ORIGINAL ARTICLE
Treatment of empyema using thoracentesis with irrigation and intrapleural
application of an antimicrobial agent*
LIANA PERES DUAILIBE, MARIA ILIZABETI DONATTI, PAULO DE TARSO MÜLLER, PEDRO NANGO DOBASHI
Background: Empyema is a serious disease classically characterized by purulence within the pleural cavity. Early diagnosis demands immediate treatment, although there is still great controversy surrounding the question of what is the best therapy.
Objective: To analyze the method of using thoracentesis and pleural irrigation, combined with the intrapleural application of an antimicrobial agent, to treat empyema — and to compare this method with others described in the literature.
Method: Between January 1999 and May 2000, 17 patients diagnosed with loculated or diffuse pleural empyema were submitted to thoracentesis, followed by thorough washing of the pleural cavity with isotonic solution and intrapleural administration of a non-irritating antimicrobial agent to the pleura.
Results: The group of patients studied consisted of 15 men and 2 women, and the average age was 44. The most common clinical symptoms were fever, productive cough, chest pain and dyspnea, and the most common cause was pneumonia. Macroscopically, 12 patients presented obviously purulent pleural fluid. In 4 (26.67%) of the patients, the etiological agent was identified, the most frequent being Staphylococcus sp. Pulmonary decortication was indicated in 2 cases, and those 2 patients were therefore excluded. The average length of hospitalization was 17.1 days, although 3 patients received the treatment as outpatients. No recurrence or mortality was observed with the use of this methodology.
Conclusion: This approach reduced the need for invasive procedures, proving to be safe and efficient, with lower rates of morbidity and mortality than other modalities of treatment.
Key words: Empyema/Pleural, Pleura/Blood Supply, Treatment Outcome, Treatment Effectiveness.
*Study carried out at the Hospital Universitário de Mato Grosso do Sul (UFMS)
Correspondence to: Dr. Liana Peres Duailibe. Rua Miraflores, 197 — Carandá Bosque I, CEP: 79032-330. Campo Grande — MS.
INTRODUCTION
Pleural empyema, or pyothorax, is classically characterized by the presence of pus in the
pleural cavity.( 1 - 3 ) This disease was initially
described by Hippocrates( 1 , 4 - 6 ). The incidence of
pleural empyema is unknown and the disease may be caused by various factors such as pulmonary infection, trauma or injury to the chest, neoplasia, postoperative complication (from abdominal or thoracic surgery), iatrogenic diseases, complications from tuberculosis, or
foreign bodies( 5 - 1 1 ). Various therapeutic methods
can be adopted in the treatment of empyema( 6 ),
although there is still great controversy surrounding the question of what is the best therapy( 6 , 7 , 1 2 , 1 3 ).
Clinical signs and symptoms range from the nonspecific or insignificant to the acute. The most common symptoms are fever, productive
cough, chest pain, weight loss and dyspnea( 1 , 2 , 1 3
-1 5 ).
The disease advances in three stages( 3 , 5 , 7 ). The
exudative stage is characterized by thin pleural fluid with low cellular content and preserved lung expansion. This is followed by the fibrinopurulent stage, in which there is accumulation of pus, increased cellularity (high polymorphonuclear neutrophil counts), fibrin presence, limited lung expansion and potential for loculation. The final stage is the organizing phase, characterized by thick fluid and increased deposition of fibrin or fibrin tissue, causing lung entrapment and preventing lung expansion.
The microorganisms most commonly involved in the pathogenesis are Staphylococcus aureus, Staphylococcus epidermidis, anaerobes,
enterobacteria, Pseudomonas sp. and
Streptococcus pneumoniae( 5 , 7 , 1 3 , 1 6 ). Multiple
agents are often present.
Although French physicians initially used
thoracocentesis followed by pleural lavage( 1 7 ),
most authors now recommend thoracotomy followed by closed pleural drainage in combination with systemic antimicrobial
drugs( 2 , 8 , 1 6 , 1 8 - 2 5 ). Other therapeutic options include
pulmonary decortication, intrapleural use of fibrinolytic agents and video-assisted
thoracoscopy( 3 , 8 ).
