REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiology www.sba.com.brSCIENTIFIC
ARTICLE
The
comparison
of
levobupivacaine
in
continuous
or
single
dose
spinal
anesthesia
for
transurethral
resection
of
prostate
surgery
Yunus
Baydilek
a,
Bülent
Serhan
Yurtlu
b,∗,
Volkan
Hanci
c,
Hilal
Ayo˘
glu
b,
Rahs
¸an
Dilek
Okyay
b,
Gulay
Erdo˘
gan
Kayhan
d,
Hüsnü
Tokgöz
e,
Görkem
Mungan
f,
Is
¸ıl
Özkoc
¸ak
baClinicofAnesthesiologySaniKonuko˘gluHospital,Gaziantep,Turkey
bDepartmentofAnesthesiologyandReanimation,BulentEcevitUniversity,Zonguldak,Turkey
cDepartmentofAnesthesiologyandReanimation,C¸anakkaleOnsekizMartUniversity,C¸anakkale,Turkey dDepartmentofAnesthesiologyandReanimation,InonüUniversity,Zonguldak,Turkey
eDepartmentofUrology,BulentEcevitUniversity,Zonguldak,Turkey
fDepartmentofBiochemistry,BulentEcevitUniversity,Zonguldak,Turkey
Received1May2012;accepted20March2013 Availableonline11October2013
KEYWORDS
Levobupivacaine;
Continuousspinal
anesthesia;
Spinalanesthesia;
Transurethral
prostateresection
Abstract
Background: Theaimofthestudyistocomparetheefficacyoflevobupivacaineinduced con-tinuousspinalanesthesia(CSA)versussingledosespinalanesthesia(SDSA)inpatientswhoare plannedtoundergotransurethralprostateresection.
Methods:Sixtyyearsorolder,ASAI---IIorIII,50patientswereincludedinthestudy.12.5mg 0.5%levobupivacainewere administered intrathecallyinSDSAgroup.InCSA group,initially 2mLof0.25%levobupivacainewereadministeredthroughspinalcatheter.Inordertoachieve sensoryblocklevelatT10dermatome,additional1mLof0.25%levobupivacainewere adminis-teredthroughthecatheterinevery10min.Hemodynamicparametersandblockcharacteristics wererecorded.Preoperativeandpostoperativebloodsamplesofthepatientsweredrawnto determineplasmacortisoneandplasmaepinephrinelevels.
Results:CSA techniqueprovidedbetterhemodynamicstability comparedtoSDSAtechnique particularly90minafterintrathecaladministration.Theriseinsensoryblocklevelwasrapidand thetimetoreachsurgicalanesthesiawasshorterinSDSAgroup.Motorblockdevelopedfasterin SDSAgroup.InCSAgroup,similaranesthesialevelwasachievedbyusinglowerlevobupivacaine doseandwhichwas relatedtofasterrecovery. Although,bothtechniqueswereeffective in preventing surgical stress respond,postoperative cortisonelevels were suppressed more in SDSAgroup.
∗Correspondingauthor.
E-mail:syurtlu68@gmail.com(B.S.Yurtlu).
0104-0014/$–seefrontmatter©2013SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Allrightsreserved.
Conclusion:CSAtechniquewith0.25%levobupivacainecanbeusedasaregionalanesthesia methodforelderlypatientsplannedtohaveTUR-Poperation.
©2013SociedadeBrasileiradeAnestesiologia.PublishedbyElsevier EditoraLtda.Allrights reserved.
Introduction
Anesthesia is appliedin 10---20% of urologic interventions.
