w w w . r b o . o r g . b r
Original
article
Clinical
aspects
of
patients
with
traumatic
lesions
of
the
brachial
plexus
following
surgical
treatment
夽
Frederico
Barra
de
Moraes
∗,
Mário
Yoshihide
Kwae,
Ricardo
Pereira
da
Silva,
Celmo
Celeno
Porto,
Daniel
de
Paiva
Magalhães,
Matheus
Veloso
Paulino
DepartmentofOrthopedicsandTraumatology,SchoolofMedicine,UniversidadeFederaldeGoiás(UFG),Goiânia,GO,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received24March2014 Accepted23October2014 Availableonline9September2015
Keywords:
Accidentprevention Multipletrauma Brachialplexus/surgery
a
b
s
t
r
a
c
t
Objective:Toevaluatesociodemographicandclinicalaspectsofpatientsundergoing opera-tionsduetotraumaticlesionsofthebrachialplexus.
Method:Thiswasaretrospectivestudyinwhichthemedicalfilesofaconveniencesampleof 48patientsoperatedbetween2000and2010werereviewed.Thefollowingwereevaluated: (1)rangeofmotion(ROM)oftheshoulder,elbowandwrist/hand,indegrees;(2)gradeof strengthoftheshoulder,elbowandwrist/hand;(3)sensitivity;and(4)visualanaloguescale (VAS)(from0to10).TheStudent’st,chi-square,Friedman,WilcoxonandKruskal–Wallis testswereused(p<0.05).
Results:Thepatients’meanagewas30.6years;60.4%ofthemhadsufferedmotorcycle acci-dentsand52.1%,multipletrauma.Themeanlengthoftimeuntilsurgerywas8.7months (range:2–48).Thirty-onepatients(64.6%)presentedcompleteruptureoftheplexus.The frequentoperationwasneurosurgeryin39cases(81.3%).TheROMachievedwas≥30◦in20 patients(41.6%),witharangefrom30◦to90◦andmeanof73◦(p=0.001).Thirteen(27.1%) alreadyhadshoulderstrength≥M3(p=0.001).Twenty-sevenpatients(56.2%)hadelbow flex-ion≥80◦
,witharangefrom30◦ to160◦
andmeanof80.6◦
(p<0.001).Twenty-twohadstrength ≥M3(p<0.001).Twenty-twopatients(45.8%)hadwristextension≥30◦startingfromflexion of45◦,witharangefrom30◦to90◦andmeanof70◦(p=0.003).Twenty-seven(56.3%) pre-sentedwrist/handextensionstrength≥M3(p=0.002).Forty-five(93.8%)hadhypoesthesia andthree(6.2%)hadanesthesia(p=0.006).TheinitialVASwas4.5(range:1.0–9.0)andthe finalVASwas3.0(range:1.0–7.0)(p<0.001).
Conclusion:Traumaticlesionsofthebrachialplexus weremoreprevalentamongyoung adults(21–40years),men,peoplelivinginurbanareas,manualworkersandmotorcycle accidents,withmultipletraumaandtotalruptureoftheplexus.Neurosurgery,witha sec-ondprocedureconsistingofmuscle-tendontransfer,wasthecommonestoperation.Surgery fortraumaticlesionsofthebrachialplexusresultedinsignificantimprovementintheROM andstrengthoftheshoulder,elbowandwrist/hand,improvementofthesensitivityofthe limbaffectedandreductionofthefinalpain.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
夽
WorkperformedintheHandandMicrosurgeryService,HospitaldasClínicas,UniversidadeFederaldeGoiás(UFG),Goiânia,GO,Brazil. ∗ Correspondingauthor.
E-mail:fredericobarra@yahoo.com.br(F.B.deMoraes). http://dx.doi.org/10.1016/j.rboe.2015.08.015
Aspectos
clínicos
de
pacientes
com
lesão
traumática
do
plexo
braquial
após
tratamento
cirúrgico
Palavras-chave:
Prevenc¸ãodeacidentes Traumatismomúltiplo Plexobraquial/cirurgia
r
e
s
u
m
o
Objetivo: Avaliaraspectossociodemográficose clínicosdepacientesoperados delesão traumáticadoplexobraquial(LTPB).