A total of 17 patients admitted to the
pulmonology clinic in the Núcleo do Hospital
Universitá rio of the Universidade Federal do Mato Grosso do Sul (UFMS) were included in this study, in which we describe the treatment of those patients. The patients were diagnosed with diffuse or loculated pleural empyema and
underwent thoracocentesis followed by thorough irrigation of the pleural cavity with saline solution and intrapleural application of a non-irritating antimicrobial agent. We also analyzed the pathogenic agents involved, clinical response, need for other invasive procedures, duration of hospitalization, complications, morbidity and mortality.
METHOD
This study included adult patients admitted to
the pulmonology clinic of the Núcleo do Hospital
Universitá rio of the UFMS between January 1999 and May 2000. All were diagnosed with diffuse or loculated pleural empyema, in accordance with established criteria: purulent pleural fluid, glucose levels lower than 40 mg/dL, pH lower than 7.20, and positive or negative (i.e.,
irrelevant) results from pleural fluid culture( 3 , 5 ).
The Ethics Research Committee of the institution approved the study protocol.
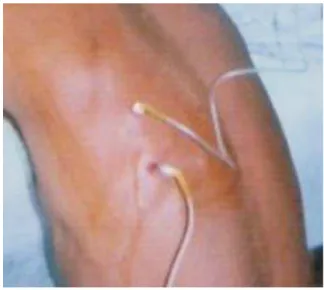
Figure 1. Diagnostic thoracocentesis producing purulent pleural fluid
Figure 2. Second pleural puncture for irrigation with saline solution, two intercostal spaces above the first
RESULTS
The study comprised 17 adult patients (15 males and 2 females) diagnosed with diffuse or loculated pleural empyema. Mean age was 44. One patient suffered from morbid obesity and was submitted to early pulmonary decortication due to limited access to the pleural space. Another patient was also submitted to surgical treatment at the discretion of the thoracic surgery department of the hospital. Both patients were excluded from the study. Of the 15 remaining patients, 10 (66.67%) were diagnosed with loculated empyema, and 5 (33.33%) were diagnosed with diffuse empyema. The most common symptoms are listed in Table 1.
Of the 15 patients evaluated, 6 (40%) were diagnosed with pneumonia, 4 with tuberculosis and 1 with thoracic trauma. One patient underwent upper abdominal surgery. Pathogenesis was not identified in 3 patients (Table 2).
Among the 15 patients, 4 (26.67%) were or had been alcoholics and 6 (40%) were active smokers.
Purulent pleural fluid was observed in 12 patients (80%). The etiologic agent was isolated in only 4 patients (26.67%), and the most frequently identified agent was Staphylococcus sp.
TABLE 1
Incidence of the most common symptoms
Symptom Incidence
Fever 100%
Productive cough 80%
Chest pain 66.7%
Dyspnea 40%
Appetite loss 40%
Weight loss 33.3%
TABLE 2 Causes of empyema
Cause Number of patients (%)
Pneumonia 6 (40%)
Tuberculosis 4 (26.67%)
Chest trauma 1 (6.67%) Upper abdominal surgery 1 (6.67%)
Unidentified 3 (20%)
The average length of hospitalization was 15.1 days, and 3 patients completed the treatment as outpatients. For resolution of the empyema, 4 (26.67%) patients were submitted to thoracocentesis once, 7 (46.67%) patients twice, 3 (20%) patients three times and 1 patient five times (Table 3).
Discrete residual pneumothorax, measured in accordance with recommended criteria, was
detected in 4 patients (less than 20%)( 2 6 , 2 7 ).
