Revista da Sociedade Brasileira de Medicina Tropical 20(2): 129-132, Abr-Jun, 1987.
P A R A C O C C I D I O I D O M Y C O S I S : A R E C E N T L Y P R O P O S E D C L A S S I F I C A T I O N O F I T S C L I N I C A L F O R M S
M arcello Fra n co1, M ário Rubens M ont enegro1, Rinaldo Pôncio M e n de s2,
Silvio Alen ca r M arques2, N eusa L. Dillon
2
and Norm a Gerusa da Silva M ot a
3
M any attem pts have been m ade to define the cli nical forms o f hum an paracoccidioidom ycosis15. Several classifications are based on different p ara meters of the disease such as entry route (tegumentary or pulm orary15); presence or absence of signs and/or symptoms (infection vs. disease2 14); organs
involved (lymphatic form; pulm onary form 15); presen ce or absence o f activity (active; latent12); type of evolution (progressive; regressive1 2 20); duration o f the
disease (acute; subacute; chronic4); clinical course (localised; systemic4 26); type o f infection (primary;
endogenous or exogenous reinfection19); presence or absence o f sequelae (cor pulmonale; A ddison’s disea se12); pathological anatom y (isolated organic form; pseudotum oral forms22) and immunohistological res ponse (polar forms21).
This variety o f criteria is an indication of the partial acceptance o f m ost o f them. This is comprehen sible since we still do not know where the fungus comes from and how it invades the hum an host, making difficult the evaluation of the early phases o f the disease.
In the “ Segundo Encontro sobre Paracoccidioi- domicose” held in Botucatu, Brazil, in 1983, a commi ttee o f experts* was nom inated with the objective o f proposing a classification o f clinical forms o f the disease. A questionnaire was circulated among the members and the committee reconvened at the Inter
1. D epartm ent o f Pathology, School of M edicine/U N E SP , Botucatu, São Paulo, Brazil.
2. D epartm ent o f Infectious and Parasitic D isease, D erm a tology, and Radiology, School o f M edicine/U N E SP , Botucatu, São Paulo, Brazil.
3. D epartm ent o f M icrobiology and Im munology/IBBM A / U N E S P , Botucatu, São Paulo, Brazil.
C orrespondence to: D r. M ário R. M ontenegro, D ept? P ato logia, F aculdade de M edicina de B otucatu/U N E S P , 18610 Botucatu, São Paulo, Brasil.
(*) T he committee include D r. M aria de A lbornoz (C aracas, Venezuela), Dr. G ildo D el N egro (S ão Paulo, Brazil), D r. A dhem ar Fiorillo (R ibeirão Preto, Brazil), D r. A lberto Londero (S anta M aria, Brazil), D r. R icardo N egroni (Bue nos Aires, A rgentina), D r. A n tar Padilha-G onçalves (Rio de Janeiro, Brazil) and D r. A ngela R estrepo (M edellin, Colom bia). In M edellin, D r. M arcello F ranco (Botucatu, Brazil) and D r. M aria Shikanai-Iasuda (S ão Paulo, Brazil) also participated. T he committee was chaired by D r. M ário Rubens M ontenegro (Botucatu, Brazil).
Recebido para publicação em 2 8 /4 /8 6
national Colloquium on Paracoccidioidom ycosis held in February 1986 in M edellin, Colombia. D uring the meeting, the written comments o f all members were analysed and a new simple classification was agreed. The members also agreed on the necessity o f dissemi nating information on the new classification to the South A m erican specialists.
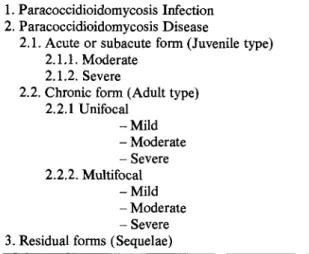
In this paper we describe this new classification (T able 1) and outline its correlation with the natural history o f paracoccidioidom ycosis (Figure 1).
Table 1 - Proposed Classification o f
Paracoccidioidomycosis.
