REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologia www.sba.com.brSCIENTIFIC
ARTICLE
Anesthesia
recovery
comparison
between
remifentanil-propofol
and
remifentanil-desflurane
guided
by
Bispectral
Index
®monitoring
Raphael
Grossi
Rocha
a,∗,
Eduardo
Giarola
Almeida
b,
Lara
Moreira
Mendes
Carneiro
b,
Natália
Farias
de
Almeida
b,
Walkíria
Wingester
Vilas
Boas
b,
Renato
Santiago
Gomez
aaUniversidadeFederalMinasGerais(UFMG),FaculdadedeMedicina,CentrodePós-graduac¸ão,BeloHorizonte,MG,Brazil bUniversidadeFederalMinasGerais(UFMG),HopitaldasClínicas,DepartamentodeAnestesia,BeloHorizonte,MG,Brazil
Received28February2016;accepted14October2016 Availableonline20February2017
KEYWORDS
Anesthesiarecovery; Desflurane;
Propofol; Intravenous anesthesia;
Balancedanesthesia
Abstract
Backgroundandobjectives: Thereisastrongdemandforfastandpredictableanesthesia recov-ery with few sideeffects. Choice of the hypnotic agent could impact on that. This study investigatedthedifferencesbetweenrecoveriesafterremifentanil-propofoland remifentanil-desfluraneanesthesiasguidedbybispectralindex(BIS®).
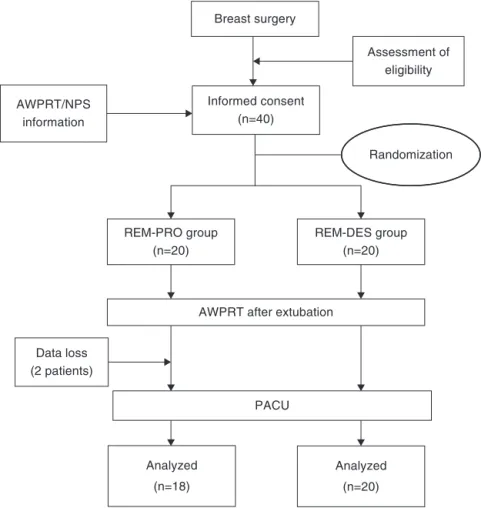
Methods:Fortypatients wererandomly assigned into 2groups according tothe anesthesia techniqueapplied: remifentanil-propofol(REM-PRO) andremifentanil-desflurane (REM-DES). Afterthediscontinuationoftheanesthetics,thetimestoextubation,toobeycommandsandto recovertheairwayprotectionreflexwererecorted.Inthepost-anestheticrecoveryroom(PACU) itwasrecordedtheoccurrenceofnauseaandvomiting(PONV),scoresofRamsaysedationscale andofnumericpainscale(NPS),morphinedoseandlengthofstayintheunit.
Results:Datafrom38patientswereanalyzed:18fromREM-PROand20fromREM-DESgroup. Anesthesiatimes were similar(REM-PRO=193min,SD79.9vs. 175.7min,SD 87.9REM-DES;
p=0.5).REM-DEShadshortertimesthanREM-PROgroup:timetofollowcommand(8.5min;SD 3.0vs.5.6min;SD2.5;p=0.0)andextubationtime(6.2min;3.1---8.5vs.9.5min;4.9---14.4;
p=0.0). Timesto recoverairway protectivereflexwere similar: 16 patients fromREM-PRO (88.9%) restored the airway protective reflex 2min after extubation vs. 17 from REM-DES (89.5%);and2patientsfromREM-PRO(11.1%)vs.2fromREM-DES(10.5%)6minafter extu-bation,p=1.Ramsaysedationscore,NPS,PONVincidents,morphinedoseandPACUstayof lengthPACUwerealsosimilar.
∗Correspondingauthor.
E-mail:raphaelgrossi@gmail.com(R.G.Rocha). http://dx.doi.org/10.1016/j.bjane.2016.10.001
Conclusion: Remifentanil-desflurane-based anesthesia has a faster extubation time and to followcommandthanremifentanil-propofol-basedanesthesiawhenbothguidedbyBIS®. ©2016SociedadeBrasileiradeAnestesiologia.Publishedby ElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
PALAVRAS-CHAVE
Recuperac¸ão pós-anestésica; Desflurano; Propofol; Anestesia intravenosa;
Anestesiabalanceada
Comparac¸ãodarecuperac¸ãopós-anestésicaentreremifentanil-propofole remifentanil-desfluranoguiadapelamonitorac¸ãodoÍndiceBispectral®
Resumo
Justificativaeobjetivos: Háumafortedemandaporrecuperac¸ãopós-anestésicarápidae pre-visívelcompoucosefeitosadversos.Aescolhadoagentehipnóticopodeinfluenciarisso.Este estudoinvestigouasdiferenc¸asdarecuperac¸ãonopós-operatórioentreastécnicasanestésicas comremifentanil-propofolecomremifentanil-desfluranoambasguiadaspeloíndicebispectral (BIS®
).
