w w w . r b o . o r g . b r
Original
Article
Parsonage–Turner
syndrome
夽
Ricardo
Barreto
Monteiro
dos
Santos
∗,
Saulo
Monteiro
dos
Santos,
Flávio
José
Câmara
Carneiro
Leal,
Otávio
Gomes
Lins,
Carmem
Magalhães,
Ricardo
Bruno
Mertens
Fittipaldi
TraumatologyService,HospitaldasClínicas,UniversidadeFederaldePernambuco,Recife,PE,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received3September2013
Accepted5June2014
Availableonline17April2015
Keywords:
Neuritisofthebrachialplexus
Shoulder Electromyography
a
b
s
t
r
a
c
t
Objective:To describe the clinical, electrophysiological and imaging findings from
Parsonage–Turnersyndromeandevaluatetheresultsfromconservativetreatment.
Methods:EightcaseswerestudiedbetweenFebruary2010andFebruary2012,witha
min-imumfollow-upofoneyear(meanof14months). Allthe patientsansweredaclinical
questionnaireandunderwentfunctionalevaluationusingtheConstantandMurleyscore.
Afterclinicalsuspicionwasraised,anelectromyographyexaminationwasperformedto
confirmthediagnosis.
Results:Eightpatients(meanageof29years)wereevaluated.Therightsidewasaffectedin
70%ofthecases,andthedominantsidein80%ofthecases.Allthepatientsreportedthat
theirshoulderpainhadstartedsuddenly,lastingfromonetofivedaysinsixcasesandup
to15daysintwocases.Inthreecases,severeatrophyofthedeltoidmusclewasobserved.
Hypotrophyofthesupraspinatusandinfraspinatusmuscleswasobservedinthreecases.A
wingedscapulawasobservedinthetworemainingcases.Electromyographydemonstrated
involvementofthelongthoracicnerveintheselasttwocasesandconfirmedthe
involve-mentoftheaxillaryandsuprascapularnervesintheremainingsixcases.Themeanscoreon
theConstantandMurleyscalewas96attheendoftheconservativetreatmentwith
non-steroidalanti-inflammatorydrugsandphysiotherapy.Sixoftheeightpatientspresented
goodrecoveryofmusclestrength.
Conclusions:Inthemajorityofthecases,thefunctionalrecoverywasgood,althoughmuscle
strengthwasnotcompletelyrestoredinsomeofthem.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora
Ltda.Allrightsreserved.
Síndrome
de
Parsonage–Turner
Palavras-chave:
Neuritedoplexobraquial
r
e
s
u
m
o
Objetivo:Descrever osachados clínicos, eletrofisiológicosede imagemna síndrome de
Parsonage–Turnereavaliarosresultadosdotratamentoconservador.
夽
WorkdevelopedattheTraumatologyService,HospitaldasClinicas,FederalUniversityofPernambuco,Recife,PE,Brazil.
∗ Correspondingauthor.
E-mail:ricardobms@hotmail.com(R.B.MonteirodosSantos).
http://dx.doi.org/10.1016/j.rboe.2015.04.002
Ombro Eletromiografia
Métodos: Foramestudadosoitocasosentrefevereirode2010efevereirode2012,com
segui-mentomínimodeumano(médiade14meses).Todosospacientesforamsubmetidosao
questionárioclínicoeavaliadosfuncionalmentecomoescoredeConstanteMurley.Após
asuspeitaclínicaoexamedeeletroneuromiografiafoifeitoparaconfirmac¸ãodiagnóstica.
Resultados: Oitopacientes(médiade29anos)foramavaliados.Oladodireitofoiacometido
em70%doscasoseeraodominanteem80%.Todosospacientesrelataramuminíciosúbito
dedornoombro,comdurac¸ãodeumacincodiasemseiscasosedeaté15diasemdoiscasos.
