REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Comparison
of
postoperative
analgesia
with
methadone
versus
morphine
in
cardiac
surgery
夽
Ana
Carolina
Carvalho
a,
Fábio
Jean
Goulart
Sebold
b,
Patrícia
Mello
Garcia
Calegari
b,
Benhur
Heleno
de
Oliveira
b,
Fabiana
Schuelter-Trevisol
c,d,∗aUniversidadedoSuldeSantaCatarina(Unisul),CursodeMedicina,CampusTubarão,Tubarão,SC,Brazil bHospitalNossaSenhoradaConceic¸ão(HNSC),Anestesiologia,Tubarão,SC,Brazil
cUniversidadedoSuldeSantaCatarina(Unisul),ProgramadePós-Graduac¸ãoemCiênciasdaSaúde,Tubarão,SC,Brazil dHospitalNossaSenhoradaConceic¸ão(HNSC),CentrodePesquisasClínicas,Tubarão,SC,Brazil
Received3August2016;accepted26September2017 Availableonline17January2018
KEYWORDS
Methadone; Morphine;
Postoperativepain; Cardiacsurgery
Abstract
Backgroundandobjectives: Painisanaggravatingfactorofpostoperativemorbidityand mor-tality.Theaimofthisstudywastocomparetheeffectsofmethadoneversusmorphineusingthe numericalratingscaleofpainandpostoperativeon-demandanalgesiainpatientsundergoing myocardialrevascularization.
Method: Arandomized,double-blind,parallelclinicaltrialwasperformedwithpatients under-goingcoronaryarterybypassgrafting.Thesubjects wererandomlydividedinto twogroups: morphinegroup andmethadonegroup.Attheend ofcardiacsurgery,0.1mg.kg−1adjusted bodyweightofmethadoneormorphinewasadministeredintravenously.Patientswerereferred totheICU,wherethefollowingwasassessed:extubationtime,timetofirstanalgesicrequest, numberofanalgesicandantiemeticdrugdoseswithin36h,numericalpainscaleat12,24,and 36hpostoperatively,andoccurrenceofadverseeffects.
Results:Eachgroupcomprised50patients.Methadoneshowed22%higherefficacythan mor-phine asityieldedanumber-needed-to-treatscoreof6andnumber-needed-to-harm score of 16. The methadone group showed a mean score of 1.9±2.2 according to the numeri-cal pain scaleat 24h after surgery, whereasas the morphinegroup showed a mean score of2.9±2.6(p=0.029). The methadone group required less morphine (29%) thanthe mor-phinegroup(43%)(p=0.002).However,thetimetofirstanalgesicrequestinthepostoperative periodwas145.9±178.5mininthemethadonegroup,and269.4±252.9inthemorphinegroup (p=0.005).
夽 StudyconductedatHospitalNossaSenhoradaConceic¸ão(HNSC),Tubarão,SC,Brazil. ∗Correspondingauthor.
E-mail:fastrevisol@gmail.com(F.Schuelter-Trevisol).
https://doi.org/10.1016/j.bjane.2017.12.001
0104-0014/©2017SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.ThisisanopenaccessarticleundertheCC
Conclusions: Methadone was effective for analgesiain patients undergoing coronary artery bypassgraftingwithoutextracorporealcirculation.
©2017SociedadeBrasileiradeAnestesiologia.Publishedby ElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
PALAVRAS-CHAVE
Metadona; Morfina;
Dorpós-operatória; Cirurgiacardíaca
Comparac¸ãodaanalgesiapós-operatóriacomusodemetadonaversus morfina emcirurgiacardíaca
Resumo
Justificativaeobjetivos: Adoréfatoragravantedamorbidadeemortalidadepós-operatória. O objetivofoi comparar oefeito da metadonaversusmorfina quanto à dore demandade analgesiapós-operatóriaempacientessubmetidosàrevascularizac¸ãodomiocárdio.
Método: Ensaioclínicorandomizado,duplo-cego,emparalelo.Pacientessubmetidosàcirurgia derevascularizac¸ãodomiocárdioforamrandomizadosporblocosemdoisgrupos:GrupoMorfina (Gmo) eGrupoMetadona(Gme). Nofimdacirurgia cardíaca,0,1mg.kg−1 pesocorrigidode metadonaoumorfinafoiadministradoporviavenosa.OspacientesforamlevadosàUTI,onde foramavaliadosotempoatéaextubac¸ãoeanecessidadedoprimeiroanalgésico,onúmerode dosesnecessáriasdeanalgésicoseantieméticosem36horas,aescalanuméricadedorem12, 24e36horasapósacirurgiaeaocorrênciadeefeitosadversos.
