscheduledfor arthro-scopicACLreconstructionwerenumberedrandomly(from1to 40).Thosewithevennumbersunderwentsurgicalcorrection usingtheipsilateralST-G,fixedwithanEndobutton®CLinthe femurandatitaniuminterferencescrewinthetibia.Those withoddnumbersreceivedtheipsilateralPTbymeansofa singleincision,fixedwithtwotitaniuminterferencescrews, inthefemurandinthetibia.Allthesurgicalprocedureswere performedunderspinalanesthesia,withatourniquetatthe rootof the thigh of the limbto be operated, with a pres-sureof350mmHg.Thegraftswereharvestedaccordingtothe patient’sgroup.Arthroscopywasperformedandthefemoral tunnelwasconstructedstartingfromtheanteromedialportal atthecenterofthescarofthenativeACL.Thetibialtunnelwas createdusingaspecificguide,withtheexitatthecenterofthe nativeACL.Thepostoperativerehabilitationprotocolwasthe sameforallthepatients.Itwasimplementedatthe institu-tion’sownphysiotherapyservice,wherethephysiotherapists wereunawareoftheresearchprojectthatwasinprogress.
Thegroupofpatientswithevennumberswascomposedof onefemalepatient(5%)and19malepatients(95%).Theages ofthesepatientsrangedfrom16to52years,withameanof 32(standarddeviation±8years),andninepatients(45%)were intheagegroupfrom30to39years.Theleftandrightsides wereaffectedatthesamerate(50%).
Thegroupofpatientswithoddnumberswascomposedof twofemalepatients(10%)and18malepatients(90%).Theages ofthesepatientsrangedfrom18to48years,withameanof 32±9,andninepatientswereintheagegroupfrom30to39 years.Therightsidewasoperatedin11patients(55%)andthe leftinnine(45%).
The Knee Society Score and the Lysholm scale, which havebeenvalidatedforthePortugueselanguage,wereused to evaluatethe functional results. The first ofthese com-binessubjectiveandobjectiveinformationandthesecondof thesepresentseightquestionswithclosedalternativesasthe responses,andtheywere appliedintheeveningbeforethe surgicalprocedureandsixmonthsaftertheoperation,with anactivesearchforpatientsiftheydidnotreturnforthe out-patientconsultation. Allthe patientswere operatedbythe seniorauthor,whohasexperienceoftreatingkneeinjuries. Thisauthordidnotparticipateintheprocessofapplyingthe questionnairebeforeandaftertheoperation.
All the patients evaluated in this study signed a free and informed consent statement. The study was submit-tedtothe institution’s research ethicscommitteeand was
approvedundertheethicsassessmentcertificate(CAAE) num-ber18321113.5.0000.0007.
ThedataweretabulatedintheMicrosoftExcel®software and the resultswerepresentedintables, graphsand mea-surements (mean, standard deviation (SD) and coefficient ofvariation).Descriptiveandinferentialanalyseswere per-formedontheresults.AllthecomparisonsrelatingtotheKSS andLysholmwereperformedbymeansoftheMann–Whitney test.Thesignificantlevelwastakentobe5%inallofthese comparisons. All of the variables were analyzed using the Minitabstatisticalsoftware,version14.1.
Results
Toensuretheprecisionofthecomparisons,thehomogeneity ofthetwosampleswasascertained.Takingthesignificance leveltobe5%,itwasobservedfromLevene’stestthat homo-geneityofthesamplewasassured(p>0.05).Inotherwords, theages,gendersandsidesaffectedwerestatisticallyequal
(Table1).
AmongtheACLreconstructionresults,bothfrompatients whoreceivedST-Gautografts(Table2)andfromthosewithPT grafts(Table3),itcouldbeseenthroughtheMann–Whitney
Table1–Homogeneitytestonthepatientsample studied,whounderwentACLreconstructionusingST-G andPTautografts.
Characteristics Standarddeviation pvaluea
ST-G PT
Age 8.565 9.136 0.782
Genderb 0.224 0.308 0.560
Sideaffectedb 0.513 0.510 0.664
ST-G,medialkneeflexors;PT,centralthirdofpatellartendon.
a Levene’stest.
b Genderandsideaffectedwerecodednumericallyinordertoapply
thetest.
Table2–Comparisonofthefunctionalcapacityofthe patientsoftheST-GgroupaccordingtotheKSSand Lysholmscales.