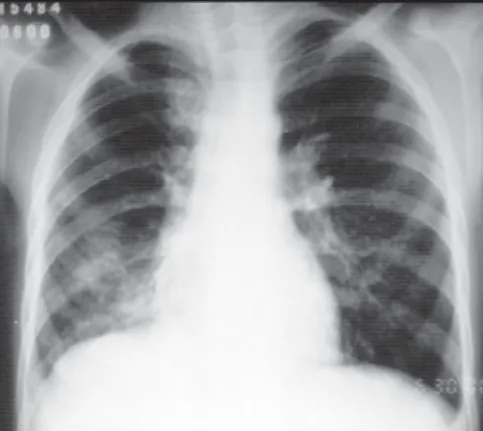
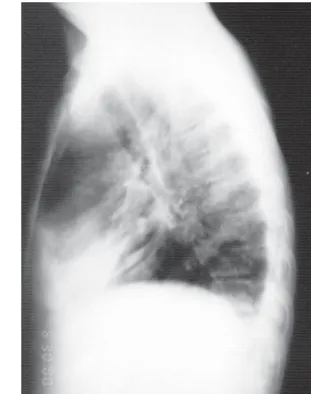
However, pleural drainage was not necessary and there was complete remission. Discrete pleural thickening was detected in 4 patients (26.67%). There was no recurrence and all patients survived (Figures 3, 4 and 6).
DISCUSSION
As an initial treatment for empyema, most authors recommend pleural drainage using a
water-sealed unit( 2 , 1 6 , 1 8 - 2 5 ). However, if there are
fibrin adhesions in the area between the wall and the chest tube or multiple pockets of pus far from the drain site, this procedure may not be successful and other more invasive surgical
procedures may be required( 5 , 1 1 , 1 5 , 2 0 , 2 8 ) . Therefore,
the best therapy for patients diagnosed with pleural empyema has not yet been determined( 6 , 7 , 1 2 , 1 3 , 1 5 , 2 9 ).
In 1998, Sarihan et al. reported that, in a series of 52 pediatric patients diagnosed with pleural empyema, 14 were successfully treated with repeated thoracocentesis and antibiotic therapy, whereas 38 patients underwent pleural
drainage( 5 ). Of the 38, 28 were cured, and 10 had
to be submitted to other therapeutic measures in order to achieve complete remission. In the same
year, Mandal et al. studied 179 patients( 8 ). As an
initial treatment, 20 of those 179 were submitted to thoracocentesis and a cure rate of 90% was achieved, whereas 52 underwent closed pleural drainage (cure rate, 62%). Of the patients who were submitted to decortication, 88% were cured. The authors also reported the use of image-assisted catheter drainage as a first procedure in 9 patients, and 8 (88.9%) were cured. Therefore, a considerable percentage of patients had loculated pockets that could not be drained through thoracocentesis, re-accumulation of fluid after decortication and incomplete resolution after closed drainage.
TABLE 3
Number of times thoracocentesis was performed Thoracocentesis Number of patients (%)
Once 4 (26.67%)
Twice 7 (46.67%)
Three times 3 (20%)
Five times 1 (6.67%)
Total 15 (100%)
We found no studies in the literature reporting empyema treatment with thoracocentesis involving post-drainage irrigation of the pleural space (with isotonic solution) and intrapleural administration of antimicrobial agents. However, other authors have reported thoracotomy with closed pleural drainage and irrigation, as well as intrapleural application of antimicrobial agents. In 1998, Gharagozloo et al. reported that intrapleural application of antimicrobial agents was necessary
in order to treat infections locally( 2 1 ).
Figure 3A. Chest X-ray in profile with air-fluid level in the right lower lobe (arrow)
Figure 4A. Chest X-ray in profile showing loculated effusion with air-fluid level
Figure 4B. Chest X-ray after treatment
Figure 5A. Chest X-ray in profile showing diffuse pleural effusion in the right hemithorax
In 1993, Takayama et al. studied patients with empyema caused by multiresistant Pseudomonas aeruginosa and reported lavage of the pleural cavity with saline solution containing tobramycin and aztreonam followed by lavage with diluted povidone-iodine solution, and culture results
were negative after 3 days( 3 0 ). Gharagozloo et al.
treated 22 patients diagnosed with post-pneumonectomy empyema through thoracic drainage and irrigation of the pleural cavity with 0.1% povidone-iodine solution followed by irrigation with saline solution and a solution containing gentamicin, neomycin, and polymyxin
B for 24 hours( 2 1 ). The authors observed that
patients achieved complete remission with no relapse and short hospital stays. In 1996, Ali et al. reported that 47 patients diagnosed with tuberculous empyema were initially submitted to closed chest drainage combined with a treatment
regimen of multiple tuberculostatic drugs( 3 1 ).
