REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
Publicação Oficial da Sociedade Brasileira de Anestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
The
practice
of
postanesthesia
visits
---
a
questionnaire
study
Tobias
Fink
a,
Hauke
Rensing
b,
Thomas
Volk
a,
Ragnar
Huhn
c,
Alexander
M.
Mathes
c,∗aSaarlandUniversityHospital,IntensiveCareandPainTherapy,DepartmentofAnesthesiology,Homburg,Germany bLeopoldinaHospital,DepartmentofAnesthesiologyandCriticalCareMedicine,Schweinfurt,Germany
cDüsseldorfUniversityHospital,DepartmentofAnesthesiology,Düsseldorf,Germany
Received1March2016;accepted28July2016 Availableonline21August2016
KEYWORDS
Postanesthesiavisit; Anesthesia;
Complication; Questionnaire
Abstract
Backgroundandobjective: Regular postanesthesia visits allow the detection of anesthesia related complications and increase patient satisfaction. Consequently, the performance of postanesthesia visitshasbeenrecommendedafter certaintypes ofanesthesia.However, no dataisavailableconcerningthecurrentpracticeofpostanesthesiavisits.Therefore,thisstudy was designed to investigate quantity, organization, contents, significance and problems of postanesthesiavisitsinGermany.
Methods:Forthisprospectiveclosed-designsurvey,aquestionnaire,consistingof13questions, wasdesignedandtestedforobjectivity,reliabilityandvalidity.Subsequently,3955registered anesthesiologistswerecontactedviaemailtoanswerthissurvey.
Results:Returnratewas31.4%;958questionnaireswereincludedinthestudy.Onlyasmall portionofpatientswasestimatedtoreceiveapostanesthesiavisit(median:20.0%).In hospi-talswithaspecificpostanesthesiavisitservice,thisnumberwassignificantlyhigher(median: 65.0%,p<0.001)vs.nopostanesthesiavisitservice.Postanesthesiavisitsusuallylastedlessthan 5minutes(60.0%),andweretypicallyconductedonthedayofsurgery(48.0%),afterregular workinghours(55.0%).38.0%oftherespondentsreportedtodetectperioperativecomplications intermittentlyduringtheir visits.While98.0%ofallrespondentsbelievethatpostanesthesia visitsimprovethequalityoftheirownwork,86.0%oftheparticipantscomplainalackoftime forthistask.
Conclusions: Our survey indicates that current working conditions prevent a regular postanesthesiavisitroutine.Consideringthehighappreciationofpostanesthesiavisitsby anes-thesiologists,aswellastherelevantincidenceofpostoperativecomplicationsdetectedduring thesevisits,itseemsdesirabletoconsiderorganizationalimprovementsforpostanesthesiacare. ©2016SociedadeBrasileiradeAnestesiologia.Publishedby ElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense(
http://creativecommons.org/licenses/by-nc-nd/4.0/).
∗Correspondingauthor.
E-mail:alexander.mathes@med.uni-duesseldorf.de(A.M.Mathes).
http://dx.doi.org/10.1016/j.bjane.2016.07.008
0104-0014/©2016SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.ThisisanopenaccessarticleundertheCC
PALAVRAS-CHAVE
Visitapós-anestésica; Anestesia;
Complicac¸ão; Questionário
Apráticadevisitaspós-anestésicas---estudodeumquestionário
Resumo
Justificativaeobjetivo:As visitas regulares pós-anestesia (VPA) permitem detectar complicac¸ões relacionadas à anestesia e aumentar a satisfac¸ão do paciente. Portanto, a realizac¸ão de VPAfoi érecomendada apóscertos tiposde anestesia.Porém, não hádados disponíveis sobreaprática atual deVPA. Logo, este estudofoi projetadopara investigar a quantidade,organizac¸ão,conteúdo,significânciaeproblemasdaVPAnaAlemanha.
Método: Para esta pesquisa de natureza fechada e prospectiva, um questionário com 13 perguntasfoicriadoetestadoparaidentificaraobjetividade,confiabilidadeevalidade. Pos-teriormente,3.955anestesiologistasregistradosforamcontatadosviae-mailpararespondera essapesquisa.
