Full
length
article
Defecatory
dysfunction
and
fecal
incontinence
in
women
with
or
without
posterior
vaginal
wall
prolapse
as
measured
by
pelvic
organ
prolapse
quanti
fi
cation
(POP-Q)
Kathiane
Lustosa
Augusto
a,b,*
,
Leonardo
Robson
Pinheiro
Sobreira
Bezerra
a,
Sthela
Maria
Murad-Regadas
c,d,e,
José
Ananias
Vasconcelos
Neto
f,
Camila
Teixeira
Moreira
Vasconcelos
g,
Sara
Arcanjo
Lino
Karbage
a,b,
Andreisa
Paiva
Monteiro
Bilhar
a,
Francisco
Sérgio
Pinheiro
Regadas
c aDepartmentofGynecology,SchoolofMedicineoftheFederalUniversityofCeará,Fortaleza,Ceará,BrazilbDepartamentofGynecology,SchoolofMedicineoftheFortalezaUniversitário(UNIFOR),Fortaleza,Ceará,Brazil cDepartmentofSurgery,SchoolofMedicineoftheFederalUniversityofCeará,Fortaleza,Ceará,Brazil
dUnitofPelvicFloorandAnorectalPhysiology,ClinicalHospital,FederalUniversityofCeará,Fortaleza,Ceará,Brazil eUnitofPelvicFloorandAnorectalPhysiology,DepartmentofColorectalSurgery,SaoCarlosHospital,Ceara,Brazil fUrogynecology,GeneralHospitalofFortaleza,Ceara,Brazil
gDepartmentofNursing,SchoolofMedicineoftheFederalUniversityofCeará,Fortaleza,Ceará,Brazil
ARTICLE INFO
Articlehistory:
Received23August2016
Receivedinrevisedform7February2017 Accepted20April2017
Availableonlinexxx
Keywords:
Pelvicfloor Pelvicorganprolapse Constipation Fecalincontinence Qualityoflife Sexualdysfunctions Psychological
ABSTRACT
Introductionandhypothesis:PelvicFloorDysfunctionisacomplexconditionthatmaybeasymptomaticor
mayinvolvealotofsymptoms.Thisstudyevaluatesdefecatorydysfunction,fecalincontinence,and
qualityoflifeinrelationtopresenceofposteriorvaginalprolapse.
Methods:265patientsweredividedintotwogroupsaccordingtoposteriorPOP-Qstage:posteriorPOP-Q
stage2andposteriorPOP-Qstage<2.Thetwogroupswerecomparedregardingdemographicand
clinicaldata;overallPOP-Qstage,percentageofpatientswithdefecatorydysfunction,percentageof
patientswithfecalincontinence,pelvicfloormusclestrength,andqualityoflifescores.Thecorrelation
betweenseverityoftheprolapseandseverityofconstipationwascalculatedusingrdeSpearman(rho).
Results:WomenwithBpstage2weresignificantlyolderandhadsignificantlyhigherBMI,numbersof
pregnanciesandbirths,andoverallPOP-Qstagethanwomenwithstage<2.Nosignificantdifferences
betweenthegroupswereobservedregardingproportionofpatientswithdefecatorydysfunctionor
incontinence,pelvicfloormusclestrength,qualityoflife(ICIQ-SF),orsexualimpact(PISQ-12).POP-Q
stagedidnotcorrelatewithseverityofconstipationandincontinence.Generalqualityoflifeperception
ontheSF-36wassignificantlyworseinpatientswithPOP-Qstage2thaninthosewithPOP-Qstage<2.
Conclusions:Thelackofaclinicallyimportantassociationbetweenthepresenceofposteriorvaginal
prolapseandsymptomsofconstipationoranalincontinenceleadsustoagreewiththeconclusionthat
posterior vaginal prolapse probably is not an independentcause defecatory dysfunction or fecal
incontinence.
©2017ElsevierB.V.Allrightsreserved.
Briefsummary
A prospective cross-sectional study to evaluate defecatory dysfunction,fecalincontinence,andqualityoflifeinrelationto presenceofposteriorvaginalprolapse.
Introductionandhypothesis
Women mayconsulturogynecology servicesbecause ofone problemsuchasurinaryincontinence,butin-depthquestionsand detailedphysicalexaminationoftenrevealsotherdisordersrelated topelvicfloordysfunction(PFD)[1].PFDisacomplexcondition that maybeasymptomaticor mayinvolvesymptomsofsexual dysfunction, anorectal dysfunction,urinary dysfunction, and/or pelvicorganprolapse(POP)[2].
