SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Original
article
Factors
associated
with
mortality
among
elderly
people
hospitalized
due
to
femoral
fractures
夽
Léo
Graciolli
Franco
∗,
Amanda
Loffi
Kindermann,
Lucas
Tramujas,
Kelser
de
Souza
Kock
UniversidadedoSuldeSantaCatarina,HospitalNossaSenhoradaConceic¸ão,Tubarão,SC,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received29September2015 Accepted15October2015 Availableonline17August2016
Keywords:
Femoralfractures Elderly
Hospitalmortality Survivalanalysis
a
b
s
t
r
a
c
t
Objective:Toanalyzefactorsassociatedwithmortalityamongelderlypeoplehospitalizedin asingle-centerregionalhospitalduetofemoralfractures.
Methods:Thiswasaretrospectivecohortstudy.Patientsaged60yearsoroverwhowere hospitalizedwithadiagnosisoffemoralfracture(ICDS72)between2008and2013were selectedthroughtheelectronicmedicalrecords.
Results:The study evaluated 195individualsof meanage 78.5±9.6years; females pre-dominated(68.2%). Themainmechanismforfallswaslow-energy(87.2%).Surgerywas performedon93.3%ofthepatients;themeanlengthofhospitalstaywas13.6±7.5days andthemeanwaitingtimeforthesurgerywas7.7±4.2days.Theprevalenceof mortal-itywas14.4%,andthisoccurredmostlyamongolderindividuals(p=0.029);patientswith leukocytosis(p<0.001);thosewhoneededintensivecare(p<0.001);andthosewhodidnot undergosurgery(p<0.001).Themeansurvivalwassignificantlylongeramongpatientswho underwentsurgeryandshorteramongthosewhoneededintensivecare.
Conclusion: Womenpredominatedamongthehospitalizations,andthedegreeof leukocy-tosisassociatedwithadvancedagepresentedarelationshipwithmortality,independentof thetypeoflesionorsurgicalprocedure.Morestudiesstillneedtobeconductedinorderto assessotherfactorsassociatedwithmortality.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Fatores
associados
à
mortalidade
em
idosos
hospitalizados
por
fraturas
de
fêmur
Palavras-chave:
Fraturasdofêmur Idoso
Mortalidadehospitalar Análisedesobrevida
r
e
s
u
m
o
Objetivo:Analisarosfatoresassociadosàmortalidadeemidososhospitalizadosporfratura defêmuremumhospitalunicêntricoregional.
Métodos:Estudo de coorte retrospectiva. Foram selecionados, por meio do prontuário eletrônico,pacientesinternadoscomdiagnósticodefraturadefêmur(CIDS72)com60anos oumaisde2008a2013.
夽
StudyconductedattheHospitalNossaSenhoradaConceic¸ão,Tubarão,SC,Brazil. ∗ Correspondingauthor.
E-mail:leosarandi@hotmail.com(L.G.Franco). http://dx.doi.org/10.1016/j.rboe.2016.08.006
Resultados: Foramavaliados195indivíduoscomidademédiade78,5±9,6eogênero fem-ininofoimaisprevalente(68,2%).Oprincipalmecanismodequedafoiodebaixaenergia (87,2%),afeituradecirurgiafoide93,3%,otempodeinternac¸ãomédiofoide13,6±7,5dias, otempodeesperaparaacirurgiamédiofoide7,7±4,2dias.Aprevalênciademortalidade foide14,4%,ocorreuprincipalmentenosindivíduosmaisidosos(p=0,029),comleucocitose (p<0,001),comnecessidadedecuidadosintensivos(p<0,001)equenãoforamsubmetidos acirurgia(p<0,001).Asobrevidamédiafoisignificativamentemaiornospacientes sub-metidosacirurgiaeinversamentenospacientesquenecessitaramdaunidadedeterapia intensiva.