Resultados: Ataxaderetornofoide31,4%;958questionáriosforamincluídosnoestudo. Ape-nasumapequenapartedospacientesfoidesignadaparareceberumaVPA(mediana:20,0%). Emhospitaiscomservic¸oespecíficodeVPA,essenúmerofoisignificativamentemaior (medi-ana:65,0%,p<0,001)vs.ausênciadeservic¸odeVPA.AsVPAnormalmentedurarammenosde 5minutos(60,0%)eforamtipicamenteconduzidasnodiadacirurgia(48,0%),apósoturno nor-maldetrabalho(55,0%).Dentreosqueresponderamoquestionário,38,0%relataramdetectar complicac¸ões perioperatóriasdeforma intermitenteduranteasvisitas. Enquanto98,0% dos entrevistadosacreditamqueasVPAmelhoramaqualidadedeseuprópriotrabalho,86,0%se queixamdefaltadetempoparaessatarefa.
Conclusões:Nossapesquisaindicaqueascondic¸õesatuaisdetrabalhoimpedemarealizac¸ão rotineiradeVPA. Considerandoaalta valorizac¸ão dasVPApor anestesiologistas, bemcomo aincidência relevante decomplicac¸ões nopós-operatório detectadasduranteessas visitas, parecedesejávelconsiderarmelhoriasorganizacionaisparaaassistênciaapósaanestesia. ©2016SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigoOpen Accesssobumalicenc¸aCCBY-NC-ND(
http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Theideaandrelevanceofpostanesthesiavisits (PAVs)was mentioned as early as 1934, with the recommendation that anesthesiologistsshould visit their patients regularly in the first two days after surgery to obtain information about the patient’s condition.1 Yet, in today’s
anesthe-siatextbooks,thiselementofperioperativecareismostly neglected.2Whilethereisextensiveliteratureonpotential
complicationsandsideeffectsofgeneralandregional anes-thesia,theperformanceof apersonalvisittodetectsuch complicationsappearstobeforgottenpractice.
Only due tothe currently increasing demandfor qual-itymanagement,theimportanceofPAVs hasinpart been revived.3Asmallnumberofstudieshavedemonstratedthat
theperformanceofPAVsmayimprovepatientsatisfaction4---6
andphysicianrecognition.7InanIndianstudy,patientswho
receivedaPAVweresignificantlymoresatisfiedthanthose withoutaPAV.8SimilarresultswereobtainedinanAustrian
study,showingthata singlePAVmaysignificantlyincrease patientsatisfaction.9AstheperfecttimeforPAVs,12---24h
after anesthesia was suggested.10 Multiple questionnaires
havebeen implemented todetermine patientsatisfaction postoperatively(Fig.1).11---13 However,‘‘receiving
informa-tion’’ and ‘feeling safe’ appear to be strong predictors of patient satisfaction.14 Therefore, for the purpose of
PAVs, face-to-face interviews may be more suitable than a questionnaire in determining patient satisfaction with
anesthesia.6 To improve perioperative quality control,
the implementation of an interdisciplinary postanesthesia servicewassuggested.5
The German Society of Anaesthesiology and Intensive CareMedicine (DGAI)guidelinesfor regionalanesthesiain obstetricsspecificallyrequireapostanesthesiavisitwithin 24h.15Fortherecognitionofintraoperativeawareness,PAV
questioning of thepatienthas been recommended.16
Fur-ther,DGAIguidelinesforthecollaborationbetweensurgeons andanesthetistsexplicitly indicatethat theanesthetist is responsible for the detection and treatment of anesthe-siarelatedcomplications.17---20Similarguidelineshavebeen
published internationally: The American Society of Anes-thesiologistsexplicitlydefinepostanestheticevaluationand therapy asthe responsibility ofan anesthesiologist.21 The
Royal College of Anaesthetists has publishedspecific rec-ommendationsforpost-anesthesiavisitsanddefinespatient groups that shouldbevisitedwithin 24h.22 Althoughboth
surgeons and anesthetists are required to inform each otheraboutcomplicationsthatmightbeattributabletothe otherspecialty,17---20itappearslikelythatcertainanesthesia
related complications --- like sensory and motor deficien-cies afterregional anesthesia---may remainunnoticed by non-anesthesiologists.
registered anesthesiologists and performed a survey con-sisting of 13 questions, evaluatingquantity, organization, contents,significanceandproblemsofpostanesthesiavisits.
