Work performed in the Multidisciplinary Residency Program in Health, Emergency Department concentration area, Clinical Hospital, Universidade Federal de Goiás – UFG – Goiânia (GO), Brazil.
(1) Multidisciplinary Residency Program in Health, Emergency Department concentration area, Clinical Hospital, Universidade Federal de Goiás – UFG – Goiânia (GO), Brazil.
Conflict of interests: No
Author’s contribution: FKCF principal researcher, development of research, development of schedule, literature review, data collection and analysis, writing and editing the article, article submission and procedures; PACN literature review, data collection and analysis; ALI guidance, developing research, editing the article; PMLF co-guidance, editing the article.
Correspondence address: Karla Cristina Freitas Faria. R. Anita Garibalde, 459, Centro, Nerópolis, Goiás (GO), Brazil, CEP: 75460-000. Email: fga-karlacff@hotmail.com
Received: 3/1/2013, Accepted: 9/11/2013
The profile of a patient receiving speech-language
therapy assistance at a school hospital emergency unit
Perfil do paciente atendido pela fonoaudiologia na unidade de
urgência e emergência de um hospital universitário
Karla Cristina Freitas Faria1, Ana Cláudia Neres Pessoa1, Lúcia Inês Araújo1, Maria Luíza de Faria Paiva1
ABSTRACT
Purpose: This paper sought to evaluate patients receiving assistance from resident speech-language therapists at a school hospital emergency room. Methods: Both adult and elderly patients were included in this study. In total, 150 individuals of both genders, including adults between the ages of 20-59 years and elderly individuals over 60 years of age, who were hospitalized from March 2010 to March 2012 were studied. Results: The patients were predominantly male and elderly, with in-complete elementary school education and a low income, and originated from the capital city and metropolitan region. The medical diagnoses predominantly revealed circulatory diseases, digestive disorders, and ner-vous system disorders. The speech-language therapy diagnoses showed normal swallowing function, neurogenic oropharyngeal dysphagia, and esophageal dysphagia. Conclusion: The prevalence of age-related sys-temic disorders may lead to swallowing disorders, which could trigger complications such as longer hospital stays. Therefore, the presence of a speech-language therapist in an emergency room is important to assess, diagnose, and treat swallowing disorders.
Keywords: Dysphagia; Adult; Aged; Emergency Treatment; Speech, Language and Hearing Sciences
RESUMO
Objetivo: Caracterizar a população atendida pelos residentes de Fono-audiologia no pronto-socorro de um hospital universitário. Métodos: A amostra foi composta por 150 sujeitos de ambos os gêneros, na faixa etária de 20 anos a 59 anos e acima de 60 anos, internados no período de março de 2010 a março de 2012. Resultados: Houve predominância de pacientes do gênero masculino, idosos, com ensino fundamental incompleto e com baixa renda, procedentes, em sua maioria, da capital, Goiânia, e região metropolitana. No diagnóstico médico, predominaram as doenças do aparelho circulatório, doenças do aparelho digestivo e do-enças do sistema nervoso. Os diagnósticos fonoaudiológicos encontrados foram: deglutição normal/funcional, disfagia orofaríngea neurogênica e disfagia esofágica. Conclusão: Faixa etária associada a doenças de base prevalentes pode levar a distúrbios da deglutição, podendo agravar o quadro e prolongar o período de permanência do sujeito na instituição, sendo de extrema importância a presença do fonoaudiólogo nos serviços de urgência e emergência, para avaliar, diagnosticar e tratar os distúrbios deglutitórios.
INTRODUCTION
One of the most concise and current definitions of speech--language therapy is a segment of the healthcare field that in-cludes individual and collective actions aimed at the promotion, protection, and recovery of health aspects involved in language, voice, hearing, and orofacial motricity(1).
