Incidence of constipation in an intensive care unit
INTRODUCTION
According to the European Society for Clinical Nutrition and Metabolism (ESPEN) guidelines, a critical patient is one who develops a systemic inlammatory response associated with organ failure, with the expectation
of support for organ function for at least 3 days.(1) Critical patients are
also characterized by increased morbidity due to infection, prolonged hospitalization, and high mortality.(2)
These patients are susceptible to developing various gastrointestinal complications. Constipation is one of these complications and has an Tatiana Lopes de Souza Guerra1, Simone Sotero
Mendonça1, Norma Guimarães Marshall1
1.Residency Program in Clinical Nutrition, Hospital Regional da Asa Norte, Secretaria de Estado de Saúde do Distrito Federal - Brasília
(DF), Brazil. of constipation in critical patients on Objectives: To evaluate the incidence
enteral nutrition in a hospital intensive care unit and to correlate this incidence with the variables found for critical patients.
Methods: he present investigation was a retrospective analytical study conducted in the intensive care unit of Hospital Regional da Asa Norte (DF) via the analysis of medical records of patients admitted during the period from January to December 2011. Data on the incidence of constipation and enteral nutritional support, gastrointestinal changes, stool frequency, ventilatory support, and outcomes were collected and analyzed.
Results: he initial sample consisted of 127 patients admitted to the unit during the period from January to December 2011. Eighty-four patients were excluded, and the inal sample consisted of 43 patients. he incidence of constipation, deined as no bowel movement during the irst 4 days of
hospitalization, was 72% (n=31). he patients were divided into a control group and a constipated group. he group of constipated patients reached the caloric target, on average, at 6.5 days, and the control group reached the caloric target in 5.6 days (p=0.51). Constipation was not associated with the length of hospital stay, suspension of nutritional support, or outcome of hospitalization. here was an association between evacuation during hospitalization and a longer duration of hospitalization for a subgroup of patients who did not evacuate during the entire period (p=0.009).
Conclusion: he incidence of constipation in the unit studied was 72%. Only the absence of evacuation during hospitalization was associated with longer hospital stays. Constipation was not associated with the length of hospital stay, suspension of nutritional support, or outcome of hospitalization.
This study was conducted in the Hospital Regional da Asa Norte, Secretaria de Estado de Saúde do Distrito Federal - Brasília (DF), Brazil.
Conflicts of interest: None.
Submitted on December 15, 2012 Accepted on June 18, 2013
Corresponding author: Norma Guimarães Marshall
SQSW 103, bloco E, apto 606 - Sudoeste Zip code: 70670-305 - Brasília (DF), Brazil E-mail: norma.guimarães@terra.com.br
ABSTRACT
Keywords: Constipation/ epidemiology; Gastrointestinal motility; Intensive care; Intensive care units
Incidência de constipação intestinal em uma unidade de terapia
intensiva
incidence varying from 15% to 83% in patients admitted to intensive care units (ICUs). This variation is due to the absence of a clear definition because there is no consensus on the concept of constipation, and studies have adopted periods without evacuation
ranging from 3 to 6 days.(3-5) Researchers define
constipation as periods of 3,(3,6-9) 4,(10) or 6 consecutive days(11,12) without evacuation. This complication is caused by infrequent evacuation or reduced intestinal motility.(3) However, investigations of gastrointestinal motility and stool consistency in critical patients are limited because most studies focus on delayed bowel evacuation.(13)
he etiology of this condition is quite complex,(6,14,15) and the literature cites a number of factors that may be related: coninement to bed, use of sedatives and opioids, neuromuscular blocking agents, vasopressors,
inlammatory mediators, electrolytic disorders,(5,6)
inadequate administration of luids, and lack of iber in enteral nutrition.(13,16) Fiber-free enteral diets are recommended for critical patients at high risk of intestinal ischemia or severe dysmotility.(2)
Observational studies relate constipation to longer hospital stays,(8,9,17) increased mortality,(12,17) intolerance to enteral nutrition,(15) abdominal distension, failure to wean
from mechanical ventilation (MV),(6,9) obstruction and
intestinal perforation,(9) and aspiration pneumonia.(14,16,18) However, the monitoring of gastrointestinal function in the ICU is usually geared toward controlling gastric residuals and diarrhea, thus neglecting constipation and its implications.(3)
herefore, the present study aimed to evaluate the incidence of constipation in critical patients on enteral nutrition in a hospital ICU of the Distrito Federal and to relate this incidence to variables found in critical patients.