Resultados: Foramincluídos50pacientesemcadagrupo.Ametadonaapresentoueficácia22% maiordoqueamorfinacomNumberNeededtoTreat(NNT)de6eNumberNeededtoHarm
(NNH)de16.Gmeapresentoumédiadedorpelaescalanuméricaem24horasapóso procedi-mentode1,9±2,2emcomparac¸ãocomoGmo,cujamédiafoide2,9±2,6(p=0,029).OGme necessitoudemenosmorfinaderesgate29%doqueogrupoGmo43%(p=0,002).Entretanto, otempo atéanecessidadedeanalgésiconopós-operatóriofoi de145,9±178,5 minutosno GrupoGmeede269,4±252,9noGmo(p=0,005).
Conclusões: A metadona mostrou-se eficiente para a analgesia em cirurgias cardíacas de revascularizac¸ãodomiocárdiosemcirculac¸ãoextracorpórea.
©2017SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigo OpenAccess sobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Longitudinalmediansternotomyisthemostcommonlyused incision for cardiac surgeries. Associated with the use of retractors,itisthebestmethodforexposingthe anatomi-calregion.1However,thedescribedmethodassociatedwith anextendedsurgerytime,placeschestmusclesundergreat tensionandstresscausinggreatpaintothepatientinthe postoperative period, which hinders deep breathing and reducestheeliminationofsecretionsfromrespiratorytract thatmaytriggeratelectasisandrespiratoryinfections.2
Despitetheadvancesinanalgesicdrugs,differentroutes ofadministration,andnon-pharmacologicaltechniquesfor painrelief,thisisstillconsideredanimportant postopera-tiveproblemand,todate,thereisnostandardizedprotocol in several hospitals. Among the options for postoperative managementofcardiacsurgeriesareopioidanalgesicsand supportivemeasures.3
Currently,manyinstitutionsuseintravenousopioidswith highclearanceandrelativelyshorthalf-lives,suchas mor-phine,thatproduceimportantfluctuationsinserumopioid levels,rangingfrominadequateanalgesiatotoxicvalues.4 The option,in thiscase, wouldbeintravenous infusionof
analgesics,eitheron-demand or continuousinfusion. Both methods,however, requirehigh-costapparatus.3Thus, an optionalmethodthatpromotescontinuousanalgesia with-outtheproblemsassociatedwithinfusiontechniqueswould betheuseofanagentwithlonghalf-lifeandlowclearance appliedintraoperatively,suchasmethadone.Methadoneis a synthetic opioid of long duration and latency, used for severalyearsinthetreatmentofdrugaddiction5and redis-coveredasan analgesic fortreating chronic pain,6 cancer pain,7andalsoforpostoperativeanalgesia,bothinadults8 andchildren.9,10
R(−)andS(+)isomersofmethadoneinpromoting antinoci-ceptiveeffect.13
Theaimofthisstudywastocomparetherepercussions onpostoperativeanalgesiaandtheoccurrenceofitsadverse effects (nausea, vomiting, and respiratory depression) in thefirst36postoperativehoursofmyocardial revasculariza-tionsurgeriesprovidedbyadoseofmethadoneormorphine administeredattheendofsurgery.
Methods
This study was approved by the Research Ethics Commit-teeoftheUniversidadedoSuldeSantaCatarina,through registrationNo.1.049.850,onMay5,2015.Itwasalso reg-istered in the Registro Brasileiro de Ensaios Clínicos No. RBR-8spkx9.
Arandomized, double-blind,phaseIVparalleltrial was conducted. Patients of both sexes, older than 18 years, withphysical statusclassificationbytheAmericanSociety ofAnesthesiologists---ASAIIIorIV,whounderwentcoronary arterybypassgraftingwithoutcardiopulmonarybypasswere selected.Participantsgavewritteninformedconsentduring thepreanestheticvisit.