Método:Estudoretrospectivo,revisãodeprontuários,amostradeconveniência,48pacientes operadosentre2000e2010.Avaliados:1)ADM–emgraus,doombro,cotoveloepunho/mão; 2)graudeforc¸adoombro,cotoveloepunho/mão;3)sensibilidade;4)EVA(0a10).Testesde
tdeStudent,qui-quadrado,Friedman,WilcoxoneKruskal–Wallis(p<0,05).
Resultados: Idadede30,6anos,60,4%acidentesmotociclísticos.Politraumatismo 52,1%. Tempoatéacirurgiade8,7meses(2a48).Trintaeum(64,6%)comlesãototaldoplexo. Cirurgiasmaisfrequentes:neuraisem39(81,3%).ADM≥30◦doombro20pacientes(41,6%) de 30◦
a90◦
,média 73◦
(p=0,001);13 (27,1%)játinhamforc¸anoombro≥M3(p=0,001). Cotovelo≥80◦deflexão,27pacientes(56,2%)de30◦a160◦,commédiade80,6◦(p<0,001); 22 comforc¸a≥M3(p<0,001).Extensãodopunho≥30◦partindo de45◦de flexãoem22 pacientes(45,8%),de30◦a90◦,média70◦(p=0,003);27(56,3%)tinhamforc¸adeextensão dopunho/mão≥M3(p=0,002);45(93,8%)hipoestesiaetrês(6,2%)anestesia(p=0,006).EVA inicial4,5(1a9)eEVAfinal3(1a7)(p<0,001).
Conclusão:AsLTPBtemmaiorprevalênciaemjovens(21–40anos),homens,urbanos, trabal-hadoresbrac¸ais,acidentesmotociclísticos,compolitrauma,lesãototaldoplexo.Cirurgias neurais,seguidasemsegundotempo,pelastransferênciasmiotendíneas.Acirurgiapara LTPBmostroumelhoriasignificativadeADMeforc¸aemombro,cotoveloepunho/mão,da sensibilidadedomembroafetadoediminuic¸ãodadorfinal.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Todososdireitosreservados.
Introduction
Traumaticbrachialplexusinjuriesare debilitatingand lead tomotorandsensorydeficit,pain,functionallimitationand significantalterationstopatients’qualityoflife.Theyaremore prevalentamongyoungadultswhohavesufferedhigh-energy trauma,especiallycaraccidents.1–3Diagnosisisdifficultand treatmentiscomplex.Theincidenceoftheseinjuriesis1.3% inmultiple-traumapatientsand 5%inmotorcycle accident victims.4
Thefirstdescriptionsoftraumaticbrachialplexusinjuries came from periods of great wars, caused by wounds that wereopenedbymeansofcuttingandbluntobjects,suchthat blowsorprojectileshittingtheshoulderwouldleadtolossof upperlimbmovement.ThefirstwrittenreportwasintheIliad, writtenbyHomer(9thcenturyB.C.;TrojanWar).5However, sci-entificpublicationsonlybeganinthe19thcenturyduringthe Americancivilwarand,later,inthe20thcentury,whenclosed injuriesstartedto becomepredominant,causedbyfirearm accidents,explosionsandmilitaryvehicles,withhigh-energy trauma.6
Surgeries for reconstructing traumatic brachial plexus injurieshavethefollowingmainobjectives:(1)stabilization andexternalrotation oftheshoulder; (2)elbowflexion;(3) wrist and finger flexion; (4) hand sensitivity; (5) thoraco-brachial clamp; and (6) pain relief.2–4 In 1900, Thorburn7 describedthefirstsurgeryfortreatinginjuriesofthebrachial plexus through a technique with direct repair, followed byHarris and Low,8 who in 1903proposed neural transfer
(neurotization),andbySeddon,9whopublishedacorrection technique with interposition of neural grafts in 1947. For better functional results from the upperlimb, the modern manner ofdealing with traumaticbrachial plexus injuries includes complex neuromicrosurgical techniques that are performed early (neurolysis, direct neural repairs, neural transfers and nerve grafts);or later on, myotendinous and bonesurgery(tendontransfer, freemuscletransfers and/or osteotomies with joint arthrodesis), which expanded the possibilitiesoffunctionalrecoveryoftheinjuredupperlimb.
Theobjectiveofthepresentstudywastoevaluatethe clin-icalcharacteristicsandfunctionalgainoftheupperlimbin patientswho underwent surgicaltreatmentaftertraumatic brachialplexusinjuries.