METHODS
he present investigation was conducted in the ICU of Hospital Regional da Asa Norte (HRAN), Brasília (DF), Brazil, and was a retrospective analytical study analyzing the medical records of patients hospitalized in the unit in the period from January to December 2011. he study was submitted to and approved by the Ethics Research Committee of the Fundação de Ensino e Pesquisa em Ciências da Saúde (FEPECS) under protocol 566/11. Because the present investigation was a retrospective
study based on medical record data, informed consent was not required.
Records were selected of patients who were admitted during the period from January to December 2011 and who met the following inclusion criteria: critical patients according to the ESPEN 2009 deinition who began enteral feeding within 72 hours of admission; admitted onto MV or starting the same within 72 hours
and remaining on the same until at least the 5th day of
admission; aged over 18 years; and length of stay greater than 5 days. he study excluded patients on parenteral nutrition therapy; patients who were orally fed; patients undergoing gastrointestinal surgery immediately before admission; and patients with colostomies, ileostomies, and intestinal istulae.
All the data were collected from electronic medical
records in the InterSystems TrakCareTM production
database, with the aid of a spreadsheet designed for this purpose, and all the data relected the protocols used in the unit.
Constipation was deined as the absence of a bowel movement during the irst 4 days of hospitalization, as in the study of Patanwala et al.(10) Based on this deinition of constipation, the selected patients were divided into two groups: one group of patients who developed constipation and the other group (designated as the control group) comprising those who evacuated during the irst 4 days of hospitalization.
he collected data included the gender, age, length of ICU stay, irst day of enteral feeding, number of days required to reach the caloric target, high gastric residuals (>500 mL), occurrence of evacuation, and outcome of hospitalization (i.e., discharge or death). Data required for a systemic inlammatory response syndrome (SIRS) diagnosis pertaining to the irst 4 days of hospitalization were also collected, along with the occurrence of at least one organ dysfunction or failure on admission, according to the aforementioned criteria.
he groups were compared regarding the early introduction of enteral nutrition (occurring within 48 hours of admission), time required to achieve energy needs, interruption of the enteral diet due to high gastric residuals, failure to wean from MV, length of stay, and mortality associated with constipation.
Kcal/kg/day, based on the actual or estimated weight(1) measured by a bed scale or reported by family members, or, failing these, the weight was estimated using the visual body mass index (BMI) scale for bedridden
patients.(19) For obese patients, the recommendation
was 22-25 Kcal/kg/day based on ideal weight.(2)
Height was measured by the recumbent-stature or knee-height formula.(20)
he inluence of an early enteral-nutrition supply on the occurrence of constipation in the diferent patient groups was ascertained. In this case, early enteral nutrition via tube feeding was considered to be introduced within the irst 48 hours of hospitalization. To evaluate whether the occurrence of constipation had an efect on the time required to meet a given patient’s energy requirements, the time (in days) required to reach the caloric target was analyzed.
An evaluation was also made of whether constipation increased the occurrence of gastric residuals, thereby interrupting the diet administration. he analysis was based on the total number of interruptions caused by high gastric residuals, which was deined by the presence of greater than 500 mL of residuals within 24 hours associated with gastrointestinal symptoms such
as vomiting and abdominal distension.(2) he efect of
interruptions on exams or hemodynamic instability were not considered for the comparison between groups. he total time on MV was observed. Finally, the outcomes (i.e., the number of deaths and discharges) were compared between the two groups.
The statistical analysis consisted of a descriptive analysis of the data and a comparison of the means and frequencies. For comparisons of the means, the hypothesis of data normality was initially tested. The Shapiro-Wilk, Kolmogorov-Smirnov, and
Anderson-Darling tests were used for this purpose.
For data showing a normal distribution, the t test was
used to compare the mean between the two groups. For data that did not follow a normal distribution, the Mann Whitney nonparametric test was used. As most contingency tables displayed expected values less than 5, the Fisher exact test was used to compare the categorical variables. The level of statistical significance was set at 5% (p<0.05). The collected data were stored on a Microsoft Office Excel 2007 spreadsheet, and the test results were generated
with the aid of Statistical Analysis Software (SAS)
version 9.2.