Anesthetic methods chosen within general principles are
topical,regionalandgeneral.1,2Mostpatientswithbladder
obstructioncausedbybenignprostatichyperplasiaare suc-cessfullytreatedbytransurethralresectionoftheprostate (TUR-P).3TUR-Pisoftenperformedonolderpatientswith
impaired renal function, cardiovascular and respiratory problems.Researchhas foundmany sideeffects ofTUR-P includingbleeding,transurethralresectionsyndrome(TUR), bladderperforation,hypothermia,intraoperativeandearly postoperative occurrence of disseminated intravascular coagulation,with high reportedmorbidity rates. To mini-mizehemodynamicchangesinthesepatientsitisimportant toprovidestableanesthesia.Generalanesthesiamaymake identification ofcomplications such asTUR syndromeand bladderperforation difficult,so regionalanesthesiaisthe preferredmethodinsuitableTUR-Pcases.4---7
Single-dose spinal anesthesia (SDSA) is widely used in theseinterventionsthough it hasthe disadvantage ofnot providingtherequireddurationinoperationsthatrunlonger thanexpected.Withthecontinuousspinalanesthesia(CSA) technique,localanestheticdosecanrepeated,thusmaking itpossibletousethisspinalanesthesiamethodinoperations withlongduration.8---12 AnotheradvantageofCSAisthatit
enablestotitrate thedose oflocalanestheticthus allow-ingbettercontrolofsensoryandmotorblocklevel,norisk oflocalanesthetictoxicityandprovidingshorterrecovery periods.ComparedtoSDSA,itsmostimportantadvantage isthatitprovidesperfecthemodynamicstability. Further-more,spinalcathetermaybeinsertedinregionalanesthesia preparationroombeforetheoperation,thuspreventingloss oftimebetweenoperations.10,13,14
Levobupivacaine,abupivacaineSisomercommonlyused in spinal anesthesia (SA), has less side effects on the cardiovascular (CVS) and central nervous systems (CNS) than bupivacaine with similar effective onset time and duration.7,15---17 Although levobupivacaine use in various
regionalanesthesia techniques have been reported previ-ously, description of its use in CSA is limited. We have hypothesizedthatlevobupivacaineprovidesbetter hemody-namicstabilitywhenusedinCSAcomparedtoSDSA.Inorder totest thishypothesis, patients scheduled tohave TUR-P operationwereadministeredeither SDSAor CSA with lev-obupivacaine; hemodynamics,sensory-motor block levels, anestheticqualityandcomplicationswerecompared.
Materials
and
methods
After receiving permission from Bulent Ecevit University Medical Faculty Hospital Ethics Committee (06.12.2007,
Decisionno.2007/09/17),thisresearchwascarriedoutin theDepartmentofAnesthesiologyandReanimationbetween December2007andJune2008.Fiftypatientsovertheage of60scheduledtohaveelectiveTUR-PinterventionsatASA I---IIIriskgroupswereincludedinthestudyafterreadingthe informedconsentform.Thepatientswererandomizedinto eithercontinuousspinalanesthesiagroup(GroupCSA,n:25) orsingle-dosespinalanesthesiagroup(GroupSDSA,n:25)by randomizednumberstable.
Exclusion criteria were refusing to be included in the study,allergiestotheresearchdrugs,severecardiacfailure (unstablecoronaryarterydisease,2ndand3rddegreeheart block, congestive heart failure, ventricular tachyarrhyth-mia) and valvular heart disease (serious aortic stenosis), coagulation abnormalities, low molecular weight heparin administrationintheprevious12h,intakeofnon-steroidal anti-inflammatorydrugwithinthe24h,historyofalcoholor drugaddiction,presenceofneurologicdisordersor psychi-atricdisease.
All the patients were premedicated with 0.03mg/kg midozolam (Dormicum®) intramuscularly 30min prior to
their arrival tooperation theater. Patients were takento thepreoperativepreparationunitandweremonitored (non-invasive bloodpressure, heartrate andperipheral oxygen saturation while breathing room air) these values were recorded as control values. Patients were given 4 l/min oxygen through a mask, a 20G cannula was inserted for intravenous accessand10mL/kg0.09% salinewasinfused within 30min, afterwards the rate was set at 5mLkg/h. Bloodsamplestaken fromeach patientwhile opening the veinwascentrifugedtoseparatedplasmafromserumand storedinafreezerat−20◦C.
