Left ventricular mass behaviour in hemodialysis patients
during 17 years
Authors
Loren Giagio Cavalcante 1 Ricardo de Souza Cavalcante 1 Ana Claudia Kochi 1 Katashi Okoshi 1 Silméia Garcia Zanati Basan 1
João Carlos Hueb 1 Rosana dos Santos e Silva Martin 1
Rogério Carvalho de Oliveira 1
Vanessa Burgungi Banin 1 Pasqual Barretti 1 Roberto Jorge da Silva Franco 1
Luis Cuadrado Martin 1
1 Universidade Estadual Paulista.
Submitted on: 12/01/2014. Approved on: 03/05/2015.
Correspondence to: Luis Cuadrado Martin. Faculdade de Medicina de Botucatu - Universidade Estadual Paulista.
Rua Rubião Jr, s/n, Botucatu, São Paulo, SP, Brasil.
CEP: 18618-970.
E-mail: cuadrado@fmb.unesp.br
I
NTRODUCTIONThe prevalence of chronic kidney disease (CKD) is increasing globally.1 The survival of patients with CKD and individuals in need of dialysis in particular is significantly shorter than that of their healthy peers within the same age range.2 Cardiovascular disease, the main cause of death in this group of patients,3,4 is directly associated with left ventricular hypertrophy (LVH), a condition found in 75% of the individuals on dialysis.5,6 The presence of LVH is a marker for fatal cardiovascular events.7-11
Sixty to eighty percent of the individuals on dialysis are diagnosed with high blood pressure (HBP),12 the
leading cause of LVH in patients on dialysis. In addition to its role in the main cause of CKD in Brazil,2 HBP may
affect the prevalence of cardiovascular death of patients with end-stage renal disease, often associated with inadequate blood pressure (BP) control13,14 and
hemodynamic changes secondary to sodium and fluid level increases occurred between dialysis sessions.6
The most characteristic morpho-logic changes seen in the hearts of dialysis patients are the enlargement of the heart cavity and the progressive thickening of the left ventricle walls,
DOI: 10.5935/0101-2800.20150054
Introduction: Ventricular hypertrophy is frequent in dialysis patients and is associated with an ominous prognosis. It is not knowledge if this ventricular change is growing or decreasing in hemodialysis patients. Objective: To assess left ventricular hypertrophy behaviour during 17 years in patients of a university dialysis center, as well as to verify the possible causes of this behavior. Methods: There was performed a retrospective longitudinal study that evaluated the echocardiographic left ventricular mass in hemodialysis patients in our dialysis facility over 17 years. Examinations of 250 patients aged 18 years or more who underwent routine echocardiography were included. Results: There was a progressive reduction of ventricular mass over studied period. This reduction was associated with blood pressure reduction. In multivariate analysis, ventricular mass was associated with blood pressure and hemoglobin. Conclusion: Left ventricular hypertrophy underwent significant reduction over 17 years in our hemodialysis patients. The factors associated with this reduction that could be identified in the current study were the progressive reduction of blood pressure and hemoglobin increase.
A
BSTRACTwhich becomes less reversible the longer the patient stays on dialysis.15 LVH is basically an
adaptive remodeling process aimed at minimi-zing the stresses applied to the ventricular wall.16
This initially adaptive process, however, may de-velop into hypertrophy, congestive heart failure, and high rates of morbidity and mortality.
The possibility of reversing LVH in patients on dialysis has been discussed in the literature. Some authors have described such reversals and associated them to reduced cardiovascular risk.17,18 Therefore,
LVH reversal may be considered as an intermediate outcome and a therapeutic goal for patients on dialysis. For that reason, echocardiography has been offered to the patients seen in our center since 1993.
The primary objective of this study was to assess 17 years of data on the progress of left ventricular hypertrophy in the patients seen at a teaching dialysis center. The secondary objective was to look into the possible causes for the patterns observed.