RESULTS
he initial sample comprised 127 patients admitted to the HRAN ICU during the period from January to
December 2011. Eighty-four patients were excluded,and
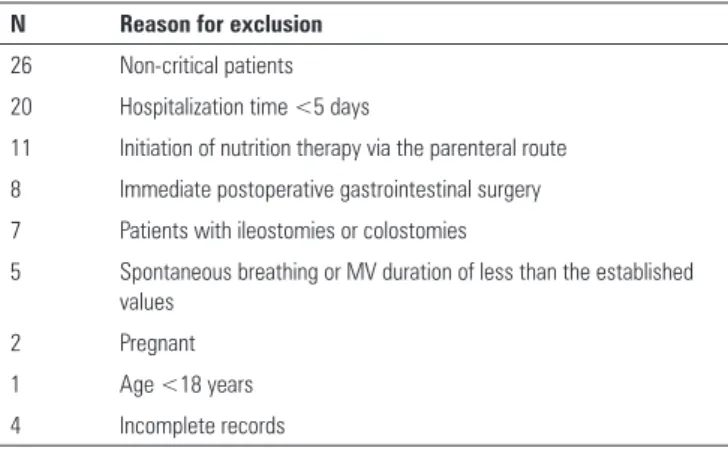
the inal sample consisted of 43 patients. he exclusion criteria are listed in table 1.
Table 1 - Reasons for exclusion based on the adopted criteria
N Reason for exclusion
26 Non-critical patients 20 Hospitalization time <5 days
11 Initiation of nutrition therapy via the parenteral route
8 Immediate postoperative gastrointestinal surgery 7 Patients with ileostomies or colostomies
5 Spontaneous breathing or MV duration of less than the established values
2 Pregnant
1 Age <18 years
4 Incomplete records
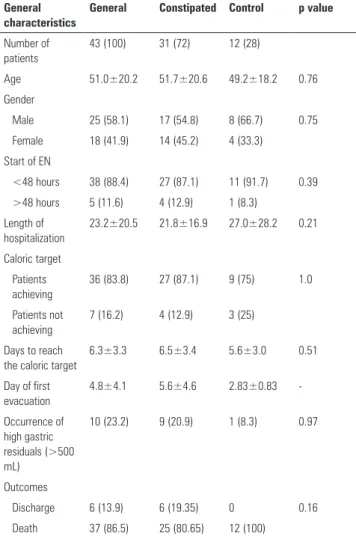
In this study, the incidence of constipation was found to be 72%. he mean time to the irst bowel movement was 5.6 days in the group of constipated patients and 2.8 days in the control group, as presented in table 2.
Regarding the commencement of enteral nutritional therapy, this type of nutrition was introduced early in both groups, occurring within the irst 48 hours for the majority of the sample. he percentages are listed in table 2. No association was found between the period of nutritional-therapy introduction and the duration until bowel evacuation. Moreover, there was no association between the age or gender of the patients and constipation.
No association was found in relation to the mean length of stay between the groups (p=0.21). However, in the group of constipated patients, when a small subgroup of ten patients was observed who did not evacuate at all during hospitalization, even with the introduction of a stimulus, a p-value of 0.009 was obtained; this inding demonstrated a negative association between the length of stay and the absence of evacuation.
here was no statistical signiicance regarding the number of days required to reach the caloric target, and on average, the constipated and control groups achieved the target caloric intake within 6.5 days and 5.3 days, respectively.
(p=0.08), abdominal distension (p=0.13), or diet suspension (p=0.48). Despite abdominal distension not being associated with constipation in the present study, it was noted that the occurrence of abdominal distension was associated with diet suspension (p=0.04).
Another variable was the observed MV duration, and no association was found between this factor and constipation. Notably, 86% of the patients remained on MV until their death, and the six (14%) patients who experienced weaning were the same patients who were discharged. No association was found between the patient outcomes and the occurrence of constipation.
DISCUSSION
In the present investigation, the incidence of constipation was high. Similar results have been observed
in other studies, varying between 15% and 83%.(3-5) his variation can be attributed to the diferent deinitions of constipation adopted by diferent researchers. However, it is noteworthy that these studies only focus on the time required for bowel evacuation, concentrating on the initial period of hospitalization. If the deinition were applied to the entire period of hospitalization, then the incidence might be much higher. Furthermore, this
deinition does not include constipation as a relection of organ dysfunction, which would have a higher correlation with patient outcomes.