Métodos: Foramrandomicamentedistribuídos40pacientesem doisgrupos deacordocoma técnicaanestésicaaplicada:remifentanil-propofol(REM-PRO)eremifentanil-desflurano (REM-DES). Após adescontinuac¸ão dos anestésicosforam registrados ostempos para extubac¸ão, obedeceracomandoserecuperaroreflexodeprotec¸ãodasviasaéreas.Nasaladerecuperac¸ão pós-anestésica(SRPA)foiregistradoaocorrênciadenáuseasevômitos(NVPO),osescoresna escaladesedac¸ãodeRamsayenaescalanuméricadedor(END),adosedemorfinautilizadae otempodepermanêncianestaunidade.
Resultados: Osdadosde38pacientesforamanalisados:18dogrupoREM-PROe20dogrupo REM-DES.Ostemposdeanestesiaforamsemelhantes(REM-PRO=193minutos,DP79,9vs.175,7 minutos,DP87,9REM-DES;p=0,5). OgrupoREM-DESapresentoutemposmaiscurtosque o grupoREM-PRO:tempoparaobedeceracomandos(8,5minutos;DP3,0vs.5,6minutos;DP 2,5;p=0,0)etempo deextubac¸ão(6,2minutos;3,1-8,5vs.9,5minutos;4,9-14,4;p=0,0). Ostempospara recuperac¸ãodo reflexodeprotec¸ão dasviasaéreasforamsemelhantes:16 pacientesdogrupoREM-PRO(88,9%)recuperaramoreflexodeprotec¸ãodasviasaéreasdois minutosapósaextubac¸ãovs.17dogrupoREM-DES(89,5%)edoispacientesdogrupoREM-PRO (11,1%)vs.doisdoREM-DES(10,5%)seisminutosapósaextubac¸ão,p=1.OsescoresdeRamsay, NPS,aincidênciadeNVPO,adosedemorfinaeotempodepermanêncianaSRPAtambémforam semelhantes.
Conclusão:Aanestesiacomremifentanil-desfluranotemumperfilderecuperac¸ãodaanestesia pós-anestésicamaisrápidoqueodaanestesiacomremifentanil-propofolquandoambasguiadas peloBIS®.
©2016SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigo OpenAccess sobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
The short-acting anesthetics, such as propofol and des-flurane, provide safe and effective anesthesia with few sideeffectsand rapidrecovery.Desfluranehasthelowest blood/gaspartition coefficient amongvolatile anesthetics andenablesagreaterintraoperativeanesthesiacontrolwith low inter-individual variability.1 In turn, total intravenous
anesthesia(TIVA)withpropofolalsoprovidesquick anesthe-siaemergenceandlowerincidenceofpostoperativenausea andvomiting(PONV).2---4
The level of anesthesia (whether superficial or deep) influencesanesthesiarecovery.1Thebispectralindex(BIS®
) isanelectroencephalogramderivedscalefirstlydeveloped for monitoring the level of consciousness amongpatients receiving general anesthesia and sedation.5 Recently,
BIS® monitoring has also proved to be also useful to control anesthesia depth, reduce drug consumption,
shorten anesthesia recovery and decrease adverse effects.5,6
Thereisastrongdemandforfasteranesthesiarecovery, asaquicker recovery maybe associatedwith earlierand bettercareofpatentairways,moreprotectionagainst aspi-ration, and greater oxygenation.1 These are essential for
ambulatory anesthesia6,7 and alsoin other circumstances,
such as in elderly, obese and critical patients.1 From an
economic perspective, aquick anesthesia recovery favors fast-tracking, increases case turnover and may improve resourceuse.1
Early anesthesia recovery has been clinically assessed afteranestheticdiscontinuationbytimetofollowcommand; extubation time and protective airway reflex restora-tion after extubation. Evidences suggest that desflurane offersshorterearlyanesthesiarecoverythanpropofol-based anesthesia.7---9However,moststudieshadsomebiasdueto
Objectives
The choice of the hypnotic agent could impact on early recovery,not only due to differences in pharmacokinetic profile but also in pharmacodynamics. In the present studywe testedthehypothesis thatremifental-desflurane balanced anesthesia has a shorter extubation time (pri-mary endpoint) than total intravenous anesthesia with remifentanil-propofolwhen both guidedby BIS®.The sec-ondary endpointswere time to follow command; time to recoverthe protectiveairwayreflexafterextubation;use ofvasopressorsduring thesurgeryandthe patient’svitals atthePost-AnesthesiaCareUnit(PACU).