As the speech-therapy field expands, new specializations have emerged, of which dysphagia is one of the most recent. This specialization is regulated by Resolution No. 356 of 12/6/2008, which “provides for the technical and legal compe-tence of speech-language therapists to work in oropharyngeal dysphagia”(2). Dysphagia is a swallowing disorder that affects the entire digestive tract running from the mouth to the stomach, or parts thereof(3).
Swallowing consists of three stages: oral, pharyngeal and esophageal. Changes that occur in the first two stages can cause oropharyngeal dysphagia, whereas alterations to the last phase lead to esophageal dysphagia. From an etiological point of view, dysphagia can be classified as neurogenic when
caused by any condition of the central and/or peripheral ner-vous system or mechanical when triggered by any anatomical
origin(4). In terms of severity, dysphagia can be classified as mild, moderate, or severe(5).
Speech-language therapy for the treatment of patients with dysphagia occurs mainly in the hospital. This approach has also gained prominence due to the significant increase in chronic noncommunicable diseases (NCDs), such as cancer, respiratory diseases, diabetes, and cardiovascular diseases, which can cause changes in swallowing. The Ministry of Health (Ministério da Saúde - MS) reports that according to the World Health Organization (WHO), NCDs are responsible for 45.9% of the global disease burden. In Brazil, these diseases represent 75% of health care spending in the National Health System (Sistema Único de Saúde - SUS)(6).
The contributions of speech-language therapy in this con-text occur during the assessment, diagnosis, and intervention of patients with dysphagia, with the aim of preventing and/or minimizing potential clinical complications(7-9).
Dysphagia is also associated with an increased risk of pulmonary conditions due to aspiration of saliva and/or food, malnourishment, dehydration, prolonged hospitalization, and death. Moreover, this condition also involves numerous psycho-social and economic-financial factors(10-14).
The speech-language therapist is not the only professional who works in the area of dysphagia, and the effectiveness of therapeutic interventions depends on the contribution of other professionals, such as physicians with various specializations, nutritionists, psychologists, and other specialists(7,15,16). This type of multidisciplinary approach has been increasingly ap-plied for all types of health services, including emergency care units, which are based on the structuring of multidisciplinary residency programs. In addition to optimizing patient care, the
presence of several professionals from different fields has also been shown to be beneficial from a cost/benefit perspective(17,18).
However, the speech-language therapist is the professional trained to evaluate swallowing function at an early stage and establish the safest method of feeding. Because emergency units are responsible for providing initial patient care, emergency rooms (ERs) should include speech-language therapists due to the significant demands of dysphagic patients(19,20).
This study sought to characterize the population served by speech-language therapy residents in the ER at the Clinical Hospital of the Federal University of Goiás (HC/UFG) between march 2010 and march 2012.
METHODS
This retrospective cross-sectional study was approved by the Research Ethics Committee of Universidade Federal de Goiás (UFG), under protocol number 078/2011. This study was part of the research project entitled “Characterization of care provided in HC/UFG”. A signature for consent was not required because no direct contact with patients was made. Moreover, the patients were not identified, and the study did not cause them any moral or material harm.
Literature reviews were performed on relevant topics using search tools such as the Virtual Health Library (VHL) and Scientific Electronic Library Online (SciELO), queries to the book of records of the HC/UFG speech-language therapy ser-vice and searching patients’ records using the form previously developed by the researchers (Appendix 1).
The speech-language therapy service of this hospital only provides bed consultations when receiving a request from the medical and/or multidisciplinary team. After implementation of the Multidisciplinary Health Residency along with the participation of speech-language therapy professionals, this service began enrolling patients by screening for the risk of dysphagia and performing a swallowing evaluation after me-dical clearance.
The study included adult and elderly patients of both gen-ders (adults 20-59 years and elderly individuals over 60 years), according to the classification used by the MS in vaccination schedules(21). These patients were admitted to the ER of the HC/UFG and were attended by speech-language therapy resi-dents from march 2010 to march 2012.
Patients whose records were not found or were incomplete regarding the variables adopted for the study were excluded. This reduced the total sample from the initial 307 participants to 150 subjects.
evaluations performed. Data collection started on 08/06/2012 and finished on 10/11/2012.