Methods Median pvalue
Beforeoperation Afteroperation
KSSknee 67.5 90.0 0.0001
KSSfunctional 80.0 90.0 0.0001
Lysholm 60.5 90.5 0.0001
Table3–Comparisonofthefunctionalcapacityofthe patientsofthePTgroupaccordingtotheKSSand Lysholmscales.
Methods Median pvalue
Beforeoperation Afteroperation
KSSknee 70.0 91.5 0.0001
KSSfunctional 80.0 90.0 0.0001
100.0 90.0 80.0 70.0 60.0 50.0 40.0 30.0 20.0 10.0
0.0
KSS knee KSS functional Lysholm
Frequency, %
Before operation After operation
Methods
Fig.1–Comparisonofthemethodsforevaluatingthe functionalcapacitybeforeandaftertheoperation,among thepatientswhoreceivedST-Gautografts.
100.0 90.0 80.0 70.0 60.0 50.0 40.0 30.0 20.0 10.0 0.0
KSS knee KSS functional Lysholm
Frequency, %
After operation Before operation
Methods
Fig.2–Comparisonofthemethodsforevaluatingthe functionalcapacitybeforeandaftertheoperation,among thepatientswhoreceivedPTautografts.
testthattherewasstrongevidencethataftertheoperation, thepatients’functionalcapacitywassignificantlygreaterthan beforethe operation,takingthesignificancelevel tobe5% (p<0.05).
Figs.1and2showgeometricallythatbothontheKSSand
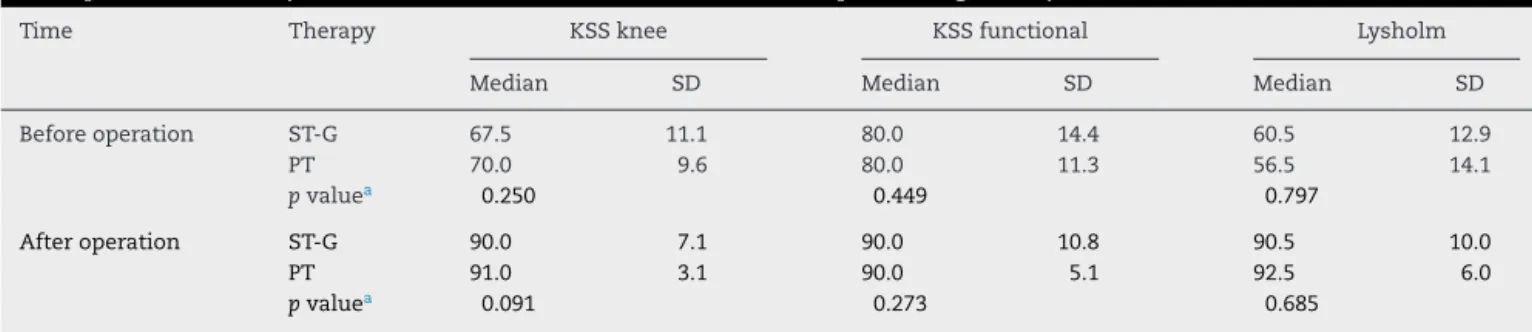
on the Lysholmscale there wasa significantimprovement aftertheoperationinbothgroups(ST-GandPT,respectively). Incomparingfunctionalcapacityfrombeforetoafterthe operationamongpatientswhounderwent boththerapeutic methods(Table4),itcouldbeseenthroughtheMann–Whitney test(whichusesthemedianastheparameter)thattherewas strongevidencethatthetwotherapeuticmethodshadsimilar resultsinallcomparisons(p>0.05).
