R e s u m o R e s u m oR e s u m o R e s u m oR e s u m o
Casos de comportamento violento (CV) durante o sono são relatados na literatura. A incidência de comportamento violento durante o sono não é muito conhecida. Um estudo epidemiológico mostra que cerca de 2% da população geral apresentava comportamento violento dormindo e eram predominantemente homens. Neste artigo, os autores descrevem aspectos clínicos e médico-legais envolvidos na investigação do comportamento violento. O comportamento violento se refere a ferimentos auto-infligidos ou auto-infligidos a um terceiro durante o sono. Ocorre, muito freqüentemente, seguindo um despertar parcial no contexto de um transtorno de despertar (parassonias). Os transtornos do sono predominantes diagnosticados são: transtorno de compor-tamento REM e sonambulismo. O comporcompor-tamento violento poderia ser precipitado pelo estresse, uso de álcool e drogas, privação do sono ou febre.
Descritores: Descritores:Descritores:
Descritores:Descritores: Violência; Transtorno do sono; Transtornos mentais; Sonambulismo; Confusão; Terror noturno; Polissonografia A b s t r a c t
A b s t r a c tA b s t r a c t A b s t r a c tA b s t r a c t
Cases of violent behavior during sleep have been reported in the literature. However, the incidence of violent behavior during sleep is not known. One epidemiological study showed that approximately 2% of the general population, predominantly males, presented violent behavior while asleep. In the present study, the authors describe clinical and medico-legal aspects involved in violent behavior investigation. Violent behavior refers to self-injury or injury to another during sleep. It happens most frequently following partial awakening in the context of arousal disorders (parasomnias). The most frequently diagnosed sleep disorders are REM behavior disorder and somnambulism. Violent behavior might be precipitated by stress, use of alcohol or drugs, sleep deprivation or fever.
K KK
KKeywords: eywords: eywords: eywords: eywords: Violence; Sleep disorders; Mental disorders; Somnambulism; Confusion; Night terrors; Polysomnography
1 Universidade Federal de São Paulo (UNIFESP, Federal University of São Paulo)
2 Universidade Federal de São Paulo (UNIFESP, Federal University of São Paulo) - Specialist in Sleep Medicine and Biology 3 Sleep Institute - Association for the Incentive Funding of Psychopharmacology (AFIP)
4 Technical University of Lisbon, Lisbon, Portugal 5 Stanford University, Stanford, California, USA
Correspondence Dalva Poyares
Rua Napoleão de Barros, 925 - Vila Clementino 04024-002 São Paulo, SP
Phone: (55 11) 5539-0155 Fax: (55 11) 5572-5092 E-mail: poyares@psicobio.epm.br
Violent behavior during sleep
Violência durante o sono
Dalva Poyares,
1Carlos Maurício Oliveira de Almeida,
2Rogerio Santos da Silva,
3Agostinho Rosa,
4I n t r o d u c t i o n I n t r o d u c t i o n I n t r o d u c t i o n I n t r o d u c t i o n I n t r o d u c t i o n
One question remains unanswered: are the reports below real cases of attempted murder or do they constitute a health problem? In this article, aspects involved in cases of violent behavior during sleep are discussed. Such behavior is defined as self-injury or injury to others during the sleep period. This commonly occurs during partial or incomplete awakening in the context of parasomnia. Violence is not a diagnosis but rather a behavior, which requires thorough and careful description, as well as precise quantification.
The prevalence of violence during sleep is not very well known. It has been reported to occur in 2% of the population, predominantly in males.1
There are many categories of violence: 1) innate (territorial or predatory); 2) defensive (reaction to restraint or perceived threat); 3) learned violence (exhibited by individuals who also present aggression or violent manifestations during a state of v i g i l a n c e o f f u l l w a k e f u l n e s s ) ; a n d 4 ) o t h e r f o r m s . Nevertheless, violent acts committed during sleep typically absolve the individual of any responsibility. Therefore, it is necessary to determine the level and nature of consciousness, as well as the degree of perception of reality during the violent act. To be legally responsible, an individual must be aware of his or her actions and have control over them.2 "Consciousness"
occurs along a continuum. An individual may be conscious, partially conscious, awakening or totally awake and conscious.