Treatment was unsuccessful, and patients were then submitted to open thoracostomy followed by daily irrigation of the cavity with povidone-iodine solution. There was complete re-expansion of lungs in 28 patients, whereas the other 11 patients, presenting various stages of re-expansion, were expected to achieve complete remission.
Recently, Colice et al. conducted a careful review of the medical literature and published evidence-based guidelines for the treatment of
parapneumonic effusions( 2 9 ). The authors
classified prognostic risk according to clinical variables such as quantity of pleural fluid, loculation, pleural fluid pH and bacteriology. Patients were classified by level of poor outcome risk. The authors defined 4 such categories: 1 (very low risk), 2 (low risk), 3 (moderate risk), and 4 (high risk). The consensus opinion of the panel recommended drainage only for patients in categories 3 and 4. In the present study, 12 (80%) of the 15 patients evaluated were classified as belonging to risk category 4 (purulent fluid and loculation).
In 1988, Thys et al. reported that systemic aminoglycosides easily penetrated and diffused
throughout normal pleura( 3 2 ). However, this
process was jeopardized by pleural thickening or purulent pleural fluid. In 2000, Teixeira et al. induced empyema in rabbits through inoculation
with Pasteurella multocida and tested the
penetration of some antimicrobial agents routinely used in the treatment of empyema,
including gentamicin( 3 3 ). The authors reported
that, when there was pleural involvement, intrapleural levels of gentamicin were much lower than were serum levels, thereby confirming similar findings reported by other authors. Although the study by Thys et al. had already been published by the time the present study was conducted, we opted for empirical use of gentamicin as an antimicrobial agent because it is inexpensive, easily procured and has been
safely used by various authors( 2 1 , 3 3 ).
Mean length of hospitalization in the present study was 15.1 days. However, in some cases, hospitalization criteria were based on logistics, since most patients came from locations in the countryside and therefore had transportation difficulties.
When we compare our study to those in which patients were submitted to closed chest drainage
as an initial treatment( 5 , 1 0 , 1 3 , 1 6 , 3 4 ), we found
hospital stays to be shorter in the present study. Shorter length of hospitalization and the simplicity of the method reduce hospital costs since the necessary materials are frequently used in hospitals and the technique requires no surgical procedures, which would increase treatment costs.
Shoseyov et al. recently published a comparative study of two groups of children
diagnosed with pleural empyema( 3 6 ). The first
group (32 patients) was submitted to early pleural drainage, and other, more invasive methods were necessary because the treatment was not effective. The second group (35 patients) was submitted to ultrasound-assisted thoracocentesis, and additional therapies were required in only 5 patients (closed pleural drainage and urokinase administration in 2 and decortication in 3).
In our study, 11 of the 14 patients were submitted to thoracocentesis more than once. This can be explained by the fact that most already presented loculation, sometimes forming multiple pockets. This allowed us to classify these 11 patients as belonging to the Colice et
al. risk category 4( 2 9 ). Likewise, Mandal et al.
reported that 13 of the 26 patients submitted to thoracocentesis as an initial treatment were required to undergo that procedure more than once( 8 ).
findings of other studies( 1 , 2 , 5 , 1 6 ). It has been
shown that sterile fluid is common during the
fibrinopurulent phase( 1 , 5 , 8 , 1 5 , 1 6 , 3 5 ). This explains
our results, since 80% of the patients evaluated in the present study presented purulent fluid during diagnostic thoracocentesis.
Clinical evidence observed in our patients was completely in accordance with data from other studies reviewed.
In our study, 26.67% of the patients presented discrete pleural thickening. Despite the fact that spirometry was not performed, we consider these results satisfactory since there was little physical limitation. Sarihan et al. reported pleural thickening in 65% of the patients studied, although the authors did not relate this finding to disease severity or therapeutic
method( 5 ).