Allpatients had lumbar puncture underaseptic condi-tions, while sitting, between L3---4 or L 2---3 according to anesthesist’s preference. The lumbar puncture level was recorded.Skinandsubcutaneous2mL2%lidocaine(Aritmal®
5mLampoule)infiltrationanesthesiawasgivenwitha22G needle.AnesthesiawasbegunforGroupCSAwith2mL0.25% levobupivacaine after a 22G spinal catheter (Spinocath®)
wasplaced2---3cmintotheintrathecal interval.Afterthe 10thminifthelevelofsensoryblockhadnotreachedT10, anextra1mL0.25%levobupivacainewasgiventhroughthe catheter, this was repeated at 10min intervals until T10 blocklevelwasreached.Thetotaldoseoflevobupivacaine wasrecorded.
Spinal anesthesia was induced in group SDSA patients with12.5mg(2.5mL)0.5%levobupivacaineinjectedintothe intrathecalintervalwitha22GQuinkeneedle.
Aftertheinjectionbloodpressure,heartrate,SpO2,
15and45min.(MBS:0noparalysis,patientcanfullyflexfoot andknee;1Canonlymovekneeandfoot,cannotliftstraight leg;2cannotbendknee,canonlymovefoot;3full paraly-sis.)After45minthepatientsweretakentotheoperating room.
In both groups the time fromthe injection to sensory block level reachingdermatome T10 wasrecordedas the surgical anesthetic duration.It wasplanned thatpatients whoreacheddermatomeT10andabovesensoryblocklevel gave permission for the operation. After spinal injection untilMBS1wasreachedwasdenotedthemotorblock ini-tiation time.Fromthe injection topeakdermatome that is sensoryblock level reached maximum dermatome, was called the peak dermatome time. From the start of the surgicalproceduretotheendwastheoperationduration.
Sensoryblocklevelwascheckedusingthepin-pricktest (needle prick). Sensory block level was assumed to have reachedthedermatomewhenthepatientnolongerfeltthe needleprick.
Whenmeanarterialbloodpressure(MAP)decreased20% fromthe basal level hypotensionwasdiagnosed and5mg ephedrine HCL(Osel drugs) wasadministered. Heart rate below 50beatsper min wasaccepted asbradycardia and 0.5mgatropine(atropine1mLamp,Drogsan)was adminis-tered.Totalliquidsgiventothepatient,aswellasephedrine andatropinedoseswererecorded.
Patientstakentotheoperatingtheaterweremonitored usinganADUanestheticmonitor(Datex-Ohmeda®S/5
Anes-theticMonitor)for5-leadsurfaceelectrocardiogram(ECG, DII),SpO2andnon-invasivearterialbloodpressure.
After the operation finished the CSA group had the catheter removed. Both groups were given a PCA unit (AbbotPainManagementProvider)withivmorphine(bolus dose:2mg,lock-outtime30min)forpostoperative analge-sia.Fromintrathecal injectiontofirstuseofthePCA was recordedasthefirstanalgesicduration.
Following intrathecal injectionall patients were moni-tored at 50, 60, 70, 80, 90, 100, 110, 120, 150, 180min and 4, 6, 9, 12, 15, 18 and 24h. Values for blood pressure, heart rate, SpO2, VRS (verbal pain evaluation
scoring), sensory block level, MBS score, PCA machine requests (Dem), number of times drugs were adminis-teredbyPCA (Del)andtotal morphinegivenbyPCA were recorded.
Degree of painwasevaluated usingVRS (0:nopain; 1 slightpain;2moderate pain;3severe pain;4 verysevere pain; 5 unbearable pain). From peak dermatome sensory blockuntilitregressedtwolevelswasrecordedasthe sec-ond dermatome reductionduration. Fromspinal injection toMBSscoreof 0 wasrecordedasBromage scale 0 dura-tion.Eighthoursaftertheoperationbloodsamplesfromall patients werecentrifugedtoseparateserumfromplasma andstoredinafreezerat−20◦C.Attheendoftheresearch serumcortisolandplasmaadrenalinelevelsinpreoperative andpostoperativeblood samplesweremeasuredusingthe ELISAmethod.
