COMPARISON OF SECURING (Rt) IJV ANATOMICAL LANDMARK
TECHNIQUE V/S U. S. GUIDED TECHNIQUE
M. Veeresham1, M. V. Bhimeswar2, Priyam3
HOW TO CITE THIS ARTICLE:
M. Veeresham, M. V. Bhimeswar, Priyam. ”Comparison of Securing (Rt) IJV Anatomical Landmark Technique v/s U. S. Guided Technique”. Journal of Evidence based Medicine and Healthcare; Volume 2, Issue 28, July 13, 2015; Page: 4114-4127, DOI: 10.18410/jebmh/2015/585
ABSTRACT: Vascular access of central venous lines especially right internal jugular vein is very commonly performed procedure during the general anaesthesia to monitor the patient’s vascular status, and giving drugs to the patients through these lines. Ultra sound guided technic improves the securing time and minimizes the complications of the surrounding structures both vascular and nerves other important structures in the securing area.
KEYWORDS: C. V. (Central Venous), IJV (Internal Jugular vein), ANL (Anatomical Land Mark Technic), U. S. (Ultrasound Guided), G. A (General Anaesthesia).
INTRODUCTION: Central venous (CV) access is a commonly performed procedure with multiple indications in routine and emergent situations.
Central venous access is defined as placement of a catheter such that the catheter is inserted into a venous great vessel. The venous great vessels include the superior vena cava, inferior vena cava, brachiocephalic veins, internal jugular veins, subclavian veins, iliac veins, and common femoral veins.
AIMS AND OBJECTIVES: The aim of this prospective observational study is to explore the safety and efficacy of RIJ vein cannulation using two techniques:
Using anatomical landmarks method.
Using Ultrasound machine.
To compare following parameters in two different techniques:
Time taken for cannulation (in seconds) from completion of skin preparation and draping to successful aspiration of venous blood.
Number of attempts required for successful cannulation of IJV.
Complications encountered, if any such as carotid puncture, hematoma, pneumothorax, injury to brachial plexus etc.
MATERIALS AND METHODS: After approval by the college ethical committee the study was undertaken in our institution Gandhi Hospital and Gandhi Medical College.
Selection of Cases: Study included a total of 50 patients of American Society of Anaesthesiologists (ASA) grade I & II, of either sex between ages 20 and 60 scheduled for elective abdominal surgery.
Inclusion Criteria: Following patients were included in our study: 1. ASA grade I and II.
2. Age between 20 and 60 years, either sex. 3. Elective abdominal surgery.
Exclusion Criteria: Following patients were excluded from our study 1. Patient’s refusal.
2. Patients with previous CVC within 15 days.
3. Anatomical deformity, e.g., neck surgery, malignancy. 4. Coagulopathy or patient on anticoagulants.
5. Burns on the site of insertion.
6. Local infection over the intended site. 7. Gross obesity.
A written informed consent was taken from each patient.
Patients were randomly allocated to one of the two groups using closed – envelope method. (25 patients in each group).
Group USG: In this group Internal Jugular cannulation was performed with the help of USG via a transverse approach.
Group ANL: In this group Internal Jugular cannulation was performed with anatomical landmarks method.
PROCEDURE FOR INTERNAL JUGULAR VEIN CANNULATION: On arrival in the operating room standard monitors (non invasive blood pressure, pulse oximeter, electrocardiography) were applied and monitored throughout the procedure. A peripheral IV line was secured.
After induction of general anaesthesia the procedure for Internal Jugular Vein Cannulation was started. All the cannulations were done by a single person in order to standardise the procedure.
Following equipment was used:
Antiseptic solution for skin cleansing.
Sterile drapes, gloves, and gown, and mask and cap.
A preassembled kit for central line cannulation LIFELINE CVP.
CATHETER DOUBLE LUMEN 7FR 15CM ADULT containing:
18-gauge introducer needle.
Two 5-mL syringes.
J-wire configured guide wire.
No. 11 blade scalpel.
Semi rigid dilator.
Suture (commonly, 3-0 silk on a straight cutting needle).
Gauze pads,
Heparinised saline solution.
Antibiotic ointment for the dressing.
Plastic occlusive dressing such as Tegaderm.