C a s e r e p o r t s C a s e r e p o r t s C a s e r e p o r t s C a s e r e p o r t s C a s e r e p o r t s C a s e 1 C a s e 1 C a s e 1 C a s e 1 C a s e 1
A 26-year-old Hispanic male, RC was recently married and the father of a three-month-old baby. The patient was arrested after throwing his son out of the window on the third floor of a building. Immediately after the occurrence, he rushed out of the apartment, mumbling, and ran down the stairs and into the street. His wife's screams from the 3rd floor window attracted the attention of neighbors and passers-by, who chased after the man and immobilized him on the ground. The police arrived promptly and arrested RC. The baby suffered mild inju-ries, since he fell onto an awning and then into a garden. The wife was not allowed to see her husband from the day he was arrested. Since RC had no memory of the event and claimed to have awoken when he was being beaten by assailants in the street, the public defender contacted the sleep center. The accused was so overwhelmed by the event that he stopped eating and became severely depressed.
C a s e 2 C a s e 2 C a s e 2 C a s e 2 C a s e 2
A 57-year-old Caucasian, GP was referred to the sleep clinic by a general clinician and was accompanied by his wife. In the previous week, his wife had been abruptly awakened during the night being strangled and attacked by GP. She only realized it was her husband when he said: "I am going to kill you, you...", while kicking the bed. She managed to disentangle herself, but GP continued to scream and beat the mattress, apparently unable to hear her pleas to stop. Some moments later, he turned over and went back to sleep. When she woke him up, he denied everything. His wife told the sleep specialist that she had not called the police because she believed her husband to be ill. However, she agreed to sleep in another room with the door locked.
G e n e r a l e v a l u a t i o n G e n e r a l e v a l u a t i o n G e n e r a l e v a l u a t i o n G e n e r a l e v a l u a t i o n G e n e r a l e v a l u a t i o n
It has been suggested that some legal aspects should be
observed by the specialist required to evaluate a certain case, such as: to conduct a thorough evaluation of the patient; to be impartial; to allow the medical report to be submitted to a review process; to make his testimonial available to lawyers of both parts.3
T h e a n a m n e s i s T h e a n a m n e s i sT h e a n a m n e s i s T h e a n a m n e s i sT h e a n a m n e s i s
The anamnesis should include a detailed description of the event and of the degree of amnesia, the family history of sleep disorders, previous medical records, social habits, use of drugs (prescribed or illicit) or alcohol, record of professional difficulties caused by sleep disorders, the frequency of the aggression and the stereotypical nature of the violence. Collection of the history should include an interview with the partner or family members. The current event and possible previous events must be investigated, including the time of night, the frequency and the degree of the accompanying amnesia. In addition, the age at onset of the disorder and the time correlation with traumatic events may also be useful data in the differential diagnosis. During the interview, the specialist should observe the attitude of the individual and his or her reaction to the event when fully awake. If possible, the current and previous events should be evaluated in terms of the relationships between the abnormal behavior and diurnal factors such as stress, sleep deprivation, alcohol consumption, drug use, fever and occurrence of other abnormal events.4-12
C l i n i c a l a n d l a b o r a t o r y e v a l u a t i o n C l i n i c a l a n d l a b o r a t o r y e v a l u a t i o nC l i n i c a l a n d l a b o r a t o r y e v a l u a t i o n C l i n i c a l a n d l a b o r a t o r y e v a l u a t i o nC l i n i c a l a n d l a b o r a t o r y e v a l u a t i o n
In all cases of violent behavior during sleep, the first course of action should be to perform a complete clinical examination, together with neurological and psychiatric evaluations. To that end, standardized questionnaires designed to assess sleep disorders and excessive daytime sleepiness.13-14 Complete
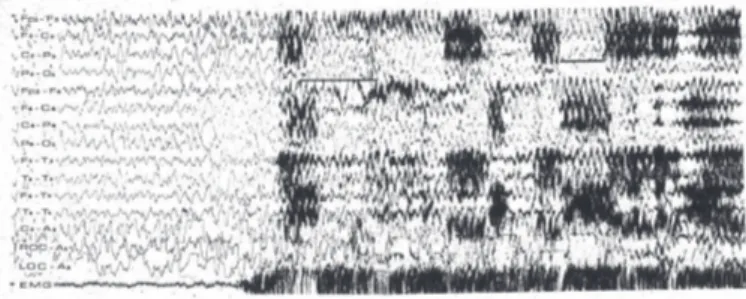