Conclusão: Asmulherespredominaramnasinternac¸õeseograudeleucocitoseassociado aidadeavanc¸adaapresentourelac¸ãocomamortalidade,independentementedotipode lesãoeprocedimentocirúrgico.Aindadevemserfeitosmaisestudosparaavaliaroutros fatoresassociadosàmortalidade.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
TheWorld Health Organization(WHO) classifies aselderly every individual aged 60 years or more.1 This population
samplepresents anacceleratedincreasingpercentagerate, generatinganincreaseintheprevalenceofchronic degener-ativediseases.2
AccordingtoMonteiro,fallsoftheelderly–inadditionto theinjuryitself–arealsodamagingthefamily,astheycreate adependencyduetothelossofautonomyafterthetrauma event,representinganimportantsocial,economic,andpublic healthissue.3Itisestimatedthatthenumberofhipfractures
worldwidewillreach4.5millioncasesin2050.4
Themainfactorsassociatedwithmortalityafterfracture areage, comorbidities,cognitive status,timebetween frac-tureand surgery,and typeofanesthesia used.5–8 However,
the association of time until surgery and risk of death is controversial. The literatureindicates that there is a rela-tionshipbetweentimeuntilsurgeryandmortality.9Altered
laboratorybloodexamssuchasleukocytelevels,whichmay present as a associated factor with death, have also been widelyaddressed.10
From this perspective, the data presented herein is expectedtoleadtoabetterunderstandingofthis problem andcontributetoabettercareofelderlypatientswithfemoral fracture.Therefore,thisstudyaimedtoevaluatethe associ-atedfactorswithmortalityinelderlypatientswithhipfracture duringhospitalization.
Material
and
methods
Thepresentstudy wasaretrospectivecohortof275elderly patients who had femoral fractures from January 2008 to December2013andwereadmittedtoasingle-center,regional referencehospital.
For sample selection, the medical patient record ofthe institutionwascontactedinordertostratifyindividuals hos-pitalizedwithadiagnosisoffemoralfracture(ICD-10S72),who wereolderthanorequalto60yearsintheproposedperiod.
The exclusion criteria comprised incomplete data on the medical charts, misdiagnosis at hospitalization, trans-fer to other hospitals, and re-admissions. The study was approved by the Research Ethics Committee under No. 34735814.2.0000.5369.
Thefollowingvariableswerecollected:gender,age, comor-bidities, type and side of fracture, type of fall, surgical treatment, typeof surgeryand timeuntil surgery,hospital lengthofstay,needforintensivecaretreatment,hematocrit andleukocytesinthefirstweekofhospitalization,and out-come,describedasdischargeordeath.
An anatomicalsubdivision wasused toclassifyfemoral fractureregions.Theproximalpartofthefemurcomprisesthe intracapsularandextracapsularfractures;thejointcapsuleis usedasareference.Inturn,theintermediateportion corre-spondstothefemoralshaft;thefinalsubdivisionconsistsof fracturesofthedistalpartofthefemur.11
DatawerestoredinanExcelspreadsheetandthen trans-ferredtotheSPSS20.0softwareforanalysis.Numerical vari-ableswerepresentedascentraltendencyanddispersion,and categoricalvariablesasabsolutefrequenciesandpercentages. Numerical variables were analyzed using the Kolmogorov–Smirnov normality test. To compare these variables with the outcome, Student’s t-test (p<0.05) was used for data with normaldistribution; for nonparametric variables, the Mann–Whitney test was used (p<0.05). For results with significant difference, accuracy was assessed throughtheareaundertheROCcurve.
For comparison amonggender, ICU hospitalization, and performance of surgery, the chi-squared test was used (p<0.05).Therelativerisksofdeath,withtheirrespective95% confidenceintervals,werecalculated.
Thesurvivalrateofpatientswhorequiredintensivecare and underwent surgerywasanalyzed usingCox regression (p<0.05)andpresentedthroughKaplan–Meiercurves.
Results
Table1–Characteristicsoftheelderlypatients
hospitalizedforhipfracture.
Variables n(%)
Gender
Female 133(68.2)
Male 62(31.8)
Agea(years) 78.5±9.6
Typesoffracture
Intracapsular 79(40.5)
Extracapsular 96(49.2)
Diaphysis 12(6.1)
Distalfemur 4(2.1)
Notreported 4(2.1)
Sideofthefracture
R 91(46.7)
L 100(51.3)
RandL 1(0.5)
Notreported 3(1.5)
Typeoffall
Low-energy 170(87.2)
High-energy 7(3.6)
Notreported 18(9.2)
Surgery
Yes 182(96.3)
No 13(6.7)
Typeofsurgery
Osteosynthesis 95(48.7)
Totalarthroplasty 44(22.6)
Partialarthroplasty 26(13.3)
Othersb 30(15.4)
Waitingtimeuntilsurgery 7.7±4.2 Waitingtimeuntilsurgery(days) 13.6±7.5 Hematocritatadmissiona(days) 33.5±5.7 Leukocytesatadmissiona(mm2) 8922±5972.6
Comorbidities
Systemichypertension 90(46.2)
Diabetesmellitus 43(23.6)
Cardiacdiseases 41(21.0)
Others 21(9.2)
Outcome
Death 28(14.4)
a Mean±standard-deviation.
b Didnotundergosurgery,typeofprocedurenotreported,bipolar
arthroplasty,Ilizarov.Heartfailure,chronicrenalfailure,tumor, COPD,stroke,dementia,hypothyroidism,hearingloss,arthritis.
records,aswellasadmissionswithoutactualfractures,with consequentdischarge,transfers,orre-admissions.Therefore, asampleof195patientswasobtained.Table1describes pop-ulationcharacteristics.