*Corresponding authorat: Department of Gynecology, School ofMedicine, FederalUniversityofCeará,2470,ap701,TiburcioCavalcantest,Fortaleza,Ceará, 60125-101,Brazil.
E-mailaddress:kathianelustosa@yahoo.com.br(K.L.Augusto).
http://dx.doi.org/10.1016/j.ejogrb.2017.04.039 0301-2115/©2017ElsevierB.V.Allrightsreserved.
ContentslistsavailableatScienceDirect
European
Journal
of
Obstetrics
&
Gynecology
and
Reproductive
Biology
POPincludessupportdefectsofthevaginalapex,theanterior vaginalwall,and theposterior vaginalwall.Mostpatientshave supportdefectsatmultiplelocations[1].Thesymptomscommonly attributed to POP include vaginal bulging, herniation, pelvic pressure, bleeding, discharge, infection, need for splinting or digitationtoassist voidingordefecation,and lowbackache[2]. Defecatory dysfunction (difficulty in defecation with excessive straining to empty the bowels, feeling of incomplete bowel emptying, constipation, and manual evacuation with digital assistance)isoftenpresentinpatientswithPOP[3–5].However, itis unclearwhethertheabnormal anatomicalpositions of the bladder, bowel, and uterus compromise bladder and bowel functiondirectly,orwhetherabnormalanatomyanddysfunction ofthepelvicfloorshareacommonetiology[6–13].
Gynecologistsdonotalwaysinquireaboutboweldysfunction [14],andDuaetal.[10]reportedthatcolorectalsymptomsmaybe ignoredinwomenpresentingtogynecologyclinicswithprolapse. The use of specific tools, including clinical assessment of constipation and continence, helps identify these disorders, allowinghealth careprofessionals todeterminetheappropriate treatment approach. The aim of this study was to evaluate defecatorydysfunction,fecalincontinence,and qualityoflifeas assessedbystandardizedquestionnairesinrelationtopresenceof posterior vaginal prolapse in women, as measured by POP-Q, referredtoaurogynecologic outpatientclinicbecauseof symp-tomsofPFD.
Methods
From July 2011 through July 2013, 265 adult women with symptoms of PFD, who were referred to the urogynecologic outpatientclinicofGeneralHospital,Fortaleza,Ceará,Brazil,were enrolledinthestudy.Theclinicalprotocolwasapprovedbythe ResearchEthicsCommitteeandallpatientsgavewritteninformed consent.
Adetailed medicaland urogynecologic historywas obtained fromeachwoman.Subjectspresentingforclinicalevaluationwith symptoms of PFD (genital prolapse or incontinence) were recruited.Weconsideredsymptomsofprolapsetobeasenseof somethingcomingorfallingoutoftheirvagina,theabilitytofeela bulge coming out of their vagina, pelvic fullness or pressure particularlywhenupright,andhavingtopushupontheperineum ordigitatethevaginainordertourinateordefecate.
Baselinedataincludeddemographics,bodymassindex(BMI), and information concerning parity, number of deliveries, and menopausalstatus.A physicalexaminationincludingstagingof theprolapsebasedonthePOP-Qsystem[15]wasperformed.All vaginalexaminations wereperformedwithan emptiedbladder andthepatientinasupineposition.
The POP-Q system considers six defined points within the vagina:twoanterior(AaandBa),twoposterior(ApandBp),and twoapical(CandD)[15].Eachpointisexpressedasthedistancein centimeters from the hymen (considered as the landmark for reference), with the woman performing a maximum Valsalva manoeuvre. Points at the level of the hymenal remnants are definedaszero,pointsabovethehymenarenegative,andpoints belowthehymenarepositive.PointApislocatedinthemidlineof theposteriorvaginalwall3cmproximaltothehymen.PointBp representsthe mostdistal positionofthe upperportionof the posteriorvaginalwallfromthevaginalcufforposteriorvaginal fornixtopointAp.
POP-Qstages0to4weredeterminedbasedonthepositionof the lowest portion of the prolapse, with stage 4 prolapse representing the maximum protrusion. POP-Q stages were determinedforeachcompartment(anterior,apical,andposterior) ofthevagina[15].