No association was found between the early initiation of enteral nutritional support and the frequency of constipation (p=0.39). his comparison aimed to assess whether the early introduction of the diet would interfere with the patients’ bowel evacuation. Nassar et al. found that early initiation of enteral support was associated with a lower incidence of constipation (p<0.01), with early support deined as that initiated within 24 hours of admission.(6) In the present study, early introduction was deined as that occurring up to 48 hours after admission,
as recommended by ASPEN.(2)
In the present study, constipation was not associated with the patient’s length of stay (p=0.21), which corroborates the indings of Nassar et al.(6) By contrast, in Gacouin et al.’s study, constipation was associated with a longer hospital stay (p<0.01),(12) and in Mostafa et al.’s study, the mean length of the ICU stay was higher for constipated patients (10 days versus6.5 days).(3)
However, this study presents an important inding because 10 of the 43 patients had no bowel movements at all during hospitalization, even with the introduction of a stimulus for 20% (n=2) of this subgroup. When these data were correlated to the length of stay, a p-value of 0.009 was obtained, thereby demonstrating a negative association between the length of stay and the absence of evacuation. his inding may be related to Nassar et al.’s assertion that evacuation may be considered a sign of preserved gastrointestinal function.(6) According to Asai, constipation can lead to bacterial overgrowth, which is a cause of nosocomial infections and sepsis in patients who are hospitalized for prolonged periods.(21)
Regarding the number of days required to reach the caloric target, no signiicant diference was found between the groups, demonstrating that the length of time before bowel evacuation did not afect the achievement of nutritional requirements. his inding is important because ASPEN recommends that the caloric target be reached within 7 days of admission.(2)
EN - enteral nutrition. The results are expressed as a number (%) or as the mean±standard deviation.
Table 2 - General characteristics of the final sample of patients hospitalized in the intensive care unit
General characteristics
General Constipated Control p value
Number of patients
43 (100) 31 (72) 12 (28)
Age 51.0±20.2 51.7±20.6 49.2±18.2 0.76
Gender
Male 25 (58.1) 17 (54.8) 8 (66.7) 0.75
Female 18 (41.9) 14 (45.2) 4 (33.3)
Start of EN
<48 hours 38 (88.4) 27 (87.1) 11 (91.7) 0.39
>48 hours 5 (11.6) 4 (12.9) 1 (8.3)
Length of hospitalization
23.2±20.5 21.8±16.9 27.0±28.2 0.21
Caloric target
Patients achieving
36 (83.8) 27 (87.1) 9 (75) 1.0
Patients not achieving
7 (16.2) 4 (12.9) 3 (25)
Days to reach the caloric target
6.3±3.3 6.5±3.4 5.6±3.0 0.51
Day of first evacuation
4.8±4.1 5.6±4.6 2.83±0.83
-Occurrence of high gastric residuals (>500 mL)
10 (23.2) 9 (20.9) 1 (8.3) 0.97
Outcomes
Discharge 6 (13.9) 6 (19.35) 0 0.16
One of the complications cited in the literature relating to the diiculty of dietary progression is the presence of high gastric residuals. However, it was found that the presence of constipation did not increase the incidence of high gastric residuals (p=0.97), vomiting (p=0.08), or abdominal distension (p=0.13) or the diet suspension (p=0.48). Despite abdominal distension not being associated with constipation in the present study, it should be noted that abdominal distension was associated with the diet suspension (p=0.04).
No association was found between the MV duration and the presence of constipation. Conversely, Gacouin et al. observed that the MV duration is higher in constipated patients (p<0.01).(12)
No association was found between patient outcomes and the occurrence of constipation. By contrast, the study of Gacouin et al. demonstrated that constipation
was associated with mortality (p<0.05).(12) Despite
death having been observed as an outcome in 86.5% of the subjects, it was not possible to establish whether the mortality rates were high in both groups, as it was impossible to compare these data with prognostic mortality rates because the calculation of these rates upon admission was not practical in the unit where the study was conducted.