Emtrêscasosfoiobservadaatrofiaseveradomúsculodeltoide.Hipotrofiadosmúsculos
supraespinhaleinfraespinhalfoiobservadaemtrêscasos.Escápulaaladafoiobservadaem
doiscasosrestantes.Aeletromiografiademonstrouenvolvimentodonervotorácicolongo
nessesdoisúltimoscasoseconfirmouoenvolvimentodosnervosaxilare
supraescapu-larnosseiscasosrestantes.Apontuac¸ãomédianaescaladeConstanteMurleyfoide96
nofimdotratamentoconservadorcommedicamentosanti-inflamatóriosnãoesteroidese
fisioterapia.Seisdosoitopacientesapresentaramboarecuperac¸ãodaforc¸amuscular.
Conclusão: Namaioriadoscasosarecuperac¸ãofuncionalfoiboa,emboraaforc¸amuscular
nãotenhasidocompletamenterestauradaemalgunsdeles.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier
EditoraLtda.Todososdireitosreservados.
Introduction
Parsonage–Turnersyndrome(PTS)isalsonamedacute
idio-pathic brachial neuritis, paralytic neuritis of the brachial
plexus, cryptogenic brachial neuropathy and scapular belt
syndrome.Thefirstrecordsofthissyndromedatefrom1887,
describedbyDreschfeld,andthiswasfollowedbymanyother
reports: Feinberg1 (1897), Bramwell and Struthers2 (1903),
Wyburn-Mason3(1941),Burnard4(1942)andSpillane5(1943).
However,theclinical characteristicsofthis syndromewere
onlyfullydescribedin1948,fromaseriesof136casesreported
byParsonageandTurner.Theseauthorsnamedit“scapular
beltsyndrome”.6
Thisisapainfulnon-traumaticdisorder thataffectsthe
scapularbelt.Clinically,thepatientpresentsapainful
condi-tionwithlocalizedupsurgesintheshoulderthatmaylastfor
somehoursoruptotwotothreeweeks,withspontaneous
improvement.Afterthepainfulcondition,muscleweakness
appears,alongwithparalysisandatrophyoftheinnervated
musculatureinthesegmentaffected.7 Topographically,this
neurologicallesionimpairstheperipheralnervesorpartof
thebrachialplexus.Inadditiontothemotorrepercussions,
theremaybesensorylosses.
Diagnosingthediseasemaygiverisetocertainanxieties
bothforthe attendingphysicianandforthe patient, since
some conditions with similar characteristics may be
con-foundedwithPTSandmayneedtoberuledout inmaking
the differential diagnosis.These conditions includerotator
cuff tears,calcareous tendinitis, adhesive capsulitis,
cervi-cal spondylopathy and neurological abnormalities such as
compressionoftheperipheralnerve,acutepoliomyelitisand
lateralamyotrophicsclerosis.However,thediagnosisbecomes
probablewhen spontaneousimprovement ofthe pain and
progressionofmuscleweaknessareobserved.
Theprecisecauseisunknown,butithasbeenattributedin
theliteraturetoviralinfectionsandautoimmuneprocesses,8,9
such as after immunization. There are also reports of
hereditary forms with specific mutations10 or even
occur-rences after strenuous physical exercise.11,12 Some viral
agents have been correlated with PTS, such as: smallpox,
fever, typhoid, influenza, coxsackievirus, parvovirus B19,
cytomegalovirus and human immunodeficiency virus, and
alsoBorreliaburgdorferi.8,13–16 Thereisstrongevidenceofan
association withviral infections,sincethere are reportsin
theliteratureofepidemicoutbreaksinisolatedpopulations,
suchasonethatoccurredinanindigenouspopulationinthe
southwesternUnitedStates,witheightcasesofPTS.7
Theincidencewasfoundtobe1.64casesper100,000
inhab-itants, inthe populationofMinnesota, UnitedStates, with
occurrences predominantly betweenthe third and seventh
decadesoflife.17,18Menaremoreaffectedthanwomen,with
aratioofbetween2:1and11.5:1.11Theprognosisisgoodin
mostcases,giventhatPTSisself-limitingandhasalow
recur-rencerate.11Thetreatmentisgenerallysuccessful,withuseof
analgesicsandphysiotherapyinordertomaintaintherange
ofmotionandstrengthenmuscles.