In conclusion, thoracocentesis followed by pleural irrigation with saline solution and local administration of gentamicin as an initial treatment for pleural diffuse or loculated pleural empyema was efficacious, presented low complication risks, reduced costs and length of hospitalization, and can be performed by non-surgeons. The procedure may be safely performed as an initial treatment in outpatients. More invasive procedures should only be used if there is treatment failure.
REFERENCES
1 . C h a m C W , H a q S M , R a h a m i m J . E m p y e m a t h o r a c i s : a p r o b l e m w i t h l a t e r e f e r r a l ? T h o r a x . 1 9 9 3 ; 4 8 : 9 2 5 -7 . 2 . M a n g e t e E D O , K o m b o B B , L e g g - J a c k T E . T h o r a c i c
e m p y e m a : a s t u d y o f 5 6 p a t i e n t s . A r c h D i s C h i l d . 1 9 9 3 ; 6 9 : 5 8 7 -8 .
3 . L i g h t R W , R o d r i g u e z R M . M a n a g e m e n t o f p a r a p n e u m o n i c e f f u s i o n s . C l i n C h e s t M e d . 1 9 9 8 ; 1 9 : 3 7 3 -8 2 .
4 . M a g o v e r n C J , R u s c h V W . P a r a p n e u m o n i c a n d p o s t -t r a u m a -t i c p l e u r a l s p a c e i n f e c -t i o n s . C h e s -t S u r g C l i n N A m . 1 9 9 4 ; 4 : 5 6 1 - 8 2 .
5 . S a r i h a n H , C a y A , A y na c i M , A k y a z i c i R , B a k i A . E m p y e m a i n c h i l d r e n . J C ar d i o v a s c S u r g ( T o r i n o ) . 1 9 9 8 ; 3 9 : 1 1 3 -6 .
6 . T h o u r a n i V H , B r a d y K M , M a n s o u r K A , M i l l e r J I J r , L e e RB . E va l ua tion of tre a tm e nt m oda litie s for thora c ic e m p y e m a : a c o s t - e f f e c t iv e ne s s a na l y s i s . A nn T h o r a c S u r g . 1 9 9 8 ; 6 6 : 1 1 2 1 -7 .
7 . W e i s s b e r g D , R a f a e l y Y . P l e u r a l e m p y e m a : 2 4 - y e a r e x p e r i e n c e . A n n T h o r a c S u r g . 1 9 9 6 ; 6 2 : 1 0 2 6 -9 .
8 . M a n d a l A K , T h a d e p a l l i H , M a n d a l A K , C h e t t i p a l l y U . O u t c o m e o f p r i m a r y e m p y e m a th o r a c i s : th e r a p e uti c a nd m i c r o b i o l o g i c a s p e c t s . A n n T h o r a c S u r g . 1 9 9 8 ; 6 6 : 1 7 8 2 -6 .
9 . R e n n e r H , G a b o r S , P i n t e r H , M a i e r A , F r i e h s G , S m o l l e -J u e t t n e r F M . I s a g g r e s s i v e s u r g e r y i n p l e u r a l e m p y e m a j u s t i f i e d ? E u r J C a r d i o t h o r a c S u r g . 1 9 9 8 ; 1 4 : 1 1 7 - 2 2 . 1 0 . A l f a g e m e I , M u n o z F , P e n a N , U m b r i a S . E m p y e m a o f
t h e t h o r a x i n a d u l t s . E t i o l o g y , m i c r o b i o l o g y f i n d i n g s , a nd m a na g e m e nt . Ch e st . 1 9 9 3 ; 1 0 3 : 8 3 9 -4 3 .
1 1 . G a l e a J L , D e S o uza A , B e g g s D , S p y t T . T h e s ur g i c a l m a n a g e m e n t o f e m p y e m a t h o ra c i s . J R C o l l S u r g E d i n b . 1 9 9 7 ; 4 2 : 1 5 -8 .