Constipation is a frequent problem in critical patients, but the available recommendations for its prevention and treatment are still scarce. Certain researchers have proposed the implementation of intervention protocols for constipation.(7,9,16,22) In this regard, Dorman et al. observed the absence of records on bowel function in 77% of the analyzed days before implementation of a protocol for this purpose.(7) Another study revealed that utilizing a protocol increases the number of days that the bowel function is recorded from 87% to 100%, with a consequent reduction in the incidence of constipation from 57.7% to 37.0%, thus representing a 20.7% decrease overall (p=0.13).(9)
Other investigators have evaluated the ability of agents capable of promoting evacuation or preventing constipation, such as in the study by van der Spoel et al. hese authors demonstrated that the use of polyethylene
glycol and lactulose is efective in inducing evacuation and is associated with a shorter hospital stay.(23) In another study, the use of lactulose was efective in preventing constipation and yielded an efect that was contradictory to the literature because patients spending a longer time
on MV had early bowel evacuations.(17)
he present investigation had several limitations, such as the use of pre-existing data records, the quality of which was compromised because the information was not recorded for scientiic purposes. Furthermore, the study was performed in a single unit, so the results cannot be extrapolated to other ICUs. Another limitation was the small sample size, which can be attributed to the fact that the unit contained only 10 beds, and there was a low patient turnover and a prolonged length of stay.
Importantly, this was a retrospective study, and it was not possible to evaluate important factors potentially related to constipation because they were not described in the evaluated medical records. Some of these factors were the following: coninement to the bed or the degree of patient mobility, the use of vasopressor drugs and opioid drugs, not having used the dosages described in all of the patients’ medical records, and attempts at MV weaning.
he present study demonstrated the necessity of monitoring hospitalized patients’ bowel function using a multidisciplinary approach, recording the frequency of the patients’ bowel evacuations, and administering laxative agents according to a standardized protocol.
Currently, few studies address constipation in critical patients and its efects on their prognosis. Published data present diferent deinitions of constipation, which can considerably afect its incidence. herefore, additional prospective studies are required for elucidating the efects of constipation on the prognosis of critical patients.
CONCLUSION
REFERENCES
1. Singer P, Berger MM, Van den Berghe G, Biolo G, Calder P, Forbes A, Griffiths R, Kreyman G, Leverve X, Pichard C, ESPEN. ESPEN Guidelines on Parenteral Nutrition: Intensive care. Clin Nutr. 2009;28(4):387-400. 2. McClave SA, Martindale RG, Vanek VW, McCarthy M, Roberts P, Taylor B,
Ochoa JB, Napolitano L, Cresci G; A.S.P.E.N. Board of Directors; American College of Critical Care Medicine; Society of Critical Care Medicine. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr. 2009;33(3):277-316.
3. Mostafa SM, Bhandari S, Ritchie G, Gratton N, Wenstone R. Constipation and its implications in the critically ill patient. Br J Anaesth. 2003;91(6):815-9. 4. Montejo JC. Enteral nutrition-related gastrointestinal complications in
critically ill patients: a multicenter study. The Nutritional and Metabolic Working Group of the Spanish Society of Intensive Care Medicine and Coronary Units. Crit Care Med. 1999;27(8):1447-53.
5. Azevedo RP, Freitas FG, Ferreira EM, Machado FR. Constipação intestinal em terapia intensiva. Rev Bras Ter Intensiva. 2009;21(3):324-31. 6. Nassar AP Jr, da Silva FM, de Cleva R. Constipation in intensive care unit:
incidence and risk factors. J Crit Care. 2009;24(4):630.e9-12.
7. Dorman BP, Hill C, McGrath M, Mansour A, Dobson D, Pearse T, et al. Bowel management in the intensive care unit. Intensive Crit Care Nurs. 2004;20(6):320-9.
8. Oliveira SM, Burgos MG, Santos EM, Prado LV, Petribú MM, Bomfim FM. Complicações gastrointestinais e adequação calórico-protéica de pacientes em uso de nutrição enteral em uma unidade de terapia intensiva. Rev Bras Ter Intensiva. 2010;22(3):270-3.
9. McPeake J, Gilmour H, MacIntosh G. The implementation of a bowel management protocol in an adult intensive care unit. Nurs Crit Care. 2011;16(5):235-42.