Discussion
The ACL presents poor potential for spontaneous healing whenitiscompletelytorn.Aroundtwo-thirdsofthepatients with this injury evolve to a high degree of knee instabil-ity, which worsens with the return to physical activities, resultsinrecurrentsubluxationandevolvestofuture func-tional incapacity,meniscallesionsand earlyappearanceof osteoarthrosis (OA).7–10 Amongthe patientswithACL tears
alone or in combination with meniscal lesions or injuries tocollateralligaments,60–90%evolvetoradiographic alter-ationsindicativeofosteoarthrosiswithin10–15years,withthe onsetofsymptomsoccurring10–20yearsearlierthanamong patientswithprimaryOA.11,12
Conservative treatment of ACL injuries may function reasonably well under certain circumstances, especially in patientswho presentminimal exposuretohigh-risk activi-tiesandgoodadaptationtoligamentinsufficiency,orwhen an advanced process of degenerative arthritis in the knee involvedcanalreadybeseen.13
Over the last two decades, the commonest question regarding ACL surgery has been “which is the best graft to choose?” The PT used to be considered to be the gold standardforACLreconstruction.Thereasonsforthisinclude thestrengthofthegraft,therelativeeaseofharvestingitand thebone-to-bonehealingwithsecurefixation.Recently,use ofST-Gautograftshasgainedinpopularityamongsurgeons’ choices.14Thecurrenttrendtowardincreaseduseofthe
ST-Gcomesfromthecaretakentoavoidthepotentialnegative effectontheextensormechanismthatmayensuefromthe PT, along withthe morbidity inthe PTdonor area, which may includeanterior knee pain and the risk of fracturing thepatella.15Nonetheless,despitetheincreasingpopularity
Table4–Comparisonoffunctionalcapacityfrombeforetoaftertheoperationamongthepatientswhounderwentboth therapeuticmethods(medialkneeflexorsandcentralthirdofthepatellarligament).
Time Therapy KSSknee KSSfunctional Lysholm
Median SD Median SD Median SD
Beforeoperation ST-G 67.5 11.1 80.0 14.4 60.5 12.9
PT 70.0 9.6 80.0 11.3 56.5 14.1
pvaluea 0.250 0.449 0.797
Afteroperation ST-G 90.0 7.1 90.0 10.8 90.5 10.0
PT 91.0 3.1 90.0 5.1 92.5 6.0
pvaluea 0.091 0.273 0.685
SD,standarddeviation;ST-G,medialkneeflexors;PT,centralthirdofpatellartendon.
ofST-Ggrafts, theyalsohavepotential limitations, includ-ingslowergraftincorporationintothetunnelthanseenwith thePT,potential wideningofthe tunnelsandresidual lax-ityandfunctionalweaknessoftheflexormusculatureonthe sidefromwhichthegraftisharvested.16,17 InBrazil,aslong
agoas 1999,CamanhoandAndrade18 statedthat although
themiddlethirdofthepatellarligamenttogetherwithbone fragmentsfromthepatellaandtibiawasforalongtime con-sideredtobetheidealgraft,useofautograftsfromthetendons ofthemedialflexormuscles wasbecomingwidely dissem-inatedbecause oftheirefficiency,fixation methodandlow aggressionofthedonorarea,andcomparisonswiththeuseof middlethirdofthepatellartendonwerestartingtobemade intheliterature.
However,inmaking comparisonsbetweenpatients with tornACLsthatweretreatedsurgicallyandpatientsfollowed upconservatively,Meunieretal.19concludedthattherewere
significantlymoremeniscallesionsinpatientswhowere man-agedconservatively,andthatone-thirdofthesecasesevolved tosurgicaltreatmentbecauseofjointinstability.
Amongauthorswhohaveconsideredthatsurgical treat-ment is the first option, ACL reconstruction has been advocatedwiththe objective ofrestoringthe normal kine-matics ofthejoint.In this manner,the instabilityand the potentialassociateddamagetothemenisciandchondral sur-facesareeliminated.Almostuniversally,indicationsforACL reconstructionaremadeinrelationtopatientswhopresent highrisksthroughtheirlifestyle,withdemandsthroughheavy work,sportsorrecreational activitiesthatmightreproduce episodesofsubluxationoftheknee.13
Many studies have already been conductedto compare theautograftsusedintreatmentsforACLinjuries,andthese haveshowedtheirbenefitsand harmforpatientsafterthe operation.20–28
Corry et al.20 made a comparison of the postoperative
resultsamongpatients whounderwent ACLreconstruction arthroscopically,using ST-GorPTautografts.Theycameto theconclusionthattherewasnostatisticallysignificant dif-ferencebetweenthetwogroups,intermsofligamentstability, rangeofmotion(ROM)andgeneralsymptoms,twoyearsafter theprocedure.
InastudybyKeaysetal.,21similarresultscouldbeseen,
with restoration of clinical stability and muscle strength betweenthesurgicalgroupsandcontrols,althoughtherewas adeficitof6%inquadricepsstrengthafterusingPTgrafts.