Table2showsthecomparisonbetweentimeuntilsurgery andhospitalization,andhematocritandleukocytecountat admission, forboth discharge and deathgroups. A signifi-cantdifferencewasobservedonlyregardingageandleukocyte count.
Intheanalysisofthenumericalvariablesthatpresented significantdifferencebetweendischargeanddeathfromthe perspectiveofthe ROCcurve,theaccuracyfordeath prog-nosisobtainedbythe areaunderthe curvewas0.761(95%
1.0
0.8
0.6
0.4
0.0 0.2 0.4 0.6
1 - Specificity
Sensitivity
0.8 Leukocytes Age Reference line
1.0 0.2
0.0
Fig.1–ROCcurveofage,whitebloodcells,anddeath prognosis.
CI:0.664–0.859), p<0.001for leukocytes,and 0.643 (95%CI: 0.525–0.762),p<0.023forage(Fig.1).
In the comparison of outcome and gender, no signifi-cantdifferencewasobserved:16.2%malesand13.5%females (p<0.630).However,individualsrequiringICUadmission pre-sented a relative risk of death of 10 (95% CI: 4.1–24.4); non-performanceofsurgeryshowedarelativeriskof30.4(95% CI:7.6–120.6),bothwithstatisticalsignificance(p<0.001).
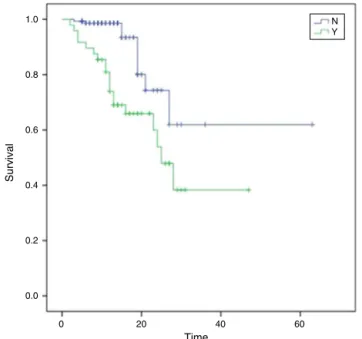
ThemeansurvivalofpatientshospitalizedintheICUwas 28.2 days(95%CI:22.1–34.4);forthosewho didnotrequire ICU admission,47 days(95% CI:36.5–57.5),with significant difference(p<0.001)(Fig.2).
Themeansurvivalofpatientswhodidnotreceivesurgery was 11.7 days (95%CI:7.9–15.5); forthose who underwent surgery,itwas45.8days(95%CI:37.9–53.8),withsignificant difference(p<0.001)(Fig.3).
Discussion
Regardinggender,thepresentstudyobservedahighernumber ofwomenwhohadsufferedfemoralfracture.Thisfindingis similartothatofaretrospectivestudyintheLazioregion,with 6896patients,inwhich78%oftheelderlypatientsadmitted withfemoralfracturewerefemales.12
Regarding typeoffractures,ahigherincidenceof extra-capsular fractures was observed when compared with intracapsularfractures.Thisdataiscorroboratedbya retro-spectivestudyof1911elderlypatientswithfemoralfractures thatobservedsimilarprevalence.13
Asforthedynamicsoftrauma,thisstudyshowedahigh prevalenceoflow-energytrauma.Thisfindingisjustifiedby thecharacteristicsofthesample,whichwascomprised pri-marily ofelderly patients. Moraeset al.14 stated that such
Table2–Comparisonofthenumericalvariablesaccordingtotheoutcomeofdeath.
Discharge Death p-Value
n=167 n=28
85.60% 14.40%
Agea(years) 78±9.5 82.1±9.8 0.029c
Timeuntilsurgerya(days) 7.5±4.0 9.44±5.1 0.105
Hospitallengthofstaya(days) 13.6±7.5 13.6±7.7 0.811
Hematocritb(%) 33.4±5.7 31.2±5.5 0.06
Leukocytesa(/mm2) 8323.3±4645.9 13,037.9±10,836.4 <0.001c
a Mann–Whitneytest.
b Student’st-test.
c p-Value<0.05.
years and ismostlikely tooccur infemales,which would explainthegreaterexposureofwomentofemoralfractures.