M
ATERIALS AND METHODSThis longitudinal retrospective study looked into cases of LVH affecting patients on hemodialysis treated at a teaching dialysis center. The study included 250 routine echocardiograms of patients with end-stage renal disease aged 18 years or older.
The echocardiograms were made between dialysis sessions (on Mondays, Wednesdays, and Fridays for patients on dialysis on Tuesdays, Thursdays, and Saturdays, and on Tuesdays and Thursdays for the other patients). The patients were clinically and biochemically stable in their hemodialysis programs and had normal sinus rhythms on their electrocardiograms. Individuals with malignant hypertension, patients presenting exceedingly challenging conditions to have their echocardiograms made, and patients with hemodynamically significant valvular heart disease were excluded. This study complied with the requirements set out in Resolution 169/96 issued by the National Board of Health and was approved by the Research Ethics Committee of the School of Medicine of Botucatu.
Echocardiograms from four different years spanning over a total of 17 years were assessed and compared to each other: 23 echocardiograms from 1993, 50 from 2000, 77 from 2006, and 100 from 2010. Data were collected from patient charts. Ten BP measurements made before the start of the hemodialysis sessions prior to the echocardiographic tests were recorded, along with patient weight and height from which the body mass index (BMI) and the mean interdialytic weight gain (IWG) were calculated.
The use of antihypertensive drugs, the number of classes of antihypertensive medica-tions, and the classes of such drugs - angio-tensin-converting-enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), beta blockers (β-blockers), calcium channel block-ers (CCB), sympatholytic drugs, and vasodi-lators - were recorded. The data concerning the type of antihypertensive medication pre-scribed to the patients seen in 1993 was not available.
The patient charts contained the test results for hemoglobin, calcium, phosphorus, and parathyroid hormone (PTH) levels measured in time periods coinciding with the times at which the echocardiograms were made. Data on PTH levels were not available for the patients seen in 1993.
Trained echocardiographers ran the tests. Echocardiograms were made with the patients in lateral decubitus with the left arm slightly flexed over the head. Images were captured in accordance with the recommendations of the American Society of Echocardiography and recorded on a VCR for further reference. The coefficient of variation between two blinded observers in our laboratory was 2%. The left ventricle (LV) was measured in three to five cycles. Systolic and diastolic function indices were obtained. Echocardiographic tests were performed in accordance with the standard technique19,20 and the following data were
were used to calculate the left ventricular mass (LVM), which was then indexed to height raised to an exponential power of 2.7 to yield the left ventricular mass index (LVMI).
The data were analyzed on software package Sigma Stat 2.03. Analysis of variance for parametric or non-parametric distributions was used when applicable to compare between continuous variables. Categorical variables were compared through the chi-square test, whereas correlations were assessed using multiple linear regression. The significance level was set at five percent (p = 0.05). Data following a parametric distribution were expressed in terms of mean values ± standard deviation; data following a non-parametric distribution were presented in terms of median values (interquartile range).
R
ESULTSTable 1 shows the data on patient age, weight, height, BMI, systolic and diastolic BP, LVM, LVMI, use of hypertensive drugs categorized as ACE inhibitors, ARBs, β-blockers, CCB, vasodilators, or sympatholytic drugs, and the number of drug classes prescribed per patient. Table 1 also contains the number of patients on dialysis at each time period and the absolute and relative number of patients with echocardiograms.
Patient mean age increased significantly (p < 0.001) over the first three time periods (1993, 2000, 2006), but no statistical difference was observed between 2006 and 2010.
Patient mean height did not change significantly over the years (p = 0.938). In general terms, patient weight and BMI increased over time (p < 0.001). In 2010, patient mean weight was statistically different from that of previous years. In 1993 and 2000, the mean BMI was lower than in 2010. In 2006 the mean BMI reached an intermediate level, and was not sta-tistically different from the mean BMI observed in the other time periods.
