www.jped.com.br
ORIGINAL
ARTICLE
Undersedation
is
a
risk
factor
for
the
development
of
subglottic
stenosis
in
intubated
children
夽
,
夽夽
Cláudia
Schweiger
a,b,∗,
Denise
Manica
a,b,
Denise
Rotta
Rutkay
Pereira
b,
Paulo
Roberto
Antonacci
Carvalho
b,c,
Jefferson
Pedro
Piva
b,c,
Gabriel
Kuhl
a,d,
Leo
Sekine
e,
Paulo
José
Cauduro
Marostica
b,faHospitaldeClínicasdePortoAlegre,UnidadedeOtorrinolaringologia,PortoAlegre,RS,Brazil
bUniversidadeFederaldoRioGrandedoSul(UFRGS),ProgramadePós-Graduac¸ãoemSaúdedaCrianc¸aedoAdolescente,
PortoAlegre,RS,Brazil
cHospitaldeClínicasdePortoAlegre,UnidadedeTerapiaIntensivaPediátrica,PortoAlegre,RS,Brazil
dUniversidadeFederaldoRioGrandedoSul(UFRGS),DepartamentodeOtorrinolaringologiaeOftalmologia,PortoAlegre,RS,
Brazil
eUniversidadeFederaldoRioGrandedoSul(UFRGS),ProgramadePós-Graduac¸ãoemEpidemiologia,PortoAlegre,RS,Brazil fHospitaldeClínicasdePortoAlegre,UnidadedePneumologiaPediátrica,PortoAlegre,RS,Brazil
Received4July2016;accepted24October2016 Availableonline25January2017
KEYWORDS
Larynx; Airway steno-sis/reconstruction; Children
Abstract
Objective: Toanalyzethelevelofsedationinintubatedchildrenasariskfactorforthe devel-opmentofsubglotticstenosis.
Methods: Allpatientsbetween30daysand5yearsofagewhorequiredendotrachealintubation inthepediatricintensivecareunitbetween2013and2014wereincludedinthisprospective study.TheyweremonitoreddailyandCOMFORT-Bscoreswereobtained.Flexiblefiber-optic laryngoscopywasperformedwithineighthoursofextubation,andrepeatedseventotendays later ifthefirst examinationshowed moderatetoseverelaryngeal injuries.If theselesions persistedand/orifthechilddevelopedsymptomsinthefollow-upperiod,microlaryngoscopy undergeneralanesthesiawasperformedtoevaluateforsubglotticstenosis.
Results: Thestudyincluded36children.Incidenceofsubglotticstenosiswas11.1%.Children with subglottic stenosis hada higher percentage ofCOMFORT-B scores between 23 and 30 (undersedated)thanthosewhodidnotdevelopsubglotticstenosis(15.8%vs.3.65%,p=0.004).
夽
Pleasecitethisarticleas:SchweigerC,ManicaD,PereiraDR,CarvalhoPR,PivaJP,KuhlG,etal.Undersedationisariskfactorforthe developmentofsubglotticstenosisinintubatedchildren.JPediatr(RioJ).2017;93:351---5.
夽夽
ThisstudywasperformedintheHospitaldeClínicasdePortoAlegre,UnidadedeTerapiaIntensivaPediátrica,PortoAlegre,RS,Brazil. ∗Correspondingauthor.
E-mail:causch@hotmail.com(C.Schweiger).
http://dx.doi.org/10.1016/j.jped.2016.10.006
0021-7557/©2017SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.ThisisanopenaccessarticleundertheCCBY-NC-ND
Conclusion: Childrenwhodevelopedsubglotticstenosiswerelesssedatedthanchildrenwho didnotdevelopsubglotticstenosis.
©2017SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/ 4.0/).