The staging system for posterior vaginal segment is: Stage 1=ProlapsewheretheBppointremainsatleast1cmaboveofthe hymenal remnants; Stage 2=Prolapse where the Bp point descendstothehymenalremnants,definedasanareaextending from 1cm above to 1cm below the hymenal remnants; Stage 3=ProlapsewheretheBppointdescendsgreaterthan1cmpast thehymenalremnants,butdoesnotrepresentcompletevaginal vault; Stage 4=Complete posterior vaginal wall is maximally prolapsedwithessentiallytheentireextentofthevaginalmucosa everted.
The patients were divided into two groups according to posterior POP-Q stage (based on the vaginal wall Bp point): posteriorPOP-Qstage2(consideredwithposteriorprolapse)and posteriorPOP-Qstage<2(withoutposteriorprolapse)[15].Itwas decidedtousethestage2asthecutoffpointforconsideringthe diagnosisofsymptomaticPOPinourstudy.Wedefinethenasa groupwithoutprolapseofposteriorvaginalwallallwomenwith< Bp-1 and consequently group with vaginal wall prolapse later women with Bp 1, because patients are more symptomatic. Thiscutoffpointwasalsofoundinotherstudies[16,17].
The twogroups werecompared regarding demographic and clinical data; overall POP-Q stage, percentage of patients with defecatorydysfunction,percentageofpatientswithfecal inconti-nence,pelvicfloormusclestrength,andqualityoflifescores.
DefecatorydysfunctionwasassessedbymeansoftheCleveland Clinic Florida(CCF) ConstipationScoringSystem[17].The scale addressesthefollowingvariables:frequencyofbowelmovements, difficulty (painful evacuation effort), completeness (feeling in-completeevacuation),abdominalpain,time(minutesinlavatory per attempt), type of assistance needed for evacuation, failure (numberofunsuccessfulattemptsper24h),andhistory(duration ofconstipationinyears),withaminimumscoreof0andmaximum score of 30. Patients with CCF constipation scores 6 were diagnosedashavingdefecatorydysfunction.
Fecal incontinence was assessed by means of the CCF Incontinence Scale [18]. The incontinence scale addresses the frequencywithwhichpatients experienceleakageofgas,liquid andsolidstool,needforpads,andlifestylealterationatvarying frequencies,andtheextenttowhich thepatient’slifeisaltered (minimum score, 0; maximum score, 20). Patients with CCF incontinence scores1werediagnosedashavingfecal inconti-nence.
Pelvicfloormusclestrengthwasevaluatedbythe physiothera-pist using the PERFECT scheme, which comprised Power (or pressure, strengthmeasured byusing a manometric perineom-eter), Endurance, Repetitions, Fast contractions, and Every ContractionTimed)[19,20].Qualityoflifewasassessedwiththe generic Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) [21], the International Consultation on Inconti-nence QuestionnaireShort Form (ICIQ-SF) [22], and the Pelvic Floor and Incontinence Sexual ImpactQuestionnaire (PISQ-12) [23]. All quality of life questionnaires used were validated to Portuguese.
SamplesizewascalculatedbasedonthestudybyDevreeseetal. [16],whichevaluatedthefunctionofpelvicfloormusclesthrough vaginal palpation in women withand without urinary inconti-nence.Thestudysamplecalculationwas basedonapilotof65 womenwithandwithoutPFD.Itwasusedthesamemethodology, questionnairesandcriteriaofinclusionandnon-inclusionofthe current study. It was consideredas an outcome worse QoL in patients with PFD and worst socioeconomic profile. With 80% power and 95% confidence. The total sample was 265 women establishedwithsymptomsofPFD,149hadPOP-Qstage2and 116hadPOP-Qstage<2posteriorprolapse(Bp).
Univariate analysiswas performedusing theMann-Whitney test for continuous nonparametric data, Student’s t test for
continuousparametricdata,andthe
x
2testfornominaldata.Thecorrelation between severity of the prolapse and severity of constipationwascalculatedusing
r
deSpearman(rho).Thelevelofstatisticalsignificancewassetatp<0.05.Statisticalanalysiswas performedusingSPSS18.0(SPSSInc,Chicago,IL).