Systolic BP changed significantly over the years (p < 0.001), reaching similar values in 2000, 2006, and 2010, and lower levels in 1993. Systolic BP also changed over the years (p < 0.001): it was lower in 2010 than in previous years; it did not change between 2000 and 2006, but it was lower than the systolic BP
seen in 1993. Therefore, BP generally decreased over the years. Urine output and the number of patients with anuria did not change significantly. Mean IWG decreased significantly.
The echocardiograms showed decreases in LVM and LVMI, which became statistically significant in the most recent time period analyzed (p < 0.001). LVM and LVMI were statistically lower in 2010 when compared to previous years, but the difference between the values found in the years prior to 2010 was not significant.
The use of ACE inhibitors (p = 0.015), ARBs, and
β-blockers (p < 0.001) increased over the years. ARBs were prescribed to dialysis patients only in 2010 (11% in 2010 vs. 0% in 2006 and 2000) [p < 0.001]. In 2010, 41% of the patients were on β-blockers, versus 20% in 2006 and 2% in 2000. The use of sympatholytic drugs (p < 0.001) and vasodilators (p = 0.038) to manage HBP decreased gradually with time. In 2010, sympatholytic drugs were administered to only 12% of the patients, versus 39% in 2006 and 36% in 2000 (p < 0.001). The number of classes of antihypertensive drugs prescribed to dialysis patients increased in 2010 when compared to 2000 (p = 0.021), but not in relation to 2006.
Table 2 shows hemoglobin, calcium, phosphorus,
and PTH serum levels. In 2010, hemoglobin levels were higher than in 1993 (p < 0.001). No significant difference was seen in the calcium and phosphorus levels over the years (p > 0.05). PTH levels increased gradually in 2000, 2006, and 2010 (p < 0.001).
Table 3 shows a multiple regression looking into the factors associated with LVH. Pre-dialysis systolic BP (p < 0.001) was independently associated with LVMI.
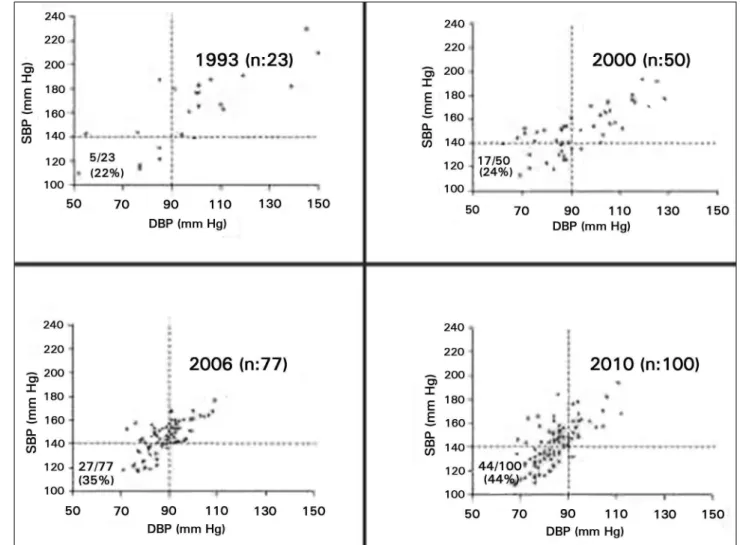
Figure 1 shows the correlation between diastolic and systolic BP in the studied time periods. In 1993, only 22% of the patients had BP below 140/90 mm Hg. In 2000, the number grew to 34% and was kept at a similar level in 2006, at 35%. In 2010, another increase was observed in the number of patients with properly managed BP, taking it to 44%.