Theobjectiveofthisstudywastodescribetheclinical
char-acteristicsofPTSandevaluatetheresultsfromconservative
treatment.
Materials
and
methods
EightcasesofPTSthatwerediagnosedbetweenFebruary2010
and February2012werestudiedprospectively.Thepatients
were followed up fora minimumofone year (meanof 14
months). All the patients were asked to answer a clinical
questionnaireontheirsymptomsandunderwentaphysical
examinationtoassessfunction.Attheendofthetreatment,
allthepatientsweregradedusingtheConstantandMurley
score.19
AftertheclinicalsuspicionofPTSwasraised,allofthese
patientsunderwent electroneuromyographyexaminationin
ordertoregistertheperipheralnervethatwasaffectedand
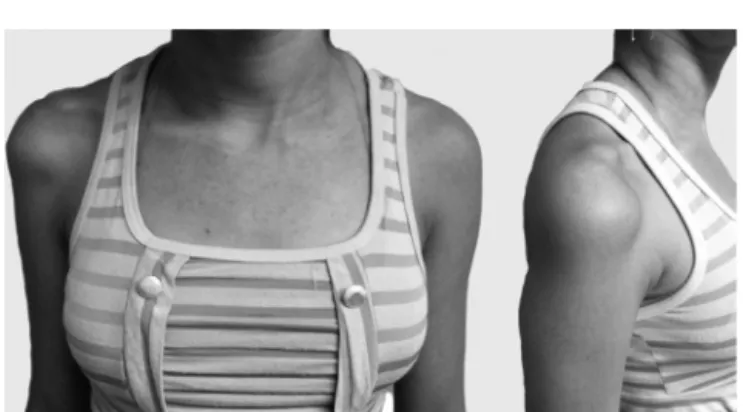
Fig.1–Fifteenyearsandthreemonthsafterthestartofthe symptoms.Notetheatrophyofthedeltoidmuscleinthe rightshoulder.
ofrulingoutassociatedconditionsandmakingadifferential
diagnosis,radiographyandmagneticresonanceexaminations
wereused.Theinclusioncriteriawerethatthepatentsneeded
to have a history of acute shoulder pain with paresis or
hypotrophy inthe scapular belt. Patients with histories of
trauma,previousshouldersurgery,rotatorcufftearsor
adhe-sivecapsulitiswereexcluded.Thisstudywasapprovedbythe
ethicscommittee.
Results
Eightpatientswereevaluated:threefemalesandfivemales.
Theirmeanagewas29years(rangefrom15to41).Theright
sidewasaffectedin70%ofthecasesandthedominantside
in80%(Table1).
Allthepatientsstudiedreportedduringthehistory-taking
thattheyhadexperienceasuddenconditionofshoulderpain
thatlastedforanaverageofonetofivedays.Intwocases,the
painlastedfor15days.Inthreecases,therewasspontaneous
remissionofthepainfulconditionwithout anyuseof
non-steroidalanti-inflammatorydrugs(NSAIDs).Insevencases,
remissionoccurredthroughuseofNSAIDsandanalgesicsthat
wereprescribedbydoctorsattheemergencyservice.
Inthephysicalexamination,whichwasperformedoneight
patients,threecasespresentedintenseatrophyintheareaof
thedeltoidmuscleandonecaseshowedhypoesthesiainthe
sensoryareaoftheaxillarynerve(Fig.1).Threecasesshowed
musclehypotrophyinthesupraspinousandinfraspinous
fos-sae,withpositiveJobetests,whichwereusedtoevaluatethe
functioningofthesupraspinatus.Theremainingtwocases
showedwingedscapulae,whichweremoreevidentwhenthe
patientsusedforcetopushagainstawall(Fig.2).
Electroneuromyographyexaminationswereperformedon
all the patients in order to confirm the diagnosis. All
of these examinations demonstrated peripheral
denerva-tion (potential for prolonged action and latency). In one
case (patient 4), a magnetic resonance examination was
performed on the shoulder, which showed hypersignal
withT2 weightingand atrophy ofthe deltoidmusculature
(Fig.3).