Methods
Trialdesign
Thiswasaunicenter,non-stratified,double-blind,with1:1 randomization,clinicalprospectivetrialconductedina qua-ternarylevelhospitalinBrazil.
Participants
Eligible participants were all female adults were over 18 years of age, classified by the American Society of
AnesthesiologistsasphysicalstatusIorII,undergoing elec-tivebreastsurgerywithgeneralanesthesia.
Exclusion criteria were history of: chronic use of any psychoactivedrug;pregnancyoncourseorsuspicionof; neu-romusculardisorders;cerebralvasculardisease;dysphagia; dysphonia;gastroesophagealrefluxdisease;previouslarynx and/or uppergastrointestinaltractsurgery;allergytoany drugtobeusedandmalignanthyperthermia.Patientswho developed hemodynamicinstability duringsurgery,and/or potential need for bloodtransfusions wereexcluded from thestudy.Patientsunabletoswallow20mLofwaterinan uprightpositionwerealsoexcluded.
Studysetting
ThisstudywasconductedintheHospitaldasClínicasofthe
UniversidadeFederaldeMinasGerais,Brazil,fromJulyuntil Novemberin2015.TheFig.1showsaflowchartthatoutlines patientselection,randomizationandanalyses.
Interventions
Upon enrollment, all subjects were familiarized with the numerical painscale (NPS), scoreof ‘‘0’’representingno pain and score of ‘‘10’’ the worst pain imaginable, and tested for ability to swallow 20mL of water (protective airway reflex test). Swallowing was judged successful if
Breast surgery
REM-DES group (n=20) REM-PRO group
(n=20)
Informed consent (n=40)
Assessment of eligibility
AWPRT/NPS information
Data loss (2 patients)
Analyzed
(n=18)
Analyzed
(n=20)
Randomization
AWPRT after extubation
PACU
nocoughing or drooling occurred after water passed into patient’smouth andnowaterremainedinheroropharynx uponsubsequentvisualinspection.11,12
In the operatingroom(OR),patients fromboth groups were monitored with EKG, pulse oximetry, non-invasive blood pressure (NIBP) and end-tidal measurements (ET) of desflurane,oxygenand carbondioxide (CO2).
Mechani-calventilationwassettotargettheseparameters:ETCO2 between 30 and 40mmHg; FiO2=30%, oxygen saturation
(SpO2)≥97%.AnesthesiadepthwastitratedwithBIS
mon-itoring(BIS VISTA® Monitoring System, USA) toobtain the valuesbetween40and60intra-operatively.Neuromuscular blockadewasguidedbytrain-of-fourmonitoring(TOF). Infu-sionworkstationwasOrchestra® BasePrimeawithModules DPS(FreseniusVialS.A.S.,France).Thetipofthe temper-atureprobewasplacedinthepatients’nasopharyngealfor temperaturemonitoring.
General anesthesia was standardized. In both groups, remifentanilwastheonlyopioidusedforanesthesia induc-tion and maintenance. Target-controlled infusion (TCI) mode was set and remifentanil administration was based on Minto’s pharmacokinetic model.13 An effect-site
tar-get of 5ng.mL−1 wassetfor induction. Adjustments were
made according toestablished BIS value range.Lidocaine 1.5mg.kg−1, was given intravenously (I.V.) before
propo-foladministration.Atracuriumwasthesoleneuromuscular blockingagentused.Abolusof0.5mg.kg−1I.V.was
admin-istered to patients in both groups after unconsciousness, definedby loss of the eyelidreflex. Intubationwas made only when train-of-four (TOF) stimulation monitor on the ulnarnervewaszero.
IntheREM-PROgroup,afterremifentanilandlidocaine infusions, propofol plasma-site TCI of 5g.ml−1 (Marsh’s
pharmacokineticmodel)wassetforinduction andajusted accordingtoBIS® values.14
In the REM-DES group, after remifentanil and lido-caine infusions, a bolus of propofol 1.5---2.5mg.kg−1 I.V.
was administered until loss of consciousness. Anesthesia maintenancewasdonewithdesflurane(Desflurane Dräger vaporizerD-Vapor3000).Adjustmentsweredoneaccording toestablishedBIS® valuerange.
Hemodynamic instability was defined by systolicblood pressure below 90mmHg, despite volume loading and intermittentusingofvasopressors.Bloodtransfusiontarget was set at 8g.dL−1 or whenever the anesthesia provider
judgednecessary.
The post-operative pain protocol consisted of: dexa-methasone 10mg I.V. (except for diabetics), ketoprofen 100mg I.V.(except for patients over 60 years of age, or withchronic renaldiseaseor usingangiotensin-converting enzyme inhibitors), metamizol (Dipirona®) 2.0g I.V. and morphine 0.1mg.kg−1 I.V. In addition to dexamethasone,
4.0mgI.V.wereusedforPONVprophylaxis.
