RevBrasAnestesiol.2016;66(2):197---199
REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
CLINICAL
INFORMATION
Laparoscopic
cholecystectomy
under
continuous
spinal
anesthesia
in
a
patient
with
Steinert’s
disease
Mariana
Correia
a,∗,
Angela
dos
Santos
b,
Neusa
Lages
b,
Carlos
Correia
baServic¸oAnestesiologia,CentroHospitalarLisboaOcidental,Lisboa,Portugal bServic¸oAnestesiologia,CentroHospitalarAltoAve,Guimarães,Portugal
Received16November2013;accepted2January2014 Availableonline6February2014
KEYWORDS Continuousspinal anesthesia; Steinert’sdisease; Laparoscopic cholecystectomy
Abstract Steinert’sdiseaseisanintrinsicdisorderofthemusclewithmultisystem manifes-tations.Myotoniamayaffectanymusclegroup,iselicitedbyseveralfactorsanddrugsused ingeneralanesthesialikehypnotics,sedativesandopioids.Althoughsomeauthorsrecommend theuseofregionalanesthesiaorcombinedanesthesiawithlowdosesofopioids,thesafest anesthetictechniquestillhastobeestablished.
WeperformedacontinuousspinalanesthesiainapatientwithSteinert’sdiseaseundergoing laparoscopiccholecystectomy using10mgofbupivacaine0.5%andprovidedventilatory sup-port intheperioperativeperiod. Continuousspinalanesthesia was safelyused inSteinert’s disease patients butisnot describedfor laparoscopiccholecystectomy. We reporteda con-tinuous spinalanesthesiaasanappropriatetechniquefor laparoscopiccholecystectomy and particularlyvaluableinSteinert’sdiseasepatients.
© 2014SociedadeBrasileirade Anestesiologia.Publishedby ElsevierEditoraLtda.Allrights reserved.
PALAVRAS-CHAVE Raquianestesia contínua;
Doenc¸adeSteinert; Colecistectomia laparoscópica
Colecistectomialaparoscópicasobraquianestesiacontínuaempacientecomdoenc¸a
deSteinert
Resumo A doenc¸a deSteinerté uma desordem intrínseca domúsculo commanifestac¸ões multissistêmicas.A miotoniapodeafetarqualquer grupomusculareéprovocadaporvários fatores emedicamentosusados emanestesia geral, como hipnóticos,sedativoseopiáceos. Emboraalgunsautoresrecomendemousodeanestesiaregionalouanestesiacombinadacom opiáceosemdosesbaixas,atécnicaanestésicamaisseguraaindaprecisaserestabelecida.
∗Correspondingauthor.
E-mail:mariana.d.correia@gmail.com(M.Correia).
198 M.Correiaetal.
Administramosraquianestesiacontínuaemumpacientecomdoenc¸adeSteinertsubmetido àcolecistectomialaparoscópica,com10mgdebupivacaínaa0,5%,efornecemossuporte ven-tilatório no período perioperatório.A raquianestesia contínua foi usada comseguranc¸a em pacientescomdoenc¸ade Steinert,mas não foirelatadaem colecistectomia laparoscópica. Relatamos a raquianestesia contínua como uma técnica adequada para a colecistectomia laparoscópicaeparticularmentevaliosaempacientescomdoenc¸adeSteinert.
©2014SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Steinert’sdisease(SD)isanintrinsicdisorderofthemuscle withmultisystemmanifestations.Inheritanceisautosomal dominant and a prevalence of about 3---5 in 100,000.1
Patientsusuallypresent between agesof 15and 35 years
withweaknessofgrip,impairedfootdorsiflexion,cataracts
and infertility. Muscular weakness is usually found in the
face,neckanddistalmusclesgroupcontributingto
charac-teristicfacialappearance.Myotoniamayaffectanymuscle
groupandiselicitedbydrugs,pain,cold,shivering,surgical
manipulationsandelectricscalpelamongotherfactors.2
Extramuscularinvolvementisalmostinvariablewith
car-diac (conducting system and cardiac muscle), ventilatory
(respiratorymusclesweakness,centralabnormalities),
gas-trointestinal(dysphagia,reductionin theratingof gastric
emptying) and endocrine affection (hypothyroidism,
pri-marygonadalfailure,diabetesmellitus).
The perioperative assessment of these patients should
target the extramuscular manifestations of the disease
which may be life-threatening. The conduct of
anesthe-sia poses particular problems which include the increase
of sensitivity to several drugs used during general
anes-thesia.The patients withthis diseasehave anincrease of
thesensibilitytohypnoticsandsedativeswhichcancause
apneaevenwithsmalldoses.3Inhalationagentsmayfurther
risk the already compromised cardiovascular and
respira-torysystems,whilepostoperativeshiveringmayprecipitate
myotoniccrisis.4Depolarizingrelaxantsshouldbeavoided
becausethey can trigger myotonic crisis and difficulty in
ventilationandintubation.5Non-depolarizing
neuromuscu-larblockingagentsusuallyevokeanormalresponsebutif
musclewastingexistsaprolongedresponsemayoccur.4
The postoperative complications usually result in
pul-monary and cardiac dysfunction and pharyngeal muscle
weakness.Regardingthisknowledge regionalanesthesiais
consideredthebestoptioninthesepatients,althoughthe
safestanesthetictechniquestillhastobeestablished.