TABLE 1 SECULARTRENDSOFTHEPARAMETERSRELATEDTOHIGHBLOODPRESSUREMANAGEMENTINPATIENTSON HEMODIALYSIS
Year 1993 2000 2006 2010
p
Patients on HD (n) 32 69 115 115
Assessed patients (%) 23 (72%) 50 (72%) 77 (67%) 100 (87%)
Age (years) 36 ± 15a 47 ± 14b 54 ± 14c 59 ± 14c < 0.001
Height (cm) 162 ± 10.3 161 ± 8.7 161 ± 9.1 162 ± 9.4 0.938 Weight (Kg) 58 ± 11.7a 58 ± 10.6a 62 ± 13.0a 67 ± 14.4b < 0.001
BMI (m/Kg2) 22 (19-24)a 22 (20-24)a 23 (21-25)ab 24 (22-29)b < 0.001
SBP (mm Hg) 163 (156-172)a 150 (135-163)b 146 (137-154)b 142 (128-153)b < 0.001
DBP (mm Hg) 105 (100-109)a 88 (83-105)b 89 (82-93)b 80 (74-90)c < 0.001
Anuria (n) - 28/50 37/77 45/100 0.424 Urine output (mL) - 60 (0-440) 190 (0-915) 200(0-800) 0.313 Mean IWG (L) - 2.9 ± 0.80a 2.7 ± 1.29ab 2.4 ± 0.90b 0.006
LVM g 303 (243-411)a 272 (234-391)a 262 (227-318)a 234 (193-266)b < 0.001
LVMI g/m2,7 85 (67-102)a 80 (66-102)a 74 (63-86)a 63 (52-76)b < 0.001
Antihypertensive drugs
ACE inhibitors (%) - 22 44 45 0.015
ARBs (%) - 0 0 11 < 0.001
ACEi/ARB (%) - 22 44 55 < 0.001
β-blockers (%) - 2 20 41 < 0.001
CCB (%) - 26 29 38 0.236
Sympatholytic drugs (%) - 36 39 12 < 0.001
Vasodilators (%) - 10 6 1 0.038
Number of classes - 1 (0-2)a 1 (0-2)ab 2 (1-2)b 0.021
BMI: body mass index; SBP: systolic blood pressure; DBP: diastolic blood pressure; IWG: interdialytic weight gain; LVM: left ventricular mass; LVMI: left ventricular mass index; ACEi: angiotensin-converting-enzyme inhibitors; ARB: angiotensin II receptor blockers; β-blockers: beta blockers; CCB: calcium channel blockers; abc equal letters indicate statistical similarity; data expressed as mean ± standard deviation; median (interquartile range) or percent rate (%).
TABLE 2 SECULARTRENDSOFHEMATOLOGICANDBIOCHEMICALPARAMETERSOFPATIENTSONHEMODIALYSIS
Year 1993 2000 2006 2010 p
Patients (n) 32 69 115 115
-Assessed patients (%) 23 (72%) 50 (72%) 77 (67%) 100 (87%) -Hemoglobin (g/dL) 7.3 (6.7-8.2)a 10.1 (9.2-11.3)b 10.7 (9.5-11.8)b 11.6 (10.6-12.7)c < 0.001
Calcium (mg/dL) 9.0 (8.6-9.6) 9.0 (8.5-9.4) 9.1 (8.3-9.7) 8.9 (8.6-9.4) 0.863 Phosphorus (mg/dL) 5.5 (4.6-6.3) 5.2 (3.9-6.7) 5.6 (4.2-7.8) 5.2 (4.3-6.2) 0.507 Parathyroid hormone (pg/dL) - 84 (49-245)a 201 (99-494)b 477 (250-810)c < 0.001
Residual renal urea clearance (mL/min) - 0.28 (0-1.1) 0.33 (0-1.9) 0.42 (0-2.0) 0.337
a,b,c equal letters indicate statistical similarity; data expressed as median (interquartile range).
D
ISCUSSIONLVH is a common finding and a marker of poor prognosis in patients with CKD. Reversing LVH may be one of the goals of the treatment offered to patients with CKD. In recent years, our service saw an increase in the intensity with which the BP of patients on dialysis is managed and in the use of drugs acting on the renin angiotensin aldosterone system (RAAS).
The impact of these measures upon patient cardiac hypertrophy is unknown. Thus, this study aimed to analyze the secular trends of the LVMI of dialysis patients seen at our center.