Erikssonetal.22 alsoconcludedthattherewas no
clini-caldifferenceover the mediumterm,betweengroupsthat underwentACLreconstructionwiththeST-GorPT.Likewise, AhlenandLiden23didnotfindanystatisticallysignificant
dif-ferencesinrelationtomusclestrength,jointinstabilityorROM amongtheirpatients,whowereevaluatedtwoyearsafterthe surgicalprocedure.
However,Samuelssonetal.24andMuellneretal.25observed
that the autograft harvesting site initially affected muscle strengthandthatuse ofthePTproducedmorepaininthe anteriorregionofthekneethandidtheST-G.However,both oftheseauthorsstatedthatthesesymptomsdisappearedover thecourseoftime.
AccordingtoKeaysetal.,26theincidenceofosteoarthritis
afterACLreconstructionisworrisome,withreportsthatup
to50%ofthesepatientsdevelopitmoderatelyorseverely,six yearsaftertheprocedure.Theseauthorsnotedthatthisevent occurredbecauseofthepresenceofchondrallesions,choice ofthePTastheautograft,presenceofaweakquadriceps,low resistanceratiosofthequadricepsandhamstringsand menis-cectomyperformedatthetimeofthesurgery.Basedonthese results,theyrecommendedthatinclinicallyunstableknees, ACLreconstructionshouldnotbeunnecessarilypostponed,so astoavoidfuturemeniscalandchondrallesions.
Pinczewskietal.27foundprospectivelythatuseofthePT
increasedtheincidenceofosteoarthriticradiographic alter-ations inthesepatients’ knees,andalsothat theobserved fixeddeformitiesofflexioncouldpresagetheappearanceof degenerativelesions.
Nonetheless,theidealtimeforACLreconstruction prob-ablydependsontheindividualfactorsofeachpatient,such astheconditionofthekneeandthepatient’smotivationto undergosurgeryandrehabilitation.23
In2012,Mascarenhasetal.3concludedthatbothtypesof
autograftallowedaround70%ofyoungathletestoreturnto somedegreeofvigorousorveryvigorousphysicalactivity(4–7 timesaweek).ACLreconstructionusingflexortendonsleads tobetterpreservationofextension,betterpatientscoresand less evidenceofosteoarthritis.Althoughwefound numeri-callysuperiorscoresinrelationtotheST-G,thesedifferences werenotstatisticallysignificant.
InalevelIsystematicreview,Reinhardtetal.28concluded
thattheriskoffailureofACLreconstructionissignificantly greaterwiththeST-GthanwiththePT.TheST-Gwas supe-riorinrelationtoresiduallaxity.Anteriorkneepainwasmore presentinreconstructionsusingthePT.Inrelationto activ-ity leveland functional evaluations,neither techniquewas superiortotheother.
In 2013, Kim et al.29 did not identify any significant
differencesintheclinicalresultsandstabilityafterACL recon-struction, inrelation tothe typeofgraft orfixation device chosen.Thus,surgeonsshouldselectthe“ideal”ACL recon-structionmethodaccordingtothepatient’sconditionsandthe surgeon’sexperience.29Thesefindingswerecorroboratedby
Abbasetal.,30whohighlightedtheconcernsregarding
ante-riorkneepainandpatellofemoralsymptomsthroughuseof thePT.
In2014,Papaliaetal.31showedthattherewereno
differ-encebetweengroupsreconstructedusingtheST-GorPT,in anyoftheclinicalscoresorfunctionaltests.
Inthepresentstudy,itcouldbeseenthattherewasa sta-tisticallysignificantimprovementaftertheoperation,among thepatientsinbothgroupsstudied(KneeSocietyScoreand Lysholm).Incomparingthepresentstudywiththose inves-tigatedinthe literature,similaritiesinthe resultscouldbe observedwhentheLysholmscalewasused.20–23However,no
relevantdatawerefoundinrelationtousingtheKSSscalein theliteratureinvestigated,whichthusmakesitimpossibleto comparetheresultsobtainedinthepresentstudy.
quadricepsforthePTorflexorfortheST-G.Evaluationofthe criteriaforthereturn tosportwas notanobjectiveofthis study.