For the USG group additional equipment used were as follows;
Portable ultrasound machine (GE LOGIQ e BT11) with high-frequency linear transducer.
Sterile transduction jelly.
Acoustically transparent sterile sheath for USG transducer
Sterile rubber bands to secure the sheath around the transducer.
Positioning: The patients were placed in the Trendelenburg position 10- 15◦ and head was turned to contralateral side.
Putting the patient in the Trendelenburg position dilates the internal jugular vein, makes cannulation easier and reduces the risk of air embolism.
Turning the patient’s head away from the side of the internal jugular vein being accessed provides access to the side of the neck and also makes the sternocleidomastoid muscle more prominent so that the landmarks are easier to identify.
Extreme head rotation was avoided as it causes the internal jugular vein to overlie the carotid artery, and increase the risk of carotid arterial puncture.
Some padding was placed under the patient’s shoulders as some head and neck extension is helpful.
Preparation:
Full aseptic precautions were taken.
This included:
Washing hands before the procedure, wearing a mask and sterile gloves and gown by the person performing the cannulation.
The patient’s skin was cleaned widely from earlobe to clavicle to sternal notch, using antiseptic (10 percent povidone-iodine).
Sterile drape with fenestration to allow visualization of the middle of the neck was applied.
The lumens of the central line are flushed with heparin.
The guide wire is passed through the needle to ensure that the guide wire threads easily.
Cap is removed from the port through which the guide wire will be threaded. This is commonly the longer lumen.
When using ultrasound, the ultrasound probe is prepared with a long sterile sleeve.
ANATOMICAL LANDMARKS METHOD – TECHNIQUE:
Anatomic landmarks, including the sternal notch, clavicle, and sternocleidomastoid muscle, were identified before preparation and draping for the sterile procedure because these landmarks are appreciated better before they are covered by the sterile drape. The carotid artery was palpated and its course in the neck determined.
After sterile preparation and draping the relevant anatomical landmarks were identified again. The apex of the triangle formed by the two heads of the sternocleidomastoid muscle and the clavicle identified.
The skin was punctured at the apex of the triangle at the medial border of the clavicular head of the SCM muscle, entering just lateral to the carotid pulse. This was done with the 18G introducer needle with 5ml syringe attached to it, the syringe contained 2-3ml heparinised saline.
During skin puncture palpation of the carotid artery was maintained with the non-dominant hand.
Using the insertion needle, the site was approached at an angle of 45 degrees from the coronal plane with the long axis of the needle directed towards the ipsilateral nipple.
The needle was advanced while applying gentle suction to the syringe.
Typically the vein was entered at a depth of 1-3cm. When the IJV was entered a flash of venous blood is obtained. Once the needle had entered the vessel and steady blood return had been obtained, the syringe was gently removed while holding the needle steady with the non-dominant hand. Dark non pulsatile flow confirmed access to the vein.
Using the introducer the curved end of the guide wire was advanced through the needle. An assistant watched the monitor looking for signs of arrhythmia while the guide wire was being advanced. If arrhythmia occurred the guide wire was withdrawn till the arrhythmia ceased.
After the guide wire was inserted to appropriate depth, the needle was withdrawn leaving the guide wire in place.
Using a no. 11 scalpel a small superficial incision was made at the entry point of the wire to facilitate the passage of the guide wire through the skin.
Next the catheter was fed over the guide wire. A firm control was maintained over the guide wire at all times in order to prevent a wire embolism. While grasping the external end of the guide wire the catheter was advanced through the skin using a rotating motion.
The guide wire was removed and blood return checked at all ports. All the ports were flushed, caps placed on the hubs. The catheter was anchored to the skin with sutures and sterile dressing was applied.
A chest x-ray was obtained to assess proper placement.
Figure shows the normal position of a right sided IJV catheter. The tip of the right sided IJV cannula should ideally lie just above the level of the carina 2. This is the junction of the left and right innominate veins with the superior vena cava (SVC).
ULTRASOUND METHOD – TECHNIQUE: Ultrasound survey was performed before starting the procedure to assess the location and patency of the internal jugular vein and to evaluate neck anatomy.
We used the transverse approach so that probe was placed parallel and cephalad to the clavicle and along the sternocleidomastoid muscle.
The probe marker was placed facing the patient's left side, corresponding to the marker on the ultrasound screen.