TABLE 3 PREDICTORSFORLEFTVENTRICULARMASS INDEXINPATIENTSWITHCHRONICKIDNEY DISEASESEENIN 1993, 2000, 2006, AND 2010
Beta p
Age (years) -0.053 0.500 BMI (Kg/m2) 0.084 0.273
SBP (mm Hg) 0.271 < 0.001 Using ACEi or ARBs 0.017 0.820 PTH (pg/mL) -0.067 0.380 Hemoglobin (g/dL) -0.105 0.181 Mean IWG (L) 0.083 0.271
BMI: body mass index; SBP: pre-dialysis systolic blood pressure; ACEi: angiotensin-converting-enzyme inhibitors; ARB: angiotensin II receptor blockers; PTH: parathyroid hormone; IWG: interdialytic weight gain.
the RAAS, and a decrease in the use of direct vasodilators over the years.
Experimental and clinical evidence suggest that reversing LVH is an attainable therapeutic goal for patients with CKD. In recent years, LVH reversal has become a hot topic and a desirable intermediate endpoint, particularly due to the possible improvements it may bring to hypertensive individuals and patients with CKD.17 Interest has revolved around the role
antihypertensive agents in protecting the vascular and myocardial structures.
The factors connected to the pathogenesis of LVH in patients with CKD relate to preload and afterload alterations. In preload, the related factors include intravascular volume expansion (salt and fluid) and anemia. In this study, a negative correlation was observed between hemoglobin levels and LVMI. Similar results have been reported for individuals with CKD off dialysis.21 However, multiple linear
regression revealed that hemoglobin level was not an independent predictor for decreased
LVH.
Afterload is determined by aortic impedance, which is basically constituted by two elements: artery compliance and peripheral vascular resistance, the latter a determinant of blood pressure. Previous studies found a strong correlation between elevated systemic BP and development of LVH in pre-dialysis CKD patients.21,22 In this study, decreases in
systolic and diastolic BP were found over the years. Consequently, significant decreases were observed in afterload and LVM. Interestingly, a direct correlation was verified between decreases in systemic BP and LMVI.
Vasodilators are a class of antihypertensive drugs that decrease blood pressure mostly without interfering with ventricular hypertrophy, although Minoxidil may increase it. The prescription of these drugs in the patients included in the study gradually decreased over the years, at the same rate as the prescription of drugs that affect disease mechanisms common to elevated BP and myocardial growth increased.
Another significant finding concerned the use of ARBs in recent years. Antihypertensive drugs do not reverse LVH by merely decreasing patient BP.23 Peripheral vascular resistance,
an indicator of afterload, is decreased when the renin angiotensin aldosterone system is inhibited, thus significantly affecting LVM. RAAS inhibition also affects the myocardium directly and independently from the impact it has in decreasing BP. However, multiple linear regression analysis revealed that ACE inhibitors and ARBs were not associated with LVMI independently from BP, thus indicating that the impact these drugs had on heart remodeling was chiefly mediated by their antihypertensive effects.
Improved pre-dialysis care may have affected the magnitude of LVH observed in this study. Patients submitted to care by a nephrologist prior to starting dialysis are known to have the alterations associated with kidney disease (hypertension, anemia, and mineral and bone disorders) treated more effectively and to, consequently, present less LVH.24
Figure 1. Scatter diagrams for diastolic blood pressure (DBP) and systolic blood pressure (SBP) of hemodialysis patients at different times between 1993 and 2010.
Figure 2. Left ventricular mass indexed to height raised to the power of2,7versus systolic blood pressure (SBP) of hemodialysis patients at different times between 1993 and 2010.
echocardiograms should be made regularly for patients on dialysis. However, despite the goodwill of both services, once there are fewer echocardiographers in Cardiology than
orders for echocardiograms, tests were run only when possible.