evaluation of sleep disorders, laboratory evaluation and other tests are also recommended for confirming the possible use of drugs and medication. Polysomnography may help to record the occurrence of abnormal phenomenon during sleep. However, in many cases, results will not be obtained for several days since the abnormal behavior may not express itself every day. When polysomnography is used, the minimum variables recorded should be the following: four electroencephalogram (EEG) channels (C3/A2, C4/A1, O1/A2 and O2/A1); chin electromyogram (EMG); electro-oculogram (EOG); modified V1 derivation electrocardiogram (ECG); respiratory parameters (expiratory flow through the nose and mouth, thoracic and abdominal respiratory effort, pulse oximetry); EMG of the an-terior tibial muscle and body position sensor. When available, actigraphy, which measures activity and rest, inferring the sleep-wake cycle with relative precision,15-16 may detect the
presence of abnormal behavior. The use of the actigraph is suggested for at least seven consecutive days. Finally, depending on the sleep disorder, additional tests may be needed, especially the Multiple Sleep Latency Test,17 which
measures the tendency for sleep during the day. Nocturnal EEG measurement in the home may need to be repeated in order to complement the diagnosis.
T TT
TTe s t e v a l u a t i o ne s t e v a l u a t i o ne s t e v a l u a t i o ne s t e v a l u a t i o ne s t e v a l u a t i o n
S l e e p d i s o r d e r s a s s o c i a t e d w i t h " a u t o m a t i s m s " S l e e p d i s o r d e r s a s s o c i a t e d w i t h " a u t o m a t i s m s " S l e e p d i s o r d e r s a s s o c i a t e d w i t h " a u t o m a t i s m s " S l e e p d i s o r d e r s a s s o c i a t e d w i t h " a u t o m a t i s m s " S l e e p d i s o r d e r s a s s o c i a t e d w i t h " a u t o m a t i s m s " 1 . A r o u s a l d i s o r d e r s
1 . A r o u s a l d i s o r d e r s 1 . A r o u s a l d i s o r d e r s 1 . A r o u s a l d i s o r d e r s 1 . A r o u s a l d i s o r d e r s
Arousal disorders, which are included in NREM sleep parasomnias, seem to be more commonly associated with violent behavior.
1) Confusional arousal or "sleep drunkenness": 1) Confusional arousal or "sleep drunkenness": 1) Confusional arousal or "sleep drunkenness": 1) Confusional arousal or "sleep drunkenness": 1) Confusional arousal or "sleep drunkenness": This condition usually occurs during slow-wave sleep (stages 3 and 4 of NREM sleep) and may occur, more rarely, during stage 2. It is characterized by mental confusion (during and after awakening), slowness of thought and time-space disorientation. The patient may present slow movements and i n c o m p l e t e r e s p o n s i v e n e s s t o e x t e r n a l s t i m u l i .5 , 1 8
Incomprehensible speech and moaning may occur, as well as automatic behavior, such as touching clothes, pinching or pulling the skin, "throwing" oneself out of bed and kicking violently. Confusional arousal may be accompanied by other parasomnias. Retrograde amnesia for the event may occur, being more common in people who sleep more deeply. The EEG shows slow alpha rhythm or more rapid theta activity (7 to 9 Hz) during the crisis, and low reactivity to light is observed. The following correlated factors may be observed: respiratory sleep disorders; periodic limb movements; gastroesophageal reflux; stress during the day; and anxiety. It may be caused by fever or may follow the ingestion of alcohol or hypnotics.19
2 ) S l e e p w a l k i n g : S l e e p w a l k i n g ( o r s o m n a m b u l i s m ) 2 ) S l e e p w a l k i n g : S l e e p w a l k i n g ( o r s o m n a m b u l i s m ) 2 ) S l e e p w a l k i n g : S l e e p w a l k i n g ( o r s o m n a m b u l i s m ) 2 ) S l e e p w a l k i n g : S l e e p w a l k i n g ( o r s o m n a m b u l i s m ) 2 ) S l e e p w a l k i n g : S l e e p w a l k i n g ( o r s o m n a m b u l i s m ) is characterized by recurrent episodes of complex abnormal behavior during a partial arousal from slow-wave sleep. The patient may get out of bed and move about in a state of confusion and disorientation, frequently causing self-injury. The episode may be preceded by a scream or by a night terror episode, with significant autonomic hyperactivity such as an increase in cardiac and respiratory frequency. In this case, movements may be much more abrupt. Eventually, the patient may run, beat the walls and windows, or even leave the house. Responsiveness is reduced, although the patient may speak or scream. Behaviors which are more elaborate, such as driving, rarely occur. Reactions, such as fleeing or defense against a threat may occur. Any attempt at restraint generally leads the patient to react violently and to attack, using the hands or any object available. Although not remembering the attack, the patient may have a memory of imminent danger, personal threats or threats against family or property.