1. Paracoccidioidom ycosis Infection 2. Paracoccidioidom ycosis D isease
2.1. A cute o r subacute form (Juvenile type) 2.1.1. M oderate
2.1.2. Severe
2.2. C hronic form (A dult type) 2.2.1 Unifocal
- M i l d - M oderate - Severe 2.2.2. M ultifocal
- M i l d - M oderate - Severe 3. Residual forms (Sequelae)
F rom its natural habitat, Paracoccidioides
bra-siliensis (P. brabra-siliensis) penetrates the host, usually
the lungs or exceptionally through the integument. Once within the tissues, the parasite may be immedia tely destroyed or m ay multiply, to produce a inoculation lesion. T he fungus then drains into the regional
lymph nodes, producing a satellite lymphatic lesion. T he inoculation and the satellite lymphatic lesions form the primary complex: lung + lymph node o f the hilus or integument + draining lymph nodes. H aem a- togenic dissem ination o f the fungus m ay occur at this moment, with the establishm ent o f lesions in any organ of the host constitutingmetastatic foci. Throughout
this period, there m ay be no apparent signs o r symp toms, the silent paracoccidioidomycosis infection.Comunicação. Franco M , Montenegro M R, M endes RP, M arques SA, Dillon NL, M ota NGS. Paracoccidioidomycosis: a recently proposed classification o f its clinical forms. Revista da Sociedade Brasileira de Medicina Tropical 20:129-132, Abr-Jun, 1987.
Fig. 1 - Paracoccidioidomycosis: natural history
and clinical forms.
H ow ever host sensitization m ay occur with the deve lopm ent o f an immunospecific response and positivity o f the paracoccidioidin intraderm al test.
The foci in this initial form may: i) regress with fungus destruction and formation o f sterile scars; ii) regress with the m aintenance o f viable fungi and form ation o f quiescent foci; o r iii) progress leading to the appearance o f signs and symptoms.
T he onset of clinical manifestations characteri ses the beginning of
paracoccidioidomycosis disease,
which m ay arise in three different ways:1. D irect evolution from the prim ary complex without latency.
2. Reactivation of quiescent foci from the primary complex (endogenous reinfection).
3. Exogenous reinfection after a previous infection. Once established, the disease m ay evolve in two ways:
(1) Acute or subacute form - the disease is established
from an usually undetected prim ary lesion and pro gresses rapidly, by lym phatic and lympho-haemato- genic dissemination to the monocytic-macrophagic system (spleen, liver, lym ph nodes, bone marrow). The clinical picture is characterised by systemic lymph node involvement, hepatosplenomegaly and bone m arrow dysfunction. This picture may mimic a systemic lymphoproliferative disease and depending on the degree of dissemination, can be subtyped to moderate o r severe forms. It affects young patients ofboth sexes. In m ost cases, the specific humoral immune response tends to be m aintained with high antibody titers, but there is severe depression o f the cellular immunity. Histopathology reveals loose granulomata with large numbers of actively multiplying fungi. (2 ) Chronic form - the disease starts from the primary complex or from quiescent foci and develops slowly, remaining localized or involving more than one organ or system. Symptoms m ay be referred to a single (unifocal form) or to m ore than one organ or system (multifocal form). A s m ost o f the cases o f chronic paracoccidioidom ycosis start in the lungs, the disease m ay rem ain there with slow and progressive morpho logic and clinical pulm onary involvement, the
pulm o
nary unifocal form. The infection may then spread by
bronchogenic, lymphatic or lympho-haematogenic routes, the multifocal form . Less frequently, prim ary progressive and isolated muco-cutaneous involvement occurs thetegumentary unifocal form.
On the other hand, the disease m ay start from m etastatic foci, such as those in the central nervous system, intestine, bone, adrenals, genital organs etc. The patients seek medical care because of the invol vem ent o f an organ or system not related to the area of inoculation, the extra pulm onary unifocal form.
D epending on the clinical findings and the patient’s general condition, chronic forms can be subtyped in mild, m oderate or severe. Patients m ay die or recover: the healed lesions m ay contain viable fungi (quiescent foci) o r leave sequelae (respiratory insuffi ciency; chronic cor pulmonale; A ddison’s disease). U nder conditions favourable to the parasite, the disease m ay be reactivated from quiescent foci, thus reinitiating the cycle.
The chronic form affects alm ost only adult males. T he specific humoral response is variable; cellular immunity is preserved in the unifocal forms but m ay be depressed in the multifocal forms. H istopatho logy reveals m ore com pact epithelioid granulom ata with sm aller numbers o f fungi.
