w w w . r b o . o r g . b r
Original
Article
Results
from
surgical
treatment
of
Morel-Lavallée
lesions:
prospective
cohort
study
夽
Evandro
Pereira
Palacio
∗,
Gabriel
Guimarães
Di
Stasi,
Ewerton
Henrique
Rodrigues
Teixeira
Lima,
Roberto
Ryuiti
Mizobuchi,
Alcides
Durigam
Júnior,
José
Antônio
Galbiatti
FaculdadedeMedicinadeMarília,Marília,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received23February2014 Accepted20March2014
Availableonline28February2015
Keywords:
Woundsandinjuries Soft-tissueinjuries/pathology Soft-tissueinjuries/surgery Multipletrauma
a
b
s
t
r
a
c
t
Objective:Topresenttheresultsfromearlydiagnosisanddelayedsurgicaltreatmentofa cohortofpatientswhowerediagnosedwithMorel-Lavalléelesions.
Methods:BetweenJanuary2006andDecember2013,weperformeddelayedsurgical debride-mentonMorel-Lavalléelesions,afterdelimitationofthelocaltissuenecrosis,followedby closurethroughsecondintentionand/oruseofgrafts/flaps.
Results:All thepatients evolved with complete closureof thelesion after the delayed debridement,granulationoftheoperativewoundandprimarysuturingorconstructionof pedunculatedflaps.Threepatients(50%)evolvedwithdeepinfectiousprocessesduetothe successiveoperativeprocedures.
Conclusion:Whateverthetreatmentmethodsusedare,theyshouldbeperformedinaradical manner.Ifnot,thepatientwillbeatriskofevolutiontosepticemiaanddeath.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
Resultados
do
tratamento
cirúrgico
da
lesão
de
Morel-Lavallée.
Estudo
coorte
prospectivo
Palavras-chave:
Ferimentoselesões
Lesõesdostecidosmoles/patologia Lesõesdostecidosmoles/cirurgia Traumatismomúltiplo
r
e
s
u
m
o
Objetivo:apresentarosresultadosdodiagnósticoprecoceedotratamentocirúrgicotardio deumacoortedepacientesdiagnosticadacomalesãodeMorel-Lavallée(LML).
Métodos:dejaneirode2006adezembrode2013osautoresfizeramodesbridamentocirúrgico tardiodaLML,apósadelimitac¸ãodanecroseteciduallocal,seguidodefechamentopor segundaintenc¸ãoe/ouenxertos/retalhos.
Resultados:todosospacientesevoluíramcomfechamentototaldalesãoapóso desbrida-mentotardioagranulac¸ãodaferidaoperatóriaea(os)suturaprimária/retalhospediculados. Trêspacientes(50%)evoluíramcomprocessoinfecciosoprofundodevidoaossucessivos procedimentosoperatórios.
夽
WorkdevelopedattheDepartmentofOrthopedicsandTraumatology,FaculdadedeMedicinadeMarília,Marília,SP,Brazil.
∗ Correspondingauthor.
E-mail:palacio@famema.br(E.P.Palacio). http://dx.doi.org/10.1016/j.rboe.2015.02.011
Conclusão:sejamquaisforemosmétodosdetratamentoempregados,estesdevemserfeitos demaneiraradical,sobriscodeevoluc¸ãodospacientesparasepticemiaeóbito.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Todososdireitosreservados.