We present a continuous spinal anesthesia(CSA) in SD
patientforlaparoscopiccholecystectomy(LC).
Case
description
A35-year-oldCaucasianfemale,withSDwasscheduledfor
electiveLC.
Sheisbeingfollowedinthepneumologydepartmentand
presentedrestrictivepulmonarydiseasewithmild
ventila-toryimpactandindicationfornocturnalBIPAPsupportthat
shedoes notadhere.Sheis currentlynotunderany
med-ication.Previous cervical cesarean undercombinedspinal
epidural anesthesia was without complications. Physical
examination revealed facial atony, mild prognatism and
shortneck.
Afterstandardmonitoring, continuousspinal blockwas
performed without any pre-medication, in right lateral
decubitus,atL2---L3levelwithparamedianapproach,using
aspinocathkitB.Braun®(24G,29G)and20mcgoffentanyl
with1mlofnormalsalinesolutionwereadministered.
Hav-ingthepatientalreadyinproneposition,5mgofhyperbaric
bupivacaine wereadministered throughthecatheterwith
2mlofnormalsalinesolution.Thesensorylevelafter5min
was T12 and subsequently a top-up with 5mg of isobaric
bupivacainewith1mlofnormalsalineallowedaspreading
throughT7level.T4levelwasachieved5minlater.
Analgesiaincluded80mcgoffentanylbeforetheincision,
acetaminophen1gand40mgofparecoxibduringthe
proce-dure.Referredleftshoulderpainwaseffectivelycontrolled
withdiaphragmaticinstillationof2%lidocaine.After40min
aspinalperfusionofropivacaine0.1%at2ml/hwasstarted
andmaintainedduring24h.
Non-invasive ventilatory (NIV) support was instituted
12h beforesurgery until24haftersurgerywithBIPAPS/T
(Spontaneous/Timed)6/14cmH2Oandcoughassistdevice.
Spirometryandbloodgasometrywereassessedduring
peri-operativeperiod(Tables1and2).Maximalintra-abdominal
pressure(IAP)was10mmHgandat theendofthesurgery
abdominal was 8mmHg. Minimal blood oxygen saturation
was92%
Nomyotoniccrisesweretriggeredduringtheprocedure.
After3h inthe PostAnesthesia CareUnit (PACU)
com-pletedmotorblockwascompletelyreversedandthepatient
referrednopainordyspnea.
At 24h the spinal catheter was removed without
complicationsandshewasdischargedhomewithoutnoticed
intercorrences.
Discussion
CSA allowed a sensoryblock suitablefor the surgery and
minimalrespiratoryimpairment.CSAwaschosenconcerning
co-morbidities of the patient, suitability to the
proce-dure and the already described complications of general
anesthesia in this context. In fact, Cope et al.6
consid-ered that regional anesthesia is the best option in these
patients because trigger drugs of myotonic crisis are not
used. March et al.7 recommended regional anesthesia or
combined generaland regional anesthesiawith restricted
use ofopioids, becausethesepatients have higherrisk of
respiratorydepression.CSAhasalreadybeenusedwith
LaparoscopiccholecystectomyundercontinuousspinalanesthesiainapatientwithSteinert’sdisease 199
Table1 Perioperativespirometricevaluation.
Baseline CSA+NIV MaximalIAP+NIV PACU+NIV
FVC(L) 2.60 2.24 2.00 2.59
FEV1(L) 1.99 1.79 1.65 1.99
FEV1/FVC(%) 76.50 79.88 82.58 78.35
FVC,functionalvitalcapacity;FEV1,forcedexpiratoryvolumein1s;NIV,non-invasiveventilation;IAP,intra-abdominalpressure;PACU, Post-anesthesiacareunit.
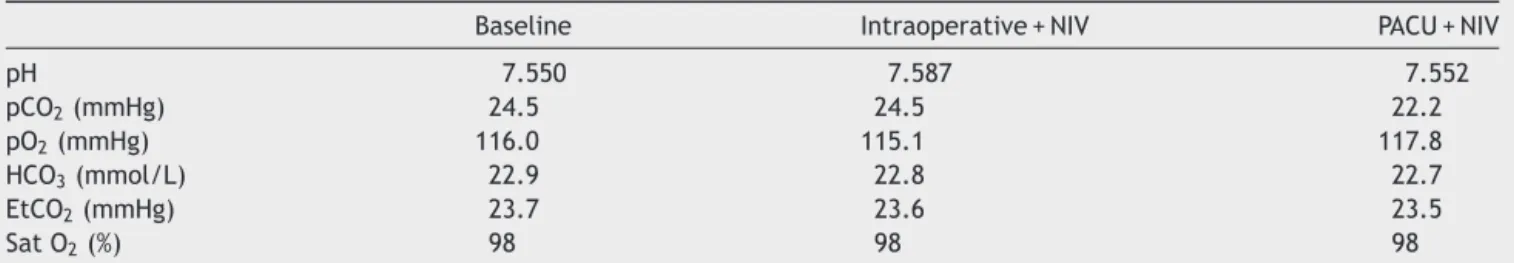
Table2 Perioperativebloodgasometricevaluation.