Moldofsky et al20 compared sleepwalkers who presented
violent behavior during sleep to those who did not and found that the following characteristics are more common in patients presenting violent behavior: male gender; family of origin problems; history of sexual abuse; Hamilton scale > 24; family history of sleepwalking or night terrors; unorganized sleep schedule, with more chaotic sleep-wake cycles; and history of substance abuse. The categories male gender, unorganized sleep-wake habits and history of substance abuse presented 18% sensitivity and 100% specificity in predicting violent behavior in the sleepwalkers studied. In addition, these patients presented a reduction in stage 4 NREM sleep, as well as in alpha periods of activity and history of recurrent episodes of somnambulism or night terrors. The most common alterations in EEG in the polysomnographic record are lower delta activity (slow waves); higher sleep fragmentation index, tachycardia and tachypnea. In addition, weak reactivity to light and lack of epileptiform activity are observed during vigilance or sleep. Somnambulism episodes may be facilitated by other factors that cause sleep to be fragmented or superficial. These include
respiratory sleep disorders, periodic limb movements and gastroesophageal reflux. In addition, these episodes may occur more frequently when accompanied by daytime stress, anxiety, fever and post-traumatic stress disorder.12,21-27 Guilleminault
et al.28 found a greater incidence of violent behavior during
sleep in patients presenting somnambulism, whereas Mahowald and Schenck29 reported a greater incidence in
patients with REM sleep behavior disorder. 3 ) R E M s l e e p b e h a v i o r d i s o r d e r : 3 ) R E M s l e e p b e h a v i o r d i s o r d e r : 3 ) R E M s l e e p b e h a v i o r d i s o r d e r : 3 ) R E M s l e e p b e h a v i o r d i s o r d e r :
3 ) R E M s l e e p b e h a v i o r d i s o r d e r : T h i s c o n d i t i o n i s characterized by a loss of skeletal muscle atonia, which is physiologically normal during this sleep stage, and by the relationship between dream and REM sleep. There is, therefore, disequilibrium between mental activity of the dream and the lack of motor inhibition associated with the dream content, causing the individual to "act out" the dream. In addition, these patients normally report intense and vivid dreams, often with an aggressive content, in some cases combined with semi-intentional, relatively coordinated movements, including activities such as running. Motor activity may affect the partner and result in bruises, laceration, fracture and direct trauma. In the anamnesis, a history of agitated dream is observed. This may be an everyday occurrence, normally happening near the end of the sleep cycle, when REM sleep is predominant. This condition may be accompanied by some neurological conditions such as olivopontocerebellar degeneration, Parkinson's disease, multisystem atrophy, progressive supranuclear paralysis and narcolepsy. Since noradrenalin is involved in the regulation of muscle tonus during REM sleep, REM sleep behavior disorder may be precipitated by the use of noradrenalin reuptake inhibitors and subsequently corrected when the drug is discontinued. It is more common in men and in elderly individuals, with an estimated prevalence of 0.5% of the population. The diagnosis is well demonstrated through polysomnography combined with video monitoring of abnormal behavior. It has been shown that muscle activity increases considerably during the REM sleep stage, possibly combined with frequent and rapid movements of the limbs or the whole body, as well as with complex or violent movements.
4) Overlap syndrome: 4) Overlap syndrome: 4) Overlap syndrome: 4) Overlap syndrome:
4) Overlap syndrome: This syndrome is characterized by the combination of NREM sleep parasomnias (confusional arousals, somnambulism or night terrors) and REM sleep behavior disorder. Abnormal behavior may occur during slow-wave sleep and during REM sleep, either on the same night or on alternate nights.