Figure 2
The common carotid artery and internal jugular vein were identified. The common carotid artery was identified as the circular, pulsating structure which was difficult to compress. The IJV was identified as the larger, easily compressible and non-pulsating structure.
The patency of the IJV was confirmed by gently compressing the vein with the transducer. If patent, slight pressure is sufficient to collapse the lumen of the IJV.
The internal jugular vein was tracked from the angle of the mandible down into the supraclavicular fossa using the linear ultrasound probe in the transverse orientation. The ideal location for needle puncture was chosen where IJV overlap with the CCA was minimal.
Skin preparation and draping was done as mentioned above.
In addition, the ultrasound probe was prepared with the help of an assistant. The assistant was asked to apply ultrasound gel to the linear probe and a sterile cover was placed on the probe. Any bubbles between the face of the probe and the inner surface of the sterile sheath were eliminated, as this leads to suboptimal imaging. Sterilized ultrasound gel was then applied to the outside of the ultrasound cover for scanning during the procedure
The Central line equipment was prepared as mentioned above.
The probe was placed on the chosen location is a transverse manner. The internal jugular vein was imaged and placed in the centre of the ultrasound field.
The needle was advanced at a 45 degrees angle and 1 cm behind the middle of the ultrasound probe while maintaining negative pressure in the syringe. The operator continually looked at the ultrasound screen and the patient's neck and needle while making adjustments in the needle position.
The needle and the corresponding soft tissue tenting was observed on the ultrasound monitor.
Although the needle tip was not visualised sometimes, the soft tissue tenting was always observed. Small in and out movements or tapping movements helps to visualise the trajectory of the needle. In addition location of the needle tip may be visualised by tilting the transducer back and forth.
When the needle was aligned correctly, this soft tissue tenting was located directly over the target vessel. If the needle tip was angled lateral or medial to the vessel, the needle was withdrawn to just below the skin surface, and its orientation changed. Once the needle was passed in the correct plane, the needle tip was seen on the ultrasound screen to "indent" the wall of the internal jugular vein.
However since ultrasonography does not necessarily confirm the location of the tip, aspiration of blood in the syringe was looked for.
Once blood flashback was obtained, the syringe was disconnected, the needle stabilized, non-pulsatile blood flow confirmed and guide wire passed through the needle into the vein.
After the guide wire was inserted to appropriate depth, the needle was withdrawn leaving the guide wire in place. At this point, the guide wire within the lumen of the vein can be visualised on the screen in both cross sectional and longitudinal views.
The dilator was used to prepare a path for the catheter. After dilation of the soft tissues and vein, the catheter was passed into the target vessel.
The guide wire was removed and blood return checked at all ports. All the ports were flushed, caps placed on the hubs and the line secured in place by suturing and sterile dressing was applied.
Chest x-ray was taken after 6hrs to rule out procedure-related pneumothorax.
INTRAOPERATIVE MONITORING: Access time was defined as the time between penetration of the skin and aspiration of venous blood into the syringe. This provided an objective comparison between the two techniques. Taking the entire procedural time into account would have clouded the issue because other parameters such as preparation and time taken to wrap the transducer in a sterile sheath could affect the measurement. The access time was measured in seconds by stopwatch by the nursing staff.
Number of attempts (needle thrusts) and complications (carotid artery puncture, skin hematoma, brachial plexus irritation) were recorded. Carotid artery puncture was noted by forceful pulsatile expulsion of bright red blood from the needle.
Illustration of a longitudinal compression wave (top) and transverse wave (bottom).
Probes include the curvilinear (Left), phased array (Center), and linear array (right) types. Figure 4
Static (indirect) method:
Static (indirect) method, showing course of right internal jugular vein identified by ultrasonography.