Methods
This was a retrospective study conductedthrough review-ingthemedicalfilesofaconveniencesampleof48patients withtraumaticbrachialplexusinjurywhowereoperated con-secutively at the Hand and Microsurgery Service between December2000andDecember2010.
Theclinicalcharacteristicsevaluatedwere:(1)agegroup; (2)sex;(3)sideaffected;(4)origin;(5)typeofworkbeforethe accident;(6)typeofaccident;(7)intervalbetweentraumatic brachialplexusinjuryandthefirstappointmentatthe spe-cializedcareservice;(8)intervalbetweentraumaticbrachial plexusinjuryandthefirstsurgeryperformedbythe special-izedteam;(9)associationwithmultipletrauma;(10)levelof theneuralinjury(trunksaffected),determinedthrough phys-icalexamination,electromyographyand the initialsurgical findings;(11)typeofneuralinjuryaccordingto electromyo-graphy;(12)typesofsurgeriesperformed.
The functional recovery parameters of the upper limb consisted of the pre- and post-surgery clinical examina-tions,inastandingposition.Regardingtheoverallfunctional characteristics,thefollowingwere evaluated:(1)jointrange of motion (ROM), in degrees, of the shoulder, elbow and wrist/hand,measuredthroughmanualgoniometry;(2)degree ofstrengthoftheshoulder,elbowandwrist/hand,measured usingthemusclestrengthscaleoftheBritishMedicalCouncil (M0=absence ofactivity;M1=fasciculation;M2=movement cannot overcome gravity; M3=movement overcomes grav-ity;M4=movementovercomesaresistanceforce;M5=normal strength);(3) sensitivityof the injured limb(classified into anesthesia,hypoesthesiaand normal); (4) pain, whichwas recordedonavisualanaloguescale(VAS),rangingfrom0to 10,where0isthetotalabsenceofpainand10theworstpain everreported(0–3=mildpain;4–7=moderate;8–10=intense). Thefollowingfunctionalparameterswereconsidered sat-isfactory (10–21): (1) ROM: shoulder abduction≥30◦, elbow flexion≥80◦, wrist extension≥30◦; (2) strength: shoulder abduction≥M3,elbowflexion≥M3,wristextension≥M3;(3) sensitivity: hypoesthesia and normal; (4) pain: VAS≤3 or reductionof50%oftheinitialvalue.
ThedataweregatheredandstoredintheExcelfor Win-dowssoftware,andwereanalyzedusingstatisticalsoftware (SPSSversion13.0forWindows).Allsampleswereevaluated usingtheStudentt,chi-square,FriedmanandWilcoxontests forparametricdataandtheKruskal–Wallistestfor nonpara-metricdata.Thesignificancelevelwastakentobep≤0.05.
Results
Outofthe48patientswithtraumaticbrachialplexusinjuries, onlyone(2%) wasfemale, and 24cases (50%)were onthe rightside.Themeanagewas30.6years(range:14–59):seven patients(14.6%)were10–20yearsold,33(68.8%)were21–40, and eight (16.7%) were 41–60. Regarding the origin of the patients,20(41.7%)werefromthestatecapital,11(22.9%)from townsintheregion surroundingthe statecapital,12 (25%) fromelsewhereinthesamestateandfive(10.4%)fromother states.Regardingthetypeofworkthatthepatientsweredoing beforetheaccident,16(33.3%)wereunemployed,18(37.5%) werelaborersand12(25%)administrative,amongwhomsix (12.5%)weremotorcyclecouriersandtwo(4.2%)were intellec-tuals.
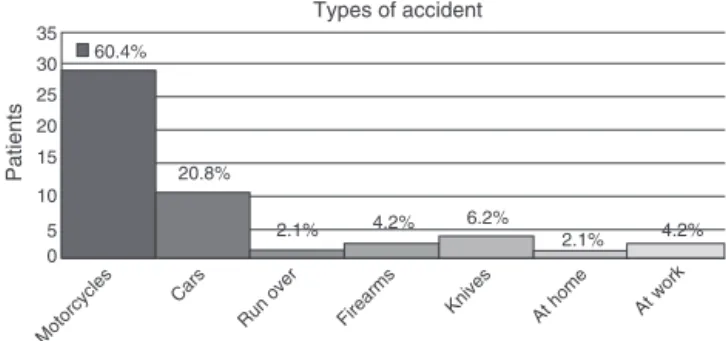
Regardingthetypesofaccidents(Fig.1),29patients(60.4%) wereonmotorcycles;10(20.8%)wereincars;one(2.1%)was runover;five(10.4%)sufferedinjuriesfromweapons,ofwhich twocases(4.2%)weregunshotwoundsandthreecases(6.2%)
35 60.4%
20.8%
2.1% 4.2% 6.2% 2.1% 4.2%
30 25 20 15
10
5 0
Patients
Types of accident
Motorcycles Cars
Run over Firearms Knives At home At work
Fig.1–Typesofaccidentssufferedbypatientswith traumaticbrachialplexusinjury,withhighestfrequencyof motorcycleaccidents.