Baseline Intraoperative+NIV PACU+NIV
pH 7.550 7.587 7.552
pCO2(mmHg) 24.5 24.5 22.2
pO2(mmHg) 116.0 115.1 117.8
HCO3(mmol/L) 22.9 22.8 22.7
EtCO2(mmHg) 23.7 23.6 23.5
SatO2(%) 98 98 98
pO2andpCO2,bloodpartialpressureofoxygenandcarbondioxide;EtCO2,endtidalcarbondioxide;SatO2,oxygensaturation;HCO3,
bicarbonateion.
LC.9---13Also,Verdagueretal.14describedacaseofCSAina
patientwithSDproposedforhysterectomy.Buttoour
knowl-edgethisisthefirstcaseofLCunderCSAinapatientwith
Steinert’s disease. Bennun et al.,15 reported a significant
decrease in mean postoperative vital capacity (from 965
to349mL) fromthepreoperative value during continuous
propofolanesthesia. Inourpatienttherewasnodecrease
inpostoperativevitalcapacitycomparingwithpreoperative
values.Accordingtothe spirometricevaluationtherewas
not a significant impairment of themechanics of
ventila-tionevenafterfullestablishmentofthesensitiveblockor
afterthepneumoperitoneum.Furthermore,seriatedblood
gasanalysisvalidatedthecontributionofperioperative
non-invasiveventilatorysupport.
Conclusion
Postoperativepaincontrol waseffective andopioidswere
avoided. No spinal headachewas noticed which could be
explainedbytheremovalofthecatheteronlyafter24h.16In
conclusion,wereportedaCSAasanappropriatetechnique
forLCandwithparticularvalueinSDpatients.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Udd B, Krahe R. The myotonic dystrophies: molecu-lar, clinical, and therapeutic challenges. Lancet Neurol. 2012;11(10):891---905.
2.MathieuJ, AllardP,GobeilG, et al.Anesthetic andsurgical complicationsin219casesofmyotonicdystrophy.Neurology. 1997;49(6):1646---50.
3.SpeedyH.Exaggeratedphysiologicalresponsestopropofolin myotonicdystrophy.BrJAnaesth.1990;64:110---2.
4.Aldridge LM. Anaesthetic problems inmyotonic dystrophy. A casereportandreviewoftheAberdeenexperiencecomprising 48generalanaestheticsinafurther16patients.BrJAnesth. 1985;57(11):1119---30.
5.AzarI.Theresponseofpatientswithneuromusculardisorders tomusclerelaxants:areview.Anesthesiology.1978;49:44---8. 6.Cope D, Miller J. Local and spinal anesthesia for cesarean
section in a patientwith myotonic dystrophy.Anesth Analg. 1986;65:687---90.
7.MarchX,RossJ,VizueteG,etal.Anestesiageneralcombinada comanestesiaperiduralenuncasodeenfermedaddeSteinert. RevEspAnestesiolReanim.1992;39(2):133.
8.Kumar CM, Corbett WA, Wilson RG. Spinal anaesthesia with a micro-catheter in high-risk patients undergoing colorec-tal cancer and other major abdominal surgery. Surg Oncol. 2008;17(2):73---9.
9.VanZundertA,StultiensG,JakimowiczJ,etal.Laparoscopic cholecystectomyundersegmentalthoracicspinalanaesthesia: afeasibilitystudy.BrJAnaesth.2007;98:682---6.
10.GramaticaLJr,BrasescoOE,MercadoLuna A,etal. Laparo-scopic cholecystectomyperformed underregional anesthesia inpatientswithchronic obstructive pulmonarydisease. Surg Endosc.2002;16:472---5.
11.Van Zundert A, Stultiens G, JakimowiczJ, et al. Segmental spinalanesthesiaforcholecystectomyinapatientwithsevere lungdisease.BrJAnaesth.2006;96:464---6.
12.Sinha R, Gurwara AK, Gupta SC. Laparoscopic surgeryunder spinalanesthesia.JSLS.2008;12(2):133---8.
13.Imbelloni LE, Sant’Anna R, Fornasari M, et al. Laparoscopic cholecystectomy underspinal anesthesia: comparativestudy between conventional-dose and low-dosehyperbaric bupiva-caine.LocalRegAnesth.2011;4:41---6.
14.Verdaguer MitjansM,BernalDzekonsky J, NogueraGarcíaJ, etal.ContinuoussubarachnoidblockinacaseofSteinert dis-ease.RevEspAnestesiolReanim.1991;38(3):204.
15.BennunM,GoldsteinB,FinkelsteinY,etal.Continuouspropofol anaesthesiaforpatientswithmyotonicdystrophy.BrJAnaesth. 2000;85:407---9.