Statisticalanalysis
SPSS11.5programwasusedforstatisticalanalysisofdata. The data was analyzed for normal distribution using the
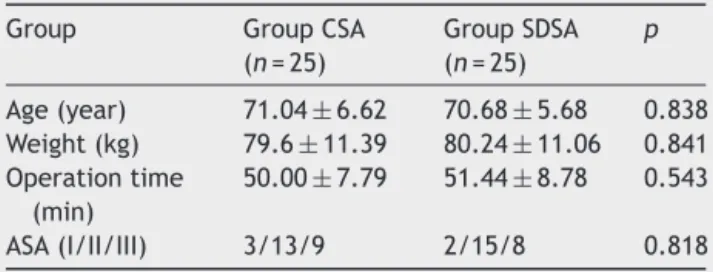
Table1 Demographicdata(mean±SD).
Group GroupCSA
(n=25)
GroupSDSA (n=25)
p
Age(year) 71.04±6.62 70.68±5.68 0.838 Weight(kg) 79.6±11.39 80.24±11.06 0.841 Operationtime
(min)
50.00±7.79 51.44±8.78 0.543
ASA(I/II/III) 3/13/9 2/15/8 0.818
Kolmogorov Smirnoff test. The Mann Whitney U test was
usedtocomparethefollowingcontinuousdatafromthetwo
groups:operationduration,height,weight,age,blood
pres-sure,heartrate,sensoryblocklevel,highestsensoryblock
level, sensory block dermatome T10 time, sensory block
twosegmentregressiontime,MBS,VRS,timeoffirst
anal-gesicdose, total analgesic use,PCA requests andnumber
oftimesdrugs wereadministeredbyPCADel/Demvalues,
totalatropineandephedrineuse,andcortisolandadrenalin
levels.To analyzetherepetition of thesedata withinthe
groups the Wilcoxon test was used. The chi-square test
was used to analyze frequency (%) results of ASA
physi-calclassification, lumbar puncture level, nausea-vomiting
andsideeffects.Descriptivestatisticsforthedatasuchas
meanand standard deviation (mean±SD),mode and
fre-quency (number and %) were determined. Graphs of the
changesindifferencebetweenthegroupsagainsttimewere
constructed. A value of p<0.05 was accepted as
signifi-cant.
Results
Thestudycomprisedatotalof50patientsin2groups,all
patientscompletedtheprotocol.
Demographicdata
Therewerenostatisticallysignificantdifferencesbetween
thetwogroupsin terms ofage, bodyweight,height,ASA
riskclassandoperationduration(Table1).
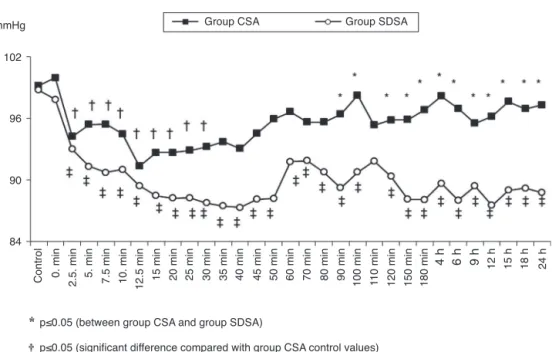
Hemodynamicchanges
Comparingthegroups blood pressurein the90, 100,120, 150,180minand4,6,9,12,15,18and24hafterintrathecal injectionthe CSA group was significantly higher than the SDSAgroup(p<0.05)(Fig.1).
WithintheCSAgroupbloodpressureinthe2.5,5,7.5,10, 12.5,15,20,25and30minafterintrathecalinjectionwas significantlylowerthanthecontrolvalues(p<0.05)(Fig.1). WithintheSDSAgroupwhenbloodpressurechangeswere examinedtheywerefoundtobesignificantlylowerthanthe controlvaluesatalltimes(p<0.05)(Fig.1).