Methods
Conceptionofthequestionnaire
InaccordancewithGermanregulations,noethicalapproval wasnecessaryforthissurvey,asonlyanonymizeddatawas collected(§15MBO-Ä),andnopatientswereinvolved (non-AMG-non-MPG-study).The questionnairewascreated with supportof theCentrefor Surveys,Opinions,andAnalyses (ZUMA,Mannheim,Germany)(foraflowchartofthestudy process)(Fig.2).Criteriaofobjectivityweremetbyusinga closedmultiple-choicedesignforthequestionnaire, exclud-ingthepossibilityofinterpretationalerrors.Theprocessof validation was performed in the Department of Anesthe-siology, SaarlandUniversity Hospital,using astandardized model of cognitive pretesting. In total, 30randomly cho-sen anesthesiologists were tested. In the final version of thequestionnaire,nodifferencesbetweenthemeasureand the underlyingconstructwere observed. Retestreliability was evaluated after validation of the questionnaire. Fif-teencandidatesthatunderwentthevalidationprocesswere randomly chosen to complete the survey a second time afterawaitingperiodof10days,withoutpriornotice.The
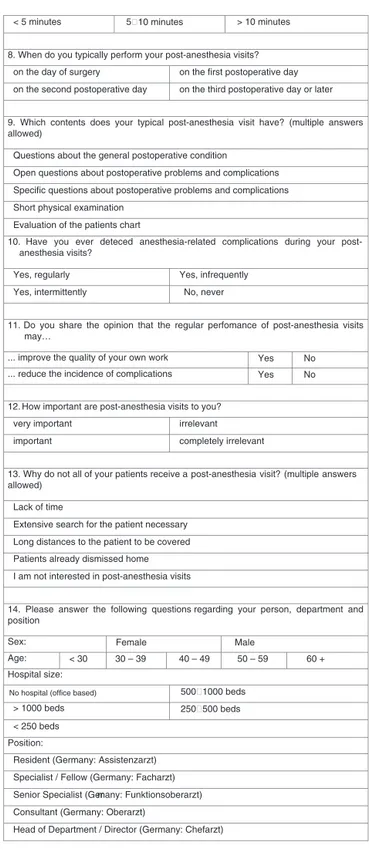
Translated Questionnaire
Please answer the following questions regarding your practice of post-anesthesia visits
for elective, non-ICU patients:
1. Please estimate the percentage of patients anesthetized in your hospital in the last
year that are visited postoperatively by an anesthesiologist.
0 – 10 – 20 – 30 – 40 – 50 – 60 – 70 – 80 – 90 – 100%
There are generally no postanesthesia visits in our hospital.
2. Isthere a post-anesthesiaservice in yourhospital that has the duty toperform
postanesthesia visits?
Yes No
3. Which information about the post-anesthesia visit is recorded in the patient chart?
Time Contents
Duration Documentation is not performed
4. Please estimate the percentage of patients anesthetized by yourself in the last
year that have received a post-anesthesia-visit
0 – 10 – 20 – 30 – 40 – 50 – 60 – 70 – 80 – 90 – 100% ... by yourself
0 – 10 – 20 – 30 – 40 – 50 – 60 – 70 – 80 – 90 – 100% ... by a colleague
5. When do you typically perform post-anesthesia visits?
Within regular working hours After regular working hours
6. How often have you performed anesthesia-v isits typically within the last year?
Less then once a week Every 2
Every 4
3 days
5 days
Only when member of a post-anesthesia-service
7. How long is your typical post-anesthesia visit per patient?
Figure1 Questionnaire.
< 5 minutes 5 10 minutes > 10 minutes
8. When do you typically perform your post-anesthesia visits?
on the day of surgery on the first postoperative day
on the third postoperative day or later on the second postoperative day
9. Which contents does your typical post-anesthesia visit have? (multipleanswers
allowed)
Questions about the general postoperative condition
Open questions about postoperative problems and complications
Specific questions about postoperative problems and complications
Short physical examination
Evaluation of the patients chart
10. Have you ever deteced anesthesia-related complications during your
post-anesthesia visits?