5) Nocturnal complex partial crises: 5) Nocturnal complex partial crises: 5) Nocturnal complex partial crises: 5) Nocturnal complex partial crises:
5) Nocturnal complex partial crises: These crises may originate in the frontal lobe or, less often, in the mesiotemporal lobe and may be correlated with dominant autosomal inheritance. During frontal lobe crises, complex motor behavior
may occur. Since the initial description of these crises and despite the lack of ictus during abnormal behavior, episodic nocturnal wandering has been considered a manifestation of the crisis, being more common in men.30 Interictal epileptiform
activity may be seen in the EEG. Complex behavior may be observed at any time of the night, although it is more common during the first half of the sleep cycle and in stage 2 of NREM sleep. In addition, the behavior may be quite stereotyped. Normally, the amnesia for the event is complete. Confusion and disorientation frequently occur.31-34
6) It has been proposed that sexual aggression 6) It has been proposed that sexual aggression 6) It has been proposed that sexual aggression 6) It has been proposed that sexual aggression 6) It has been proposed that sexual aggression is a special form of violence during sleep. Patients feel embarrassed and are reluctant to admit such behavior. In addition, the partner may also be reluctant to discuss the problem, which will remain undiagnosed if not investigated properly. This parasomnia may have medico-legal implications.3 In a study
by Guilleminault et al, 11 cases were documented (4 women and 8 men). Aggressive sexual behavior included: disrobing; fondling/molesting the partner; attempting to disrobe the partner; attempts at forced intercourse. The authors found this type of behavior to present in varied forms, including forcefulness and violence, depending on the individual and the situation, possibly leading to bruises and other evidence of aggression. They also reported that the attempt may be interrupted abruptly, with no intercourse, or may lead to forced penetration, with or without ejaculation in men. In the case of women, self-stimulation signs were observed. Amnesia for the event may also be observed, which means that if the patient is awakened during the act, he may deny the attempt and reject the response of the partner. The diagnoses documented were: somnambulism, REM sleep behavior disorder and fron-tal lobe seizures.
T h e r a p e u t i c m e a s u r e s T h e r a p e u t i c m e a s u r e s T h e r a p e u t i c m e a s u r e s T h e r a p e u t i c m e a s u r e s T h e r a p e u t i c m e a s u r e s
In order to protect patient and partner, security measures are indicated.5,11,35 To that end, separate beds or bedrooms
may be recommended, as well as sleeping on the ground floor, in a large bedroom; locking the windows or covering them with heavy drapes; removing mirrors and furniture from the room; removing sharp objects and objects with sharp corners. In more severe cases, the patient should sleep in a sleeping bag closed with a zip. Aggravating factors, such as everyday stress, anxiety and inappropriate sleep habits should be treated to prevent sleep deprivation. Benzodiazepines, psychotherapy, relaxation and measures to improve sleep hygiene may be indicated. In addition, accompanying clinical conditions, such as: irregular sleep-wake cycle, depression, respirator y sleep disorders, narcolepsy, periodic limb movements, and neurological diseases, should be treated.36-42
Symptomatic treatment using medication may be required. In this case, it is recommended to use low doses of clonazepam, which can be increased according to therapeutic response. In rare cases, other benzodiazepines may be indicated. In the case of confirmed seizures, antiepileptics are used.