For sample size calculation, we consider the percent-ageofnon-exposedpositives;thatis,satisfactoryanalgesia in50%of thepatientsreceivingmorphine(Control Group) and80%amongtheexposedpositives;(InterventionGroup) witha95% confidence level andstudy power of 80%,and weobtainedaminimumsamplenecessaryforthestudyof 80patients(40ineachgroup).Patientstakenillicitdrugs, thosewithahistoryofallergiestoanyof themedications usedinthestudy,andthosewhohadtoremainintubated postoperativelyformorethan12hwereexcluded.
Patient randomizationwasperformed by blockswitha sequenceoffourparticipants.Patientswereallocated ran-domly by blocks into two groups: MeG (methadone) and MoG(morphine). The blockswere drawn by the research teamandpassedontotheheadofanesthesiologyto deter-mine the drug used. Both the investigators and research assistants,responsiblefordatacollection,andthepatients wereblind tothe allocated groups, ensuring study blind-ness.In the operating room,all patients were monitored with invasive blood pressure, cardioscopy, pulse oxime-try,capnography,temperature,diuresis,andcentralvenous pressure.Inductionofanesthesiawasperformedwith sufen-tanil(0.5g.kg−1)anda10gbolusasneeded,etomidate (0.2mg.kg−1),androcuronium(0.1mg.kg−1).
Anesthesia was maintained with sufentanil (0.25---0.5g.kg−1.h−1); sevoflurane (0.5---1 MAC). At the end of anesthesia, MeG received methadone(0.1mg.kg−1 correctedweight)or MoG receivedmorphine(0.1mg.kg−1 correctedweight).
The anesthetic dosage calculation for induction and maintenance of anesthesia had as reference the ideal weight (IW) for rocuronium and corrected weight (CW) for etomidate in which IW=height−100cm for men and height−105cm for women and CW=IW+[0.4×(real weight)−IW]. At the end of procedure the patient was immediatelytakentotheICU, intubated,where the post-operativefollow-up wasperformed. TheICU professionals wereblindtowhichofthegroupsthepatientswereassigned
to and according to the ICU medical and nursing team criteriareceivedintravenous dipyrone(1g)every 6h con-tinuously (IV). And ifthere wasa complaint of moderate or severe pain, intravenous morphine (0.03mg.kg−1) was given,withalimitof0.1mg.kg−1in4h.Incaseofnausea or vomiting,metoclopramide hydrochloride(10mgIV)was given.
Durationofanesthesiainminutes,numberofdoses,and typeofanalgesicandantiemeticsrequiredduringthe post-operativeperiodwererecorded,aswellastheoccurrence of possible adverse reactions, such as nausea, vomiting, andrespiratorydepression.Thesereactionswereobserved bythenursesand/or researchteamduring ICUadmission. Respiratory depression was considered when there were eightrespiratorymovementsorlessperminuteand/orneed forreintubation.Theresearchteamwiththehelpoftrained anesthesiology nursesandresidentsappliedthenumerical scale of pain at 12, 24, and 36h post-operatively. Time tofirstanalgesic administrationandextubationtimewere also recorded, in agreement with the ICU’s on-call staff medicalrecords.Allmeasurementsweremade byblinded researchers.
Thenumericalpainscale rangesfrom0to10,inwhich 0=nopainand 10=the worst painpossible.14 Inaddition, categorically 0---3 is considered mild pain, 4---7 moderate pain,and8---10severepain.15
Forsamplesizecalculation, theOpenEpiprogram, ver-sion 2.3.1,wasused. Datacollectedwere registered in a database created using the public domain software Epi-data,version3.1(EpiDataAssociation,Odense,Denmark). Statistical analysis was performed using Statistical Prod-uct for Service Solutions software (SPSS for Windows v20 Chicago, IL, USA). Descriptive epidemiology was used to present the data;qualitative variables werepresented as proportionsandquantitativevariablesasmeasuresof cen-tral tendency and dispersion. Foranalysis of quantitative variables,Kolmogorov---Smirnovtest wasusedfornormally distributed data. Student’s t-test was used to compare means, using parametric statistic. In cases of non-normal distribution, non-parametric statistics were used apply-ingWilcoxon---Mann---Whitney Utest. Inordertoverifythe associationbetweenthevariablesofinterest,Pearson chi-squaretestwasusedforcategoricalvariables.