The proposed classification is based on the natural history o f the disease. W e started from the principle th a t the natural history o f paracoccidioidom ycosis, as has been described for other deep mycoses, should follow the same steps as th at classically described for tuberculosis, the model disease for chronic granuloma tous disorders6 7 1 1 13.
There is both direct and indirect evidence for the occurrence o f paracoccidioidom ycosis infection without disease. N am ely the detection o f fibrous and/or calcified pulm onary nodules containing dead or viable fungi3; the existence o f scarred lesions in the lymph nodes o f the pulm onary hilus31; the detection of a pulm onary prim ary complex with lymphangitis and satellite adenopathy in a surgical fragment from a patient with lung carcinom a3 2 and the relatively
Comunicação. Franco M, Montenegro M R, Mendes RP, M arques SA, Dillon N L, M ota NGS. Paracoccidioidomycosis: a recently proposed classification o f its clinical forms. Revista da Sociedade Brasileira de Medicina Tropical 20:129-132, Abr-Jun, 1987.
high percentage of positive skin tests for paracoccidi oidomycosis among norm al individuals living in endemic areas2 1 4
11.
Although well characterised forhistoplasmosis and coccidioidomycosis15, a sympto m atic paracoccidioidomycosis infection (F ava Netto: personal com m unication) is seldom diagnosed.
F o r the classification of the clinical forms of paracoccidioidomycosis we started from the fact that the mycosis may evolve: 1) rapidly with a
tendency towards dissemination and im pairment of patient’s general condition, usually affecting young individuals of both sexes, or 2) slowly, with localized
lesions, involving a smaller num ber of organ systems and generally affecting adult males. These two types o f evolution respectively characterize the acute or subacute form and the chronic form4 1 0 1 2 1 9 2 8 30.
T he recognition of the acute or subacute form is widespread in the literature. The entry route o f the fungus usually goes undetected, since these patients rarely have a history o f tegum entary lesion or radiolo- gically detectable lung damage45 15. The disease may
diffusely involve the reticuloendothelial system, re placing these tissues with macrophages that do not succeed in destroying the fungus or blocking its multiplication. The overall picture may simulate leukemia or malignant systemic reticulosis in severe forms. It may involve more localized segments of the lymphoid or reticuloendothelial system with a picture simulating a lymphoma (m oderate form)5. Patients with the acute or subacute forms have been classified as belonging to the anergic or negative pole o f paracoccidioidomyco
sis33. They usually exhibit a m arked decrease of the cellular immune response to P. brasiliensis antigens21. Antibody titers are high8.
However m ost o f the patients have chronic forms o f disease. In these cases the host has greater defense against the parasite which leads to a more protracted and localized course. Progressing from the inoculation lesion the disease m ay rem ain restricted or localized thus characterising the unifocal pulmonary (m ore frequent) o r the tegumentary unifocal chronic forms9 16. The disease may also manifest itself by
symptoms referred to other organs or systems starting from reactivation o f quiescent m etastatic foci (other unifocal forms). It should be pointed out here th at in cases o f unifocal organic involvement specific lesions in other organs, with no clinical manifestations have been found2 4 25. W hen the lesions in these other organs
expand and cause clinical manifestations, the patients exhibit the multifocal chronic form. Frequent exam ples are tegumentary-pulmonary, pulm onary-adrenal and pulm onary-lymphatic involvement.
A few chronic forms originating from metastatic foci are more circumscribed and encapsulated charac
terizing the pseudotum oral forms, the m ost outstan ding example being the paracoccidiom a2 7 29.
Patients with chronic forms maintaining a good general condition, intact cell immunity and exhibiting granulom ata o f the sarcoid type are classified as belonging to the hyperergic o r positive pole of the disease33.
Paracoccidioidom ycosis usually behaves as a disease o f insidious onset and slow evolution, with relapses in which clinical manifestations m ay differ from those o f previous attacks11. Variations in the intensity, extent, dissemination, and characteristics of the lesions will occur in a given patient depending on changes in fungal virulence, fluctuations o f the defense and immunological mechanisms o f the host and on environmental factors11. W hen a patient is classified in a clinical form, we should not forget th at he is at a particular phase o f a dynamic and polymorphic disea se.