10. Patanwala AE, Abarca J, Huckleberry Y, Erstad BL. Pharmacologic management of constipation in the critically ill patient. Pharmacotherapy. 2006;26(7):896-902.
Objetivos: Avaliar a incidência de constipação em pacientes críticos em uso de nutrição enteral internados em uma unidade de terapia intensiva e correlacioná-la a variáveis encontradas em pacientes críticos.
Métodos: Estudo de caráter retrospectivo analítico, realiza-do na unidade de terapia intensiva realiza-do Hospital Regional da Asa Norte (DF), por meio da análise de prontuários de pacientes internados no período de janeiro a dezembro de 2011. Foram coletados e analisados dados referentes a incidência de consti-pação intestinal e ao suporte nutricional enteral, alterações gas-trintestinais, frequência de evacuação, assistência ventilatória e desfechos.
Resultados: A amostra inicial foi de 127 pacientes admi-tidos na unidade no período de janeiro a dezembro de 2011. Foram excluídos 84 pacientes e a amostra inal compôs-se de 43 pacientes. A incidência de constipação, deinida como ausência
de evacuação nos primeiros 4 dias de internação, foi de 72% (n=31). Os grupos foram divididos em constipados e controle. O grupo de pacientes constipados atingiu a meta calórica, em média, com 6,5 dias e o grupo controle em 5,6 dias (p=0,51). A constipação não se associou ao tempo de internação, suspen-são do aporte nutricional e desfecho da internação hospitalar. Houve associação entre ausência de evacuação durante toda a internação por um subgrupo dos pacientes que não evacuaram em todo o período e tempo maior de internação (p=0,009).
Conclusão: A incidência de constipação intestinal na uni-dade pesquisada foi de 72%. Somente a ausência de evacuação durante toda a internação associou-se a maior tempo de inter-nação. Tempo de internação, suspensão do aporte nutricional e desfecho da internação hospitalar não apresentaram associação.
RESUMO
Descritores: Constipação intestinal/epidemiologia; Motilidade gastrintestinal; Cuidados intensivos; Unidades de terapia intensiva
11. van der Spoel JI, Schultz MJ, van der Voort PH, de Jonge E. Influence of severity of illness, medication and selective decontamination on defecation. Intensive Care Med. 2006;32(6):875-80.
12. Gacouin A, Camus C, Gros A, Isslame S, Marque S, Lavoué S, et al. Constipation in long-term ventilated patients: associated factors and impact on intensive care unit outcomes. Crit Care Med. 2010;38(10):1933-8. 13. Bishop S, Young H, Goldsmith D, Buldock D, Chin M, Bellomo R. Bowel
motions in critically ill patients: a pilot observational study. Crit Care Resusc. 2010;12(3):182-5.
14. Chappell D, Rehm M, Conzen P. Opioid-induced constipation in intensive care patients: relief in sight? Crit Care. 2008;12(4):161.
15. López-Herce J. Gastrointestinal complications in critically ill patients: what differs between adults and children? Curr Opin Clin Nutr Metab Care. 2009;12(2):180-5.
16. Ferrie S, East V. Managing diarrhoea in intensive care. Aust Crit Care. 2007;20(1):7-13.
17. Masri Y, Abubaker J, Ahmed R. Prophylactic use of laxative for constipation in critically ill patients. Ann Thorac Med. 2010;5(4):228-31.
18. Staats PS, Markowitz J, Schein J. Incidence of constipation associated with long-acting opioid therapy: a comparative study. South Med J. 2004;97(2):129-34.
19. Fogaça KC, Oliveira MR. Escala de figuras aplicada à avaliação subjetiva do IMC de pacientes acamados. Saúde Rev. 2003;5(10):35-41.
20. Kamimura MA, Baxmann A, Sampaio LR, Cuppari L. Avaliação nutricional. In: Cuppari L. Guias de medicina ambulatorial e hospitalar da UNIFESP/EPM: Nutrição clínica no adulto . 2a ed. São Paulo: Manole; 2005. p. 89-115. 21. Asai T. Constipation: does it increase morbidity and mortality in critically ill
patients? Crit Care Med. 2007;35(12):2861-2.
22. McKenna S, Wallis M, Brannelly A, Cawood J. The nursing management of diarrhoea and constipation before and after the implementation of a bowel management protocol. Aust Crit Care. 2001;14(1):10-6.