Results
Theoverallsampleconsistedof265womenagedbetween29 and85(meanSD,53.312.2)years.Mostwereoverweight(BMI, 28.85.1), multiparous (4.12.9 births), and postmenopausal (56.5%).Defecatorydysfunctionwasdiagnosedin36.6%(97/265) andfecalincontinencein30.4%(80/265).
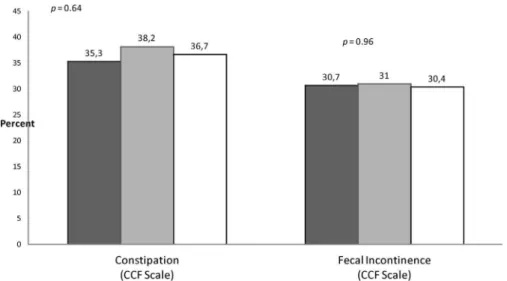
Ofthe265women, 149(56%)hadPOP-Qstage2and116(44%) hadPOP-Qstage<2posteriorprolapse(Bp).AsshowninTable1, womenwithPOP-Qstage2weresignificantlyolder(p=0.001) andhadsignificantlyhigherBMI(p=0.005),numberof pregnan-cies(p=0.01),numberofbirths(p=0.027),andoverallPOP-Qstage (p <0.001) than women with POP-Q stage <2. No significant differenceswereobservedbetweenthegroupsregarding propor-tionofpatientswithdefecatorydysfunction(POP-Qstage2=57/ 38.2%vsPOP-Qstage<2=41/35.3%/p=0.64)orincontinence (POP-Qstage2=45/30.2vsPOP-Qstage<2=36/31%/p=0.96)(Fig.1). No significant correlation was observed between the POP-Q assessment of severity of the prolapseof theposterior vaginal wall and theseverityof constipation asassessed withthe CCF constipationscores(p=0.19)andseverityoffecalincontinenceas assessedwithCCFincontinencescore(p=0.86)
AsshowninTable2,nodifferenceswereobservedbetweenthe twogroupsregardingpelvicfloormusclestrengthasassessedwith thePERFECTscheme,qualityoflifeassessedwiththeICIQ-SF,or sexualimpactasassessedwiththePISQ-12.Intheevaluationofthe SF-36, general health perception was significantly worse in patients withPOP-Q stage 2 than in those with POP-Qstage
<2(p=0.02),butnoothersignificantdifferenceswereobserved (Fig.2).
Discussion
Inourstudyof265womenattendinganoutpatient urogyne-cologyclinic,posteriorvaginalprolapsewassignificantlyrelatedto age,BMI,numberofpregnancies,andnumberofbirths.Themost important finding of our study was the lack of a clinically importantassociationbetweenthepresenceofposteriorvaginal prolapse and defecatory dysfunction or incontinence. We also foundnoassociationwithpelvicfloormusclestrengthorqualityof life, except that women with posterior vaginal prolapse had significantlyworsescoresontheSF-36subscaleforperceptionof generalhealth.
Theoverallprevalence ofanorectaldisorders inourpatients (constipation,36.7%;fecalincontinence,30.4%)wassimilartothat foundinotherseries[3–5].Soligoetal[14]founda32%prevalence ofconstipationinwomenwithurinarysymptomsand/orgenital prolapse.Inotherstudiesofwomenwithpelvicfloordysfunction, twothirdshadconstipationand31%to41%ofthepatientsreported experiencingepisodesofanalincontinence[1,6].
Resultsintheliteraturearecontroversial,Slieker-tenHoveetal. [24]foundPOPtobestronglyassociatedwithobstructivebowel disorders.Inapopulation-basedstudy,womenwithsymptomatic pelvic organ prolapse were two times more likely to report symptomsofobstructivedefecationthanthosewithoutprolapse. [12]Digesuetal.[5]andCollinsetal.[3]foundastrongcorrelation betweenposteriorprolapseasmeasuredbythePOP-Qsystemand bowel symptoms. However, Ellerkmann et al. [6] found that advancedposteriorvaginalwall prolapsewas weaklycorrelated withincompleteevacuationanddigitalmanipulation.Inastudyby Groenendijketal,[11]althoughPOPandprolapsesymptomswere weaklyassociated,nostrongrelationshipwasfoundbetweenthe affectedcompartmentanddefecationsymptoms.
Table1
Patients’demographicandclinicalcharacteristicsinrelationtoPOP-Qstage.