Before discontinuinganesthetics, TOF shouldbe above 90%. If not, atropine 0.02---0.04mg.kg−1 I.V. and
neostig-mine0.04---0.06mg.kg−1 I.V.boluseswere administeredto
achieveit.
Outcomes
The primary endpoint was the extubation time, defined by the discontinuation of anesthetic delivery until the
endotracheal tube cuff deflation. When the anesthetics were discontinued, the fresh gas flow was set above patient’s respiratory minute volume. Patients were extu-batedwhenhavingrespiratoryrategreaterthan12breaths perminute; tidalvolumeabove6mL.kg−1,SpO
2≥97%and
followingacommandorheavilycoughingduringanesthesia emergence.
Thesecondaryendpointsandtheirdefinitionswereas fol-lows:anesthesiatime(timefrominductionuntilanesthetics discontinuation)and time tofollow command (time from anestheticsdiscontinuationtofollowastandardcommand). This commandconsisted of ‘‘patient’s name,squeeze my hand!’’ and was said to each patient by the anesthesia provider every 15s from anesthetic discontinuation until patient’sanswer.
The time to recover the protective airway reflex was evaluatedbytheprotectiveairwaytest,describedearlier, at2,6,14,22and30minafterextubationuntilthefirst suc-cessfulpatient’sattempt.Toperformsuchtest,thepatient waspositionedat 60◦ upright positiononthesurgical bed
and asked to swallow 20mL of water. Protective airway reflexwasconsideredrestoredifswallowingwasadequate (describeabove).
At the PACU,patients were monitored withEKG, SpO2
and NIBP. A blind observer evaluated the patients on admissionandevery5minafterwarduntilbeingdischarged. Measuredoutcomesalsoincludedvitalsigns;Ramsayscale sedation; NAS and PONV scale (1=no symptoms; 2=mild to moderate nausea and/or vomiting, not needing anti-emetics; 3=severe nausea and/or vomiting, anti-emetics needed;4=severenauseaand/orvomiting,notresponding toanti-emetics).
Samplesize
Samplesizewascalculatedbasedontheprimaryoutcomeof thestudy(extubationtime).Accordingtopreviousstudy,15
adifferenceof3.1mininmeanextubationtimefrom propo-folanddesfluranewithastandarddeviation(SD)of3.0min were considered clinically significant. Sample size calcu-lationrevealed that 17 subjects per group were required toachievea powerof 85% withatypeone errorof 0.05. Becauseofthepotentiallossofpatientsalongthestudy,we included20patientsoneachgroup.
Randomization
The randomization scheme was developed by a com-puterprogramMicrosoftExcel® 2013(Microsoft,Redmond, USA) and covered in sealed envelopes. These envelopes were prepared by an independent anesthesiologist who was not associated with study. Patients were allocated into two groups according to its anesthetic regime: remifentanil-propofol (REM-PRO group) or remifentamil-desfluraneanesthesia(REM-DESgroup).
Blinding
Table1 DemographiccharacteristicsoftheREM-PROandREM-DESgroups.
REM-PRO REM-DES p-value
n Mean Median % n Mean Median %
Age(years) 19 56.3(±15.2) 20 46.7(±11.1) 0.03a Weight(kg) 19 65.4b 62.2(51---92.5) 20 72.4(±19.2) 69.5(43.9---106.5) 0.04
Height(m) 19 1.55(±0.1) 20 1.6(±0.08) 0.08
BMI(kg.m−2) 19 28.6(±5.0) 20 29(±6.1) 0.62
ASAI 4 21.1 8 40 0.15
ASAII 15 78.9 12 60
Mean(±SD);Median(Minimum---Maximum);BMI,bodymassindex;ASA,AmericanSocietyofAnesthesiologists’physicalstatusclassification system.
aSignificantdifference. b Non-normaldistribution.
Table2 Anesthesiatime,timetofollowcommandsandextubationtimeintheREM-PROandREM-DESgroups.
REM-PRO(n=18) REM-DES(n=20) p-value Anesthesiatime(min) 193.5(±79.9) 175.7(±87.9) 0.52 Timetofollowcommand(min) 8.5(±3.0) 5.6(±2.5) 0.00a
Extubationtime(min) 9.5b(4.9---14.4) 6.2(3.1---18.5) 0.00a
Mean(±SD);Median(Minimum---Maximum).
aSignificantdifference. b Non-normaldistribution.