A physiotherapeutic rehabilitationprogram was started
justafterthediagnosishadbeenmade.Theprotocolconsisted
Fig.2–Patientwithright-sidewingedscapula,resulting fromimpairmentofthelongthoracicnerve.
of analgesic electrotherapy with TENS in association with
deepthermaltherapyorcryotherapyduringthepainfulphase,
kinesiotherapy to maintainand gain range ofmotionand,
when gradesclosetonormality werereached,isometric or
resistanceexerciseswerestartedfortheentirescapularbelt.
Functionalelectricalstimulation(FES)wasalsousedwiththe
aimofincreasingmuscletonus.
Allthepatientspresentedimprovementsinpain,strength
andmuscletrophism(Fig.4)overthecourseofthefollow-up.
TheConstantand Murleyscoresobtainedwerebetween94
and100points,withameanof96.37pointsattheendofthe
follow-up(Table2).Sixoftheeightpatientstreatedpresented
FH 25 head 2 cm
3 cm
FH 13 feet
L L
A
A
B
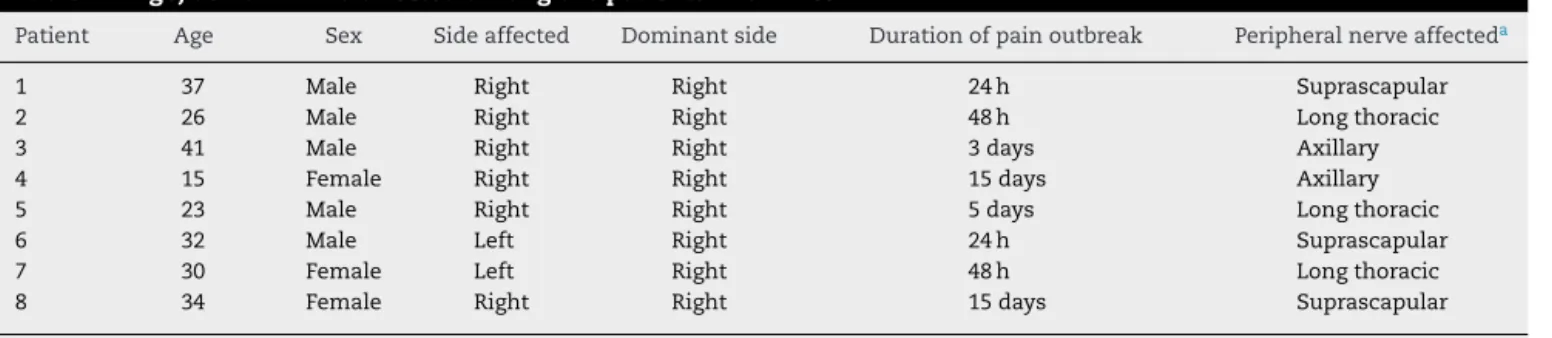
Table1–Age,sexandlimbaffectedamongthepatientswithPTS.
Patient Age Sex Sideaffected Dominantside Durationofpainoutbreak Peripheralnerveaffecteda
1 37 Male Right Right 24h Suprascapular
2 26 Male Right Right 48h Longthoracic
3 41 Male Right Right 3days Axillary
4 15 Female Right Right 15days Axillary
5 23 Male Right Right 5days Longthoracic
6 32 Male Left Right 24h Suprascapular
7 30 Female Left Right 48h Longthoracic
8 34 Female Right Right 15days Suprascapular
Source:researchdata.
a Basedonclinicalexaminationandcomplementaryelectroneuromyographyexamination.
Fig.4–PatientwithPTSintherightshoulder,affectingthe axillarynerve.(A)Atrophyintheareaofthedeltoid: appearanceatthetimeofthediagnosis.(B)Appearance afterthreemonthsofphysiotherapeuticrehabilitation.
fullrecoveryofmuscle strength.Intheother twopatients,
althoughmusclehypotrophycouldstillbeseen,thisdidnot
haveanyrepercussionontheirdailyandsportsactivities.