PosteriorPOP-Qstage(Bp)2n=149(56%) PosteriorPOP-Qstage(Bp)<2(n=116(44%) p*
MSD Minimum Maximum MSD Minimum Maximum
Age,y 56.011.7 35 85 50.912.3 29 81 0.001
Schooling,y 6.44.5 0 16 6.74.2 0 19 0.68
Income,BRL 1132776 102 4000 1230985 0 7000 0.53
BMI 27.85.2 16.0 42.3 29.84.8 19.7 47.1 0.005
Numberofpregnancies 5.23.2 0 18 4.33.1 0 15 0.01
Numberofbirths 4.43.0 0 17 3.72.8 0 15 0.03
Numberofvaginaldeliveries 3.83.1 0 17 3.22.9 0 15 0.08
NumberofCesareansections 406 0 3 305 0 2 0.25
Weightofthelargestnewborn,g 3850759 2000 6900 3820963 2200 5300 0.83
OverallPOP-Qstage 2.40.6 2 4 1.50.9 0 3 <0.001
BMI=bodymassindex;BRL=Brazilianreais;POP-Q=PelvicOrganProlapseQuantification;SD=standarddeviation. *Mann-Whitneytestforcontinuousnonparametricdata;Student’sttestforcontinuousparametricdata.
Table2
Pelvicfloormusclestrength,quality-of-life,andsexualimpactscoresinrelationtoPOP-Qstageoftheposteriorvaginalwall.
PosteriorPOP-Qstage(Bp)2n=149(56%) PosteriorPOP-Qstage(Bp)<2(n=116(44%) p*
Score MSD Minimum Maximum MSD Minimum Maximum
PERFECT 2.01.1 0 4 2.11.2 0 5 0.53
ICIQ-SF 12.26.8 0 21 14.25.1 0 21 0.07
PISQ 27.48.9 12 44 26.58.4 9 47 0.35
ICIQ-SF=InternationalConsultationonIncontinenceQuestionnaireShortForm;PERFECT=Power(or pressure,i.e.,strengthmeasuredby meansofa manometric perineometer),Endurance,Repetitions,Fastcontractions,EveryContractionTimed;PISQ=PelvicFloorandIncontinenceSexualImpactQuestionnaire;POP-Q=PelvicOrgan ProlapseQuantification;SD=standarddeviation.
*Mann-Whitneytestforcontinuousnonparametricdata.
Saksetal.[9]reportedthatwomenwithposteriorvaginalwall prolapseweremorelikelythanthosewithoutposteriorprolapseto reportobstructivesymptoms,andtherelationshippersistedeven aftercontrolling for confounding factorssuchas age,BMI, and concomitantapicalandanteriorvaginalwallprolapse.However, obstructivebowelsymptomswerenotassociatedwiththeseverity of prolapse. Weber et al. [7] found that approximately 80% of women with posterior vaginal prolapse reported one or more bowelsymptomsbut alsofoundnoassociationbetweenbowel symptomsandtheextentoftheprolapse.Theydid,however,finda weakly positive correlation between more advanced posterior vaginalprolapseandseverityofbowelsymptoms.
Consistent withourfindings, Jelovsek etal. [25] foundthat neitheroverallstageofPOPnorstageofposteriorvaginalprolapse was significantly associated with any of the functional bowel disorders, including constipation and its subtypes. Grimes and Lukacz[26]foundnocorrelationbetweensymptomsandrectocele size.Thislackofcorrelationwasalsoconfirmedradiographically with evacuation proctography [27]. Recently, Grimes et al. [8] concluded that they were unable to identify an obstructive defecatory symptom measure that correlates well with any
anatomic finding of posterior vaginal prolapse. Their study explored a variety of anatomic measures beyond the POP-Q. Furthermore,daSilvaetal.[13]couldnotprovideanyevidenceto support a relationship between the anatomic defect of the posterior vaginal wall and fecal symptoms even using anal physiological studies.Vaginal digitationwas theonly symptom significantly associatedwithtrue rectocele.Othersymptoms of obstructeddefecationwereassociated withstoolquality rather thanrectocele.Dietz[28]alsoconcludedthatstoolqualitymaybe of greaterrelevance in theetiology ofsymptoms ofobstructed defecationthanthepresenceofrectocele.