PALAVRAS-CHAVE
Laringe;
Estenose/Reconstruc¸ão dasviasaéreas; Crianc¸as
Subsedac¸ãoéumfatoderiscoparaodesenvolvimentodeestenosesubglótica emcrianc¸asintubadas
Resumo
Objetivo: Analisaronível desedac¸ãoem crianc¸asintubadas comoum fatorderiscoparao desenvolvimentodeestenosesubglótica(ES).
Métodos: Todosospacientesentre30diase5anosdeidadesquenecessitaramdeintubac¸ão endotraquealnaUnidadedeTerapiaIntensivaPediátricaentre2013e2014foramincluídosneste estudoprospectivo.Elesforammonitoradosdiariamenteeforamobtidososescoresdaescala COMFORT-B.Foifeitalaringoscopiacomtuboflexíveldefibraópticaem8horasdaextubac¸ão erepetida7-10diasdepois,casooprimeiroexametenhamostradolesõeslaríngeasmoderadas agraves.Casoessaslesõestenhampersistidoe/oucasoacrianc¸atenhadesenvolvidosintomas noperíododeacompanhamento,foifeitamicrolaringoscopiasobanestesiageralparaavaliara ES.
Resultados: Incluímos36crianc¸as.AincidênciadaESfoide11,1%.Ascrianc¸ascomES apresen-taramummaiorpercentualdeescoresdaescalaCOMFORT-Bentre23e30(subsedados)queos quenãodesenvolveramES(15,8%emcomparac¸ãoa3,65%,p=0,004).
Conclusão: Ascrianc¸asquedesenvolveramESforammenossedadasqueascrianc¸asquenão desenvolveramES.
©2017SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Este ´eumartigo OpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4. 0/).
Introduction
Acquiredsubglotticstenosis(SGS)ismostcommonlya con-sequence of prolonged endotracheal intubation, with a reportedincidenceof2.8---11.3%.1---3Thereareseveralrisk
factorsalreadyunderconsideration;however,thereareonly afewstudieswithsufficientlyadequatedesigntoascertain itsassociation.
Whileprevious publications havesuggested that inade-quatesedationisariskfactorforthedevelopmentofSGS,4,5
thesestudies wereeitherexpert opinionsor retrospective reviewswithnocontrolgroup.Theproposedmechanismof injuryisthattheagitationofthechild couldcause exces-sivemovementoftheendotrachealtube(ETT)intheairway, predisposingtolaryngealstenosis.
In2007,astudyfromthepresentresearchgroupenrolling 35pediatricpatientsshowedthatthenumberofadditional dosesofsedationthatthechildreceivedduringthe intuba-tionperiodwasariskfactorforSGS.6Later,anotherarticle
by the same group including 142 children confirmed that thenumberofextradosesofsedationwaseffectivelyarisk factor, and alsoidentified prolonged intubationtime asa significantpredictorofthe developmentof SGS.However, solelyfromthedata collected,it couldnotbe concluded whetherthereasonforthelarynxinjurywastraumabecause ofthechild’sexcessiveagitation,orhypoperfusionandlocal ischemiabecauseofexcessivesedation,which,alongwith the trauma due to the ETT in contact with the airway mucosa,culminatedinthedevelopmentofSGS.7
Inordertoclarifythisissueinchildrenbeyondthe neona-talperiod,theauthorsconductedresearchinthepediatric intensive care unit(PICU)of thishospital,collecting data regarding the sedation of patients. The aim of this study wasthereforetoverifyifthereisanyassociationbetween thedegreeofsedationduringtheintubationperiodandthe developmentofSGSafterextubation.
Methods
This wasaprospectivecohortstudythat includedall chil-dren from 30 daysto 5 yearsof age who wereintubated inthePICUofHospitaldeClínicasdePortoAlegre(HCPA), between 2013 and 2014, and whose parents or guardians agreed to participate by signing an informed consent. Patientswereexcludediftheyhadsignsofprevious laryn-gealdisease,suchasdysphoniaandstridor,priorintubation, current or past tracheostomy, craniofacial malformations, or children in poor general condition. The protocol was approvedbytheResearchandEthicsCommitteeofHCPA.