Pre and post dialysis volume variations were significant and had a decisive impact on the results.25 The tests presented herein do
not reflect the pre or immediate post-dialysis reality. Echocardiograms were made on days in which the patients were not on dialysis. There might be minor volume variations from the first to the second or third day between dialysis sessions, but these variations were certainly much smaller than the ones seen between the pre and post-dialysis periods.
IWG, independently associated with BP by other authors,25 decreased gradually, as shown in
This study had some limitations. First, there was no information on the drugs prescribed in the first time period. The echocardiograms included in the study were produced in different echocardiography systems over the years, but the medical staff responsible for analyzing and interpreting the tests was never changed. The decrease in LVM could have been explained from the standpoint of survival, i.e., the patients who survived over the years were the ones with lower LVM. However, after excluding repeat patients, the decrease in LVM was still statistically significant (p = 0.001; data not presented), thus excluding the occurrence of survival bias. Some of the data from 1993 were incomplete. Other factors not included in our analysis - new technologies and improved diet therapy - may not have their roles in LVM improvement ruled out.
To sum up with, left ventricular hypertrophy decreased significantly within the last 17 years in our center. The factors associated with this decrease identified by the present study were the gradual decrease in blood pressure and the increase in hemoglobin levels. The effects from the more frequent use of medications acting on the renin angiotensin aldosterone system upon left ventricular hypertrophy reversal seems to have been mediated by the decrease in BP.
A
CKNOWLEDGEMENTThe authors would like to thank Professor Beatriz Bojikian Matsubara, Ph.D.; Adjunct Professor Jacqueline Teixeira Caramori, Ph.D.; João Henrique Castro, M.D.; and Bianca Balarin Albino, M.Sc., for their decisive support in data collection and invaluable input and criticism.
R
EFERENCES1. Wright J, Hutchison A. Cardiovascular disease in patients with chronic kidney disease. Vasc Health Risk Manag 2009;5:713-22. 2. Oliveira RB, Moura LRR. Censo de Diálise SNB 2011 [base
de dados na Internet]. São Paulo: Sociedade Brasileira de Ne-frologia. 2011 [Acesso em: 8 Março 2013]. Disponível em: http://www.sbn.org.br/pdf/censo2011.pdf
3. Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, et al.; American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Pre-vention. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascu-lar Disease, High Blood Pressure Research, Clinical Car-diology, and Epidemiology and Prevention. Circulation 2003;108:2154-69. DOI: http://dx.doi.org/10.1161/01. CIR.0000095676.90936.80
4. London GM. Cardiovascular disease in chronic renal failure: pathophysiologic aspects. Semin Dial 2003;16:85-94. DOI: http://dx.doi.org/10.1046/j.1525-139X.2003.16023.x 5. Martin Rdos S, Martin LC, Franco RJ, Barretti P, Caramori
JC, Castro JH, et al. Ventricular hypertrophy and cardiovas-cular mortality in hemodialysis patients with low educational level. Arq Bras Cardiol 2012;98:52-61. PMID: 22218412 6. Martin LC, Franco RJ. Renal disease as a cardiovascular risk
factor. Arq Bras Cardiol 2005;85:432-6. PMID: 16429206 7. Mailloux LU, Haley WE. Hypertension in the ESRD patient:
pathophysiology, therapy outcomes, and future directions. Am J Kidney Dis 1998;32:705-19. PMID: 9820438 DOI: http://dx.doi.org/10.1016/S0272-6386(98)70146-5
8. Lopez-Gomez JM, Verde E, Perez-Garcia R. Blood pressu-re, left ventricular hypertrophy and long-term prognosis in hemodialysis patients. Kidney Int Suppl 1998;54:S92-8. PMID: 9839291 DOI: http://dx.doi.org/10.1046/j.1523-1755.1998.06820.x
9. Amann K, Rychlik I, Miltenberger-Milteny G, Ritz E. Left ventricular hypertrophy in renal failure. Kidney Int Sup-pl 1998;54:S78-85. PMID: 9839289 DOI: http://dx.doi. org/10.1046/j.1523-1755.1998.06818.x
10. De Lima JJ, Lopes HF, Grupi CJ, Abensur H, Giorgi MC, Krieger EM, et al. Blood pressure influences the occurren-ce of complex ventricular arrhythmia in hemodialysis pa-tients. Hypertension 1995;26:1200-3. DOI: http://dx.doi. org/10.1161/01.HYP.26.6.1200
11. Parfrey PS, Foley RN. The clinical epidemiology of car-diac disease in chronic renal failure. J Am Soc Nephrol 1999;10:1606-15.