Statisticalmethods
Dataarepresentedasmeanswithstandarderrors(in paren-theses)for variablewithnormaldistribution.Forvariables withnon-normal distribution,data areshowed with max-imumandminimum values.Differencesin recovery times between the desflurane and propofol groups were com-paredusingcontingencytableswithchi-squaredanalysisor Fisher’s exact test. For continuous variables (duration of anesthesiaand extubation time), a two-tailed t-test was used.Ordinaldataandnon-Gaussiancontinuousdatawere compared between groups using the Mann---Whitney test. AllstatisticswereperformedusingSPSSStatisticssoftware (IBM,Armonk,USA)
Results
DemographicdataareshowedinTable1.Bothgroupswere homogeneous,exceptfrompatientmeanages(p=0.03).
Data from one patient from REM-PRO group were lost andexcludedfromanalysis.AnotherpatientfromREM-PRO groupawokeveryagitated,preventingfurtherassessment. Onlyherdemographicdatawereincludedintheanalysis.
TheREM-PROandREM-DESmeananesthesiatimeswere similar(p=0.52).However,thePearsoncorrelationanalysis (agevs. extubationtimeand age vs.timetofollow com-mand)revealedthatagehadnoinfluenceontheoutcomesin eithergroup(p>0.05).Therewasnodifferencebetweenthe groupsregardingtheanesthesiatimes(Table2),193.5min (±79.9)vs.175.7min(±87.9)fortheREM-PROandREM-DES respectively.IntheREM-PROgroup,themeantimetofollow command was 8.5min (±3.0), whereas in the REM-DES, it was5.6min (±2.5),p-value=0.003.This representeda
difference of 2.9min (Table 2). In the REM-PRO group, median time to extubation was 9.5min (4.9---14.4), while in the REM-DES was 6.2min (3.1---18.5), p-value=0.012 (Table2).
Theairwayprotectiontestresultsweresimilarbetween the REM-PRO and REM-DES groups. Among the patients fromREM-PROgroup, 16(88.9%) and2(11.1%) succeeded in the airway protection test at the 2nd and 6th minute aftertheextubationrespectively.Similarly,intheREM-DES group,17(89.5%)and2(10.5%)patients succeededinthe airwayprotectiontest2ndand6thminuteafterthe extuba-tionrespectively.OneparticipantfromtheREM-DES group refusedtodothetestaftertheextubation.
Therewasnodifferencein theuseof vasopressor dur-ingsurgerybetweentheREM-PROandREM-DES groupsfor hypotensiontreatment.Ineachgroup,cardiovasculardrugs wereused4timesasawhole,representing21.1%and20% respectively(p=1).
OnPACUadmissionandatthefollowing15and30min,no statisticalsignificantdifferencewasfoundinanymeasured outcomes:episodesofhypotension(definedbymean arte-rialNIBPlessthan60mmHg)andbrady/tachycardia(defined by heart rate lower than 60 or higher 100bpm); use of supplemental oxygen, NPS, Ramsay sedationscale scores, episodesofPONV.Transportationtimebetweenextubation andPACU admission;dose ofmorphine inthe PACU; max-imum PACU stay times were also not statically different betweenthegroups.
Discussion
REM-DESgroup,inotherwords,51.7%and53%longer respec-tively.Differencesintimetofollowcommand(oremergence time) and extubation time among anesthetics are exten-sively studied,7,9,16 although the best strategy for short
anesthesia emergence and extubation time has not been defined.7,17
It isknownthatthe advantagesof oneanestheticover anothermay not necessarilytranslate into rapidrecovery from anesthesia, especially if the patient received other drugsthatcouldtendtoequalizedifferencesbetweenthese anesthetics.7,16 Therefore,inthisstudy,nopre-medication
was given prior to the surgery and remifentanil was the soleopioidadministrated,differingonlyinhypnoticagents applied. Unlike other studies,7,9,16,18 the addition of BIS®
monitoringhelpedtheanestheticadministration,sincethe use of somatic and autonomic monitoring to judge the dosage ofanesthetic agents canlead toeither anesthetic overorunderdosage.Inameta-analysis,Liuetal. demon-stratedthatBIS®monitoringconsistentlyreducedanesthetic use by 19% compared with standard clinical practice for ambulatory anesthesia.6 In another meta-analysis,
Punja-sawadwong et al. showed that BIS monitoring reduced anesthetic consumption: a decrease of 1.32mg.kg−1.h−1
and 1.02 MAC equivalents for propofol and desflurane respectively.5 Thus, in the present study, all patients
weresubjectedtosimilaranesthesiadepththroughoutthe surgery,andthetimestofollowcommandandthe extuba-tiontimesweremeasuredatcomparableanesthesiadepth. Giventhat,thequickerrecoveryintheREM-DESgroupcould onlybetheresultofthedifferencesinpropofol’sand des-flurane’spharmacology.