Yes, infrequently Yes, regularly
No, never Yes, intermittently
11. Doyou share the opinion that the regular perfomance of post-anesthesia visits
may…
... improve the quality of your own work Yes No
... reduce the incidence of complications Yes No
12. How important are post-anesthesia visits to you?
irrelevant very important
completely irrelevant important
13. Why do not all of your patients receive a post-anesthesia visit? (multiple answers
allowed)
Lack of time
Extensive search for the patient necessary
Long distances to the patient to be covered
Patients already dismissed home
I am not interested in post-anesthesia visits
14. Please answer the following questions regarding your person, departmentand
position
Sex: Female Male
Age: 40 – 49 50 – 59 60 +
500 1000 beds
> 1000 beds 250 500 beds
30 – 39 < 30
Hospital size:
< 250 beds
Position:
Resident (Germany: Assistenzarzt)
Specialist / Fellow (Germany: Facharzt)
Senior Specialist (Germany: Funktionsoberarzt)
Consultant (Germany: Oberarzt)
Head of Department / Director (Germany: Chefarzt)
No hospital (office based)
Figure1 (Continued)
sequenceofquestionsandanswerswasarbitrarilychanged. Retestreliabilitywas0.872(Pearsoncorrelation;p<0.01).
Implementationofthesurvey
Thequestionnairewasbuiltusingacommercialweb-based online platform (EquestionnaireTM). Using a commercial
serial email program (SuperMailerTM), 3955 members of
Conception
Objectivity: closed multiple-choice design Validity: cognitive pretesting (30 candidates)
Reliability: retesting (15candidates)
3955 anesthesiologists contactcted (e-mail)
3285 successful e-mail contacts
1024 returned questionnaires
958 questionnaires evaluated
Excluded: 12 without correct ID 46 multiple surveys for same ID
2 technical errors 6 internal inconsistencies Reminder after 2 and 4weeks (e-mail)
670 e-mail failure notices
Figure2 Flowchartofthestudyprocess.ID,identifying
num-berforeachanesthesiologist.
Medicine(DGAI)werecontacted.Anonymizationwas estab-lishedbyassigningIdentificationNumbers(ID)toeachemail. Afterawaitingtimeoftwoandfourweeks,areminderwas sentbyemailtorecruitasmanyrespondentsaspossible.
AnysurveythatwascompletedwithoutacorrectID,or thatcontainedanIDthatwasfoundinmorethanone sur-vey,resultedin theexclusionof allaffectedrespondents. Anyquestionnairethatwascompletedinlessthan120swas tested for internal consistency by comparingthe answers ofdifferentitemsthatwouldresultinimpossible constella-tions.
Statisticalanalysis
Statistical evaluation was performed using the software SigmaPlot 9.0 with SigmaStat integration (Erkrath, Ger-many). Parametric data was compared using a one-way ANOVA,afterpassingnormalitytest,followedbyaposthoc multiple comparisonaccording to the Student---Newmans---Keulsmethod.Non-parametricdatawerecomparedusinga Mann---WhitneyUtest,followedbyaposthocmultiple com-parisonaccordingtotheDunn’smethod.Avalueforp<0.05 wasconsideredsignificant.
Results
Responderrateandexclusions
Of3955emailaddressesprovidedbytheDGAI,670contacts resulted in e-mail failure notices; leaving 3285 function-ingemail addresses (Fig.2).Fromthese, 1024completed surveys were returned (return rate=31.2%). In total, 66 respondentshadtobeexcludedbecausetheydidnot con-tainacorrectIDnumber(n=12),becauseofmorethanone completedquestionnaireforthe sameID(n=46),because oftechnicaldifficulties(n=2),orbecauseofinconsistencies withintheansweredquestionnaires(n=6).Finalassessment ofthesurveyincluded958completedquestionnaires. Demo-graphicdataisdisplayedinTable1.
Table1 Demographicdata.