ThePOP-Qexamrepresentssignificantprogressincreatinga standard, reproducible means of physical evaluation of pelvic organprolapse.InthestudybyCollinsetal.[3]althoughthePOP-Q measurement at Bp correlated well with symptoms of stool trapping,theperinealbodylength(pb)didnot.Thismayindicate that, while women with clinically significantperineoceles may haveelevatedBpmeasurements,manywomenwithelevatedBp measurementsdonothaveperineoceles.ThePOP-Qexammaynot sufficientlydescribethisareaofthepelvicfloorwellenoughto diagnose perineoceles, which can often be palpated on Fig.1.Proportionofpatientswithdefecatorydysfunctionandfecalincontinenceinthetotalsample(n=265)andbystudygroup(x2test).
rectovaginalexaminationorvisualizedonMRI.Moreresearchis needed to evaluate whether additional standardized measure-mentsonpelvicexaminationcouldmorereliablyidentifyclinically significantrectaldefectsintotheperineum.
Severalauthors[7,9,11]havesuggestedthat,althoughposterior vaginalwallprolapseandobstructivebowelsymptomsfrequently coexist, posterior vaginal prolapse probably does not cause obstructivesymptoms.Ourfindingthatposteriorvaginalprolapse determined by physical examination was not associated with bowelsymptomsareconsistentwiththisconclusion. Dietz[27] concludedthatthecombinationofsymptomsresultingfromPOP, urinaryincontinence,andconstipationshareacommonetiology. AccordingtoGroenendijketal.[11]collagendisease,abnormally weak pelvic floor muscles due to childbirth, and pelvic floor neuropathymayplayarole.Morelongitudinalstudiesarerequired toassessthecausalrelationshipbetweenPOPandfecal inconti-nenceand/ordefecatorydisordersaswellasmultivariateanalyses thatcouldanalyzetheinteractionsamongpotentiallyimportant determinantsofdefecatorydysfunctionandfecalincontinence.
Nevertheless,inviewoftheconflictingresultsreportedinthe literatureinregardtotherelationshipofposteriorvaginalprolapse to defecatory dysfunction and fecal incontinence, this study provides that the POP-Q exam represented limited physical evaluationconcerningposteriorvaginalprolapseandsymptoms, despiteofdiferenceinpopulation,methodologyandquestionnaire applied. On the other hand, to identify dysfunctions in the posteriorcompartmentinvolvingobstructeddefecationsyndrome (rectocele,rectalintussusception,anismusand entero/sigmoido-cele)andfecalincontinencesymptoms(sphincterinjuryandnerve damage),it is necessary associate dynamic and morphological imagesandfunctionalinvestigations,suchasdynamicultrasound ormagneticresonanceimageanddefecography.
WefoundadecreasedperceptionofgeneralhealthontheSF-36 in women with posterior vaginal wall prolapse, but no other associationbetweenposteriorvaginalprolapseandqualityoflife. Varmaet al.[12]showedobstructivedefecationtobe indepen-dentlyassociated with a diminished general quality of life as measuredbytheSF-36,withagreaterimpactonmentalhealth than on physical health [12]. Wald et al. [29] also found that functionalconstipationhasasignificantimpactonQoL, particu-larlyinregardtomentalwell-being.InthestudybyJelovseketal. [30] women with advanced POP reported significantly lower qualityoflifeonthephysicalscaleoftheSF-12.Theyweremore likelytofeelself-conscious,lesslikelytofeelphysicallyattractive, lesslikelytofeelfeminine,andlesslikelytofeelsexuallyattractive thannormalcontrols.
Thibault et al. [31] found that the degree of POP was not statistically associated with sexual function, although urinary, pelvic,anddefecatorysymptomswereassociatedwithadecrease inacouple'ssexualwell-being.Weobservednodifferencein PISQ-12scoresbetweengroups;despitethedecreased perceptionof general health (SF-36) in women with posterior vaginal wall prolapse.Sexualfunctionmaybeinfluencedmoresignificantlyby factorsotherthandefecatorydysfunction.Moreover,thePISQ-12is designedforpatientswithurinaryincontinenceandPOPandmay nothavequestionsthatcandetectchangesinsexualqualityoflife relatedtofecalincontinenceordefecatorydisorders.