Introduction
Morel-Lavallée lesions (MLLs), also known as degloving injuries,werefirstdescribedbytheFrenchphysicianMaurice Morel-Lavalléein1853.Theyareraresoft-tissueinjuriesthat areassociatedwithhighratesofmorbidityandmortality.1–8 Theyoccurbecauseofsudden applicationofhigh-intensity forcestoacertainareaofthebodyandtheireffectisto sepa-rateskinandsubcutaneoustissuefromtheunderlyingmuscle fascia.9,10 Thespacethuscreatedbecomesfilledwithblood, lymphornecroticfattytissue,andthisnotuncommonlyleads tosevereinflammatoryandinfectiousprocesses.3,7–10
DiagnosingMLLsisnotaneasytask.Inthegreatmajorityof thecases,theseareclosedinjuriesandthisoftencauses con-fusionorevenfailuretodiagnosethecondition.Duringcareful clinicalexamination,itcanbeseenthatintheacutephase, thevolumeoftheareaaffectedisgreater,andthisis accom-paniedbyfloating,hypermobilityandhypoesthesia.4,5,7,9The lesionusuallyaffectsanareagreaterthantheareathatcan initiallybeassessedinthecourseofthephysicalexamination, duringemergencyattendance.3,10Thecirculationoftheskin andsubcutaneoustissueintheinjuredsegmentiscommonly compromisedandthereisoftengreatdifficultyin determin-ingwhetherthesetissuesarerecoverable.3Innormaltissues, theviabilityofthecapillaryperfusioncangenerallybe eas-ilyestimatedbymeansofapplyinglocalcompressionusing afingerorthroughidentifyingactivebleedingintheregion affected.However,inthecaseofcomplextissuedamage,as occursinMLL,thesetestsmaynotbethemostreliabletype fordiagnosticpurposes. Typically,the treatmentcomprises early radical debridement of the tissuesaffected, followed bysecond-intentionhealingofthewound.5–8,11,12 However, someauthors havetakenthe viewthatpostponingthe ini-tialtreatmentuntilthetimewhendelimitationornecrosisof thetissueshasoccurredisthebestapproach.13Whateverthe therapyused,thereisunanimitythatsuchpatientswilloften havetoundergomultipleproceduresandsurgicalrevisions, withahigherriskofinfection.3,5–7,9
Giventhepoorprognosisofthistypeofinjuryandthe diffi-cultyinmakingprecisediagnosesandtreatments,alongwith thecompletelackofinformationonthistopicinthevarious databasesavailable,andparticularlyintheBrazilian orthope-dicdatabases,thepresentstudywasproposedwiththeaimof evaluatingtheresultsfromlatediagnosisandsurgical treat-mentofMLL.
Patients
and
methods
This was a prospective cohort study that was approved byourinstitution’s ethicscommitteeforresearchinvolving humanbeings(CAAE04497812.4.0000.5413).Allthepatients,
or theirlegalguardians, agreedtoparticipateandsigneda freeand informedconsentstatementafterhavingreceived detailed information about the content and form of the study.
Thesamplesizewas determined beforehand,bymeans ofspecificstatisticaltests. The␣ risk(5%)and risk(20%) weretakenintoconsideration,alongwiththevariabilityofthe variables(p1=0.13andp2=0.9),thusarrivingataminimum numberoffiveindividuals.
Initially,11patientswithadiagnosisofMLLconfirmedby meansoftomographyand/ormagneticresonance examina-tionwereselected,betweenJanuary2006andDecember2013. Patientswereexcludediftheypresentedanyofthefollowing: previousclinicalorsurgicaltreatmentonthelesionin ques-tion(n=3);generalstateofhealththatwasconsideredtobe poororserious(n=1);refusaltosignthefreeandinformed consentstatement(n=1).Thus,thefinalcohortconsistedof sixpatients.
Alltheoperativeprocedureswereperformedbythesame orthopedicteam,alwaysunderthesamepreand postopera-tiveprotocols.
Afterthepatientshadarrivedattheemergencyserviceand had gonethrough theadvancedtraumalifesupport(ATLS) protocol, simpleradiographs of the contused regionswere produced,always intwoorthogonalviews.On thebasisof specificabnormalitiesseenintheclinicalexamination (exces-sivelocalpainthatwasoutoflinewiththeintensityofthe trauma;extensiveecchymosisorhematomas;andespecially, local/regional hypermobilityofthe skin),the patients then underwenttomographyormagneticresonanceexaminations, inordertoconfirmthediagnosisofMLL.
Afterobtainingconfirmationthatdetachmentoftheskin and/orsubcutaneouscellulartissuehadoccurred,wewaited anotherfourtofivedaysforthelesiontobecomedelimited with the first signs of necrosis. Atthat time, the patients were taken tothe surgicalcenter to undergo debridement procedures,alwaysinassociationwithirrigationandprofuse washing(Figs.1–5).
Once the infectious processes had been brought under control,granulationoftheoperativewoundwasawaited,in ordertobeabletoconstructmyocutaneousflapsand/or per-formprimaryclosureofthegranulatededgesofthewound (Figs.6and7).
Results
Table1–Generalcharacteristicsofthepatients.