Total
n(%)
Gender
Female 200(21.03%)
Male 751(78.97%)
Age
<30years 7(0.73%) 30---39years 359(37.51%) 40---49years 360(37.62%) 50---59years 199(20.79%) >60years 32(3.34%)
Sizeofhospital
Notworkinginahospital(office-based) 7(0.73%) >250beds 171(17.85%) 251---500beds 284(29.65%) 501---1000beds 267(27.87%) >1000beds 233(24.32%)
Position
Resident 186(19.42%) Specialist/Fellow 220(22.96%) SeniorSpecialist 54(5.64%) Consultant 310(32.36%) HeadofDepartment/Director 188(19.62%)
QuantityofPAV
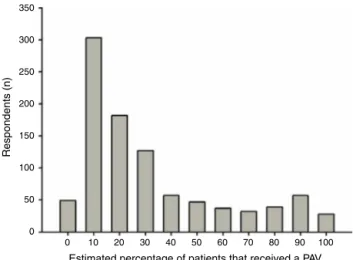
Respondents estimated that only a small portion of all anesthetizedpatientsintheirinstitutionhadreceivedaPAV duringthe lastyear (median:20.0%;mean 31.9%;25thto 75thpercentile:10.0---42.5%)(Fig.3).While7.8%of respon-dentsclaimthattheyemployaspecificPAVservice,16.7% respondthattheydonotperformanyPAVat all.In hospi-talswithaPAVservice,thenumberofvisitedpatientswas significantly higher (median: 65.0%, mean 61.4%, 25th to 75thpercentile:30.0---90.0%),comparedtohospitals with-outsuchaservice(median:20.0%,mean29.9%,25thto75th percentile:10.0---40.0%;p<0.001vs.noPAVservice)(Fig.4).
350
300
250
200
Respondents (n)
150
100
50
10 0
Estimated percentage of patients that received a PAV
20 30 40 50 60 70 80 90 100 0
Figure3 Performanceofpostanesthesiavisits.PAV,
120 P<.001
100
80
60
40
Hospital (%)
20
0
Without PAV service With PAV service
Figure 4 Relevance of a postanesthesia service. Data are
presented as median values, 25th to 75th percentiles, min-imum/maximum and outliners (circles). PAV, postanesthesia visit.
PAVservicewasestablishedmoreofteninsmallerhospitals; however, this was not statistically significant (<250 beds: 26%,251---500beds:35%,501---1000beds:20%,>1000beds: 19%).
The estimatedpercentageofpatientsthatwere anaes-thetized and visited by the respondents in the last year (median:20%)wassimilartotheanticipatedpercentageof patientsanesthetizedbytherespondentbutvisitedby col-leaguesoftherespondents(median:20%).Only22.0%ofall respondentsperformPAVsonadailybasis,whilealmostthe sameamountofanesthetistsvisitstheirpatientsless than onceaweek.
Timing,durationandcontentsofPAV
Mostpatientswerevisitedonthedayofsurgeryandonthe followingday.Lessthan10percentofpatientswerevisited on subsequentdays (Fig. 5). Durationof PAVs is typically less than 5min, and rarely lasts longer than 10min. Most PAVsincludedface-to-faceinterviewswithopenandclosed questions regarding the general condition of the patient, problemsandcomplications.Onethirdof therespondents reviewedthepatient’scharts(notevaluatedwhetherpaper or electronic), and only a minority performed a physical examination of their patients. A great number of anes-thetists documented the PAV in the chart; however, in 28.8%, no informationwas documented at all. Almost all respondents detected postoperative complications during PAV,41.0%infrequently,33.7%intermittently,and1.7% reg-ularly.
SignificanceandproblemsofPAV
Almostall anesthetistsbelieved thatperformance of PAVs improvedthequalityoftheirownwork,and76.0%agreed
500
400
300
200
Respondents (n)
100
48.0% 43.9% 4.5% 3.6%
0
Day of surger y
1.post-OP da y
2.post-OP da y
After 2.post-OP da y
Figure5 Timingofpostanesthesiavisits.Post-OP,
postopera-tive.
1000
800
600
400
Respondents (n)
200
95.2%
Lac k of time
Patient dismissed Long distance s
Extensiv e search
Lack of interes
t 40.0% 25.9% 23.4% 2.3% 0
Figure6 Problemthatpreventstheregularperformanceof
postanesthesiavisits.PAV,postanesthesiavisit.
thatregularPAVsmightreduceperioperativecomplications. Consequently,over85.0%oftherespondentsvaluedPAVsas veryimportantorimportant,while13.0%wereindifferent withrespecttothatquestion.Onlyaminoritybelievedthat PAVswereirrelevantorcompletelyirrelevant.
Almost all respondents complained a lack of time for performance of PAVs. In over a third of the cases, the anesthetists claimed that the patients had already been dischargedfromthehospital.Interestingly,25.9%of respon-dentsstatedthatnotallpatientshadtobeseenbecauseof longdistancesthathadtobecoveredtoreachthepatient (Fig.6).