were stabbings; one patient (2.1%) suffered an accidentat home and two(4.2%) atwork. Themean interval between traumaticbrachialplexusinjuriesandthefirstdoctor appoint-mentwas4.2months(range:1–17)anduntilthesurgerywas 8.7 months(range: 2–48). Eightpatients (16.8%) underwent surgerybetween1and3monthsaftertheirinjury,19(39.3%) between3and6months,12(25%)between6and12months, andnine(18.9%)morethan12monthsaftertraumaticbrachial plexusinjury.Theseweremusculoskeletaloperations,andnot neural,becauseofthetimeatwhichtheyarrived.Patientsin the agegroupbetween21 and 40years underwentsurgery significantlyearlier(lessthan6monthsafterinjury)thanthe others(p=0.023).
Regarding the presenceof multiple trauma, 25 patients (52.1%)presentedother formsoftraumainaddition tothe brachialplexusinjury(Table1).
Thecomplementaryexaminationusedforevaluating trau-matic brachial plexusinjuries was electroneuromyography. Concerningtheleveloftheneuralinjury(Fig.2),31patients (64.6%)presentedtotalbrachialplexusinjury:12(25%)inthe uppertrunk,three(6.2%)intheupperandmiddletrunks,and two(4.2%)inthemiddleandlowertrunks.Regardingthetype of neural injury (Fig. 3), 20 (41.6%) presentedneurotmesis, 24 (50%) axonotmesis and four (8.4%), neuropraxia,among which10(20.8%)wereavulsions.TheClaude–Bernard–Horner syndromewasfoundinfivepatients(10.4%).Asignificant cor-relationwasobservedbetweenthelevelofneuralinjuryseen onphysicalexamination(trunksaffected), electroneuromyo-graphy(p<0.001)andtheinitialsurgicalfinding(p=0.003).In addition, factorssuchbeingalaborer(p=0.007)or havinga
Table1–Traumaassociatedwithbrachialplexusinjury.
Trauma No.ofpatients (%)
1.Claviclefracture 11 22%
2.Traumaticbraininjury 5 10%
3.Forearmfracture 5 10%
4.Faceinjury 3 6%
5.Lower-limbfracture 2 4%
6.Upper-limbfracture 2 4%
7.Arterialinjuryoftheshoulder 2 4%
35
30
25
20
15
10
5
0
Patients
64.6%
25%
4.2% 6.2%
Total injury of the brachial plexus
Upper and middle trunks
Upper trunk Lower trunk
Level of neural injury
Fig.2–Levelofneuralinjuryinpatientswithtraumatic brachialplexusinjury.
motorcycleaccident(p=0.012)presentedacorrelation with totalbrachialplexusinjury.
Regarding the type of surgery performed initially, 39 patients (81.3%)underwent neural surgery(Table 2), seven (14.5%) muscle-tendon transfers (flexor-pronators for the wristandfingersextensors)andtwo(4.2%)wristarthrodesis. Asecondsurgical procedurewasperformed on20patients (41.6%),amongwhich18weremuscle-tendontransfers,one neurotizationandonewristarthrodesis.
Thetimeuntilthesecond surgeryvariedgreatly,from 2 to60monthsafterthefirstprocedure.Outofthe18 muscle-tendontransfers performedon this occasion,twowere for stabilizingtheshoulder,twoforfingermovementand14for elbowflexion.
RegardingthegainofROMoftheshoulder,thefollowing resultswereobserved:42patients(87.5%)didnotpresentany movementafterthetraumaticbrachialplexusinjuryandonly six(12.5%)hadROM≥30◦(stable).Afterthesurgicaltreatment, 20patients(41.6%)improvedtheirROM,andthischangewas significant(p=0.001).Therangewasfrom30◦to90◦,witha meanof73◦,in14patientswhodidnothaveanyROMandsix whoalreadyhadsomeROMandachievedimprovements.