In a study, BIS® monitoring reduced all components of early post-anesthesia recovery: time to eye opening (1.93min),timeforresponsetocommand(2.73min),time toextubation(2.62min)andtimetoorientation(3.06min).5
OurfindingsarealsoinaccordancewiththestudyofGupta etal.7thatsystematicallyreviewedpost-anesthesia
recov-ery profiles in ambulatory setting with many anesthetics and found that the time to follow command was 1.3min quickerwithdesfluranethanwithpropofol-based anesthe-sia.Ameta-analysisconductedbyWachteletal.reported 23% and 21%reductions in the mean timeto follow com-mand and the mean extubation time, respectively, with desflurane.9 Desflurane hasalsoa more predictable
anes-thesia emergence,sinceit reducedthevariabilityin time toextubationand in followingcommand by26% and 39%, respectively,incomparisonwithpropofol.9InterestinglyWu
etal.18reportedthatpropofol-basedTIVAreducedthemean
timetoextubation byatleast9% incomparisonwith des-flurane.Inthisstudy,however,itisimportanttonotethat BIS® monitoringwasnotused,caseswereranbydifferent anesthesiologists,ahighgasflowwasnotsetafterturning off thedesfluranevaporizer andpatients received repeti-tivebolusesofneuromuscularblockingagentandfentanyl asnecessarythroughouttheprocedures.Alloftheseaspects coulddelaypost-anesthesiaearlyrecovery.7
Anesthesia recovery has been demonstrated to be dependent on many factors, in particular the anesthesia durationand depthand alsoonpatient’s characteristics.1
Juvinetal.compareddesflurane-basedwithpropofol-based anesthesiainmorbidlyobesepatientsandshowedthat des-fluranedecreasedearlyrecoverytimesby60%(6.5min)for
timetoeye opening;57%(7.6min)for timetoextubation and58%(8.6min)fortimetostatingname.Ameta-analysis conductedbyLiuetal.8alsofoundthat,inobesepatients,
desflurane-basedanesthesiatooklesstimetorespondtoa commandandtoopentheireyesthanwithpropofol-based anesthesia.
Thepharmacoeconomicaspectsofusingdifferent anes-theticswerenot addressedin thepresent study.The cost ofthenewanesthetics,inparticulardesflurane,isagreat concern.However,althoughthedirectdrugconsumptionis theeasiest wayof assessing thecosts, anesthesia-related expensesaremuchbroader.Notonlydrugsshouldbetaken intoconsideration,butalsopersonnel,equipmentusedfor druginfusion andanesthesiamonitoring, surgicalaspects, anesthesiarecoveryanddischargetimes.1Infact,
anesthet-icsconstitutelessthan4%ofthetotalanestheticcostsfor shortcaseprocedure,19 whereasorganizationaland
opera-tionalissues,especiallypersonal costs,haveafar greater impactonoverallspendingandmayaccountfortwo-thirds oftotalanestheticexpense.20Additionally,theuseof
desflu-ranehasbeenshowntodecreasedirectcostsincomparison withTIVA,especiallywhenconsideringwastage.1,4
Further-more, reducing fresh gas flow has a profound effect on inhaledanestheticconsumption.1
AccordingtoDexteretal.,21 extubationtimeinfluences
operation room (OR) workflow: longer extubation times increasetheoddsofatleastonepersonbeingidleintheOR (waitingfortrachealextubation),therebyslowingworkflow. Reductioninextubationtimemaydecreasethelaborcosts oftheORuse time.22 This maybethecase inprocedures
withlongextubationtime,whentheextubationtimeisthe bottlenecktothepatientleavingtheOR,or whentheOR isoverutilizedorbookedformorethan8handthestaffing canbereducedto8h.22Still,thegreatestreductionindirect
costwillapplytohospitalsatwhichallORsareconsistently overutilized.Inanysituation,eachminutedecreases from OR time reduces from 1.1 to 1.2min in overall regularly scheduled labor costs.22 Consequently, a small reduction
in OR timeby reducing the extubation time, as reported inthisstudy,wouldreasonablybeconsidered asasaving, sinceourusualORworkdayislongerthan8h.Additionally, a faster and more predictable post-anesthesia recoveries mayleadtointangiblebenefits,forinstance:fewerunhappy surgeonscomplainingtohospitaladministrators.22
Interest-ingly,whensurgeonsscoreanesthesiologists’attributesona scalefrom0,‘‘noimportance’’,to4,‘‘afactorthatwould makemeswitchgroups/hospital’’,theiraveragescoreis3.9 wheninquiredfor‘‘patientquicktoawaken’’.23
There was no difference in the use of cardiovascular drugs in either group. This shows that hemodynamic sta-bilitywassatisfactorilyprovidedbythesimilaranesthetic levelofeach ofthemaintenanceregimesasalsoreported byCamcietal.24
Mckayetal.11,12demonstratedthatdesfluraneallowsan
earlierreturnofprotectiveairwayreflexesthansevoflurane. Consequently,ourhypothesiswasthatashorteremergence andextubation times withdesfluraneanesthesia, in com-parison with propofol, would also translate into a faster recoveryoftheprotectiveairwayreflexes.However,whenit testedinthisstudy,theresultsweresimilarinbothgroups. Instudies performed by Mckayet al.,11,12 midazolam was
neededthroughouttheproceduresandnoBIS® monitoring wasappliedtobothstudies.Incontrast,inthepresentstudy, nopre-medicationwasgiven,ashort-livedopioid (remifen-tanil)wasadministeredandBIS® monitoringwasusedinall patients.Onecouldspeculatethatthesefactorsmighthave diminished the differences on protective airway reflexes betweenthegroupsevaluated.