1 2 . D a v i e s R J , G l e e s o n F V . T h e d i a g n o s i s a n d m a n a g e m e n t o f p l e u r a l e m p y e m a . C u r r O p i n P u l m M e d . 1 9 9 8 ; 4 : 1 8 5 -9 0 .
1 3 . F e r g u s o n A D , P r e s c o t t R J , S e l k o n J B , W a t s o n D , S w i n b u r n C R . T h e c l i n i c a l c o u r s e a n d m a n a g e m e n t o f t h o r a c i c e m p y e m a . Q J M e d . 1 9 9 6 ; 8 9 : 2 8 5 - 9 .
1 4 . S o l a k H, C e r a n S , S una m G S , G o k M , A k y o l K G , S o l a k T , e t a l . E m p y e m a t h o r a c i s — a s e r i e s o f 2 3 0 c a s e s. I n d i a n J M e d S c i . 1 9 9 6 ; 5 0 : 2 6 9 - 7 1 .
1 5 . L e M e n s e G P , C h a r l i e S , S a h n S A . E m p y e m a t h o r a c i s . T h e r a p e u t i c m a n a g e m e n t a n d o u t c o m e . C h e s t . 1 9 9 5 ; 1 0 7 : 1 5 2 3 -7 .
1 6 . B o r g e J H , M i c h a v i l a I A , M é n d e z J M , R o d r í g u e z F C , G r i ñ a n N P , C e r r a t o R V . T h o r a c i c e m p y e m a i n H I V -in f e c t e d p a t ie n t s : m ic r o b io lo g y , m a n a g e m e n t , a n d outc om e . Che st. 1998; 113: 732-8.
1 7 . M u i r J F , C u v e l i e r A , T r e h o ny A. P le ur e sie s p ur ule nt e s. R e v P r a t . 1 9 9 7 ; 4 7 : 1 3 1 5 - 9 .
1 8 . L a w r e n c e D R , O h r i S K , M o x o n R E , T o w n s e n d E R , F o u n t a i n S W . T h o r a c o s c o p i c d e b r i d e m e n t o f e m p y e m a t h o r a c i s . A n n T h o r a c S u r g . 1 9 9 7 ; 6 4 : 1 4 4 8 -5 0 .
1 9 . S a s s e S , N g u y e n T K , M u l l i g a n M , W a n g N S , M a h u t t e C K , L ig h t R W . T h e e f f e c t s o f e a r ly c h e s t t u b e p la c e m e n t o n e m p y e m a r e so lut io n. Ch e st . 1 9 9 7 ; 1 1 1 : 1 6 7 9 -8 3 . 2 0 . K e l l y J W , M o r r i s M J . E m p y e m a t h o r a c i s : m e d i c a l a s p e c t s
o f e v a l u a t i o n a n d t r e a t m e n t . S o u t h M e d J . 1 9 9 4 ; 8 7 : 1 1 0 3 -1 0 .
2 1 . G h a r a g o z l o o F , T r a c h i o t i s G , W o l f e A , D u b r e e K J , C o x J L . P l e u r a l s p a c e i r r i g a t i o n a n d m o d i f i e d c l a g e t t p r o c e d u r e f o r t h e t r e a t m e n t o f e a r l y postpne um one c tom y e m py e m a . J T h o r a c C a r d i o v a s c S u r g . 1 9 9 8 ; 1 1 6 : 9 4 3 -8 .
2 2 . S a h a n S A . U s e o f f i b r i n o l y t ic a g e nt s in t h e m a na g e m e nt o f c o m p l i c a t e d p a r a p n e u m o n i c e f f usio ns a nd e m p y e m a s. T h o r a x . 1 9 9 8 ; 5 3 ( S u p p l 2 ) : S 6 5 - 7 2 .
2 3 . G r i l l o I A , T e k l u B , A l - S a i g h A H , M a l a t a n i T S , A l S h e h r y M Y , B a t o u k A , e t a l . E m p y e ma th o r a c i s i n a d ul ts i n S a u d i A r a b i a . E a s t A f r M e d J . 1 9 9 5 ; 7 2 : 7 6 6 - 9 .