Gender Age Anatomicalregion Injurysize Traumamechanism
Patient1 Female 25 Posteriorfaceofforearm/elbow Approx.20cm Fallfrom
motorbike
Patient2 Male 44 Thighandgluteus Morethan30cm Fallfromaheight
Patient3 Male 37 Knee/calf Approx.15cm Caraccident
Patient4 Male 31 Hipandflank Morethan30cm Caraccident
Patient5 Male 55 Lateralfaceofhip Approx.20cm Directtrauma
(workaccident)
Patient6 Female 47 Anteriorfaceofthigh Approx.15cm Caraccident
Fig.1–Coronaltomographicsliceshowinglarge accumulationoffluid(arrow),betweenthesubcutaneous tissueandmusclefascia.
Fig.2–Axialtomographicsliceshowinglarge
accumulationoffluid(arrow),betweenthesubcutaneous tissueandmusclefascia.
Discussion
MLL,ordegloving injury,isarareformofsoft-tissueinjury thatisassociatedwithhighmorbidity.12,14,15Theareasthat
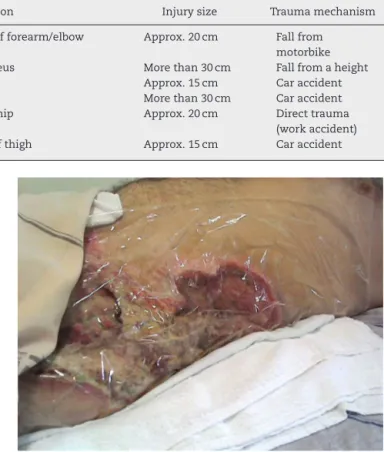
Fig.3–Imageofflankandhipafterinitialdebridement, showingnecrosisandinfection.
Fig.4–Imageofflankandhip,undergoingsecondary healingprocess(granulationtissue).
are mostlikelytosuffersuchinjuriesare theanterolateral thigh,gluteal,lumbodorsalandscapularregions.6–8,12,14
ThepatientsaffectedbyMLLaregenerallyyoung.Inthis study,thecohortofpatientsconsistedofindividualsbetween theagesof25and55yearswhowereeconomicallyactive.They weremostlymale(Table1).9,13
Fig.5–Imageofflankandhip,undergoingsecondary healingprocess(granulationtissue).
Fig.6–Attempttobringtogethertheedgesofthewound, beforeconstructingmyocutaneousflaps.
that the subcutaneous tissue becomes detached from the musclefascia,therebyinjuringthevesselsthatpassthrough theselayers.1,5,15Thehemolymphfluidbecomessurrounded bygranuloustissue,whichmayleadtoformationofafibrous pseudocapsule,preventionoffluidreabsorptionand predis-positiontowardbacterialcolonizationandinfection.9,11–14
Historically,thetreatmentforsuchinjurieshascomprised serialopendebridementfollowedbysecond-intention heal-ing.Recently,methodsthatarelessinvasivehavebeentried out.OneoftheseiscompressionbymeansofaVicrylmesh, which distributes the surface tension in the region ofthe woundtoalargersurface,therebyprovidingreliefforthe ten-sionintheopenarea.However,thereisnoevidencethatthis treatmentisfreefromsequelae.10,11,16Somelesionsmay per-sist,despiteconventionaltreatments.Inthesecases,methods thatare moreaggressiveare commonlyindicated, such as serialaspirationandtheuseofchemicalsclerosis,incases offormationofpseudocysts.3,8,13,15
Compromisedcirculation in the skinand subcutaneous tissue in the injured segment is always observed and
Fig.7–Finalimageafterperforminggrafting.
it is often difficult to determine whether the tissue is recoverable.3,10–12,15 Cutaneous capillary filling tests and bleedingtests havedubiousvalueinevaluatingMLL cases, giventhatthelocalorregionalcapillaryfilling mayremain withinnormalparametersforupto36h,duetotheactionof thecapillarynetworkadjacenttotheinjuredarea.Thelack ofreliableparametersmaymaketheinitialdiagnosisofthe injurydifficult,therebyleadingtosevereconditionsof necro-sisandsepticemia.
Inthisstudy,althoughthediagnosiswasinvariablymade during the acute phase, by means of detailed physical examinationandimagingexaminations,itwasdecidedto per-formed latedebridement,four or fivedaysafter theinitial injury.Overthisperiod,localsignsoftissuenecrosisand con-sequentdelimitationoftheregionaffectedcouldalreadybe observed.Infact,overaseven-dayperiodfollowingtheinitial injury,threeofthepatientsinoursample(50%)evolvedwith extensiveareasofsuperficialanddeepnecrosis(skin, subcu-taneoustissue,fascias,muscles,tendonsandnerves)8,10,13–16 andtheypresentedsevereinfectiousprocesses.Debridement, withradicalremovalofallthedevitalizedstructures,therefore becameimperative,duetotheriskofsepticemiaand progres-siontodeath.