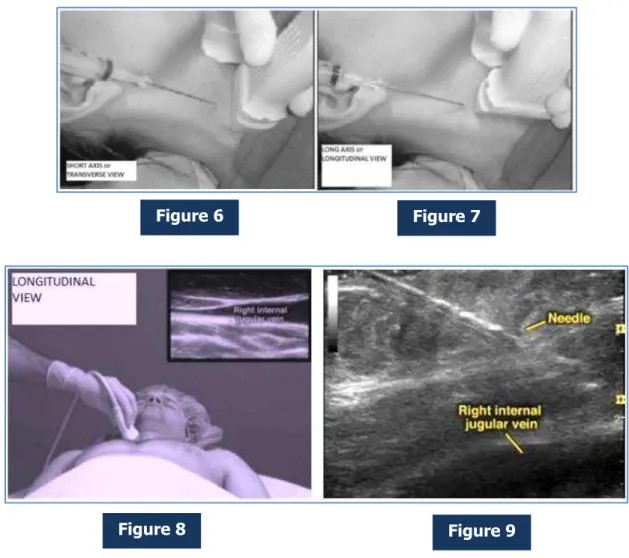
Figure 6 Figure 7
Figure 8 Figure 9
OBSERVATION AND RESULTS: Total 50 patients were selected. All patients were posted for abdominal surgeries and randomly divided into two equal groups.
USG Group: IJV cannulation was performed with the help of USG.
ANL Group: IJV cannulation was performed with anatomical landmarks method.
Data are presented as mean ± SD or as the number of patients per category. A chi-square test was used to compare categorical variables, and a Student's t-test was used to compare independent means. P-values < 0.05 were considered statistically significant.
USG ANL p
Age in yr
(Mean±SD) 38.8±9.874 40.48±8.302 0.518† Weight in kg
(Mean±SD) 62.2±9.138 61.8±9.882 0.882†
Sex Male 20 (80%) 19 (76%) 0.99*
Female 5 (20%) 6 (24%)
Table 1: Comparison of age, gender and weight in between two groups undergoing Internal Jugular Cannulation with different technique:
†student’s unpaired t-test *chi-square test.
The two group ware compared with respect to age, weight (students t-test) and sex (chi square test). There were no statistically significant differences between the two groups (p>>0.05).
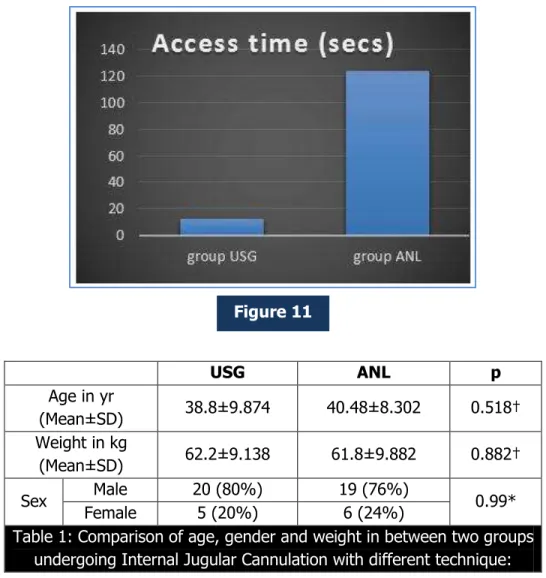
USG ANL p Venous Access time (secs)
Mean ± SD 12.52±4.655 123.68±138.339 0.0002† Range (min – max) 6 – 25 secs 7- 600 secs
Table 2: Access Time in group USG and group ANL
†student’s unpaired t-test.
The primary outcome, i.e., time required for insertion is summarized in [Table 2]. In the USG group, the mean time to successful aspiration of venous blood after completion of draping was 12.52 seconds, while in group II, i.e., the anatomical landmarks group, this time was 123.68 seconds. Statistically this difference was highly significant (t=4.015, p=0.0002).
USG ANL p
No. of attempts
Mean±SD 1.24±0.435 1.68±0.802 0.0198† Range (min – max) 1- 2 1 - 4
Table 3: Number of attempts in group USG and group ANL
†student’s unpaired t-test.
Our next outcome measure was the no. of attempts required for successful cannulation [Table 3]. An average of 1.24 attempts per cannulation was required for USG-guided cannulation, while for anatomical landmarks method average 1.68 attempts were required. Statistically this difference was significant (t = 2.409, p=0.019).