There are signs indicating th at paracoccidioido mycosis exhibit variations in the frequency of clinical forms in different regions o f the same country51 5 or in
different countries1 1 2 1 5 1 8 2 3 28. This suggests either
the existence o f distinct P. brasiliensis strains, varia tion in the susceptibility of exposed individuals or environmental factors. These are im portant and as yet unelucidated aspects o f the disease. The only way o f comparing patients from different regions is by esta blishing an easily appliable, generally accepted sim ple classification of the clinical forms. This is the main purpose o f this communication.
R E F E R E N C E S
1. Albornoz MB. Paracoccidioidomicosis: estúdio clinico y inmunologico en 40 pacientes. Archivos del Hospital Vargas (C aracas) 18:5-22, 1976.
2. A lbornoz M B.Paracoccidioidomicosis-infección. In: Paracoccidioidomicose. Blastomicose sul-americana. D e lN e g ro G , L a c a z C S ,F io rillo A M (e d s), São Paulo, Sarvier-Edusp. pp. 91-96, 1982.
3. A ngulo-Ortega A . Calcifications in paracoccidioido mycosis: are they the morphological m anifestation of subclinical infections? In: Paracoccidioidomycosis. Proceedings F irst Panam erican Symposium, P A H O , W ashington, Scientific Publications n.° 254, pp. 129-
133, 1972.
4. B arbosa W . Blastomicose sul-americana. Contribuição ao seu estudo no E stado de G oiás, G oiânia. Tese de docência livre. F acuidade de M edicina da Universidade Federal de G oiás, G oiânia, 1968.
5. B arbosa W , D ah er R, O liveira AR. F orm a linfática abdominal da blastom icose sul-americana. R evista do Instituto de M edicina Tropical de São P aulo 10:16-27, 1968.
6. B ayerA S. Fungai pneumonias: pulm onary coccidioidal syndromes (P a rt I). Prim ary and progressive primary
Comunicação. Franco M, Montenegro M R. Mendes RP, Marques SA, Dillon N L , M ota NGS. Paracoccidioidomycosis: a recently proposed classification o f its clinical forms. Revista da Sociedade Brasileira de Medicina Tropical20:129-132, Abr-Jun, 1987.
coccidioidal pneumonias - D iagnostic, therapeutic and prognostic considerations. C hest 79: 575-583, 1981. 7. Bayer A S. F ungal pneumonia: pulm onary coccidioidal
syndromes (P a rt II). M iliary, nodular, and cavitary pulm onary coccidioidomycosis; chemotherapic and surgical considerations. C hest 79: 686-691, 1981. 8. Biagioni L, Souza M J, Cham m a L G , M endes RP,
M arques SA , M ota N G S , F ranco M. Serology o f paracoccidioidomycosis. II. C orrelation betw een class-specific antibodies and clinical forms o f the disea se. T ransactions o f the Royal Society o f Tropical M edicine and Higiene 78: 617-621, 1984.
9. Castro RM , Cucé L G , F av a N etto C. Paracoccidioi domicose. Inoculação experimental “ in anim al nobile” . Relato de um caso. M edicina C utânea Ibero-Latino- A m ericana 3: 289-292, 1975.
10. F ava N etto C. Contribuição para o estudo imunológico da blastomicose de Lutz. Revista do Instituto Adolfo Lute 21: 99-194, 1961.
11. Franco M F , M ontenegro M R G . A natom ia patológica. In: Paracoccidioidomicose. Blastomicose sul-america- na. Del Negro G, Lacaz CS, Fiorillo AM (eds) São Paulo, Sarvier — E dusp. pp. 97-117, 1982.
12. G iraldo R, R estrepo A , G utiérrez F , Robledo M , Londono F , H ernandez H, Sierra F , Calle G . Patho genesis o f paracoccidioidomycosis: a model based on the study o f 45 patients. M ycopathologia 58: 63-70, 1976.
13. Goodwin J r RA, Shapiro JL , Thurman G H , Thurman SS, D es Prez RM. D issem inated histoplasmosis: clini cal and pathological correlations. M edicine 59:1-33, 1980.