In the analysis of survival curve and comparison of individuals with or without surgical indication, a signifi-cantdifferencewasobservedbetweenthesegroups;survival ratewassignificantlyhigherinindividualswho underwent surgery.Rocheet al.15 concludedthat thegreatestrisk
fac-torformortalitywasdirectlyrelatedtothepresenceofthree ormorecomorbiditiesevaluatedpreoperatively.Incontrast, anotherstudyshowedthat,forpatientswithoutclinical condi-tionsforsurgery,notperformingsurgerywasthebestchoice, and there was no significant difference in functional out-come and mortalitywhen compared with patients treated surgically.16Althoughthepresentstudydidnotcompare
mor-talitywithmorbidities,itcanbededucedthattheearlydeath observedisrelatedtothenumberofcomorbiditiesinthese patients.
Regardingtypeofprocedure,osteosynthesisandtotalor partialarthroplasty were the most frequentchoices. How-ever,surgicalapproachhadnosignificantrelationshipwith recoverytime, nor with death.A Norwegianstudy of4335 elderlypatientscomparedosteosynthesiswitharthroplasty inthetreatment offemoralneckfracture andobservedno
1.0
0.8
0.6
0.4
0.2
0.0
0 20 40
Time
Survival
60 N Y
Fig.2–Survivalinpatientswhowereorwerenotadmitted totheICU.
differencesinmortalityratesoneyearaftersurgery.Thissame studyfoundthatpatientsundergoingosteosynthesisreported higherpainlevels,greaterdissatisfactionwiththeresultsof surgery,andlowerqualityoflifethanthearthroplastygroup.17
Regardingwaitingtimeuntilsurgery,therewasno signif-icant differencebetweendischargeand deathoutcomesfor thesepatients.Althoughtheliteratureisquitecontroversial,9
accordingtoGrimesetal.,18timebetweentraumaandsurgery
appearstoinfluencemortalityinelderlypatientswithfemoral fractures.Inastudyof8383subjects,patientswere divided into threegroups:firstgroupwereoperatedwithinthefirst 24hoursafterfracture;secondgroup,after24hoursof frac-ture, but without activedisease; and third groupwas also operated after24hours, but withactivepathology.Patients withactivediseasehadtheirsurgerypostponedduetothe presenceofdecompensateddisease.Attheendofthestudy, the mortality of the individuals operated within the first 24hourswaslower.However,whenthegroupswere homog-enized for presence of associateddiseases, this difference disappeared.18
Thereareseveralpossibleexplanationsforthisfinding.The firstpossibilitymaybelinkedtothefactthattheoccurrence ofmanypost-surgicalcomplicationsinpatientswhodiedmay
1.0
0.8
0.6
0.4
0.2
0.0
0 20 40
Time
Survival
60 N Y
notnecessarilybeassociatedwithwaitingtime.Secondly, dur-ingthecollectionphase,amarkedpatternofpostponementof surgicalprocedureswasobserved(althoughnotdescribedin thestudy),duetoeitherlackofbedsintheICUorinadequate clinicalconditionsofpatients, bothofthosewho were dis-chargedandthosewhodied.However,anobservationalstudy of2660patientsfoundthatdelayingsurgerybyuptofourdays didnotaffectmortality,whileadelayofmorethanfourdays significantlyincreasedmortalityrates.19Nevertheless,a
sys-tematicreviewof256,367patientsobservedthatadelay of morethan48hoursincreasestheriskofall-causemortalityat 30daysaftersurgerybyupto41%.20
MeansurvivalofpatientswhodidnotrequireICU admis-sion was higher than that of those who did. The main hypothesiswasthatthelatterhadamoreunfavorable clin-icalpicture,agreaternumberofcomorbidities,andolderage whencomparedwithpatientswhodidnotrequireintensive care.However,Fuchsetal.,21with7265patientsover65years,
observedthatthemainreasonforICUadmissionwas asso-ciatedcomorbidities.Oldageshouldbeconsideredasarisk factor,especiallyforpatientsolderthan75yearsadmittedin theseunits.
Fewstudieshavesoughttoanalyzetheprognosticimpact ofinflammatorycellsinfemurfractures.Inthisstudy,a sig-nificantdifferencewasobservedintherelationshipbetween total leukocyte countduring hospitalization and death. In thisrespect,accordingtotheROCcurveanalysis,leukocytes wereshowntohaveadiscriminativeabilitytoidentifythose patientswithfemoralfracturewhohadahigherriskofdeath. Whiteetal.10observedaprevalenceofleukocytosisof43.5%.