Intubationproceduresfollowedaprotocoloffast intuba-tion sequence, with theuse of midazolam, fentanyl, and rocuronium. Children were then sedated withmidazolam 0.2mg/kg/handfentanyl2mcg/kg/hduringtheentire intu-bation period. All extra sedative medication doses were considered‘‘additionaldosesofsedation.’’
and need for ETT repositioning were collected. The size ofthe ETTwasdeterminedbyguidelinesfromthe Ameri-canHeart Association.8 Verificationoftube size adequacy
isperformedbyevaluatingthedifferenceofinspiratoryand expiratorytidalvolumes,asmeasuredbythePICUassistant; tubesizeisconsideredadequatewhenthereisadifference of around20---25% between thetwomeasured volumes. If thedifferenceis greaterthanthat,thenPICUstaffupsize theETT.Ifthedifferenceissmaller,theydownsizeit.
In2013,theapplicationoftheCOMFORT-Bsedationscale was implemented at the PICU of HCPA in order to mea-sure the level of sedation and toassist in evaluating the needforadditionaldosesofsedation.Nurseswhohadbeen previously trained applied this scale every three hours. It evaluates items such as level of consciousness, calm-ness/agitation, respiratory response, physical movement, muscletone,andfacialtension.9
Patients underwent flexible fiber-optic laryngoscopy (FFL)inthePICUwithineighthoursafterextubation,with nasaltopicalanesthesiaandwithoutsedation.Allchildren used supplemental oxygen due to the recent extubation. The patients were positioned, and oxygen saturation and heart rate were monitored throughout the examination. The examinationswererecordedandlater examinedby a blindedreviewer,whoclassifiedtheminGroup1---no laryn-geal injuries or mild injuries, or Group 2 --- moderate to severelaryngeal lesions,accordingtoacriteriapreviously publishedbytheauthors.1
All childrenwerefollowed-up afterdischarge fromthe PICU. Those with moderate to severe lesions on the ini-tial post-extubationFFL, andanyadditionalchildren with laryngealsymptomsduringfollow-up,underwentasecond FFLseventotendaysafterextubation,andwerefollowed upfurther.Thosewithpersistentlaryngeallesionsreceived subsequentmicrolaryngoscopytoevaluateforpossibleSGS. Families wereasked tobringtheir children exclusively tothe researchmedicalstaffwheneverrespiratory symp-tomsdeveloped.NoneofthepatientshadadiagnosisofSGS establishedwithoutmicrolaryngoscopybeingperformed.
Patientswerethendivided intotwofinalgroups: those whodevelopedSGSandthosewhodidnot.Childreninthe SGSgroupwereenrolledinafollow-up programandwere treatedbytheotolaryngologyteam.
The program Predictive Analytics Software (PASW) version 17.0.2 (Somers, NY, USA) was used for statis-tical analysis. Quantitative variables were expressed as mean±SDwhen theyhadnormal distribution.Otherwise, they were described as median, 25th and 75th per-centiles, as well as minimum and maximum values. The Mann---Whitney U-test was used for calculating the dif-ference between the groups. Categorical variables were expressed as number of patients (n) and percentage (%). Fisher’sexacttestwithchi-squareddistributionwasusedto calculatethedifferencebetweentheproportions.For cal-culationofthe95%confidenceinterval(95%CI),theWilson scoremethodwasused.