Discussion
The etiology of PTS is not well defined, but it has been
attributedtoviral infectionsand autoimmunereactions.In
someclinicalreports,beforethesymptomsappeared,aperiod
offeverorinfectionoftheupperairwaysorevenan
immuno-logical reaction after vaccination was described. No such
associationwasdeterminedinourstudy.
Males are more frequentlyaffected, in proportionsthat
accordingtotheliteraturerangefrom2:1to11.5:1.11,18,20There
isno preferenceregardingthe lateralityofthe disorder,or
anycorrelationwiththedominantlimb.However,onethirdof
thepatientsmaybeaffectedbilaterallyandasymmetrically.21
Turnerdescribedacaseofbilateralimpairment,sixmonths
Table2–ResultsfromConstantandMurleyscoresatthe endofthemeanfollow-upperiodof14months.
ConstantandMurleyscore Mean(min–max)
Pain 15(15–15)
Activities 20(20–20)
Mobility 40(40–40)
Strength 21.37(19–25)
Total 96.37(94–100)
Source:researchdata.
after the start of the symptoms. Around one third of the
patientsdevelopPTSbilaterally.11Inourstudy,theproportions
relatingtosexwere1.6mentoonewoman.Themeanagewas
29yearsandtherewerenocasesofbilaterality.
Thereisnoconsensusregardingtheperipheralnervemost
frequentlyaffected.AccordingtoTurnerandParsonage,11the
long thoracic nerve is the one most affected. Magee and
DeJong20andTsairisetal.11reportedthatthesuprascapular
nervewastheonemostfrequentlyaffected.Accordingto
Mul-veyetal.,22eventhephrenicnervecanbeaffectedincasesof
PTS.Inoursample,itwasseenthatthelongthoracicnerve
(n=3)andsuprascapularnerve(n=3)wereequallyaffected,
followedbytheaxillarynerve(n=2).
The characteristicpattern ofsudden pain with
sponta-neousimprovementfollowedbyweaknessofthemusculature
ofthescapularbeltisthekeytodiagnosingthissyndrome.In
all ofourpatients,weidentifiedthis pattern.Thepainhas
beendescribedassevereandexcruciating,anditmaypersist
forhoursorevenuptothreeorfourweeks.23Inourpatients,
thepainlastedonaverageforfivedays,withaminimumof
24handmaximumof15days.Theconsequencesof
impair-mentofthemotornervefibers,suchasweaknessandmuscle
atrophy,wereperceptibleandconstitutedthepatients’main
complaintafterthehyperalgesicphase.Regardingalterations
tosensitivity,suchasanalgesiaandhypoesthesia,thesewere
minimalandoftenlimitedtoasmallarea.Thesefindingswere
compatiblewiththeclassicaldescriptionsandalsowithmore
recentstudiescomprisingcaseserieswithlargenumbersof
patients.12,24,25
Electroneuromyography examinations are important for
confirmingthediagnosis.Alterationsontheseexaminations
are generally perceptiblethreeweeksafterthe start ofthe
symptoms.26,27 These usually consistof acute denervation
andindicate situationsofaxonaldegeneration,with
poten-tialpositivefibrillationspikewaves.Frommagneticresonance
examinations, the following findings in the musculature
affectedhavebeendescribedintheliterature:intramuscular
edemaandmuscleatrophythatmayormaynotbeassociated
withfattyinfiltration28,29(Fig.3).TheincreasedsignalwithT2
weightingisduetomuscleedema.AccordingtoWessigetal.,30
thereisanincreaseincapillarybloodvolume48haftermuscle
denervation, whichfavorsextravasationfromintracapillary
sitestoextracellularsites.Thesealterations,whichhavebeen
describedinmagneticresonanceexaminations,were
ThetreatmentforPTScanbedividedintotwophases.In
thefirstphase(hyperalgesia),analgesicsandrestforthelimb
affected,withuseofasling,areprescribed.Nocorticosteroid
anti-inflammatory agents were used, since the etiological
identityofthesyndromecouldnotbedetermined(i.e.viralor
autoimmune).Thus,wedonotrecommenduseofthisclass
ofdrugs, althoughstudies have shown thattheir use may
shortenthetimetakenforrecoveryofstrengthtostartand
improvethepainduringtheacutephase.11,21 Afterthepain
hasimproved,thesecondphasecanbestarted,whichaims
toreestablishandmaintaintherangeofmotion,followedby
musclestrengthening.In1960,MageeandDeJong20reported
that fullrecovery might take aslong aseight years.