Discussion
aservice. MostPAVs areconductedontheday ofsurgery, lasting usually less than 5min, and are performed after regular working hours. Most anesthetists claim to detect postoperativecomplicationsduringtheirvisits.Althoughthe majorityofanesthesiologistsbelievethatPAVsmayimprove thequalityof their ownwork andmay reduce anesthesia relatedcomplications,theycriticizealackoftimeforthis duty.
Althoughourresultsindicatethatthenumberofpatients thatarevisitedpostoperativelyisratherlow,thequestion ariseswhatpercentageofpatientswe wouldliketoreach withPAVs.Theanswertothiscomplexissuedependsonthe purposethatweattributetoPAVs.Ontheonehand,if qual-itymanagement should bethe only reason for PAVs, spot checksmaybesuitableandsufficient.Ontheotherhand,if weaimforimprovementsinpatientsatisfaction,thecurrent performanceofPAVsmayberegardedtoolow.
Patientsatisfactioncouldbereachedbyseveralmeans, andmultiplequestionnaireshavebeen developedto mea-sure satisfaction after receiving general anesthesia.11---13
However, the performance of a postoperative question-naireitselfdoesnotincreaseoverallanesthesiasatisfaction significantly.9 Mostimportantly,patients expressthe need
tobeinformedandtofeelsafe.14Bothneedscannotbe
ful-filledbyapersonwhoisneitherananesthesiologistnorhas been involved in the anestheticprocedure of the specific patient.
Previousstudieshaveshownthatpatientsatisfactionmay be significantly improved by PAVs, especially when using face-to-face interviews.6 Capuzzo and colleagues
demon-stratedthatmorethantwovisitsbyanesthesiologistsafter surgery may significantly increase patient satisfaction.4
However, other reports suggest that increasing numbers of PAV do not necessarily increase patient contentment.7
Yet,thequalityofthe visitsmay bemoreimportantthan thenumber of times the patient is visited.23 The perfect
timefor suchavisitappearstobeafter12---24hafterthe procedure.10
Whilequality managementand ‘consumersatisfaction’ may certainly be regarded important attributes of mod-ernanesthesiology,medicalreasonscouldbemorerelevant triggersfortheperformanceofPAVs.ThepurposeofPAVs, whenintroduced in1934,wastoimprovepatientcare.1It
wasthought that the anesthesiologist should examine his patienttodetermineanycomplicationsduetoanesthesia. Althoughtoday,patientsareusuallytransferredtoa Post-operativeCareUnit(PACU)andfurthertoasurgicalward, thedetectionofanesthesiarelatedcomplicationsremains thespecialtyoftheanesthesiologist.17---20
Certainly, we trust our colleagues from the surgi-cal specialties that they will notice anesthesia related complicationsaswell,especiallywhentheyareeasily per-ceptible.Wefurtherbelievethattheywillinformusabout thesecomplicationsimmediately,shouldtheyrequireexpert help.However,ourstudy indicates that mostrespondents have detected postoperative complications during their PAVs;hardly anyhave never noticedany complications at all.
Unfortunately,thetypeofcomplicationandtheir treat-mentwasnotfurtherdefinedinourstudy,anditisunknown whetherthesecomplicationswouldhave goneunobserved without PAVs.Only alimited number ofrespondents have
reportedthetypeofcomplicationaftertheinitial question-naire;asthiswasnotevaluatedsystematically, thepower of this analysis is weak. Typical complications observed included insufficient analgesia, postoperative nausea and vomiting, vocal cord paralysis, allergic reactions, urinary retention and intraoperative awareness. The anesthesiol-ogistmay helpnot only indetecting these complications, but mayalsosupporttheir treatment,guiding thepatient throughtheprocessthatappearsnecessaryafterthe anes-theticprocedure.Inapilotstudy,systematicpostoperative visits by anesthesiologists reduced the need for internal medicinevisitssignificantlyinpatientswithhipfractures.24
ItappearsreasonabletoassumethatwithoutPAVs,a cer-tainpercentageofanesthesiarelatedcomplicationswould have remainedunnoticed.This mayespeciallybetruefor ambiguoussymptomsandobscuresyndromes,likethe anti-cholinergic syndrome, or sensory and motor deficiencies after regional anesthesia. Further, we believe that the reportedcomplicationscouldhavecontributedtoalonger hospitalstayorincreasedtreatmentcost,iftheywouldhave not been observed. Thus, it is reasonable toassume that PAVsmaynotonlyallowearlyandspecifictreatmentofsuch complications,butmayalsoreducehospitalstay,mortality andcost.10