At thePACU, theintermediated post-anesthesia recov-eryprofilewereakininbothgroups.Vitalsignswerestable inaccordancewithastudyconductedbyLoopandPriebe.4
Still, levelof sedation wassatisfactoryin both groups, as showedbythepredominanceof theRamsayscoreof 2on admission,after 15and 30min. Because of therapid off-setofactionofremifentanil,immediatepostoperativepain wasagreatconcern.Painscoresweresimilarinbothgroups in agreement with other studies.25,26 However, although
ourpaincontrolprotocolpraisedmultimodalpain manage-ment,thehighpainscores(NPS>5)observedinbothgroups throughoutthePACUstayindicatespoorpaincontrol. Dia-betic,elderly patients,angiotensin receptor blockersand angiotensin-convertingenzymeinhibitortakers,which rep-resentedasignificantfractionofourpatients(28.9%),did notreceiveeitherketoprofen ordexametasoneor both,a factthatmayexplainthehighpainscoresnotedreported. Anotherconcernregardsdesfluraneanditshigherincidence of PONVin comparison withpropofol.27 Despitethat, the
incidenceswereequalinbothgroupsinthepresentstudy. TheuseofBIS®monitoringalsoexplainsthisfindingas meta-analysis demonstrated that it reduces the risk of PONV, probablyduetothereductioninanestheticuse.5,6
The major limitation of this study was the lack of dataregardingremifentanil,desfluraneandpropofol admin-istered doses to each patient. Additionally, end-tidal desflurane, propofol plasma-site and remifentanil effect-siteconcentrationswerenotrecordedattheendofsurgery andatextubation.Thesepossibleconfoundingfactorswere indirectly controlled by keeping BIS® value within appro-priate range during surgeries for all patients. However, thatdoesnotcompromisethefindings,sincepatientswere extubatedafterfullingobjectiveandclinicalcriteria (respi-ratoryrategreaterthan12breathsperminute;tidalvolume ≥6mL.kg−1, SaO
2≥97%, prompt response to a standard
command;orheavycoughingduringanesthesiaemergence). In respect to the significant differences in patient mean agesbetween thegroups,thePearsoncorrelationanalysis (age vs. time tofollow command and age vs. extubation time)revealedthatagehadnoinfluenceontimetofollow commandand extubationtime ineither groups (p>0.05). Still,althoughinhalationinductionwouldbethebeststudy designforpatientsreceivingdesfluraneinthisstudy, propo-folwastheonlyhypnoticagentusedforinduction inboth groups.Desflurane’sgreatpungencyincreasesairway reac-tivityand also stimulates the sympatheticsystem, which makeitsinductionimpractical.1
Conclusion
Remifentanil-desflurane-basedanesthesiahasafastertime tofollowcommandandextubationtimethan remifentanil-propofol-basedanesthesiawhen both guided byBIS® with similarindeterminaterecoveryatPACU.
Registration
This study was approved by the Ethics Committee of the Federal University of Minas Gerais (CAAE ---31820014.8.0000.5149).Patientswererecruitedfor enroll-ment preoperatively on the day of the surgery and gave written informed consentbeforeenrollment (Fig. 1).The studywasregisteredatClinicalTrials.gov(NCT02631525).
Funding
The authors did not receive any funding supporting this paper.Desfluranevaporizeranditsanesthetic(Desflurane) were provided by Baxter Hospitalar Co. Ltd. Bispectral index® sensorswereprovidedbyCovidienCo.Ltd.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.JakobssonJ.Desflurane:aclinicalupdateofathird-generation inhaledanaesthetic.ActaAnaesthesiolScand.2012;56:420---32. 2.TramerM,MooreA,McQuayH.Propofolanaesthesiaand postop-erativenauseaandvomiting:quantitativesystematicreviewof randomizedcontrolledstudies.BrJAnaesth.1997;78:247---55. 3.LoopT,PriebeHJ.Recoveryafteranesthesiawithremifentanil combinedwithpropofol,desflurane,orsevofluranefor otorhi-nolaryngealsurgery.AnesthAnalg.2000;91:123---9.