D i s c u s s i o n D i s c u s s i o n D i s c u s s i o n D i s c u s s i o n D i s c u s s i o n Case 1: Case 1: Case 1: Case 1:
Case 1: The patient known as RC had suffered from sleepwalking since the age of 6. The crises became more frequent in times of stress, improving in calmer times. The episodes were typically limited, characterized by calm and simplistic behavior, and the patient returned to bed when asked by his wife. Prior to the event in question, RC and his family
were at the epicenter of an earthquake. His apartment was demolished and the family slept in a tent for two weeks. The aftershocks were frightening, and RC experienced an increase in the frequency of his parasomnia, presenting a number of confusional arousals every night and suffering from sleep deprivation. After the family had moved to a new apartment, his wife realized that RC was more anxious, and that the sleepwalking events were occurring every night. In describing the event, RC stated that he had only a vague memory of the occurrence but recalled that his son was in danger and needed help. The clinical evaluation by EEG and computed tomography of the brain provided no additional evidence. The psychiatric evaluation indicated the presence of moderate anxiety. Polysomnography showed prolonged sleep latency and sleep fragmentation not explained by any other sleep disorder. There was a slow-wave sleep period which was abruptly interrupted. This interruption was followed by motor behavior, such as getting out of bed, combined with confusion and mumbling. The patient did not answer the intercom phone when the technician called but complied when the technician entered the room and ordered him back to bed. The patient immediately entered stage 2 NREM sleep. He was awakened after 10 minutes so that his memory of the episode could be evaluated. The patient presented complete amnesia for the event when fully conscious. The court accepted the event as a case of sleepwalking and decided that medical treatment was necessary. Although the charges were dropped, RC had spent three months in prison prior to this ruling.
Case 2: Case 2:Case 2:
Case 2:Case 2: This patient presented a history of abnormal behavior during sleep for the preceding five years. His wife reported that usually during the second half of the night he would make noises, laugh and sometimes speak in complete sentences. On other occasions, the patient moved irregularly in bed during the night, flailing his arms and legs and thereby bruising his wife. The patient remembered dreaming about golf games (he often played golf), during which he might make a great shot and speak enthusiastically with friends about the game. When he drank alcohol, the behavior worsened. Despite the bruises and agitated sleep, neither of them mentioned the problem to the physician. Clinical evaluation of the patient showed mild obesity (body mass index of 26.6 kg/m2), arteri-al hypertension and dyslipidemia. The wife reported that the patient frequently snored, but there was no mention of sleep apnea. The patient denied having any other symptom of sleep disorder. The EEG was normal. Polysomnography showed REM sleep behavior disorder, with a characteristic increase in the amplitude for muscular activity during REM sleep. The videotape showed extensive movements of the arms. Once awake, the p a t i e n t s t a t e d t h a t h e h a d d r e a m e d o f p u s h i n g h i s granddaughter on a swing. At the time of the aggression against his wife, there had been a robbery in his neighborhood, and he was seriously concerned about his house and family. The patient had many dreams in which he confronted the robbers. This dream recurred on the night of the aggression (he dreamed that he was fighting). The long interval between the first occurrence of the symptoms reported and its eventual report is not rare, since non-violent abnormal behaviors during sleep are not reported. In addition, violent behavior may be denied by the patient, who presents amnesia for the event.
R e f e r ê n c i a s R e f e r ê n c i a s R e f e r ê n c i a s R e f e r ê n c i a s R e f e r ê n c i a s
1 . 1 . 1 . 1 .
1 . Ohayon MM, Caulet M, Priest RG. Violent behavior during sleep. J Clin Psychiatry. 1997;58(8):369-76; quis 377.
2 . 2 . 2 . 2 .
2 . Lacerda P. Código Civil Brasileiro: lei 3071 de 1º de janeiro de 1916. Rio de Janeiro: Jacintho Ribeiro dos Santos; 1916.
3 . 3 . 3 . 3 .
3 . Guilleminault C, Moscovitch A, Yuen K, Poyares D. Atypical sexual behavior during sleep. Psychosom Med. 2002;64(2):328-36.
4 . 4 . 4 . 4 .
4 . Guilleminault C, Palombini L, Pelayo R, Chervin RD. Sleepwalking and sleep terrors in prepubertal children: what triggers them? Pediatrics. 2003;111(1):e17-25.
5 . 5 . 5 . 5 .
5 . Broughton RJ. Behavioral Parasomnias. In: Chokroverty S. Clinical companion to sleep medicine disorders. 2ª ed. New York: Butterworth-Heinemann; 1999. p. 635-60.
6 . 6 . 6 . 6 .
6 . Gastaut H, Broughton R. A clinical and polygraphic study of episodic phenomena during sleep. In: Wortis J. Recent advances in biological psychiatry. New York: Grune and Stratton; 1965. p. 197.
7 . 7 . 7 . 7 .
7 . Negi A, Thoung D, Dabbous F. Nightmares with topical beta-blocker. Eye. 2000;14(Pt 5):813-4.
8 . 8 . 8 . 8 .