A total of 93 of the 150 participants (62%) were male and 57 (38%) were female. Of these subjects, 80 (53.3%) came from Goiânia or its metropolitan region, 66 (44%) from the interior, and only 4 (2.7%) from other states.
The majority of patients (85, 56.7%) were elderly, and 65 (43.3%) were adults (20-59 years).
RESULTS
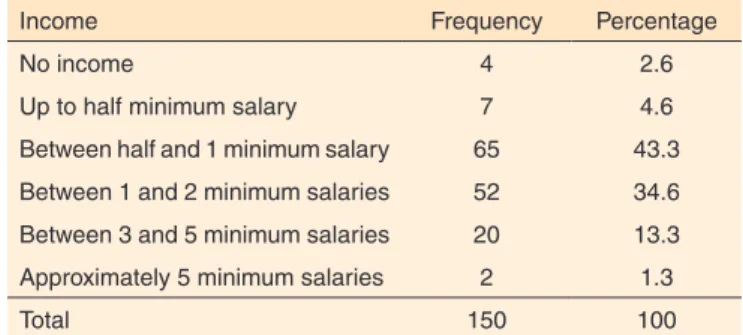
The socioeconomic data indicated a patient profile consis-ting of low education, low income, and dependency on social security benefits (Tables 1, 2, 3).
The medical diagnoses that appeared most frequently in-cluded circulatory diseases (19%), digestive diseases (16%), and nervous system disorders (14%) (Figures 1, 2).
It is important to note that of the 150 participants, 97 (64.7%) had 2 medical diagnoses, 43 (28.7%) had 3 diagnoses,
8 (5.3%) had 4 diagnoses, and 1 (7%) had 5 diagnoses. Regarding the type of access among the 150 patients treated, 129 (86%) were spontaneous addressed by speech-language therapy residents at the time of admission into the ER, 14 (9.3%) were referred by doctors, and only 7 (4.7%), were referred by other health care providers (Figure 3).
According to the records of the speech-language therapy service, 563 consultations made by residents were recorded for the sample of 150 patients; of these, 205 were assessments, and 358 were treatments. This result indicates a mean of 1.3 assessments and 2.3 treatments per patient.
The main speech-language therapy diagnoses made during the studied period included normal swallowing function (44%), neurogenic oropharyngeal dysphagia (29.3%), and esophageal dysphagia (24.6%) (Figure 4).
DISCUSSION
The data obtained concerning the prevalence of oropha-ryngeal dysphagia in patients with cardiovascular diseases and esophageal dysphagia in patients with diseases of the digestive tract (Figure 2) are in agreement with a survey conducted in 2009 in a hospital in Pernambuco. This previous study reported that changes in the swallowing function of elderly individuals, even in the absence of neurological changes, may result from
Table 1. Education
Education Frequency Percentage
Illiterate 53 35.3
Incomplete elementary school 71 47.3
Complete elementary school 5 3.3
Incomplete high school 7 4.6
Complete high school 12 8
Incomplete higher education 0 0
Complete higher education 2 1.3
Total 150 100
Table 2. Income
Income Frequency Percentage
No income 4 2.6
Up to half minimum salary 7 4.6
Between half and 1 minimum salary 65 43.3
Between 1 and 2 minimum salaries 52 34.6
Between 3 and 5 minimum salaries 20 13.3
Approximately 5 minimum salaries 2 1.3
Total 150 100
Table 3. Employment situation
Employment situation Frequency Percentage
Employed 9 6
Unemployed 11 7.3
Self-employed 16 10.6
Receiving pension 100 66.6
Not applicable 14 9.3
Total 150 100
Figure 1. Medical diagnoses divided into groups, with the sample number shown absolute numbers (CID 10)
aging of the phono-articulatory organs(23). These changes are mainly related to the oropharyngeal phase of swallowing and can be explained in detail by the literature focused on orofacial motricity(3,4).