How-ever,allthepatientstreatedinourstudyoverthe14-month
periodpresentedimprovementsintrophismandstrengthin
theaffectedlimb.Sixoftheeightpatientsdeclaredthatthey
didnotfeelanydifferenceinrelationtostrengthandpain,in
comparisonwiththecontralateralside.
AlthoughParsonage–Turnersyndrome isnot acommon
condition inclinical practice, it isimportant that
orthope-dists shouldbecome familiar with it and includeit inthe
differential diagnosis whenpatients complain ofpain and
weaknessinthescapularbelt.Thediagnosisisclinicaland
theelectroneuromyographyexaminationcanbeusedto
con-firmit.Otherexaminationsareonlyneededforthedifferential
diagnosis.Theprognosisisgood,withspontaneous
resolu-tionofthepaininaround80–90%ofthecases.11,31However,
strengthisnotalwaysfullyrecoveredandtheconditionmay
presentrecurrence.11,12 Conservativetreatment,comprising
useofanalgesicsandphysiotherapeuticexercises,generally
bringssatisfactoryresults,buttherehavebeenreportsof
sur-gicaltreatmentwithtendontransfers,aslatetreatmentfor
lossofstrength.
Thepresentstudyhastheadvantageofprovidingareport
on a series of cases of a rare disease that needs to be
rememberedasadifferentialdiagnosisforapainfulshoulder
condition,especiallywhenassociatedwithmuscleweakness
andhypotrophy.Themaindisadvantagewasthesmall
num-berofpatientsinthesample.Nonetheless,ourfindingsdidnot
divergefromthereportsintheliteratureinothercountries,
withlargesamplesofpatients.
Conclusion
Amyotrophicneuralgiaisapathologicalconditionthatis
dif-ficulttodiagnoseintheacutephase.Itmostoftenpresentsas
anacuteconditionofintensepaininthescapularbelt,which
isgenerallyself-limitedand inmostcasesevolvesto
func-tionalrecovery.Carefulclinicalevaluationandearlydiagnosis
usingelectroneuromyographyhelptowardadequate
manage-mentofthediseaseandbringreassuranceforpatientsand
theirdoctors,alongwithinformationregardingtherecovery.
Correctdiagnosisalsohastheadvantageofavoiding
unnec-essaryexaminations.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.FeinbergJ.FallvonErb-Klumpkescher:lahmungnach influenza.Centralbl.1897;16:588–637.
2.BramwellE,StruthersJW.Paralysisoftheserratusmagnus andlowerpartofthetrapeziusmuscles.RevNeurolPsychiatr. 1903;1:717–30.
3.Wyburn-MasonR.Brachialneuritisoccurringinepidemic form.Lancet.1941;1:662–3.
4.BurnardED,FoxTG.Multipleneuritisofshouldergirdle: reportofninecasesoccurringinsecondNewZealand expeditionaryforce.NZMedJ.1942:41.
5.SpillaneJD.Localisedneuritisoftheshouldergirdle:areport of46casesintheMEF.Lancet.1943;2:532–5.
6.ParsonageMJ,TurnerJW.Neuralgicamyotrophy;the shoulder-girdlesyndrome.Lancet.1948;1(6513):973–8.
7.AugeWK2nd,VelazquezPA.Parsonage–Turnersyndromein theNativeAmericanIndian.JShoulderElbowSurg. 2000;9(2):99–103.
8.PellasF,OlivaresJP,ZandottiC,DelarqueA.Neuralgic amyotrophyafterparvovirusB19infection.Lancet. 1993;342(8869):503–4.