12. Rodrigues Júnior AG, Martin LC, Barretti P, Kochi AC, Bal-bi AL, Caramori JST, et al. Fisiopatologia da hipertensão arterial em diálise. J Bras Nefrol 2006;28:225-31.
13. Jones MA, Sharpstone P, Dallyn PE, Kingswood JC. Reduced nocturnal blood pressure fall is similar in continuous ambulatory peritoneal dialysis to that in hemodialysis and undialysed end--stage renal disease. Clin Nephrol 1994;42:273-5.
14. Cheig JS, Milite C, Sullivan JF, Rubin AL, Stenzel KH. Hypertension is not adequately controlled in hemodialy-sis patients. Am J Kidney Dis 1992;19:453-9. DOI: http:// dx.doi.org/10.1016/S0272-6386(12)80954-1
15. Martin LC, Franco RJ, Gavras I, Matsubara BB,
Gar-cia S, Caramori JT, et al. AssoGar-ciation between hypervole-mia and ventricular hypertrophy in hemodialysis patients. Am J Hypertens 2004;17:1163-9. DOI: http://dx.doi. org/10.1016/j.amjhyper.2004.07.017
16. Zoccali C, Benedetto FA, Mallamaci F, Tripepi G, Giacone G, Cataliotti A, et al. Prognostic impact of the indexation of left ventricular mass in patients undergoing dialysis. J Am Soc Ne-phrol 2001;12:2768-74.
17. London GM, Pannier B, Guerin AP, Blacher J, Marchais SJ, Darne B, et al. Alterations of left ventricular hypertrophy in and survival of patients receiving hemodialysis: follow-up of an inter-ventional study. J Am Soc Nephrol 2001;12:2759-67.
18. Zoccali C, Benedetto FA, Mallamaci F, Tripepi G, Giacone G, Stancanelli B, et al. Left ventricular mass monitoring in the follow-up of dialysis patients: prognostic value of left ventri-cular hypertrophy progression. Kidney Int 2004;65:1492-8. DOI: http://dx.doi.org/10.1111/j.1523-1755.2004.00530.x 19. Sahn DJ, De Maria A, Kissio J, Weiman A. Recomendation
regar-ding quantitation in M-mode echocardiography: results of a survey of echocardiographyc measurements. Circulation 1978;58:1072-83. DOI: http://dx.doi.org/10.1161/01.CIR.58.6.1072
20. Devereux RB, Reichek N. Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation 1977;55:613-8. PMID: 138494 21. Okumura K, Io H, Matsumoto M, Seto T, Takagi M,
22. Matsumoto M, Io H, Furukawa M, Okumura K, Masuda A, Seto T, et al. Risk factors associated with increased left ven-tricular mass index in chronic kidney disease patients eva-luated using echocardiography. J Nephrol 2012;25:794-801. DOI: http://dx.doi.org/10.5301/jn.5000066
23. Cuadrado L, Franco RJS, Christovan JC, Gut AL, Okoshi K, Sampaio M, et al. Efeito do tratamento anti-hipertensivo com enalapril sobre o índice de massa ventricular esquerda em hi-pertensos idosos com ou sem hipertrofia ventricular esquerda. Nefrologia 1993;13:4-7.
24. Portolés J. The beneficial effects of intervention in early renal disease. Nephrol Dial Transplant 2001;16:12-5. DOI: http:// dx.doi.org/10.1093/ndt/16.suppl_2.12