8 . Pradalier A, Guittard M, Dry J. [Propranolol and somnambulism]. Therapie. 1986;41(4):318. French.
9 . 9 . 9 . 9 .
9 . Landry P, Warnes H, Nielsen T, Montplaisir J. Somnambulistic-like behaviour in patients attending a lithium clinic. Int Clin Psychopharmacol. 1999;14(3):173-5.
1 0 . 1 0 . 1 0 . 1 0 .
1 0 . Huapaya LV. Seven cases of somnambulism induced by drugs. Am J Psychiatry. 1979;136(7):985-6.
1 1 . 1 1 . 1 1 . 1 1 .
1 1 . Rosen G, Mahowald MW, Ferber R. Sleepwalking, confusional arousal and sleep terrors in the child. In: Feber R, Krieger MH. Principles and practice of sleep medicine in child. Philadelphia: Saunders; 1995. p. 99-106.
1 2 . 1 2 . 1 2 . 1 2 .
1 2 . Kales JD, Kales A, Soldatos CR, Chamberlin K, Martin ED. Sleepwalking and night terrors related to febrile illness. Am J Psychiatry. 1979;136(9):1214-5.
1 3 . 1 3 . 1 3 . 1 3 .
1 3 . Hoddes E, Dement WC, Zarcone V. The history and use of The Stanford Sleepiness Scale [abstract]. Psychophysiology. 1972;9(2):150 .
1 4 . 1 4 . 1 4 . 1 4 .
1 4 . Johns MW. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14(6):540-5.
1 5 . 1 5 . 1 5 . 1 5 .
1 5 . Keenan SA. Polysomnographic technique: an overview. In: Chokroverty S. Clinical companion to sleep medicine disorders. 2ed. New York: Butterworth-Heinemann; 1999. p. 151-69.
1 6 . 1 6 . 1 6 . 1 6 .
1 6 . Sadeh A, Hauri PJ, Kripke DF, Lavie P. The role of actigraphy in the evaluation of sleep disorders. Sleep. 1995;18(4):288-302.
1 7 . 1 7 . 1 7 . 1 7 .
1 7 . Carskadon MA, Dement WC, Mitler MM, Roth T, Westbrook PR, Keenam S. Guidelines for the Multiple Sleep Latency Test (MSLT): a standard measure of sleepiness. Sleep. 1986;9(4):519-24.
1 8 . 1 8 . 1 8 . 1 8 .
1 8 . Broughton R. Sleep disorders: disorders of arousal? Enuresis, somnambulism, and nightmares occur in confusional states of arousal, not in "dreaming sleep". Science. 1968;159(819):1070-8.
1 9 . 1 9 . 1 9 . 1 9 .
1 9 . Guilleminault C, Poyares D, Aftab FA, Palombini L, Abat F. Sleep and wakefulness in somnambulism: a spectral analysis study. J Psychosom Res. 2001;51(2):411-6. Erratum in: J Psychosom Res. 2001;51(4):621.
2 0 . 2 0 . 2 0 . 2 0 .
2 0 . Moldofsky H, Gilbert R, Lue FA, MacLean AW. Sleep-related violence. Sleep. 1995;18(9):731-9.
2 1 . 2 1 . 2 1 . 2 1 .
2 1 . Laberge L, Tremblay RE, Vitaro F, Montplaisir J. Development of parasomnias from childhood to early adolescence. Pediatrics. 2000;106(1 Pt 1):67-74.
2 2 . 2 2 . 2 2 . 2 2 .
2 2 . Woodward SH, Leskin GA, Sheikh JI. Movement during sleep: association with posttraumatic stress disorder, nightmares and comorbid panic disorder. Sleep. 2002;25(6):681-8.
2 3 . 2 3 . 2 3 . 2 3 .
2 3 . Glod CA, Teicher MH, Hartman CR, Harakal T. Increased nocturnal activity and impaired maintenance in abuse children. J Am Acad Child Adolesc Psychiatric. 1997;36(9):1236-43.
2 4 . 2 4 . 2 4 . 2 4 .
2 4 . Ghaemi SN, Irizarr y MC. Parasomnias as neuropsychiatric complication of electrical injury. Psychosomatics. 1995;36(4):416.