The 20 patients with nervous system disease who presen-ted with oropharyngeal dysphagia corroborapresen-ted the results of studies in patients with compromised neurological function showing a prevalence rate of 50% for this type of dysphagia with the occurrence of episodes of stroke (CVA)(8,9).
Regarding the prevalence of esophageal dysphagia and its relationship with digestive tract diseases, the literature shows that this type of alteration is common in several diseases such as chagasic megaesophagus and Zenker diverticulum(24).
The high prevalence of dysphagia identified in this sample and in other studies emphasizes the importance of the partici-pation of speech-language therapy professionals in structuring a care network for patients with dysphagia. Moreover, this type of care should range from evaluation in the ER to home care, especially with regard to elderly patients(16).
According to the Brazilian Institute of Geography and Statistics (Instituto Brasileiro de Geografia e Estatísticas - IBGE), there are more than 20 million seniors in Brazil; in other words, approximately 8.6% of the population is aged 60 years or over. According to the MS, circulatory system diseases most com-monly affect this age group, representing 37% of deaths among elderly patients(25). These data were confirmed in the present study, as 56.7% of the studied patients were elderly. In addition, we found that the most common medical diagnosis for these patients was cardiovascular disease (19%), followed by diseases of the digestive tract (16%) and nervous system diseases (14%).
The socioeconomic profile of the patients in this study revealed that most had a low level of education (47.3%), low income (43.3%), and depended on pension benefits (66.6%). These results are in agreement with a survey conducted in 2011 in Fortaleza - Ceará, which reported a similar profile of elderly subjects registered in the city’s primary health care network(26).
In the United States, a study published in 2009 showed that during the period from 1996 to 2005, there was an increase in the number of emergency service users (from 12.7% to 13.8%), and the majority of these patients were elderly(27). However, no other studies with similar characteristics were found in the searched databases, precluding further comparison.
A study conducted in 2011 revealed that of the 20,390 spe-ech-language therapists registered with the National Register of Health Facilities (Cadastro Nacional de Estabelecimentos de Saúde - CNES), only 0.34% offered this type of service. According to the authors, from 2005 to 2011, there was an increase in speech-language therapists working in emergency units, especially after the creation of multidisciplinary residency programs in health, although the number of professionals re-mained insufficient to meet the current demands(28).
Another important finding of this study was the significant increase in the number of speech-language therapy consulta-tions made in ERs during periods in which there were perma-nent speech-language therapy residents on site. Prior to the onset of multi-professional residency programs, consultations only took place following referrals from doctors (Figure 3).
However, the retrospective nature of this study limited our ability to collect information, and it was also not possible to draw further comparisons to data from other studies due to the scarcity of publications on this subject.
CONCLUSION
The association between advanced age and prevalent un-derlying disease may lead to dysphagia, which can aggravate the clinical picture of patients and extend their period of hos-pitalization. Thus, the presence of speech-language therapists is extremely important in ERs to assess, diagnose, and treat swallowing disorders.
Figure 4. Speech-therapy diagnoses made by residents
This study showed that over 50% of the population treated in the HC/UFG ER presented dysphagia or risks for develo-ping this disorder, suggesting that this trend may also occur throughout the country.
Based on these findings, the multidisciplinary team should initiate and develop care plans and subsequently address treat-ment continuity or referral to other health institutions.
REFERENCES
1. Lessa F, Ferrite MTPCS.Fonoaudiologia e Epidemiologia. In Fernandes FDM, Mendes BCA, Navas ALPGP (Org.). Tratado de Fonoaudiologia. 2a. ed. São Paulo: Roca; 2010. p. 34-44.