However, the high leukocyte count was at the expense of increasingthenumberofneutrophils; thisvariablewasnot evaluatedinthepresentstudy.Thisfindingisrelatively com-moninpatientswithhipfracture,indicatingpossiblepresence ofaprevious infectionor aninfectionthat developedafter thefracture.10 Thus,it isimportanttonote that the
cellu-larandhumoralelementsdecreasewithincreasingage;the presentstudyconsistedofelderlypatientswithamean82.1 yearsinthehighermortalitygroup,whichmayexplainthe highermeantotalleukocytecountinpatientswho died.In addition,whenanalyzingtheROCcurve,agealsopresenteda discriminativeabilitytoidentifyindividualsathigherriskof death.
Theoverallmortalityof14.4%canbeconsideredhigh,and isconsiderablydifferentfrom the resultsfoundin interna-tionalstudies,wheredeathrateswerelower.Inaretrospective study inCanada with3981patients, the hospitalmortality ratewas6.3%.22 Inthiscontext,anotherretrospectivestudy
inItalywith6629elderlypatients presentedanevenlower rateof5.4%.23Furthermore,atthenationallevel,theresults
ofthisstudyweresimilartoaretrospectivestudythatreported amortality rateof 14.61%. Theliteratureshows that over-all mortality inrelationship to thesetypes offracture has variedamongservices, depending onthe existing hospital complex.24
This study was conducted in a single-center reference regionalhospital.Inthiscontext,theliteratureindicatesthat ininstitutions withhigher volumeofhip surgeries,higher mortalityratesareobserved.Higherin-hospitalmortalityin thesehospitals,whencomparedwithlower-demandservices,
was reflectedinthe present study.24 Inorderto generalize
dataforelderlypatientshospitalizedforvarioustypesofhip fracture,theauthorsbelievethereisnoreasonforthistobe different,whichcouldexplainthepresentfindingsregarding deathrates. Moreover,another factorto beassessedisthe perioperativemortality,whichalsocontributestooverall mor-talityrateandisnotassociatedwithqualityofthetherapeutic approachoffered,butrathertotheclinicalconditionofthese patients,whichisusuallyhigh-riskduetotheirageandthe presenceofmanyassociatedcomorbidities.
The association of the fracture site with mortality was notsignificantinthepresentstudy.However,inasystematic reviewwith544,733patients,mortalitywashigherinpatients withintracapsularfracture.Thatstudyalsoobservedageover 85yearsasafactorassociatedwithmortality.Thisfindingis similartothatofthepresentstudy,whichhadasimilarmean ageatdeath.25
Themainlimitationofthepresentstudywasthe inabil-itytocollectdatarelatedtocertainvariables,duetolackof informationinthemedicalcharts,whichmayhave underesti-matedtheactualclinicalconditionofthepatients.Inaddition, thepresentstudywasobservational,sotheassociationsfound donotimplycausality;thepresentfindingsshouldbe con-firmedbyfurtherstudies.
Conclusion
Inthepresentstudy,itwasobservedthatwomencomprised themajorityofadmissions,andthatthedegreeofleukocytosis associatedwithadvancedagewascorrelatedwithmortality, regardlessoftypeofinjuryandsurgicalprocedure.Ahigher meansurvivalrateofpatientswhodidnotrequireICU admis-sionwasalsoobserved.Itisnoteworthythatthewaitingtime forsurgeryand hospitalstay werenot associatedwith the in-hospital mortalityoutcome.Thesefindingshighlight the importanceofdevelopingprotocols forbettermanagement of these patients. They alsoemphasize the importanceof including theassessmentofleukocytesratesintothe clini-calevaluation,asthisvariablepresentedanimportantability topredictworseoutcomes.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.Organizac¸ãoMundialdaSaúde.Envelhecimentoativo:uma políticadesaúde.Brasília,DF:Organizac¸ãoPan-Americanade Saúde;2005.
2.BortolonPC,AndradeCLT,AndradeCAF.Operfildas internac¸õesdoSUSparafraturaosteoporóticadefêmurem idososnoBrasil:umadescric¸ãodotriênio2006–2008.Cad SaúdePúbl.2011;27(4):733–42.
3.MonteiroCR,FaroACM.Avaliac¸ãofuncionaldeidosovítima defraturasnahospitalizac¸ãoenodomicílio.RevEscEnferm USP.2010;44(3):719–24.