2 5 . 2 5 . 2 5 . 2 5 .
2 5 . Kravitz M, McCoy BJ, Tompkins DM, Daly W, Mulligan J, McCauley RL, et al. Sleep disorders in children after burn injury. J Burn Care Rehabil. 1993;14(1):83-90.
2 6 . 2 6 . 2 6 . 2 6 .
2 6 . Espa F, Dauvilliers Y, Ondze B, Billiard M, Besset A. Arousal reactions in sleepwalking and night terrors in adults: the role of respiratory events. Sleep. 2002;25(8):871-5.
2 7 . 2 7 . 2 7 . 2 7 .
2 7 . Ohayon MM, Guilleminault C, Priest RG. Night terrors, sleepwalking, and confusional arousals in the general population: their frequency
and relationship to other sleep and mental disorders. J Clin Psychiatry. 1999;60(4):268-76; quiz 277.
2 8 . 2 8 .2 8 . 2 8 .
2 8 . Guilleminault C, Moscovitch A, Leger D. Forensic sleep medicine: nocturnal wandering and violence. Sleep. 1995;18(9):740-8.
2 9 . 2 9 .2 9 . 2 9 .
2 9 . Mahowald MW, Schenck CH. Complex motor behavior arising during the sleep period: forensic science implications. Sleep. 1995;18(9):724-7.
3 0 . 3 0 .3 0 . 3 0 .
3 0 . Pedley TA, Guilleminault C. Episodic nocturnal wanderings responsive to anticonvulsant drug therapy. Ann Neurol. 1977;2(1):30-5.
3 1 . 3 1 .3 1 . 3 1 .
3 1 . Chokroverty S, Christine Q. Sleep and epilepsy. In: Chokroverty S. Clinical companion of sleep medicine disorders. 2 ed. New York: Butterworth-Heinemann; 1999. p. 697-727.
3 2 . 3 2 .3 2 . 3 2 .
3 2 . Kellaway P. Sleep and epilepsy. Epilepsia.1985;26(Suppl 1):S15-30.
3 3 . 3 3 .3 3 . 3 3 .
3 3 . Broughton RJ. Polysomnography: principles and aplications in sleep and arousal disorders. In: Niedermeyer E. Electroencephalography: basic principles, clinical applications and related fields. 4th edition. Lippincott: Williams & Wilkins; 1999. p. 858-95.
3 4 . 3 4 .3 4 . 3 4 .
3 4 . Pedley TA. Differential diagnosis of episodic symptoms. Epilepsia. 1983;24(Suppl 1):S31-44.
3 5 . 3 5 .3 5 . 3 5 .
3 5 . Broughton R, Shimizu T. Dangerous behaviors by night. In: Sharpiro C, Smith AM. Forensic aspects of sleep. New York: John Wiley & Sons; 1997. p. 216.
3 6 . 3 6 .3 6 . 3 6 .
3 6 . Wills L, Garcia J. Parasomnias: epidemiology and management. CNS Drugs. 2002;16(12):803-10.
3 7 . 3 7 .3 7 . 3 7 .
3 7 . Mahowald MW, Schenck CH. Parasomnias including the restless legs syndrome. Clin Chest Med. 1998;19(1):183-202.
3 8 . 3 8 .3 8 . 3 8 .
3 8 . Hening WA, Allen R, Walters AS, Chokroverty S. Motor function and dysfunction of sleep. In: Chokroverty S. Clinical companion of sleep medicine disorders. 2 ed. New York: Butterwor th-Heinemann; 1999. p. 441-507.
3 9 . 3 9 .3 9 . 3 9 .
3 9 . Barthlen GM, Stacy C. Dyssomnias, parasomnias and sleep disorders associated with medical and psychiatric diseases. Mt Sinai J Med. 1994;61(2):139-59.
4 0 . 4 0 .4 0 . 4 0 .
4 0 . Garcia-Borreguero D, Larrosa O, Bravo M. Parkinson's disease and sleep. Sleep Med Rev. 2003;7(2):115-29.
4 1 . 4 1 .4 1 . 4 1 .
4 1 . Lilie JK, Lahmeyer H. Psychiatric management of sleep disorders. Psychiatr Med. 1991;9(2):245-60.
4 2 . 4 2 .4 2 . 4 2 .