Regarding the gain ofROM ofthe elbow, the following resultswereobserved:43patients(89.6%)didnotpresentany motionaftertraumaticbrachialplexusinjuriesandonlyfive (10.4%)hadROM≥30◦.Afterthetreatment, againofelbow flexion≥80◦occurredin27patients(56.2%),witharangefrom 30◦to160◦,withameanof80.6◦(p<0.001),22didnothaveany ROMandfivehadsomeROMandachievedimprovement.
30
25
20
15
10
5
0
Patients
Type of neural injury
41.6%
50%
8.4%
Neurotmesis Axonotmesis Neuropraxia
Fig.3–Typeofneuralinjuryinpatientswithtraumatic brachialplexusinjury.
Table2–Neuralsurgicalproceduresperformedon brachialplexusinjuries.
Typeofneuralsurgery No.ofpatients (%)
1.Neurolysisandsuralgrafts 28 58.4 2.Neurotizationfromtheulnartothe
medianandmusculocutaneousnerves
13 27
3.Neurotizationfromtheaccessorytothe suprascapularnerve
10 20.8
4.Directneurorrhaphyoftheulnar 9 187 5.Neurotizationfromtheulnartothe
musculocutaneousnerve
5 10.4
6.Neurotizationfromtheintercostalto themusculocutaneousnerve
4 8.4
RegardingthegainofROMofthewrist/hand,the follow-ingresultswereobserved:34patients(70.8%)presentedthe wrist/handinthetotalflexion position(45◦)withoutactive
motionaftertraumaticbrachialplexusinjury,seven(14.6%) had ROM≥30◦ andseven(14.6%)hadtotalROM(90◦).After
treatment,againofwristextension≥ 30◦beginningat45◦of
flexionoccurredin22patients(45.8%)andthisrangedfrom 30◦ to90◦,withameanof70◦ forthesepatients(p<0.001).
Therewere13whodidnothaveanyROMandninewhohad
someROMandachievedimprovement.
Regarding the gain of shoulder strength, the following
resultswereobserved:42patients(87.5%)didnotpresentany functional muscle activity aftertheir injury to the plexus, and onlysix(12.5%)hadstrength≥M3.Afterthesurgeries,
13 (27.1%) had strength≥M3and six (12.5%) evolvedfrom
M0toM2(stableshoulder).These changeswere significant (p<0.001).
Regardingthegainofelbowstrength,thefollowingresults wereobserved:44patients(91.6%)didnotpresentany func-tionalmuscleactivityaftertraumaticbrachialplexusinjury, and onlyfour (8.4%)had strength≥M3.Aftertreatment, 30
patients (62.5%) presented improvements in elbow flexion
strength,and22achievedstrength≥ M3(p<0.001).
Regarding thegainofwrist/handstrength,thefollowing results were observed: 26 patients (54.2%) did not present anyfunctionalmuscleactivityaftertraumaticbrachialplexus injury,while22(45.8%)hadstrength≥ M3.Afterthesurgeries,
27(56.3%)hadstrength≥ M3.Thesechangesweresignificant
(p=0.002).
Regardingsensitivityaftertheplexusinjury,33(68.6%) pre-sentedhypoesthesiaand15(31.2%)hadanesthesia.Afterthe surgicalprocedures,45 (93.8%)presentedhypoesthesiaand three(6.2%)hadanesthesia.Thisevolutionofsensitivitywas significant over the course of time (p=0.006). None of the patientsrecoverednormalsensitivity,incomparisonwiththe uninjuredside.
Painaftertrauma,evaluatedthroughthevisualanalogue
scale (VAS), rangedfrom 1to 9, with amean of4.5. Nine
Discussion
Thereisgreatdifficultyindiagnosingandtreatingtraumatic brachialplexusinjurybecauseitisinfrequentandhighly com-plex.Fewcentershavespecializedprofessionalsandmaterial forthistypeoftreatment,eitherinBrazilorinothercountries. Thepost-surgicalfunctionalresultsareobtainedoverthelong term(usuallyafter1or2years)andmanypatientsareunable toadheretorehabilitationduetotheirprecarious socioeco-nomicconditions.