Results
Duringthetwo-yearperiodofresearchinPICU,45children were eligiblefor the study. Of these, ninechildren were
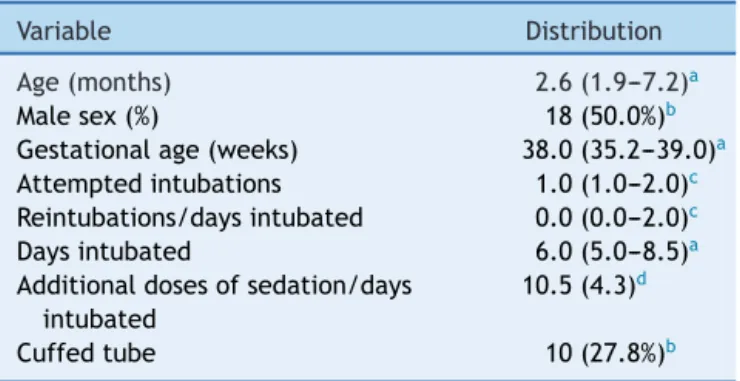
Table1 Populationcharacteristics(n=36).
Variable Distribution
Age(months) 2.6(1.9---7.2)a
Malesex(%) 18(50.0%)b
Gestationalage(weeks) 38.0(35.2---39.0)a
Attemptedintubations 1.0(1.0---2.0)c
Reintubations/daysintubated 0.0(0.0---2.0)c
Daysintubated 6.0(5.0---8.5)a
Additionaldosesofsedation/days intubated
10.5(4.3)d
Cuffedtube 10(27.8%)b
a Median(interquartilerange,P25---P75). b Numberofpatients(percentage). c Median(range,minimum---maximum). d Mean(standarddeviation).
notincluded because theirparents refused to participate (twochildren),theyunderwenttracheostomyforprolonged mechanicalventilation(three children),died before extu-bation(two children),or died aftertheinitial assessment (twochildren).Thus,therewasan eventuallossof20%of patients,and36childrenwereincluded.
Themedianageoftheincludedchildrenwas2.6months (25th---75thpercentiles:1.9---7.2)and50%(18)weremale.
Inthe initialFFL,16 children(44.4%) hadmoderate to severeinjuries.TheincidenceofSGSattheendoffollow-up was11.1%(fourchildren;95%CI,4.17---29.60).
Dataregardingpopulationcharacteristicsarepresented inTable1.
Dataregardingotherpossibleriskfactors,includingthe number of days of intubation, additional doses of seda-tion/days of intubation, number of intubations/days of intubation, and the presence of a cuffed tube, are pre-sentedinTable2.Univariateanalysisshowednostatistically significanceforthesevariables.
Children who developed SGS had a mean COMFORT-B scoreof16.00±1.76,whilethemeanCOMFORT-Bscoreof thosewhodidnotdevelopSGSwas12.76±2.13,witha sta-tisticallysignificantdifference(p=0.006).ChildrenwithSGS hadahigherpercentageofCOMFORT-Bscoresbetween23 and30thanthosewhodidnotdevelopSGS(15.8%vs.3.65%,
p=0.004).DataareshowninTable3andFig.1.
Discussion
OwingtothecomplexityofSGSmanagementandthe asso-ciated morbidity, it is important to identify risk factors associatedwith its development.There are few prospec-tivestudiesonthissubject,andmostofthemwereheldin neonatalintensivecareunits.10,11
The authors’ previous studies identified the duration ofintubation7 andnumberof additionaldoses ofsedation
receivedbythechild6,7asriskfactorsforSGS.Thenumber
ofreintubationattemptsandtheuseofacuffedtubewere notconsideredsignificant.
Sedationwasmentioned insomearticlesasapotential factorforthedevelopmentofSGS,4,7althoughtodatethis
Table2 Analysisofisolatedriskfactorforsubglotticstenosis(n=36).
Variable NoSGS(n=32) SGS(n=4) p
Malesexa 17(53.1%)c 1(25.0%)c 0.29
Attemptedintubationsb 1(1---2)d 1(1---1)d 0.94
Daysintubatedb 6(5.0---9.0)e 6(2.7---7.0)e 0.61
Additionaldosesofsedation/daysintubatedb 9.9(4.0)f 15.1(4.3)f 0.05
Cuffedtubea 9(28.1%)c 1(25.0%)c 0.89
Reintubations/daysintubatedb 0(0---0.18)d 0(0---0.20)d 0.68
SGS,subglotticstenosis. aPearson’schi-squared. b Mann---WhitneyU-test.
c Numberofpatients(percentage). d Median(range,minimum---maximum). e Median(interquartilerange,P25---P75).
f Mean(standarddeviation).