As a measure of effect, the relative risk reduction or efficacyofmethadonecomparedtothecontrolgroupwas calculated.Forthis,satisfactoryanalgesiawasconsidered when the patientpresented results below 3 in the three pain scale measurements. In addition,number needed to treat (NNT) andnumber needed toharm(NNH) regarding the use of methadonewere calculated,considering satis-factoryanalgesiaandoccurrenceofadversedrugreactions. Dataanalysiswasperformedonanintentiontotreat.The levelofsignificancewas95%.
Results
Patients undergoing cardiac surgery (n = 145)
Patients not eligible due to non-myocardial revascularization
n = 32
112 eligible patients
Patients excluded for needing cardiopulmonary bypass during
surgical procedure n = 8
Sample submitted to randomization n = 104
Morphine group n = 50
Morphine group n = 52 Methadone group n = 52
Exclusion 1 death 1
intubation > 12h Exclusion 1 reintubation 1 intubation > 12h
Morphine group n = 50
Figure1 Flowchartofselectionofstudyparticipants.
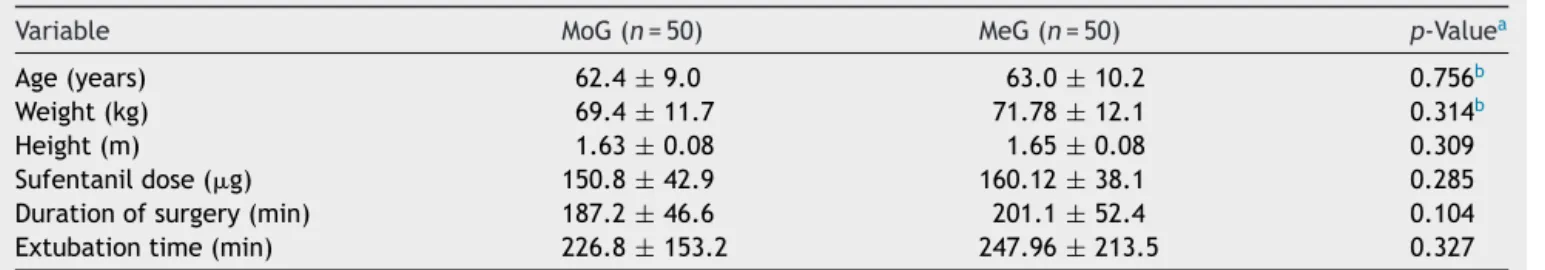
Table1showstheclinicalandproceduralcharacteristics andcomparisonof groups:morphine(MoG,control group) andmethadone(MeG,interventiongroup).
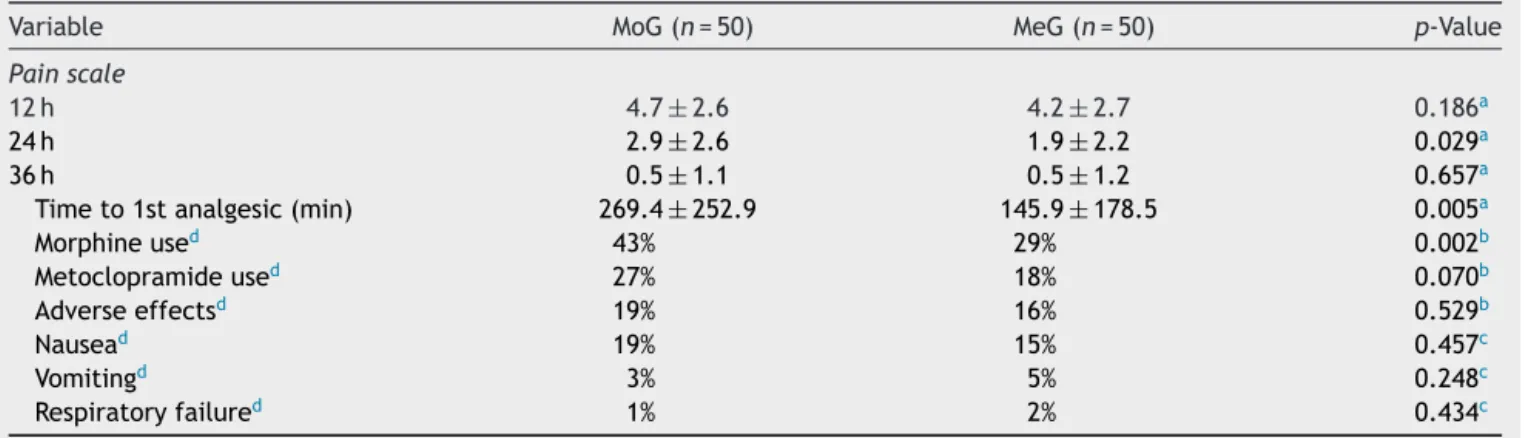
Table2showsthepostoperativedistributionofvariables. Ifweconsiderthenumericalscaleofpaininwhich0=nopain and10=theworstpainpossible,therangewasbetween0 and10in36h.