Based on our findings, a lack of time appears to be themajorproblemthatpreventstheregularconductionof postanesthesiavisits.Organizationalimprovementsof work-ing conditions may be necessary to allow a regular PAV routine.Ourstudyshowsthattheimplementationofa des-ignated PAVservice might bea useful waytosignificantly increase the number of patients visited postoperatively. Unfortunately,nospecificinformationabouttheseservices is available fromoursurvey.Yet,personal communication indicatesthathospitalswithsuchaserviceallowtheir anes-thesiologistsaspecifictimeforPAVs(e.g.1hattheendof the shift), or employ one anesthetist to perform all PAVs during oneday. Awritten questionnaire couldbeauseful aidtooptimizepostoperativevisitsandpatientsatisfaction. Asourdatashows,PAVservicesdidnotreachallpatients, and the absence of such a service did not mean that no patient was visited. This indicates that the implementa-tion of a PAV service alone is not sufficient to optimize postanesthesiacareandmaynottheonlysolutionfor this task. Especiallyregarding costeffectiveness, future stud-iesneed toevaluatewhich model issuperior indetecting complicationsinthepostanesthesiasetting.Sufficienttime, precise organizational structures (e.g. standard operating procedures)andmaybeeveninclusionofthisaspectin res-identtrainingcouldbeofhighvaluetoestablishasolidPAV routine.
respondents shouldhave, by position,a broad perception of postanesthesia care. Further, our survey resulted in a responserateof31percent.Althoughremindersweresent and planning of this study involved an expert institution forsurveys,wewereunabletoreachahigherreturnrate. However,wearestillwithinthetypicalrangeforpublished questionnairestudies inacademic journals,25 with33
per-centbeingtheoverallmeanforonlinequestionnaires.Thus, webelievethatourdatapoolisasufficientbasisforour eval-uations.Finally,somerespondentsmayhavebeenmembers ofthesameinstitution.Yet,aswereceivedmorethan180 responses fromheads of staff,it is reasonable toassume thatwe receivedinsightintoat least 180departments, if notmanymore.Thisshouldallowagoodoverviewoverthe practiceinasufficientnumberofhospitals.
We would liketoconclude that currently, onlya small numberofanesthesiologistsperformpostanesthesiavisits, mainlyduetoalack oftimefor thistask.Consideringthe high appreciation andsignificance of PAVs andthe poten-tialmedico-legalconsequencesoftheirneglect,itappears desirable to implement organizational improvements for postanesthesiacare.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Hesse F, Lendle L, Schoen R, et al. Allgemeinnarkose und örtliche Betäubung. Zusammenfassende Darstellung für die Praxis auf pharmakologischerundklinischer Grundlage. New York:Barth;1934.
2.WitteW.Premedication,preoperaiveandpostoperativevisits. Importanceasreflectedinanaesthesiologytextbooks. Anaes-thesist.2007;56:1252---6.
3.DahmenKG,AlbertDM.Anapproachtoqualitymanagementin anaesthesia:afocusonperiopertivecareandoutcome.EurJ AnaesthesiolSuppl.2001;23:4---9.
4.Capuzzo M, Gilli G, Paparella L, et al. Factors predic-tive of patient satisfaction with anesthesia. Anesth Analg. 2007;105:435---42.
5.BothnerU,SchwilkB,SteffenP,etal.Perioperative monitor-ingofthecourseofanesthesia,thepostanesthesia visitand inquiryofpatientsatisfaction.Aprospectivestudyof parame-tersinprocessandoutcomequalityinanesthesia.Anasthesiol IntensivmedNotfallmedSchmerzther.1996;31:608---14.
6.BauerM,BöhrerH, Aichele G, et al. Measuring patient sat-isfactionwithanaesthesia:perioperativequestionnaireversus standardisedface-to-faceinterview.ActaAnaesthesiolScand. 2001;45:65---72.
7.ZvaraDA, Nelson JM,Brooker RF, et al. The importance of thepostoperativeanestheticvisit:dorepeatedvisitsimprove patient satisfaction or physician recognition? Anesth Analg. 1996;83:793---7.