2. Brasil. Diário Oficial Imprensa Nacional nº. 239 - DOU de 09/12/08, p. 163. Conselho Federal de Fonoaudiologia. Resolução nº 356, de 6 de dezembro de 2008. [Internet] [citado 2012 Nov. 20]. Disponível em: ftp://ftp.saude.sp.gov.br/ftpsessp/bibliote/informe_ eletronico/2008/iels.dez.08/iels234/U_RS-CFFa-356_061208.pdf 3. Rofes L, Arreola V, Almirall J, Cabré M, Campins L, García-Peris P,
et al. Diagnosis and management of oropharyngeal dysphagia and Its nutritional and respiratory complications in the elderly. Gastroenterol Res Pract. 2011;2011:1-14.
4. Prodomo LPV, Angelis EC, Barros ANP. Avaliação clínica fonoaudiológica das disfagias. In: Jotz GP, Angelis EC, Barros APB. Tratado da deglutição e disfagia: no adulto e na criança. Rio de Janeiro: Revinter; 2010. p. 61-7.
5. Souza BBA, Martins C, Campos DJ, Balsini ID, Meyer LR. Nutrição e disfagia: guia para profissionais. Curitiba: Nutroclínica; 2003. p. 17-22.
6. Portal da Saúde. Sistema Único de Saúde. [Internet] [citado 2012 Nov. 20]. Disponível em: http://portal.saude.gov.br/portal/saude/ profissional/visualizar_texto.cfm?idtxt=31877
7. Silvério CC, Hernandez AM, Gonçalves MIR. Ingesta oral do paciente hospitalizado com disfagia orofaríngea neurogênica. Rev CEFAC. 2010;12(6):964-70.
8. Moraes DP, Andrade CRF. Indicadores de qualidade para o gerenciamento da disfagia em Unidades de Internação Hospitalar. J Soc Bras Fonoaudiol. 2011;23(1):89-94.
9. Lawrence ES, Coshall C, Dundas R, Stewart J, Rudd AG, Howard R, et al. Estimates of the prevalence of acute stroke impairments and disability in a multiethnic population. Stroke. 2001;32(6):1279-84. 10. Kröger E, Tourigny A, Morin D, Côté L, Kergoat MJ, Lebel P,
et al. Selecting process quality indicators for the integrated care of vulnerable older adults affected by cognitive impairment or dementia. BMC Health Serv Res. 2007;7:195.
11. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnostic and pulmonary complications. Stroke. 2005;36(12):2756-63.
12. Geeganage C, Beavan J, Ellender S, Bath PM. Interventions for dysphagia and nutritional support in acute and subacute stroke. Cochrane Database Syst Rev. 2012;10:13p.
13. Baroni AF, Fabio SR, Dantas RO. Risk factors for sawallowing dysfunction in stroke patients. Arq Gastroentrol. 2012;49(2):118-24. 14. Ashley J, Duggan M, Suticliffe N. Speech, language, and swallowing
disorders in the older adult. Clin Geriatr Med. 2006;22(2):291-310. 15. Abdulmassih EMS, Macedo Filho ED, Santos RS, Jurkiewicz
AL. Evolução de pacientes com disfagia orofaríngea em ambiente hospitalar. Arq Int Otorrinolaringol. 2009;13(1):55-62.
16. Farneti D, Consolmagno P. The Swallowing Centre: rationale for a multidisciplinary management. Acta Otorhinolaryngol Ital. 2007;27(4):200-7.
17. Saar SRC, Trevizan MA. Papéis profissionais de uma equipe de saúde: visão de seus integrantes. Rev Latino-Am Enfermagem. 2007;1(15):106-12.
18. Santoro PP, Furia CLB, Forte AP, Lemos EM, Garcia RI, Tavares RA, et al. Otolaryngology and speech therapy evaluation in the assessment of oropharyngeal dysphagia: a combined protocol proposal. Braz J Otorhinolaryngol. 2011;77(2):201-13.
19. Marques CHD, André C, Rosso ALZ. Disfagia no AVE agudo: revisão sistemática sobre métodos de avaliação. Acta Fisiátrica. 2008;15(2):106-10.