Difficultiesinpublicservicesinrelationtomakingclinical diagnosesandprovidingcareinreferralcenters,difficultyin performingcomplementaryexaminationssuchas electroneu-romyographyandmagneticresonanceimaging,longintervals betweenaccidentandsurgery,constantneed(formanyyears) togototherehabilitationcenterandfunctionalresultsbelow patients’expectationsarethemostcommonfactorsthatlead patientstoabandontheir treatment.1 Inthepresent study, thiscouldbeobservedbecauseofthediversifiedoriginsofthe patients.Inaddition,the meanintervalfrom thetraumatic brachialplexusinjurytothefirstappointment(4.2months), anduntilthesurgery(8.7months),worsenedtheprognosis. Twenty-onepatients (43%)underwent surgerymorethan 6 monthsaftertheirinjury.
Many ofour patients were performing low-qualification manualactivitiesbeforetheiraccidents.Manyofthese activ-ities demand physical effort, which limits these patients’ reintegrationintotheworkmarketaftertheaccidentand com-promisestheirincomes.Manydonotevenhavesocialsecurity benefits(INSS)orarereassignedtootherfunctionsbecause theyarenotperformingworkunderaformalcontractorare unemployed.10Ourdatashowthatatthetimeoftheaccident, thestudy populationconsistedofyoungunemployed men, laborersormotorcyclecouriers.Thispatientgroupwasunable toreturntotheworkmarket,andthisalsoleadstolossesfor society,whichhastobearthecostoftheirearlyretirement.
Accordingto the MinistryofHealth,young people have more motorcycle accidents than the general population.11 Motorcycleaccidentsarecloselyrelatedtotraumaticbrachial plexusinjuries.Severalstudieshaveproventhishigh preva-lence ofmorbidity and mortality. Even in countries where peopledonotridemotorcyclesbecause thesnowdoes not allowthem todo so, accidentsinvolving similar means of transportationsuchassnowmobilespresenthighincidenceof traumaticbrachialplexusinjuries.10–14Datafromthe micro-surgeryserviceofourinstitutionrevealthatbetween2004and 2007,amongthe160patientswithtraumaticbrachialplexus injurieswho were treated, approximately60% ofthe cases werecausedbymotorcycleaccidents.1Inthepresentstudy, 62%ofthepatients withtraumaticbrachial plexusinjuries hadhadmotorcycleaccidents.
Regardingthecliniccharacteristicsofpatientswith trau-maticbrachialplexusinjuries,therewasastrongassociation withthe presenceofmultipletraumain25 patients(52%), especiallyclaviclefracturesin11(22%)and traumaticbrain injury(TBI)infive(10%).Severalstudiesintheliteraturehave shownthisclinicalassociation,whichcanhampertheinitial diagnosisoftraumaticbrachialplexusinjuriesanddelaythe beginningofpropertreatment.2–4Manypatientsareonlysent
forevaluationoftheplexusinreferralcentersafterfractures andmultipletraumahavebeentreated.
Regardingtheleveloftheneuralinjury,31patients(64.5%) presented total brachial plexus injury, which corroborates thedataintheliteratureandtransformstraumaticbrachial plexus injuries into quite a severe situation that leaves sequelae.1–4,14–19Thetraumamechanismcomprisingtraction of the brachial plexus in car accidents, due to the high-energyimpact,leadstoneuralinjuriesofgreaterseverity.This was alsoconfirmed bythe electromyographyperformedon thesepatients,regardingthetypeofneuralinjury:20patients (41.6%)presentedneurotmesisand24(50%)axonotmesis.
Surgeries fortreating traumatic brachial plexusinjuries can bedivided into neural, muscle-tendonand bone. Neu-ralsurgeries shouldpreferablybeperformednotmorethan 6monthsafterinjury inordertoobtain abetterprognosis regardingreinnervation.Neuralprocedurescanbe intraplex-ural or extraplexural and are considered to present high complexity.14–19Inthepresentstudy,theinitialsurgical pro-cedures were most frequently of neural type, which were performedin39cases:28casesofneurolysisinassociation withneurorrhaphy withsural grafts;24 casesof neurotiza-tionofwhichthemostcommononeswere13fromtheulnar tothemedianandmusculocutaneousnervesand10fromthe accessorytothesuprascapularnerves;andnineneurorrhaphy procedures.Inthesecondoperation,theproceduremostoften performedwasmuscle-tendon,with18transfers,ofwhich14 wereforelbowflexion.