Conclusion
Theresults from the ACL reconstructions using autografts fromthecentralthirdofthepatellartendonormedialknee flexorsweresimilarwithregardtofunctionalrecoveryofthe kneeandimprovementofqualityoflife.Thus,becauseofthe proximityofthestatisticalresultsfromthisstudy,itwasnot possibletopreciselyidentifythesurgicaltreatmentthatwould providegreatest benefitforpatients, withleast aggression. Therefore,webelievethatclinicalexperience,thesurgeon’s techniqueandrespectforpatients’individualitymakethe dif-ferenceatthetimeofchoosingthetypeofautograftforusein surgicaltreatmenttoreconstructtheACL.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. GomesJLE,MarczykRLS.Reconstruc¸ãodosligamentos
cruzadosdojoelhocomotendãoduplodosemitendinoso.
RevBrasOrtop.2004;39(4):137–46.
2. GuimarãesMV.Reconstruc¸ãoartroscópicadoligamento
cruzadoanterior:estudocomparativoentreosenxertos
autólogosdeligamentopatelaredetendãodoquadríceps.
RevBrasOrtop.2004;39(1/2):30–41.
3. MascarenhasR,TranovichMJ,KropfEJ,FuFH,HarnerCD.
Bone-patellartendon-boneautograftversushamstring
autograftanteriorcruciateligamentreconstructioninthe
youngathlete:aretrospectivematchedanalysiswith2–10
yearfollow-up.KneeSurgSportsTraumatolArthrosc.
2012;20(8):1520–7.
4. AlbuquerqueRP,GiordanoV,CalixtoA,MalzacF,AguiarC,
AmaralNP,etal.AnálisedoprotocolofuncionaldeLysholm
modificadoempacientescomjoelhosnormais.RevBras
Ortop.2011;46(6):668–74.
5. SilvaALP,DemangeMK,GomesR,SilvaTFC,PécoraJR,Croci
AT.Traduc¸ãoevalidac¸ãodaescalakneesocietyscore:KSS
paraalínguaportuguesa.ActaOrtopBras.2012;20(1):
25–30.
6. PeccinM,CiconelliR,CohenM.Questionárioespecíficopara
sintomasdojoelhoLysholmkneescoringscale(traduc¸ãoe
validac¸ãoparaalínguaportuguesa).ActaOrtopBras.
2006;14(5):268–72.
7. O’DonoghueDH,RockwoodCAJr,FrankGR.RepairoftheACL
indogs.JBoneJointSurgAm.1966;48(3):503–19.
8. ArnoczkySP,RubinRM,MarshallJL.Microvasculatureofthe
cruciateligamentsanditsresponsetoinjury.JBoneJoint
SurgAm.1979;61(8):1221–9.
9. AmielD,KuiperS,AkesonW.Cruciateligaments.Responseto
injury.In:DanielDM,AkesonW,O’ConnorJ,editors.Knee
ligaments:structure,function,injuryandrepair.NewYork:
RavenPress;1990.p.365–77.
10.BeynnonBD,JohnsonRJ,AbateJA,FlemingBC,NicholsCE.
Treatmentofanteriorcruciateligamentinjuries,PartII.AmJ
SportsMed.2005;33(11):1752–67.
11.SegawaH,OmoriG,KogaY.Long-termresultsof
non-operativetreatmentofanteriorcruciateligamentinjury.
Knee.2001;8(1):5–11.
12.RoosH,AdalberthT,DahlbergL,LohmanderLS.
Osteoarthritisofthekneeafterinjurytotheanteriorcruciate
ligamentormeniscus:theinfluenceoftimeandage.
OsteoarthrCartil.1995;3(4):261–7.
13.BeynnonBD,JohnsonRJ,AbateJA,FlemingBC,NicholsCE.
Treatmentofanteriorcruciateligamentinjuries,PartI.AmJ
SportsMed.2005;33(10):1579–602.
14.McRaeS,ChahalJ,LeiterJ,MarxRG,McDonaldPB.Asurvey
studyofmembersoftheCanadianOrthopaedicAssociation
regardingthenaturalhistoryandtreatmentofanterior
cruciateligamentinjury.In:AOSSMAnnualMeeting.2009.
15.BiauDJ,TournouxC,KatsahianS,SchranzPJ.Bonepatellar
tendon-boneautograftsversushamstringautograftsfor
reconstructionofanteriorcruciateligament:meta-analysis.
BMJ.2006;332(7548):995–1001.
16.HollisR,WestH,GreisP,BrownN,BurksR.Autologousbone
effectsonfemoraltunnelwideninginhamstringanterior
cruciateligamentreconstruction.JKneeSurg.