20. Itaquy RB, Favero SR, Ribeiro MC, Barea LM, Almeida ST, Mancopes R. Disfagia e acidente vascular cerebral: relação entre o grau de severidade e o nível de comprometimento neurológico. J Soc Bras Fonoaudiol. 2011;23(4):385-9.
21. Brasil. Ministério da Saúde. Portaria nº 3.318, de 28 de outubro de 2010. [Internet] [citado 2012 Nov. 20]. Disponível em: http://bvsms. saude.gov.br/bvs/saudelegis/gm/2010/prt3318_28_10_2010.html. 22. Organização Mundial da Saúde. CID-10 Classificação Estatística
Internacional de Doenças e Problemas Relacionados à Saúde. 10ª. rev. São Paulo: Universidade de São Paulo; 1997. vol.1.
23. Lima RMF, Amaral AKFJ, Aroucha EBL, Vasconcelos TMJ, Silva HJ, Cunha DA. Adaptações na mastigação, deglutição e fonoarticulação em idosos de instituição de longa permanência. Rev CEFAC. 2009;11(3):405-22.
24. Nascimento WV, Cassiani RA, Dantas RO. Disfagia em pacientes com doença de Chagas e divertículo de Zenker. Rev Soc Bras Fonoaudiol. 2010;15(2):277-81.
25. Portal Brasil. Sistema Único de Saúde. País investe em prevenção a doenças da terceira idade. [citado 2012 Nov. 20] Disponível em: http://www.brasil.gov.br/saude/2012/04/pais-investe-em-prevencao-a-doencas-da-terceira-idade.
26. Clares JWB, Freitas MC, Almeida PC, Galiza FT, Queiroz TA. Perfil de idosos cadastrados numa Unidade Básica de Saúde da Família de Fortaleza-CE. Rev Rene. 2011;12(n.esp.):988-94.
27. Xu TK, Nelson BK, Berk S. The changing profile of patients who used emergency department services in the United States: 1996 to 2005. Ann Emerg Med. 2009;54(6):805-10.
Appendix 1. Patient profile treated by speech-language therapy in the emergency unit of a university hospital
Form number ______ Date: ___/___/_____
Sociodemographic data
Record number:
Age range: 1. ( ) Adult 2. ( ) Elderly
Gender: 1. ( ) female 2. ( ) Male
Origin
1. ( ) Goiânia and metropolitan region 2. ( ) Goiás (interior)
3. ( ) Other state
Income 1. ( ) No income
2. ( ) Up to half a minimum salary 3. ( ) Between half and 1 minimum salary 4. ( ) Between 1 and 2 minimum salaries 5. ( ) Between 3 and 5 minimum salaries 6. ( ) Above 5 minimum salaries
Education 1. ( ) Illiterate
2. ( ) Incomplete elementary school 3. ( ) Complete elementary school 4. ( ) Incomplete high school 5. ( ) Complete high school 6. ( ) Incomplete higher education 7. ( ) Complete higher education
Diseases found
1. ( ) Infectious and parasitic diseases 2. ( ) Neoplasias
3. ( ) Blood and hematopoietic organ diseases 4. ( ) Endocrine, nutritional and metabolic diseases 5. ( ) Mental and behavioral disorders
6. ( ) Nervous system diseases
7. ( ) Hearing diseases and mastoid apophysis 8. ( ) Circulatory system diseases
9. ( ) Respiratory system diseases 10. ( ) Digestive system diseases
11. ( ) Musculoskeletal system and connective tissue diseases 12. ( ) Genitourinary diseases
13. ( ) Injuries, poisoning and other external causes 14. ( ) Others
Access to patient 1. ( ) Spontaneous 2. ( ) Via doctor referral
3. ( ) Via referral from other professional
Speech-language therapy diagnosis 1. ( ) Normal/functional swallowing 2. ( ) Neurogenic oropharyngeal dysphagia 3. ( ) Mechanical oropharyngeal dysphagia 4. ( ) Esophageal dysphagia