Regardingthesensitivityaftersurgicaltreatmentof trau-maticbrachialplexusinjuries,asignificantimprovementwas observed in12 patients (25%)who moved from anesthesia tohypoesthesia(p=0.006),althoughnoneofthemrecovered theirnormalsensitivity,comparedwiththeuninjuredside. Post-traumapainvariedinintensity,withaninitialmeanof 4.5(range:1–9)andfinalof3(range:1–7).This25%reduction ofpainwassignificantoverthecourseoftime(p<0.001).This agreeswiththeliterature,whichshowsalong-term improve-mentofpainof30%,aftersurgery.20Painmayhaveanimpact onthequalityoflifeofthesepatients,eveniftheypresent significantfunctionalgains.21,22
Regarding the gain ofshoulderstrength,onlyathirdof thepatientspresentedabduction≥M3afterthefirstsurgery, whilerecoveryinapproximatelytwo-thirdsofthepatientshas beenreportedinliteratures.23,24 Regardingthegainofelbow strength,onlyhalfofthepatientspresentedflexion≥M3by the end ofthe treatment, whilerecovery ofapproximately twothirdsofthepatientshasbeenreportedinliteratures.23–25 Theseresultscanbeexplainedbythedifficultiesanddelaysin accessingbettertreatmentthatexistinthird-worldcountries, withfewreferralcentersfortreatingtraumaticbrachialplexus injury.
throughquestionnairesandscalessuchasDASH(Disability ofArm,ShoulderandHand).Inaddition,itdoesnottakeinto considerationanevaluationofthepatienthimself,whichcan beperformedthroughinstrumentssuchastheMcGill,SF-36 andWHOQOL-brefscales,forevaluatingqualityoflife.27–30
Conclusion
Traumaticbrachialplexusinjuriespresenthigherprevalence amongyoungmaleadults(21–40yearsold),individualsliving inurbanareasandlaborers.Theyaremostlycausedby motor-cycleaccidentsandareassociatedwithmultipletrauma,with totalplexusinjury,mostfrequentlycomprisingneurotmesis oraxonotmesis.Themostcommonsurgicalprocedureswere neural(neurolysis,neurorrhaphy,grafts and neurotization), followedinasecondprocedure bymuscle-tendontransfers fortoachievegainsofelbowflexion.
Surgical treatmentof traumaticbrachial plexus injuries waseffective,withimprovementsofrangeofmovementand the strength of shoulders, elbows and wrists/hands, along withimprovementofthesensitivityoftheaffectedlimband reductionofthefinalpain.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. TraspadinePC.Acidentesdemtocicletasesuarelac¸ãocoma
lesãodoplexobraquial.In:BijosP,CorreaJFG,editors.Plexo
braquial.RiodeJaneiro:DiLivros;2011.p.43–58.
2. TerzisJK,KostopoulosVK.Thesurgicaltreatmentofbrachial
plexusinjuriesinadults.PlastReconstrSurg.
2007;119(4):73e–92e.
3. BijosP.Lesõesdeplexobraquial.In:BijosP,ZumiottiAV,
RochaJR,FerreiraMC,editors.Microcirurgiareconstrutiva.
SãoPaulo:Atheneu;2005.p.199.
4. OberlinC.Brachialplexuspalsyinadultswithradicular
lesions,generalconcepts,diagnosticapproach,andresults.
ChirMain.2003;22(6):273–84.
5. HomeroOM,NienkotterS.Ilíada.Campinas,SP:Editora
Unicamp;2008.
6. ToffoloL,SilvaJB.Lesõestraumáticasdoplexobraquialno
adulto:diagnosticoetratamento.ActaMéd(PortoAlegre).
2010;31:157–64.
7. ThorburnW.Secondarysutureofbrachialplexus.BrMedJ.
1900;1:1073–5.
8. HarrisW,LowVW.Importanceofaccuratemuscularanalysis
inlesionsofthebrachialplexusandthetreatmentofErb’s
palsyandinfantileparalysisoftheupperextremityby
cross-unionofnerveroots.BrMedJ.1903;2:1035–8.
9. SeddonHJ.Theuseofautogenousgrafitsfortherepairof
largegapsinperipheralnerves.BrJSurg.1947;35(138):151–67.
10.CavalcanteJ,JorgeNetoF.Oportadordedeficiênciano
mercadoformaldetrabalho.SãoPaulo:Atheneu;2001.
11.Brasil.AnálisedoMinistériodaSaúderevelaqueosacidentes commotosforamosquemaiscresceramnopaísdesdea décadade1990.Disponívelem:www.saude.gov.br.