2 4 . F i l o m e n o L T B , C a m p o s J RM , F e r na nd e s P M P . E mp i e ma p l e ur a l . I n: C uk i e r A . , Na k a ta ni J , M o r r o ne N. P ne umo l o g i a — a tua l i z a ç ão e r e c i c l a g e m. 2 a e d . S ão P a ulo : At h e ne u; 1 9 9 8 . Ca p .; 6 1 , p .4 2 8 -4 2 .
2 5 . C a m a r g o J J . E m p i e m a p l e u r a l . I n : S i l v a L C C d a . C o m p ê n d i o d e p n e u m o l o g i a . 2 a e d . S ão P a u l o : F u n d o E d i t o r i a l B Y K ; 1 9 9 1 . C a p . 7 8 , p . 9 1 1 - 9 .
2 6 . L i g h t R W , O ´ H a r a V S , M o r itz T E , M c E l h i nne y A J , B utz R , Ha a k e nso n C M , e t a l . I ntr a p l e ur a l tetr a c y c l i ne fo r th e p re v e nt io n o f r e c ur r e nt sp o n t a n e o u s p n e u m o t h o r a x . J A M A . 1 9 9 0 ; 2 6 4 : 2 2 2 4 - 3 0 .
2 7 . R h e a J T , D e L u c a S A , G r e e n e R E . D e t e r m i n i n g t h e s i z e o f p n e u m o t h o r a x i n t h e u p r i g h t p a t i e n t . R a d i o l o g y . 1 9 8 2 ; 1 4 4 : 7 3 3 -6 .
2 8 . M a r t e l l a A , S a n t o s G H . D e c o r t i c a t i o n f o r c h r o n i c p o s t p n e u m o n i c e m p y e m a . J A m C o l l S u r g . 1 9 9 5 ; 1 8 0 : 5 7 3 -6 .
2 9 . C o l i c e G L , C u r t i s A , D e s l a u r i e r s J , H e f f n e r J , L i g h t R W , L it t e n b e r g B , e t a l. M ed ic a l a nd s u r g ic a l t r e a t m e n t o f p a r a p n e u m o n i c e f f u s i o n s : a n e v id e n c e -b a s e d g u id e lin e . Ch e st . 2 0 0 0 ; 1 1 8 : 1 1 5 8 -7 1 .
3 0 . T a k a y a ma K , Hi r a ta M , Na b e s h i ma S , Na b e s h i ma A , Ha r a H , K a s h i w a g i S . P l e u r a l w a s h i n g w i t h p o v i d o n e - i o d i n e f o r t r e a t m e n t o f e m p y e m a . K a n s e n s h o g a k u Z a s s h i . 1 9 9 3 ; 6 7 : 2 1 8 -2 2
3 1 . A l i S M , S i d d i q u i A A , M c L a u g h l i n J S . O p e n d r a i n a g e o f m a s s iv e t u b e r c u lo u s e m p y e m a w it h p r o g r e s s iv e reex pa nsion of the lung: a n old c o nc ept revisited. A nn T h o r a c S u r g . 1 9 9 6 ; 6 2 : 2 1 8 - 2 3 .
3 3 . T e i x e i r a L R , S a s s e S A , V i l l a r i n o M A , N g u y e n T , M u l l i g a n M E , L i g h t R W . A n t i b i o t i c l e v e l s i n e m p y e m i c p l e u r a l fluid. Che st. 2000; 117: 1734-9.
3 4 . M te ta K A . T h o r a c i c e mp y e ma i n D a r e s S a l a a m, T a n z a n i a . E a s t A f r M e d J . 1 9 9 4 ; 7 1 : 6 8 4 - 6 .
3 5 . L i m t h o n g k u l S , W o n g t h i m S , C h a r o e n l a p P , U d o m p a n i c h V , N u c h p r a y o o n C . P n e u m o n i a w it h p le u r a l e f f u s io n s . J M e d A s s o c T h a i . 1 9 9 4 ; 7 7 : 2 2 5 - 3 0 .