Table3 COMFORT-Bscores:comparisonbetweenthetwogroups(n=36).
Variable SGSn=4 Normallarynxn=32 p
MeanCOMFORT-Bscore 16.00±1.76 12.76±2.13 0.006
%ofCOMFORT-Bscoresbetween23and30(undersedated) 15.8% 3.65% 0.004 %ofCOMFORTBscoresbetween11and22(adequatelysedated) 58.25% 56.43% 0.511 %ofCOMFORTBscoresbetween6and10(oversedated) 25.95% 39.92% 0.05
SGS,subglotticstenosis.
70
60
50
40
30
20
10
0
Over sedated (scores between
6-10)
Adequately sedated (scores between 11-22)
Undersedated (scores between
23-30)
SGS p = 0.05
p = 0.004 p = 0.511
39.92
58.25 56.43
25.95
15.8
3.65
No SGS/Normal larynk
P
ercentage of comf
or
t- B scores in each categor
y
Fig. 1 Percentagesof COMFORT-B scores ineach category. SGS,subglotticstenosis.
Theidealapproachforassessingthedegreeofsedation ofpatientsistouseexistingstandardscales.Sedationscales havebeenincreasinglyusedinpediatricintensivecareunits toguidetheadministrationofsedatives,evaluatingtheneed toincreasethedoseofthebasalsedationandtheneedto administerextradosesofsedation.12
TheCOMFORT-Bscaleiswidelyusedinstudiesassessing children’ssedationlevelsandithasproventobeadequate for the management of intubatedchildren in mechanical ventilation.9,13 Thisscale wasvalidatedforthePortuguese
language by Amoretti et al., in 2008.14 A recent study
showedthattheCOMFORT-Bscalealsodetects treatment-related changes in pain or distress intensity, and can effectivelybeusedtoguidesedationtreatmentincritically illchildren.15
Theresultsofthepresentstudyshowthatchildrenwho developedSGSarepotentiallythosethatareundersedated inthePICU,whichwasconfirmedbytwovariables:‘‘mean COMFORT-Bscore’’and‘‘percentageofCOMFORT-Bscores between23and30(undersedatedchildren).’’Dueto rest-lessness,thesechildrenrequired moredosesofadditional sedation,i.e.,dosesbeyondthoseprescribedroutinely by anintensivecareteam.Thisexplainsthefindingsinprevious studies,inwhichthenumberofadditionaldosesofsedation systematically emerged asan independentrisk factor for SGS.6,7
Thelackofsedationandtheconsequentmovementofthe ETTintheairwayhavebeenalreadycitedbyexpertsinthe fieldofpediatriclaryngologyasriskfactorsforSGS,16,17but
This studyfailedtodemonstrate‘‘daysintubated’’and ‘‘numberof additionaldoses ofsedation/daysintubated’’ assignificant riskfactors,probablybecauseof thelimited number of patients. However,these factors were already provedtobesignificantinthepreviousstudiespublished.
ItisparadoxicalthatcurrentlytheetiologyofmostSGS isendotrachealintubation,butontheotherhandthatthe ETTitselfisindicatedbyexpertstotreatacuteinjuriesafter intubation,servingasastentforthehealingofglotticand subglottic injuries.15 Itcould be inferred,therefore, that
the problemis probably not thetube itself--- considering thatthisisofthepropersizeforthechild---butthechild’s excessivemovementandthelengthoftimethetuberemains intheairway.