Of the interviewees, 3% were sedated and could not respondtothe painscale.Inthis case,prolonged extuba-tiontimewasconsideredanadverseeffect.Table3shows thedistributionof groupsregarding efficacyandsafetyof analgesicsused.Fordefinitionof efficacy,analgesiaequal toorlessthanthree(consideredasmildpain)wasusedas thecut-off point onthenumerical painscale throughthe follow-uptime(36h).
Taken Table 3 data into consideration, the methadone efficacyasapostoperativeanalgesiceffect,calculatedby
relative risk reduction, was 22%. The NNT for a favor-able event of satisfactory analgesia in the first 36h was sixpatients and the NNH,that is, an adverse reaction to methadone,wasequalto16patients.
Discussion
Methadone group had greater analgesia within 24h after surgical procedure and required less use of morphine in theperiod.However,thetimeelapsedbetweentheendof surgeryanduseofanalgesicduringICUstaywaslowerthan thatofcontrolgroup.Ifweconsidersatisfactoryanalgesia equaltoorlessthanthreewitha36-hpainscaleand con-sidermildpainas‘nopain’,themethadoneefficacywas22% higherthanmorphine.
Opioidsaretraditionallyusedforpaincontrolfromthe first to the third day after cardiac surgery; it should be notedthattheintermittentadministrationof short-acting opioids,suchasmorphine,resultsinfluctuationsinplasma concentrations,whichmayexplaintherelatively elevated painlevelsinthis patientpopulation.This study revealed theinterest of usingintraoperative methadonein cardiac surgeries,since the number of opioid dosesrequired was significantlylowerinmethadonegroupattheendof anes-thesia.
Theuseofmethadoneattheendofanesthesiaallowed formoreeffectiveanalgesia,sothatduringthefirst36 post-operativehoursthenumberofpatientsrequiringanalgesia waslowerwithmethadone.Inaddition,patientsatisfaction withthequalityofanalgesiainthisgroupresultedinapain scorealsolowerthanthatofmorphinegroupand,evenso, thetimerequiredforextubationwasnotprolonged.
The results of the present study are similar to those reportedbyMurphyetal.16thatconcludedthatmethadone (0.3mg.kg−1) used in induction of anesthesia for cardiac surgery resulted in a significant reduction of postopera-tiveanalgesicrequirement;betterpainscores,betterpain perception by the patient, and improved pain manage-mentfor 72haftertrachealextubation,inadditiontothe non-observation of adverse events related to methadone administration.
However, Gottschalk et al.17 reported less opioid use postoperativelyonly after 48h of methadone administra-tion.Thelowerneedforopioidsinthepostoperativeperiod bythosewhoreceivedmethadonemayjustifythelower inci-denceofnauseaandvomitinginthisgroup,whichisquite
Table1 Patientdemographicsandanesthesia/surgerydata.
Variable MoG(n=50) MeG(n=50) p-Valuea
Age(years) 62.4±9.0 63.0±10.2 0.756b
Weight(kg) 69.4±11.7 71.78±12.1 0.314b
Height(m) 1.63±0.08 1.65±0.08 0.309
Sufentanildose(g) 150.8±42.9 160.12±38.1 0.285
Durationofsurgery(min) 187.2±46.6 201.1±52.4 0.104
Extubationtime(min) 226.8±153.2 247.96±213.5 0.327
Datapresentedasmeanandstandarddeviation.
MeG,methadonegroup;MoG,morphinegroup;kg,kilograms;m,meters;g,micrograms;min,minutes.
a Wilcoxon-Mann---WhitneyUtest.