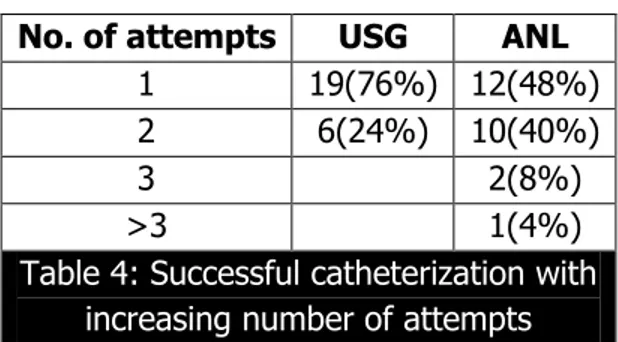
No. of attempts USG ANL
1 19(76%) 12(48%)
2 6(24%) 10(40%)
3 2(8%)
>3 1(4%)
Table 4: Successful catheterization with increasing number of attempts
In Group I, i.e., the ultrasound group, 6 patients (24%) required more than one attempt, whereas in the anatomical landmarks group 13 patients (52%) required more than one attempt. Statistically this difference was significant (t = 2.04, p =0.0469).
Group USG Group ANL
Arterial puncture 0 4
Pneumothorax 0 1
Table 5: Complications Encountered
We also tabulated the complications encountered in both the procedures [Table 4]. In the anatomical landmarks group, we witnessed carotid puncture in four patients (16%) with 2 patients (8%) developing a visible hematoma, and pneumothorax in one patient (4%). There were no such complications in the ultrasound group. External compression was applied for carotid puncture. Pneumothorax was mild and didn’t require any intervention.
There were no incidents of brachial plexus irritations or neurological damage in either group.
DISCUSSION: Percutaneous cannulation of the IJV using external landmarks was first described in 1966.[1] Out of the various routes available IJV catheterization is most preferred in patients
undergoing cardiac surgery because it is safe convenient and easily accessible and there is no risk of catheter kinking during sternal retraction.[2]
Right IJV cannulation is preferred over the left IJV because it has a larger diameter, and a straighter course to the RA.[3]
On the other hand, left IJV cannulation is more time consuming, requires more attempts and is associated with a higher rate of complications including the risk of thoracic duct injury.[4]
The landmark technique has been used traditionally with a success rate of 85-95%.[5,6] It is
a blind procedure primarily based on the anatomical landmarks but an experienced operator also locates the vein by balloting it by finger.[6,7]
First described in 1984 by Legler and Nugent ultrasound has been used as either a pre locating device or a real time guidance device for central venous cannulations.[8] Real-time
ultrasound guidance may be provided either through the external application of an ultrasound probe to visualize the vessels or with Doppler probe for identifying needle entry into the vein.
Troianos et al.,[9] Denys et al.,[10] and Turker et al.,[11] compared landmark technique with
and 97.36%, respectively (in the landmark technique) to 100% (99.47% in the study by Turker et al.,[11]) in the ultrasound-guided group and the number of successful first attempt at cannulations
also increased in the ultrasound group.
IJV cannulation was possible in all of the patients in our study. The anatomical landmark technique had a successful cannnulation of 85% which is in accordance with the success rate reported in previous studies using anatomical landmarks (85-90%).[10,12]
Most of the studies have not specified the definition of successful cannulation, and it varied from<3 attempts without carotid artery puncture to <7 attempts and some investigators have defined it as access time less than 4 minutes.
In our study cannulation was considered successful when done <3 attempts without carotid artery puncture.
Success rate with real-time ultrasound imaging is also in accordance results of previous studies (94-100%).[9,10]
The median venous access time in this study was also found to be statistically different, which is in accordance with previous studies. In this study, 48% of patients in the ANL group in comparison to 76% in the USG group could be cannulated in first attempt. Previous studies showed similar results of success rate with the first attempt in the anatomical landmark technique (28-87%) and in the ultrasound-guided real-time imaging technique (43-96%).[9,10]
The higher success rate in the present study when compared with the landmark technique of the studies by Troianos et al.,[9] Denys et al.,[10] and Turker et al.,[12] is difficult to explain, but it
may be due to the fact that cannulations were performed in anesthetized and mechanically ventilated patients, whereas in all the above mentioned studies, the patients were spontaneously breathing.
Application of positive end expiratory pressure in mechanically ventilated patients also increases the cross sectional area of IJV and facilitates cannulation.[5]
Incidence of carotid artery puncture is in accordance with previous studies using similar techniques.[5,6,9,10,12] Hematoma formation occurred only in one patient who belonged to the AL
group, which was managed by external compression.