5. SilveiraVAL,MedeirosMMC,CoelhoJM,MotaRS,NoletoJCS, CostaFS,etal.Incidênciadefraturadoquadrilemárea urbanadoNordestebrasileiro.CadSaúdePúbl. 2005;21:907–12.
6. SakakiMH,OliveiraAR,CoelhoFF,LemeLEG,SuzukiI, AmatuzziMM.Estudodamortalidadenafraturadofêmur proximalemidosos.ActaOrtopBras.2004;12(4):242–9. 7. SouzaRC,PinheiroRS,CoeliCM,JuniorKRC,TorresTZG.
Aplicac¸ãodemedidasdeajustederiscoparaamortalidade apósfraturaproximaldefêmur.RevSaúdePúbl.
2007;41(4):625–31.
8. deRooijSE.Hipprotectorstopreventfemoralfracture.BMJ. 2006;332(7541):559–60.
9. Etxebarria-ForondaI,MarJ,ArrospideA,RuizdeEguinoJ. Costandmortalityassociatedtothesurgicaldelayofpatients withahipfracture.RevEspSaludPubl.2013;87(6):639–49. 10.WhiteSM,SangheraP,ChakladarA.Leukocytosisincreases
lengthofinpatientstaybutnotage-adjusted30-day mortality,afterhipfracture.AgeAgeing.2010;39(5):650–3. 11.FaloppaF,AlbertoniWM.Guiadeortopediaetraumatologia
daUnifesp-EPM.SãoPaulo:Manole;2008.
12.CastronuovoE,PezzottiP,FranzoA,DiLalloD,GuasticchiG. Earlyandlatemortalityinelderlypatientsafterhipfracture: acohortstudyusingadministrativehealthdatabasesinthe Lazioregion,Italy.BMCGeriatr.2011;11:37.
13.ConstantinoH,PatrícioPF,PedrosaC,PintoFG,PereiraV, DiogoN.Fraturaproximaldofémurbilateral:incidênciae fatoresderiscodefraturacontralateral.RevPortOrtop Traumatol.2013;21(3):381–7.
14.MoraesFB,SilvaLL,FerreiraFV,FerroAM,RochaVL,Teixeira KS.Avaliac¸ãoepidemiológicaeradiológicadasfraturas diafisáriasdofêmur:estudode200casos.RevBrasOrtop. 2009;44(3):199–203.
15.RocheJJ,WennRT,SahotaO,MoranCG.Effectof
comorbiditiesandpostoperativecomplicationsonmortality afterhipfractureinelderlypeople:prospectiveobservational cohortstudy.BMJ.2005;331(7529):1374.
16.HossainM,NeelapalaV,AndrewJG.Resultsofnon-operative treatmentfollowinghipfracturecomparedtosurgical intervention.Injury.2009;40(4):418–21.
17.GjertsenJE,VinjeT,EngesaeterLB,LieSA,HavelinLI,Furnes O,etal.Internalscrewfixationcomparedwithbipolar hemiarthroplastyfortreatmentofdisplacedfemoralneck fracturesinelderlypatients.JBoneJointSurgAm. 2010;92(3):619–28.
18.GrimesJP,GregoryPM,NoveckH,ButlerMS,CarsonJL.The effectsoftime-to-surgeryonmortalityandmorbidityin patientsfollowinghipfracture.AmJMed.2002;112(9):702–9. 19.MoranCG,WennRT,SikandM,TaylorAM.Earlymortality
afterhipfracture:isdelaybeforesurgeryimportant?JBone JointSurgAm.2005;87(3):483–9.
20.ShigaT,WajimaZ,OheY.Isoperativedelayassociatedwith increasedmortalityofhipfracturepatients?Systematic review,meta-analysis,andmeta-regression.CanJAnaesth. 2008;55(3):146–54.
21.FuchsL,ChronakiCE,ParkS,NovackV,BaumfeldY,ScottD, etal.ICUadmissioncharacteristicsandmortalityrates amongelderlyandveryelderlypatients.IntensiveCareMed. 2012;38(10):1654–61.
22.JiangHX,MajumdarSR,DickDA,MoreauM,RasoJ,OttoDD, etal.Developmentandinitialvalidationofariskscorefor predictingin-hospitaland1-yearmortalityinpatientswith hipfractures.JBoneMinerRes.2005;20(3):494–500. 23.FranzoA,FrancescuttiC,SimonG.Riskfactorscorrelated
withpost-operativemortalityforhipfracturesurgeryinthe elderly:apopulation-basedapproach.EurJEpidemiol. 2005;20(12):985–91.