Table2 Postoperativeanalgesia,useofanalgesics,andadverseevents.
Variable MoG(n=50) MeG(n=50) p-Value
Painscale
12h 4.7±2.6 4.2±2.7 0.186a
24h 2.9±2.6 1.9±2.2 0.029a
36h 0.5±1.1 0.5±1.2 0.657a
Timeto1stanalgesic(min) 269.4±252.9 145.9±178.5 0.005a
Morphineused 43% 29% 0.002b
Metoclopramideused 27% 18% 0.070b
Adverseeffectsd 19% 16% 0.529b
Nausead 19% 15% 0.457c
Vomitingd 3% 5% 0.248c
Respiratoryfailured 1% 2% 0.434c
%,percentage;MeG,methadonegroup;MoG,morphinegroup;h,hours;min,minutes.
aWilcoxon---Mann---WhitneyUtest.
b Pearson’schi-squaretest.
c Fisherexacttest.
d Relativetopercentageofpatients.
Table3 Satisfactoryanalgesiaandoccurrenceofadverse
eventsinthefirst36postoperativehours.
MoG(n=50) MeG(n=50) p-Valuea
Painanalgesia≤3 0.096 Failure 36(72%) 28(56%)
Success 14(28%) 22(44%)
Adversereaction 0.529 Yes 19(38%) 16(32%)
No 31(62%) 34(68%)
%,percentage;MoG,morphinegroup;MeG,methadonegroup.
aPearson’schi-squaretest.
interestingininterventionswithgreaterpainpotential,such assternotomy.
Another fact observed was the time to first analgesic administration that was significantly lower in methadone group.ThisdivergesfromtheresultsofUdelsmannetal.18 whose methadone use in the induction of anesthesia for cardiacsurgeryallowedmoreprolongedanalgesia,sothat thefirstdoseofanalgesicinpatientsreceivingmethadone wasonlygivenalmost4hafterthatofthemorphinegroup. In another double-blind study comparing methadone and morphine for upper abdominal surgeries, the mean time required for rescue analgesia was significantly longer in patients receiving methadone (21 vs. 6h).14 One possi-ble explanation may have been the dose chosen, which interferes with the drug clearance time, and duration of methadoneeffect,whichisinfluencedbythepatient’s indi-vidualcharacteristics.Inthiscase,themethadonedosewith concentrationshigherthan20mgisrecommended,always consideringpatient’sage,surgical procedure,and respira-toryrate.19,20
Intravenousmorphineshowsapeakofanalgesiceffectat 20minafteritsadministrationandthedurationofanalgesic actionis4---5h.21 Itisalsoworthnotingthat,evenifthere isnostatisticaldifferencebetweengroups,onaverage,the
durationofsurgeryinmethadonegroupwashigherthanin morphinegroup.
Becauseofitsprolongedaction,methadonehasbecome an interesting analgesic option in postoperative pain management, particularly in major surgeries with pro-longedrecovery time,suchascardiacsurgeries.However, methadonelikeother opioidshasamongthepossible side effects nausea, vomiting, pruritus, and dose-dependent respiratory depression, which may delay extubation time and increase institutional costs. Although already used in othercountries,itisonlyrecentlyavailableforparenteral useinBrazilianinstitutions.
Methadone efficacy was 22% higher than that of mor-phine. The NNT result of six (considered a high-impact treatment of less than 25) and NND of 16 reveal that methadoneisagood,effective,andsafetherapeuticoption forpostoperativeanalgesiawhenadministeredattheendof surgery.Itshouldbeemphasizedthatthecontrolgroupin thisstudy is morphine(whichwasconsidered the conven-tionaltreatment);therefore,thesearesatisfactoryindexes thataidinclinicaldecision,astheypresenttherisk-benefit ofbothdrugs.
Amongthelimitationsofthisstudy,itshouldbe empha-sized that pain is extremely subjective and difficult to measure, despite the option of using ascale already val-idated for its measurement, but that may influence the resultsofthisstudy.Thevariationsinpainseverityin24h, despitepresentingastatisticallysignificantdifference,are clinicallysimilarandfullysatisfactoryforpostoperativepain in this type of procedure. No standardized measure was used for assessing sleepiness,which may have influenced theperceptionofpain.Therefore,multicenterstudieswith afollow-upperiodofmorethan36harerequiredtoprove thisdata.