As reported in earlier studies, this study demonstrates that ultrasound guidance to be useful in placement of IJV catheters, and decreasing complications.
In 2002, NICE recommended the use of ultrasound for CV cannulation as the preferred method for elective insertion of CV catheters in adults and children, based on studies that show a significant decrease in the rate of failed punctures (86%) and a reduction in complications (57%) and a shorter performance time (1.1 minutes vs. 2.6 minutes).
One important implication of the NICE guidelines is that when ultrasound has not been used, the event of a serious complication will be difficult to defend.
Other drawbacks of using the US-guided technique for IJV catheterization are the procedural complexity of maintaining transducer sterility and the requirement for training the staff to use a new technique.
A small sample size and non-blinded assessment of outcomes were the limitations of this study.
CONCLUSION: In conclusion, application of ultrasound-guided techniques increases the success rate of IJV cannulation, decreases complications, and time of catheterization in comparison to anatomical landmark technique.
Hence, ultrasound guidance should be used as a part of training wherever the facility is available so that it can be used as a backup in difficult situations.
We recommend that all anesthesiologists should be encouraged to teach, train, and practice the skill of CV cannulation using ultrasound guidance.
BIBLIOGRAPHY:
1. Hermosura B, Vanags L, Dickey MW. Measurement of pressure during intravenous therapy. JAMA 1966; 195: 181.
2. Murlidhar K. Left internal versus right internal jugular vein access to central venous cannulation using the seldinger technique. J Cardiothorac Vasc Anesth 1995; 9: 115-6. 3. Khalil KG, Parker FB Jr., Mukherjee N, Webb WR. Thoracic duct injury. A complication
of jugular vein catheterization. JAMA 1972; 221: 908-9.
4. Ishizuka M, Nagata H, Takagi K, Kubota K. Right internal jugular vein is recommended for central venous catheterization. J Invest Surg 2010; 23: 110-4.
5. Sulek CA, Blas ML, Lobato EB. A Randomized study of left versus right internal jugular vein cannulation in adults. J Clin Anesth 2000; 12: 142-5.
6. Sznajder JI, Zveibil FR, Bitterman H, Weiner P, Bursztein S. Central venous catheterization. Failure and complication rates by three percutaneous approaches. Arch intern Med 1986; 146: 259-61.
7. Hayashi H, Ootaki C, Tsuzuku M, Amano M. Respiratory jugular venodialtion: A new landmark for right internal jugular vein puncture in ventilated patients. J Cardiothorac Vasc Anesth 2000; 14: 40-4.
8. Verghese ST, Nath A, Zenger D, Patel RI, Kaplan RF, Patel KM. The effects of the simulated Valsalva maneuver, liver compression, and/or Trendelenburg position on the cross-sectional area of the internal jugular vein in infants and young children. Anesth Analg 2002; 94: 250-4.
9. Legler D, Nugent M. Doppler localization of the internal vein facilitates central venous cannulation. Anesthesiology 1984; 60: 481.
10.Troianos CA, Jobes DR, Ellison N. Ultrasound-Guided cannulation of the internal jugular vein. A prospective, randomized study. Anesth Analg 1991; 72: 823-6.
12.Turker G, Kaya FN, Gurbet A, Aksu H, Erdogan C, Atlas A. Internal jugular vein cannulation: An ultrasound-guided technique versus a landmark-guided technique. Clinics 2009; 64: 989-92.
NAME ADDRESS EMAIL ID OF THE CORRESPONDING AUTHOR:
Dr. M. Veeresham, # 16-11-511/D/360/A/1, Shalivahana Nagar, Moosarambagh, Malakpet-500036.
E-mail: drveeresham79@gmail.com
Date of Submission: 07/07/2015. Date of Peer Review: 08/07/2015. Date of Acceptance: 11/07/2015. Date of Publishing: 13/07/2015.
AUTHORS:
1. M. Veeresham 2. M. V. Bhimeswar 3. Priyam
PARTICULARS OF CONTRIBUTORS:
1. Associate Professor, Department of Anesthesiology, Gandhi Medical College, Gandhi Hospital, Hyderabad. 2. Professor, Department of
Anesthesiology, Gandhi Medical College, Gandhi Hospital, Hyderabad. 3. Post Graduate, Department of