Itwasalsoseenthatlatedebridementofthelesion,only afterthenecroticareahadbecomedelimited,greatly dimin-ished the chances of inadvertent removal of healthy soft tissues,i.e.thosethatstillpresentedeffectivecirculation.
Finally,scarsretractinmanycases,andthisparticularly wors-enstheprognosisforthesepatients,giventhatnewsurgical proceduresareneedsinordertoachieveaminimumdegree ofjointmovement.
Conclusion
MLLisstillalittleknownconditionamongtheprofessionals whoworkonthefrontlineofemergencyservices,including orthopedicsurgeons.Perhapsforthisreason,itisan under-diagnosedtypeofinjury.Whatever thetreatment methods usedare,theyshouldbeimplementedinaradicalmanner, becauseoftheriskofevolutiontosepticemiaanddeath.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. PitrezEH,PellandaRC,SilvaME,HolzGG,HertzFT,Hoefel FilhoJR.LesãodeMorel-Lavallée:relatodecaso.RadiolBras. 2010;43(5):336–8.
2. DemirelM,DereboyF,OzturkA,TurhanE,YazarT. Morel-Lavalléelesion:resultsofsurgicaldrainagewiththe useofsyntheticglue.SaudiMedJ.2007;28(1):65–7. 3. MelloDF,DemarioLA,SoldaSC,HeleneJúniorA.
Desenluvamentosfechados:lesãodeMorel-Lavallée.RevBras CirPlast.2010;25(2):255–60.
4. TsengS,TornettaP3rd.Percutaneousmanagementof Morel-Lavalléelesions.JBoneJointSurgAm.2006;88(1):92–6. 5. VanGennipS,vanBokhovenSC,vandenEedeE.Painatthe
knee:theMorel-Lavalléelesion,acaseseries.ClinJSport Med.2012;22(2):163–6.
6.MoriartyJM,BorreroCG,KavanaghEC.Ararecauseofcalf swelling:theMorel-Lavalléelesion.IrJMedSci.
2011;180(1):265–8.
7.TejwaniSG,CohenSB,BradleyJP.Managementof
Morel-Lavalléelesionoftheknee:twenty-sevencasesinthe nationalfootballleague.AmJSportsMed.2007;35(7):1162–7. 8.LuriaS,YaakovA,YoramW,MeirL,PeyserA.Talc
sclerodhesisofpersistentMorel-Lavalléelesions (posttraumaticpseudocysts):casereportof4patients.J OrthopTrauma.2006;20(6):435–8.
9.AnakwenzeOA,TrivediV,GoodmanAM,GanleyTJ.Concealed deglovinginjury(theMorel-Lavalléelesion)inchildhood sports:acasereport.JBoneJointSurgAm.2011;93(24):e148. 10.MontbrunS,KhaliliK,MacLellanS,EassonA.Morel-Lavallée
lesionofthelowerbackmimickinganabscess:acasereport. SurgSci.2012;3(4):213–5.
11.GwinnDE,MorganRA,KumarAR.Gluteusmaximusavulsion andcloseddeglovinglesionassociatedwithathoracolumbar burstfracture.Acasereport.JBoneJointSurgAm.
2007;89(2):408–12.
12.CollingeC,TornettaP3rd.Softtissueinjuriesassociatedwith pelvicfractures.OrthopClinNorthAm.2004;35(4):451–6. 13.WoodGW.Generalprinciplesoffracturetreatment.In:Canale
ST,BeatyJH,editors.Campbell’soperativeorthopaedics.11th ed.Philadelphia:MosbyElsevier;2008.p.3032–5.
14.HarmaA,InanM,ErtemK.TheMorel-Lavalléelesion:a conservativeapproachtocloseddeglovinginjuries.Acta OrthopTraumatolTurc.2004;38(4):270–3.
15.DemirelM,DereboyF,OzturkA,TurhanE,YazarT. Morel-Lavalléelesion.Resultsofsurgicaldrainagewiththe useofsyntheticglue.SaudiMedJ.2007;28(1):65–7. 16.HakDJ,OlsonSA,MattaJM.Diagnosisandmanagementof