Conclusion
Basedondatafound,methadonewaseffectivefor analge-sia in patientsundergoing coronaryarterybypassgrafting withoutcardiopulmonarybypass.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Maxwell C, Nicoara A. New developments in the treatment of acute pain after thoracic surgery. Curr Opin Anesth. 2014;27:6---11.
2.CoganJ.Painmanagementaftercardiacsurgery.Semin Cardio-thoracVascAnesth.2010;14:201---4.
3.AmericanSocietyofAnesthesiologistsTaskForceonAcutePain Management.Practiceguidelinesforacutepainmanagementin theperioperativesetting:anupdatedreportbytheAmerican SocietyofAnesthesiologistsTaskForceonAcutePain Manage-ment.Anesthesiology.2012;116:248---73.
4.UdelsmannA,MacielFG,ServianDCM.Methadoneandmorphine intheinductionofanesthesiaincardiacsurgery.Impacton post-operativeanalgesiaandprevalenceofnauseaandvomiting.Rev BrasAnestesiol.2011;61:695---701.
5.NielsenS,LaranceB,DegenhardtL,etal.Opioidagonist treat-mentfor pharmaceuticalopioiddependentpeople.Cochrane DatabaseSystRev.2016;9:CD011117.
6.DowellD,HaegerichTM,ChouR.CDCguidelinefor prescrib-ing opioids for chronic pain --- United States, 2016. JAMA. 2016;315:1624---45.
7.MercadanteS,FerreraP,VillariP,et al.Switchingfrom oxy-codone to methadone in advancedcancer patients. Support CareCancer.2012;20:191---4.
8.NetoJO,MachadoMD,deAlmeidaCorreaM,etal.Methadone patient-controlled analgesia for postoperative pain: a ran-domized,controlled, double-blind study. J Anesth.2014;28: 505---10.
9.ZernikowB,MichelE,CraigF,etal.Pediatricpalliativecare: use ofopioids for the managementof pain. PaediatrDrugs. 2009;11:129---51.
10.SimoniRF, CangianiLM,PereiraAMSA,etal. Effectivenessof theuseofmethadoneandclonidineforintraoperativecontrol ofimmediatepostoperativepainafterremifentanil.RevBras Anestesiol.2009;59:421---30.
11.KraycheteDC,SiqueiraJTT,GarciaJBS.Recomendac¸õespara usodeopioidesnoBrasil:parteI.RevDor.2013;14:295---300.
12.SimoniRF,CangianiLM,PereiraAMSA,etal.Eficáciadoemprego dametadonaoudaclonidinanointraoperatórioparacontrole dadorpós-operatóriaimediataapósusoderemifentanil.Rev BrasAnestesiol.2009;59:421---30.
13.Inturrisi CE. Pharmacology of methadone and its isomers. MinervaAnestesiol.2005;71:435---7.
14.Calil AM, Pimenta CAM. Intensidade da dore adequac¸ão de analgesia.RevLatinoAmEnfermagem.2005;13:692---9.
15.Murphy GS, Szoko JW, Greenberg SB, et al. Intraoperative methadoneforthepreventionofpostoperativepaina random-ized,double-blindedclinicaltrialincardiacsurgicalpatients. Anesthesiology.2015;122:1112---22.
16.Gottschalk A, Durieux ME, Nemergut EC. Intraopera-tive methadone improves postoperative pain control in patients undergoing complex spinal surgery. Anesth Analg. 2011;112:218---23.
17.UdelsmannA,MacielFG,ServianDCM,etal.Metadonaemorfina nainduc¸ãodaanestesiaemcirurgiacardíaca.Repercussãona analgesiapós-pperatóriaeprevalênciadenáuseasevômitos. RevBrasAnestesiol.2011;61:695---701.
18.GourlayGK,WillisRJ,LambertyJ.Adouble-blindcomparisonof theefficacyofmethadoneandmorphineinpostoperativepain control.Anesthesiology.1986;64:322---7.
19.ShaiovaL,BergerA,BlindermanCD,etal.Consensusguideline onparenteralmethadoneuseinpainandpalliativecare.Palliat SupportCare.2008;6:165---76.
20.Kharasch ED. Intraoperative methadone: rediscovery, reap-praisal,andreinvigoration?AnesthAnalg.2011;112:13---6.