4.LoopT, Priebe HJ. Prospective, randomized costanalysis of anesthesia with remifentanil combined with propofol, des-flurane or sevoflurane for otorhinolaryngeal surgery. Acta AnaesthesiolScand.2002;46:1251---60.
5.Punjasawadwong Y, Phongchiewboon A, Bunchungmongkol N. Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst Rev. 2014;6:Cd003843.
6.LiuSS.Effects ofbispectral indexmonitoring onambulatory anesthesia:ameta-analysisofrandomizedcontrolledtrialsand acostanalysis.Anesthesiology.2004;101:311---5.
7.GuptaA,StiererT,ZuckermanR,etal.Comparisonofrecovery profileafterambulatoryanesthesiawithpropofol,isoflurane, sevofluraneanddesflurane:asystematicreview.AnesthAnalg. 2004;98:632---41.
8.LiuFL,CherngYG,ChenSY,etal.Postoperativerecoveryafter anesthesiainmorbidlyobesepatients:asystematicreviewand meta-analysisofrandomizedcontrolledtrials.CanJAnaesth. 2015;62:907---17.
9.Wachtel RE, Dexter F, Epstein RH, et al. Meta-analysis of desflurane and propofol average times and variability in timestoextubationandfollowingcommands.CanJAnaesth. 2011;58:714---24.
10.SongD,JoshiGP,WhitePF.Fast-trackeligibilityafter ambula-toryanesthesia:acomparisonofdesflurane,sevoflurane,and propofol.AnesthAnalg.1998;86:267---73.
11.McKayRE,MalhotraA,CakmakkayaOS,etal.Effectofincreased bodymassindexandanaestheticdurationonrecoveryof pro-tectiveairway reflexes after sevoflurane vsdesflurane. Br J Anaesth.2010;104:175---82.
13.Minto CF, Schnider TW, Shafer SL. Pharmacokinetics and pharmacodynamicsofremifentanil.II.Modelapplication. Anes-thesiology.1997;86:24---33.
14.MarshB, White M, Morton N, et al. Pharmacokinetic model driven infusion of propofol in children. Br J Anaesth. 1991;67:41---8.
15.Wilhelm W, Berg K, Langhammer A, et al. Remifentanil in gynecologiclaparoscopy. A comparison of consciousnessand circulatory effects of a combination with desflurane and propofol. Anasthesiol Intensivmed Notfallmed Schmerzther. 1998;33:552---6.
16.DexterF,TinkerJH.Comparisonsbetweendesfluraneand isoflu-raneorpropofolontimetofollowingcommandsandtimeto discharge.Ametaanalysis.Anesthesiology.1995;83:77---82. 17.VaughanJ,NagendranM,CooperJ,etal.Anaestheticregimens
for day-procedure laparoscopic cholecystectomy. Cochrane DatabaseSystRev.2014;1:Cd009784.
18.Wu ZF, Jian GS, Lee MS, et al. An analysis of anesthesia-controlled operating room time after propofol-based total intravenous anesthesia compared with desfluraneanesthesia in ophthalmic surgery: a retrospective study. Anesth Analg. 2014;119:1393---406.
19.Rowe WL. Economics and anaesthesia. Anaesthesia. 1998;53:782---8.
20.EppleJ,KubitzJ,SchmidtH,etal.Comparativeanalysisofcosts oftotalintravenousanaesthesiawithpropofolandremifentanil
vs. balancedanaesthesia withisofluraneand fentanyl.EurJ Anaesthesiol.2001;18:20---8.
21.MasurskyD,DexterF,KwakyeMO,etal.Measuretoquantifythe influenceoftimefromendofsurgerytotrachealextubationon operatingroomworkflow.AnesthAnalg.2012;115:402---6. 22.Dexter F, Bayman EO, Epstein RH. Statistical modeling of
average and variability of time to extubation for meta-analysis comparing desflurane to sevoflurane. Anesth Analg. 2010;110:570---80.
23.VitezTS,MacarioA.Settingperformancestandardsforan anes-thesiadepartment.JClinAnesth.1998;10:166---75.
24.Camci E, Koltka K, Celenk Y, et al. Bispectral index-guided desfluraneandpropofolanesthesiainambulatoryarthroscopy: comparison of recovery and discharge profiles. J Anesth. 2006;20:149---52.
25.OrtizJ,ChangLC,TolpinDA,etal.Randomized,controlledtrial comparingtheeffectsofanesthesiawithpropofol,isoflurane, desfluraneandsevofluraneonpainafterlaparoscopic cholecys-tectomy.BrazJAnesthesiol.2014;64:145---51.
26.Fassoulaki A, Melemeni A, Paraskeva A, et al. Postopera-tive pain and analgesic requirements after anesthesia with sevoflurane,desfluraneor propofol.AnesthAnalg. 2008;107: 1715---9.