8.GebremedhnEG,ChekolWB,AmberbirWD,etal.Patient sat-isfactionwithanaesthesiaservicesand associated factors at theUniversityofGondarHospital,2013:across-sectionalstudy. BMCResNotes.2015;8:377.
9.SaalD,HeideggerT,NueblingM,etal.Doesapostoperative visitincreasepatientsatisfactionwithanaesthesiacare?BrJ Anaesth.2011;107:703---9.
10.Bajwa SJS, Takrouri MSM. Post-operative anesthesia rounds: needofthehour.AnesthEssaysRes.2013;7:291---3.
11.Schiff JH, Fornaschon AS, Frankenhauser S, et al. The Heidelberg peri-anaesthetic questionnaire-development of a new refined psychometric questionnaire. Anaesthesia. 2008;63:1096---104.
12.Auquier P, Pernoud N, Bruder N, et al. Development and validationofaperioperativesatisfactionquestionnaire. Anes-thesiology.2005;102:1116---23.
13.CaljouwMA,vanBeuzekomM,BoerF.Patient’ssatisfactionwith perioperativecare:development,validation,andapplicationof aquestionnaire.BrJAnaesth.2008;100:637---44.
14.CapuzzoM,LandiF,BassaniA,etal.Emotionaland interper-sonalfactorsaremostimportantforpatientsatisfactionwith anaesthesia.ActaAnaesthesiolScand.2005;49:735---42.
15.Durchführung von Analgesie- und Anästhesie in der Geburtshilfe.Hisom A, Sorgatz H, editors. Entschließungen - Empfehlungen - Vereinbarungen: Ein Beitrag zur Qual-itätssicherung in der Anästhesiologie. Ebelsbach, Germany: AktivDruck&VerlagGmbH;2011.p.183---90.
16.Schneider G. Intraoperative awareness. Anästhesiol Inten-sivmedNotfallmedSchmerther.2003;38:75---84.
17.Vereinbarung über die Zusammenarbeit bei der operativen Patientenversorgung desBerufsverbandesDeutscher Anästhe-sistenunddesBerufsverbandesderDeutschenChirurgen.Hisom A, Sorgatz H, editors. Entschließungen - Empfehlungen -Vereinbarungen:EinBeitragzurQualitätssicherunginder Anäs-thesiologie.Ebelsbach,Germany:AktivDruck&VerlagGmbH; 2011.p.9---12.
18.Vereinbarung über die Zusammenarbeit in der Gynäkologie undGeburtshilfe.HisomA,SorgatzH,editors.Entschließungen - Empfehlungen - Vereinbarungen: Ein Beitrag zur Qual-itätssicherung in der Anästhesiologie. Ebelsbach, Germany: AktivDruck&VerlagGmbH;2011.p.19---24.
19.Vereinbarung über die Zusammenarbeit bei der operativen Patientenversorgung desBerufsverbandesDeutscher Anästhe-sistenunddesBerufsverbandesderÄrztefürOrthopädie.Hisom A, Sorgatz H, editors. Entschließungen - Empfehlungen -Vereinbarungen:EinBeitragzurQualitätssicherunginder Anäs-thesiologie.Ebelsbach,Germany:AktivDruck&VerlagGmbH; 2011.p.31---6.
20.Vereinbarung über die Zusammenarbeit in der HNO-Heilkunde.Hisom A, Sorgatz H, editors. Entschließungen - Empfehlungen - Vereinbarungen: Ein Beitrag zur Qual-itätssicherung in der Anästhesiologie. Ebelsbach, Germany: AktivDruck&VerlagGmbH;2011.p.25---6.
21.American Societyof Anesthesiologists.Guidelines forpatient careinanesthesiology.ASAHouseofDelegates;2011.p.1---4.
22.SimpsonDK,WalburnB.Post-operativecare.In:PhillipsJ, edi-tor.RaisingtheStandard:acompendiumofauditrecipes.New York:RoyalCollegeofAnaesthetists;2012.p.128---9.
23.KlockPA,RoizenMF. Moreorbetter--- educatingthepatient abouttheanaesthesiologist’sroleasperioperativephysician. AnesthAnalg.1996;83:793---7.
24.Foss NB, Christensen DS, Krasheninnikoff M, et al. Post-operative rounds by anaesthesiologists after hip fracture surgery: a pilot study. Acta Anaesthesiol Scand. 2006;50: 437---42.