12.KoizumiS.Padrãodaslesõesnasvítimasdeacidentespor
motocicletas.RevSaudePublica.1992;26(5):306–15.
13.Denatran.Estatísticarelacionadaaosacidentescomvítimas fataisenãofataisentre2002e2006envolvendomotocicletas. Disponívelem:www.denatran.gov.br.
14.BengtsonKA,SpinnerRJ,BishopAT,KaufmanKR,
Coleman-WoodK,KircherMF,etal.Measuringoutocomesin
adultbrachialplexusreconstruction.HandClin.
2008;24(4):401–15.
15.BishopAT.Functioningfree-muscletransferforbrachial
plexusinjury.HandClin.2005;21(1):91–102.
16.VekrisMD,BerisAE,LykissasMG,KorompiliasAV,VekrisAD,
SoucacosPN.Restorationofelbowfunctioninseverebrachial
plexusparalysisviamuscletransfers.Injury.2008;39Suppl.
3:S15–22.
17.BarrieKA,SteinmannSP,ShinAY,SpinnerRJ,BishopAT.
Gracilisfreemuscletransferforrestorationoffunctionafter
completebrachialplexusavulsion.NeurosurgFocus.
2004;16(5):E8.
18.DoiK,HattoriY,IkedaK,DhawanV.Significanceofshoulder
functioninthereconstructionofprehensionwithdouble
free-muscletransferaftercompleteparalysisofthebrachial
plexus.PlastReconstrSurg.2003;112(6):1596–603.
19.DoiK,MuramatsuK,HattoriY,OtsukaK,TanS,NandaV,
etal.Restorationofprehensionwiththedoublefreemuscle
techniquefollowingcompleteavulsionofthebrachialplexus.
Indicationsandlong-termresults.JBoneJointSurgAm.
2000;82(5):652–66.
20.TerzisJK,VekrisMD,SoucacosPN.Outcomesofbrachial
plexusreconstructionin204patientswithdevastating
paralysis.PlastReconstrSurg.1999;104(5):1221–40.
21.KretschmerT,IhleS,AntoniadisG,SeidelJA,HeinenC,Börm
W,etal.Patientsatisfactionanddisabilityafterbrachial
plexussurgery.Neurosurgery.2009;654Suppl.:A189–96.
22.CiaramitaroP,MondelliM,LogulloF,GrimaldiS,BattistonB,
SardA,etal.Traumaticperipheralnerveinjuries:
epidemiologicalfindings,neuropathicpain,andqualityoflife
in158patients.JPeripherNervSyst.2010;15(2):120–7.
23.MerrellGA,BarrieKA,KatzDL,WolfeSW.Resultsofnerve
transfertechniquesforrestorationofshoulderandelbow
functioninthecontextofameta-analysisoftheEnglish
literature.JHandSurgAm.2001;26(2):303–14.
24.ChuangDC,LeeGW,HashemF,WeiFC.Restorationof
shoulderabductionbynervetransferinavulsedbrachial
plexusinjury:evaluationof99patientswithvariousnerve
transfers.PlastReconstrSurg.1995;96(1):122–8.
25.TerzisJK,KostasI.Muscletargetresponsivenessto718
intercostalnerveneurotizationsinsevereposttraumatic
brachialplexuslesions.PlastReconstrSurg.2008;110:615.
26.BengtsonKA,SpinnerRJ,BishopAT,KaufmanKR,
Coleman-WoodK,KircherMF,etal.Measuringoutcomesin
adultbrachialplexusreconstruction.HandClin.
2008;24(4):401–15.
27.ChoiPD,NovakCB,MackinnonSE,KlineDG.Qualityoflife
andfunctionaloutcomefollowingbrachialplexusinjury.J
HandSurgAm.1997;22(4):605–12.
28.KitajimaI,DoiK,HattoriY,TakkaS,EstrellaE.Evaluationof
qualityoflifeinbrachialplexusinjurypatientsafter
reconstructivesurgery.HandSurg.2006;11(3):103–7.
29.Ahmed-LabibM,GolanJD,JacquesL.Functionaloutcomeof
brachialplexusreconstructionaftertrauma.Neurosurgery.
2007;61(5):1016–22.
30.FleckMP,LouzadaS,XavierM,ChachamovichE,VieiraG,
SantosL,etal.ApplicationofthePortugueseversionofthe
abbreviatedinstrumentofqualitylifeWHOQOL-bref.Rev