Conclusion
The lack of a clinically important association between the presenceofposteriorvaginalprolapseandsymptomsof constipa-tionoranalincontinenceleadsustoagreewiththeconclusionthat posteriorvaginalprolapseprobablyisnotanindependentcause defecatory dysfunction or fecal incontinence. We could get differentresultsifthissamplewashigherthanit.
Conflictofinterest
None.
Financialdisclaimer
Kathiane Lustosa, Leonardo Bezerra, Sthela Murad-Regadas: conceptionanddesignanddraftingthearticle.
JoséAnaniasV.Neto,CamilaM.Vasconcelos,SaraA.L.Karbage and Andreisa PaivaMonteiroBilhar: acquisitionand analysisof data.
Francisco Regadasand Sthela Murad-Regadas, Kathiane Lus-tosa,Leonardo Bezerra:analysisand interpretation of dataand revising.
References
[1]BezerraLR,VasconcelosNetoJA,VasconcelosCT,KarbageSAL,LimaAC,Frota
IPR,etal.Prevalenceofunreportedbowelsymptomsinwomenwithpelvic
floordysfunctionandtheimpactontheirqualityoflife.IntUrogynecolJ
2014;25:927–33.
[2]HaylenBT,deRidderD,FreemanRM,SwiftSE,BerghmansB,LeeJ,etal.An
InternationalUrogynecologicalAssociation(IUGA)/InternationalContinence
Society (ICS) joint report on the terminology for female pelvic floor
dysfunction.NeurourolUrodyn2010;29:4–20.
[3]Collins SA, O'Sullivan DM, Lasala CA. Correlation of POP-Q posterior
compartment measures with defecatory dysfunction. Int Urogynecol J
2012;23:743–7.
[4]CundiffGW,FennerD.Evaluationandtreatmentofwomenwithrectocele:
focus on associated defecatory and sexual dysfunction. Obstet Gynecol
2004;104:1403–21.
[5]DigesuGA,ChalihaC,SalvatoreS,HutchingsA,KhullarV.Therelationshipof
vaginalprolapseseveritytosymptomsandqualityoflife.BJOG2005;112:971–
6.
[6]EllerkmannRM,CundiffGW,MelickCF,NihiraMA,LefflerK,BentAE,etal.
Correlationofsymptomswithlocationandseverityofpelvicorganprolapse.
AmJObstetGynecol2001;185:1332–8.
[7]WeberAM,WaltersMD,BallardLA,BooherDL,PiedmonteMR.Posterior
vaginalprolapseandbowelfunction.AmJObstetGynecol1998;179:1446–9
discussion1449–1450.
[8]GrimesCL,Tan-KimJ,NagerCW,DyerKY,MenefeeAS,DiwadkarGB,etal.
Outcomemeasurestoassessanatomyandfunctionoftheposteriorvaginal
compartment.IntUrogynecolJ2014;25:893–9.
[9]SaksEK,HarvieHS,AsfawTS,AryaLA.Clinicalsignificanceofobstructive
defecatorysymptomsinwomenwithpelvicorganprolapse.IntJGynaecol
Obstet2010;111:237–40.
[10]DuaA,RadleyS,BrownS,JhaS,JonesG.Theeffectofposteriorcolporrhaphyon
anorectalfunction.IntUrogynecolJ2012;23:749–53.
[11]GroenendijkAG,BirnieE,RooversJP,BonselGJ.Contributionofprimarypelvic
organprolapsetomicturitionanddefecationsymptoms.ObstetGynecolInt
2012;2012:798035.
[12]VarmaMG,HartSL,BrownJS,CreasmanJM,VanDenEedenSK,ThomDH.
Obstructivedefecationinmiddle-agedwomen.DigDisSci2008;53:2702–9.
[13]daSilvaGM,GurlandB,SleemiA,LevyG.Posteriorvaginalwallprolapsedoes
notcorrelatewithfecalsymptomsorobjectivemeasuresofanorectalfunction.
AmJObstetGynecol2006;195:1742–7.
[14]SoligoM,SalvatoreS,EmmanuelAV,DePontiE,ZoccatelliM,CorteseM.
Patternsofconstipationinurogynecology:clinicalimportanceand
patho-physiologicinsights.AmJObstetGynecol2006;195:50–5.
[15]BumpRC,MattiassonA,BoK,etal.Thestandardizationofterminologyof
femalepelvicorganprolapseandpelvicfloordysfunction.AmJObstetGynecol
1996;175:10–7.