14. Lacaz C S, Passos Filho M C R , F a v a N e to C, M acarron B. Contribuição para o estudo da “ blastomicose in fecção” . Inquérito com a paracoccidioidina. Estudo sorológico e clínico-radiológico dos paracoccidioidino- positivos. Revista do Instituto de M edicina Tropical de São Paulo 1: 254-259, 1959.
15. Lacaz CS. M icologiam édica, 6?. ed, São Paulo, Sarvier S /A Editora,pp. 229-274, 1977.
16. Lacaz CS, C astro RM, M inam i PS, Viegas A C. Blas- tomicosis sudam ericana con localizacion perianal pri mitiva. D erm atologia (M éxico) 8: 242-250, 1964. 17. Londero A T. Epidemiologia da paracoccidioidomi-
cose. A rs Curandi 7: 14-22, 1975.
18. Londero A T. Paracoccidioidomycosis. In: Infectious diseases. H oeprich P D (ed) 3rd ed, H arper & Row Publication, M aryland, U S A , in press.
19. Londero A T , Ram os C D , Lopes JO . Paracoccidioido micose: classificação das formas clinicas. Revista Uru- guaya de Patologia Clinica y Microbiologia 14: 3-9,
1976.
20. Londero A T. Paracoccidioidomicose. I - Patogenia, formas clinicas, manifestações pulm onares e diag nóstico. Jornal de Pneumologia 12: 41-57, 1986. 21. M o ta N G S , Iw asso M T R , Peraçoli M T S, A udi R C ,
M endes R P, M arcondes J, M arques SA , D illon N L, F ranco M F . Correlation between cell-m ediated immu nity and clinical forms of paracoccidioidomycosis. Transactions o f the R oyal Society o f Tropical Medicine and Hygiene 79: 765-772, 1985.
22. M otta LC, Pupo JA . G ranulom atose paracoccidióidica (blastom ycose brasileira). A nais da Faculdade de M e dicina de São Paulo 12: 407-426, 1936.
23. N egroni P, N egroni R. N uestra experiencia de la blastom icosis sudam ericana en la Argentina. M ycopa thologia 26: 264-272, 1965.
24. P adilha G onçalves A. Localizações ganglionares da micose de Lutz (Blastomicose brasileira). Boletim da A cadem ia N acional de M edicina 1: 5-17, 1962. 25. Padilha G onçalves A. A denopathy in paracoccidioi
domycosis. In: Paracoccidioidomycosis. Proceedings of F irst Panam erican Symposium, P A H O , Washington, Scientific Publication n.° 254: 189-190, 1972. 26. Padilha Gonçalves A. Paracoccidioidomicose. A tuali
dade, Classificação. A nais Brasileiros Derm atologia 60 (supl 1): 271-280, 1985.
27. Pereira W C , R aphael A , Sallum J. Lesões neurológicas na blastomicose sul-americana. E studo anatom opato lógico de 14 casos. Arquivos de N euro-Psiquiatria 23: 95-112, 1965.
28. R estrepo A. Paracoccidioidomycosis. A cta M edica Colom biana 3: 33-65, 1978.
29. R estrepo A , Bedout C, C ano L E , Arango M D , Bedoya V. Recovery o f Paracoccidioides brasiliensis from a partially calcified lymph node lesion by microaero- philic incubation o f liquid media. Sabouradia 19: 295- 300, 1981.
30. R estrepo A , Robledo M , G iraldo R, H ernandez H, Sierra F , G utiérrez F , Londono F , López R, Calle G. The gamut o f paracoccidioidomycosis. American Journal o f M edicine 61: 33-42, 1976.
31. Severo LC. Paracoccidioidomicose. E studo clínico e radiológico das lesões pulm onares e seu diagnóstico. Tese de M estrado. Porto Alegre, 1979.
32.Severo LC, G eyer G .R , Londero A T , P orto N S, Rizzon C F C . The prim ary pulm onary lym ph node complex in paracoccidioidomycosis. M ycopathologia 67: 115-118, 1979.
33. Zam ith VA, Lacaz CS, Siqueira A M , Santos CRA , O liveira Z N P . Paracoccidioidomicose - forma hiperér- gica com prováveis lesões de mícide (blastomícide ou paracoccidioidomícide). Registro de um caso. A nais Brasileiros de Derm atologia 56: 273-278, 1981.