In conclusion, in this prospective study including only children beyondtheneonatalperiod,children who devel-opedSGSwerelesssedatedduringthetimetheyneededan ETTthanchildrenwhodidnotdevelopSGS,asmeasuredby theCOMFORT-Bscale.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Schweiger C, Smith MM, Manica D, Kuhl G, Carvalho PRA, MarosticaPJ.Incidenceofpost-intubationsubglotticstenosisin children:prospectivestudy.JLaryngolOtol.2013;127:399---403. 2.CordeiroAM, Fernandes JC, Troster EJ. Possible riskfactors associatedwithmoderateorsevereairwayinjuriesinchildren whounderwentendotrachealintubation.PedCrit CareMed. 2004;5:364---8.
3.JorgensenJ,WeiJL,SykesKJ,KlemSA,WeatherlyRA,Bruegger DE,etal.Incidenceofandriskfactorsforairwaycomplications followingendotrachealintubationforbronchiolitis.Otolaryngol HeadNeckSurg.2007;137:394---9.
4.Meneghini L, Zadra N, Metrangolo S, Narne S, Giusti F. Post-intubation subglottal stenosis in children: risk factors andpreventionin pediatricintensive care.MinerAnestesiol. 2000;66:467---71.
5.BishopMJ.Mechanismsoflaryngotrachealinjuryfollowing pro-longedtrachealintubation.Chest.1989;96:185---6.
6.Smith MM,Kuhl G,CarvalhoPA,MarosticaPJ.Flexible fiber-optic laryngoscopy in the first hours after extubation for theevaluationoflarynngeallesions dueto intubationinthe pediatric intensive care unit.IntJPediatr Otorhinolaryngol. 2007;71:1423---8.
7.ManicaD,SchweigerC,MarosticaPJ,KuhlG,CarvalhoPR. Asso-ciationbetweenlengthofintubationandsubglotticstenosisin children.Laryngoscope.2013;123:1049---54.
8.2005AmericanHeartAssociation(AHA)guidelinesfor cardiopul-monaryresuscitation(CPR)andemergencycardiovascularcare (ECC) ofpediatric andneonatalpatients:pediatricadvanced lifesupport.Pediatrics.2006;117:e1005---28.
9.IstaE,vanDijkM,TibboelD,deHoogM.Assessmentofsedation levelsinpediatricintensivecarepatientscanbeimprovedby usingtheCOMFORT‘‘behavior’’scale.PediatricCritCareMed. 2005;6:58---63.
10.FanLL,FlynnJW,PathakDR.Riskfactorspredictinglaryngeal injuryinintubatedneonates.CritCareMed.1983;11:431---3. 11.Grundfast KM, Camilion FS, Pransky S, Barber CS, Fink R.
Prospectivestudyofsubglotticstenosisinintubatedneonates. AnnOtolRhinolLaryngol.1990;99:390---5.
12.DeJongheB,CookD,Appere-de-VecchiC,GuyattG,MeadeM, OutinH.Usingandunderstandingsedationscoringsystems:a systematicreview.IntensiveCareMed.2000;26:275---85. 13.VanDijkM,PetersJW,vanDeventerP,TibboelD.The
COMFORT-BehaviorScale:atoolforassessingpainandsedationininfants. AmJNurs.2005;105:33---6.
14.AmorettiCF,RodriguesGO,CarvalhoPR,TrottaEA.Validationof sedationscoresinmechanicallyventilatedchildrenadmittedto atertiarypediatricintensivecareunit.RevBrasTerIntensiva. 2008;20:325---30.
15.BoerlageAA,Ista E,DuivenvoordenHJ,deWildt SN,Tibboel D,vanDijkM.TheCOMFORT-behaviorscaledetectsclinically meaningfuleffectsofanalgesicandsedativetreatment.EurJ Pain.2015;19:473---9.
16.MonnierP.Pediatricairway surgery:management of laryngo-tracheal stenosisin infantsand children.Berlin,Heidelberg: Springer-Verlag;2011.