[16]DevreeseA,StaesF,DeWeerdtW,etal.Clinicalevaluationofpelvicfloor
musclefunctionincontinentand incontinentwomen.NeurourolUrodyn
2004;23(3):190–7.
[17]BarberMD,BrubakerL,NygaardI,Wheeler2ndTL,SchafferJ,ChenZ.Defining
successaftersurgeryforpelvicorganprolapse.ObstetGynecol2009;114:600–
9.
[18]AgachanF,ChenT,PfeiferJ,ReissmanP,WexnerSD.Aconstipationscoring
systemtosimplifyevaluationandmanagementofconstipatedpatients.Dis
ColonRectum1996;39:681–5.
[19]JorgeJM,WexnerSD.Etiologyandmanagementoffecalincontinence.Dis
ColonRectum1993;36:77–97.
[20]TalaszH,KremserC,KoflerM,KalchschmidE,LechleitnerM,RudischA.
Phase-lockedparallelmovementofdiaphragmandpelvicfloorduringbreathingand
coughing-adynamicMRIinvestigationinhealthyfemales.IntUrogynecolJ.
2011;22:61–8.
[21]CiconelliRM, Ferraz MB, Santos W, Meinao I, Quaresma MR.
Brazilian-PortugueseversionoftheSF-36:Areliableandvalidqualityoflifeoutcome
measure[Traduc;aoparaalfnguaportuguesaevalidac;aodoquestionario
genericodeavaliac;aodequalidadedevidaSF-36(BrasilSF-36)].RevBras
Reumatol1999;39:143–50.
[22]TamaniniJTN, DambrosM,D’AnconaCAL.Valida’ço paraoportuguãs do
êInternationalConsultationonIncontinenceQuestionnaire-ShortForm“
(ICIQ-SF) Validation of the êInternational Consultation on Incontinence
Questionnaire-ShortForm“ (ICIQ-SF)forPortuguese.RevSaudePublica
2004;38:438–44.
[23]SantanaGWRM.Validação paraoportuguêsdoquestionáriosexualpara
incontinênciaurinária/prolapsodeórgãospélvicos[PelvicOrganProlapse/
UrinaryIncontinenceSexualQuestionnaire–PISQ–12].SãoPaulo:Dissertação
deMestradoFaculdadedeCiênciasMédicasdaSantaCasa-SP;2010.
[24]Slieker-tenHoveMC,Pool-GoudzwaardAL,EijkemansMJ,
Stiegers-Theuwis-senRPM,BurgerCW,VierhoutME,etal. Theprevalenceofpelvicorgan
prolapsesymptomsandsignsandtheirrelationwithbladderandbowel
disordersin a generalfemale population. Int Urogynecol J Pelvic Floor
Dysfunct2009;20:1037–45.
[25]Jelovsek JE, Barber MD, ParaisoMF, Walters MD.Functional bowel and
anorectaldisordersinpatientswithpelvicorganprolapseandincontinence.
AmJObstetGynecol2005;193:2105–11.
[26]GrimesCL,LukaczES.Posteriorvaginalcompartmentprolapseanddefecatory
dysfunction:aretheyrelated?IntUrogynecolJ2012;23:537–51.
[27]KelvinFM,MaglinteDD.Dynamiccystoproctographyoffemalepelvicfloor
defectsandtheirinterrelationships.AJRAmJRoentgenol1997;169:769–74.
[28]DietzHP.Rectoceleorstoolquality:whatmattersmoreforsymptomsof
obstructeddefecation?TechColoproctol.2009;13:265–8.
[29]WaldA,ScarpignatoC,KammMA,Mueller-LissnerS,HelfrichI,SchuijtC,etal.
Theburdenofconstipationonqualityoflife:resultsofamultinationalsurvey.
AlimentPharmacolTher2007;26:227–36.
[30]JelovsekJE,BarberMD.Womenseekingtreatmentforadvancedpelvicorgan
prolapsehavedecreasedbodyimageandqualityoflife.AmJObstetGynecol
2006;194:1455–61.
[31]ThibaultF,WagnerL,RouvellatP,SeniG,BrouziyneM,TyracdeR,etal.[Sexual
function beforesurgeryfor pelvicorganprolapse] Prolapsusuro-génital:
analysedelasexualitépréopératoire.ProgUrol2012;22:665–70.