9.SuarezGA,GianniniC,BoschEP,BarohnRJ,WodakJ,Ebeling P,etal.Immunebrachialplexusneuropathy:suggestive evidenceforaninflammatory-immunepathogenesis. Neurology.1996;46(2):559–61.
10.KuhlenbäumerG,HannibalMC,NelisE,SchirmacherA, VerpoortenN,MeulemanJ,etal.MutationsinSEPT9cause hereditaryneuralgicamyotrophy.NatGenet.
2005;37(10):1044–6.
11.TsairisP,DyckPJ,MulderDW.Naturalhistoryofbrachial plexusneuropathy.Reporton99patients.ArchNeurol. 1972;27(2):109–17.
12.VanAlfenN,vanEngelenBGM.Theclinicalspectrumof neuralgicamyotrophyin246cases.Brain.2006;129Pt 2:438–50.
13.BardosV,SomodskaV.Epidemiologicstudyofabrachial plexusneuritisoutbreakinnortheastCzechoslovakia.World Neurol.1961;2:973–9.
14.SerorP,HarbachS.Parsonage–Turnersyndromeafter cytomegalovirusinfection.PresseMed.1990;19(11):527–8.
15.BotellaMS,GarciaM,CuadradoJM,MartinR.
Parsonage–TurnersyndromeinpositiveHIVpatients.Rev Neurol.1997;25(137):143[Letter].
16.JiguetM,TroussierB,PhelipX.ParsonageandTurner syndrome.Aproposofacase,withdemonstrationofBorrelia burgdorferiinfection.RevRhumMalOsteoartic.
1991;58(5):409–11.
17.BeghiE,KurlandLT,MulderDW,NicolosiA.Brachialplexus neuropathyinthepopulationofRochester,Minnesota, 1970–1981.AnnNeurol.1985;18(3):320–3.
18.TurnerJW,ParsonageMJ.Neuralgicamyotrophy(paralytic brachialneuritis);withspecialreferencetoprognosis.Lancet. 1957;273(6988):209–12.
19.ConstantCR,MurleyAH.Aclinicalmethodoffunctional assessmentoftheshoulder.ClinOrthopRelatRes. 1987;(214):160–4.
20.MageeKR,DejongRN.Paralyticbrachialneuritis.Discussion ofclinicalfeatureswithreviewof23cases.JAMA.
1960;174:1258–62.
21.VanAlfenN.Theneuralgicamyotrophyconsultation.J Neurol.2007;254(6):695–704.
22.MulveyDA,AquilinaRJ,ElliottMW,MoxhamJ,GreenM. Diaphragmaticdysfunctioninneuralgicamyotrophy:an electrophysiologicevaluationof16patientspresentingwith dyspnea.AmRevRespirDis.1993;147(1):
23.McCartyEC,TsairisP,WarrenRF.Brachialneuritis.Clin OrthopRelatRes.1999;(368):37–43.
24.FaveroKJ,HawkinsRH,JonesMW.Neuralgicamyotrophy.J BoneJtSurgBr.1987;69(2):195–8.
25.MisamoreGW,LehmanDE.Parsonage–Turnersyndrome (acutebrachialneuritis).JBoneJtSurgAm.1996;78(9): 1405–8.
26.WeikersNJ,MattsonRH.Acuteparalyticbrachialneuritis.A clinicalandelectrodiagnosticstudy.Neurology.
1969;19(12):1153–8.
27.RubinDI.Neuralgicamyotrophy:clinicalfeaturesand diagnosticevaluation.Neurologist.2001;7(6): 350–6.
28.ScalfRE,WengerDE,FrickMA,MandrekarJN,AdkinsMC.MRI findingsof26patientswithParsonage–Turnersyndrome.AJR AmJRoentgenol.2007;189(1):W39–44.
29.GaskinCM,HelmsCA.Parsonage–Turnersyndrome:MR imagingfindingsandclinicalinformationof27patients. Radiology.2006;240(2):501–7.
30.WessigC,KoltzenburgM,ReinersK,SolymosiL,BendszusM. Musclemagneticresonanceimagingofdenervationand reinnervation:correlationwithelectrophysiologyand histology.ExpNeurol.2004;185(2):254–61.