2009;22(2):114–9.
17.BizziniM,GorelickM,MunzingerU,DrobnyT.Jointlaxityand
isokineticthighmusclestrengthcharacteristicsafteranterior
cruciateligamentreconstruction:bonepatellartendonbone
versusquadrupledhamstringautografts.ClinJSportMed.
2006;16(1):4–9.
18.CamanhoGL,AndradeMH.Estudocomparativoda
reabilitac¸ãodospacientessubmetidosàreconstruc¸ãodo
ligamentocruzadoanteriorcomenxertosdoterc¸omédiodo
tendãopatelarecomosdostendõesdosmúsculosflexores
mediaisdojoelho.RevBrasOrtop.1999;34(9/10):
513–8.
19.MeunierA,OdenstenM,GoodL.Long-termresultsafter
primaryrepairornon-surgicaltreatmentofanteriorcruciate
ligamentrupture:arandomizedstudywitha15-year
follow-up.ScandJMedSciSports.2007;17(3):230–7.
20.CorryIS,WebbJM,ClingelefferAJ,PinczewskiLA.
Arthroscopicreconstructionoftheanteriorcruciateligament:
acomparisonofpatellartendonautograftandfour-strand
hamstringtendonautograft.AmJSportsMed.
1999;27(3):444–54.
21.KeaysSL,Bullock-SaxtonJE,KeaysAC,NewcombePA,Bullock
MI.A6-yearfollow-upoftheeffectofgraftsiteonstrength,
stability,rangeofmotion,function,andjointdegeneration
afteranteriorcruciateligamentreconstruction:patellar
tendonversussemitendinosusandgracilistendongraft.AmJ
SportsMed.2007;35(5):729–39.
22.ErikssonK,AnderbergP,HambergP,LöfgrenAC,Bredenberg
M,WestmanI,etal.Acomparisonofquadruple
semitendinosusandpatellartendongraftsinreconstruction
oftheanteriorcruciateligament.JBoneJointSurgBr.
2001;83(3):348–54.
23.AhlenM,LidenM.Acomparisonoftheclinicaloutcomeafter
anteriorcruciateligamentreconstructionusingahamstring
tendonautograftwithspecialemphasisonthetimingofthe
reconstruction.KneeSurgSportsTraumatolArthrosc.
2011;19(3):488–94.
24.SamuelssonK,AnderssonD,KarlssonJ.Treatmentofanterior
cruciateligamentinjurieswithspecialreferencetografttype
andsurgicaltechnique:anassessmentofrandomized
controlledtrials.Arthroscopy.2009;25(10):1139–74.
25.MuellnerT,KaltenbrunnerW,NikolicA,MittlboeckM,
SchabusR,VecseiV.Shorteningofthepatellartendonafter
anteriorcruciateligamentreconstruction.Arthroscopy.
1998;14(6):592–6.
26.KeaysSL,NewcombePA,Bullock-SaxtonJE,BullockMI,Keays
afteranteriorcruciateligamentsurgery.AmJSportsMed. 2010;38(3):455–63.
27.PinczewskiLA,DeehanDJ,SalmonLJ,RussellVJ,Clingeleffer
A.Afive-yearcomparisonofpatellartendonversus
four-strandhamstringtendonautograftforarthroscopic
reconstructionoftheanteriorcruciateligament.AmJSports
Med.2002;30(4):523–36.
28.ReinhardtKR,HetsroniI,MarxRG.Graftselectionforanterior
cruciateligamentreconstruction:alevelIsystematicreview
comparingfailureratesandfunctionaloutcomes.OrthopClin
NorthAm.2010;41(2):249–62.
29.KimHS,SeonJK,JoAR.Currenttrendsinanteriorcruciate
ligamentreconstruction.KneeSurgRelatRes.
2013;25(4):165–73.
30.AbbasMM,AbulabanAA,DarwishHH.Functionaloutcomes
ofbonetendonboneversussofttissuearthroscopicanterior
cruciateligamentreconstruction:acomparativestudy.Saudi
MedJ.2013;34(2):153–60.
31.PapaliaR,FranceschiF,TecameA,D’AdamioS,MaffulliN,
DenaroV.Anteriorcruciateligamentreconstructionand
returntosportactivity:posturalcontrolasthekeytosuccess.