102
96
90
84
Group CSA mmHg
p≤0.05 (between group CSA and group SDSA)
p≤0.05 (significant difference compared with group CSA control values)
p≤0.05 (significant difference compared with group SDSA control values)
Control 0. min 2.5. min 5. min 7.5 min 10. min 15 min 20 min 25 min 30 min 35 min 40 min 45 min 50 min 60 min 70 min 80 min 90 min 100 min 110 min 120 min 150 min 180 min
4 h 6 h 9 h 12 h 15 h 18 h 24 h
12.5 min
Group SDSA
Figure1 Changesinmeanarterialbloodpressure(MAP).*p<0.05(betweenGroup CSAandGroupSDSA).†p<0.05(significant
differencecomparedwithGroupCSAcontrolvalues).‡p<0.05(significantdifferencecomparedwithGroupSDSAcontrolvalues).
Group CSA
HR (beat/min)
76
Time 72
68
64
60
p≤0.05 (significant difference compared with group CSA control values)
p≤0.05 (significant difference compared with group SDSA control values)
Control 0. min 2.5. min 5. min 7.5 min 10. min 15 min 20 min 25 min 30 min 35 min 40 min 45 min 50 min 60 min 70 min 80 min 90 min 100 min 11
0 min
120 min 150 min 180 min 4 h 6 h 9 h
12 h 15 h 18 h 24 h
12.5 min
Group SDSA
Figure2 Changesinheartrate(HR).†p<0.05(significantdifferencecomparedwithGroupCSAcontrolvalues).‡p<0.05
(signifi-cantdifferencecomparedwithGroupSDSAcontrolvalues).
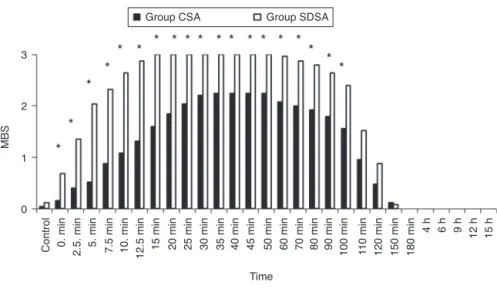
Anestheticproperties
LumbarpuncturewasperformedatL2---L3intervalin8and atL3---L4intervalin17patientsintheCSAgroup;6patients hadlumbarpuncture at L2---L3intervaland19patients at L3---L4intervalintheSDSAgroup.Therewasnostatistically significantdifferenceinlumbarpuncturelevelbetweenthe twogroups(p>0.05).
Comparing the groups modified Bromage scores (MBS) from5to120minvaluesweresignificantlyhigheringroup SDSAthaningroupCSA(p<0.05)(Fig.3).
Comparingthegroupssensoryblocklevelsat2.5,5,7.5, 10,12.5,15,20,25,30and35minafterintrathecalinjection theSDSAgroupvaluesweresignificantlyhigherthantheCSA group(p>0.05)(Fig.4).
Nostatisticallysignificantdifferencewasfoundbetween VRS scores for the groups (p>0.05). Average peak der-matome valueswereT8for theCSA group andT7for the SDSA group. There was no significant difference between thetwogroupspeakdermatomevalues(p>0.05).
Group CSA
MBS
3
2
0 1
Time
Control 0. min 2.5. min 5. min 7.5 min 10. min 15 min 20 min 25 min 30 min 35 min 40 min 45 min 50 min 60 min 70 min 80 min 90 min 100 min 110 min 120 min 150 min 180 min 4 h 6 h 9 h
12 h 15 h
12.5 min
Group SDSA
p≤0.05 (between group CSA and group SDSA)
Figure3 MBSchangesinthegroups.*p<0.05(betweenGroupCSAandGroupSDSA).
Table2 BlockTimes(min)(mean±SD).
Blocktimes GroupCSA(n=25) GroupSDSA(n=25) p
Timetoreachpeakdermatome 31.64±11.94 25.10±5.89 0.019*
Twosegmentregressiontime 79.28±18.66 90.08±14.66 0.030* Surgicaloperationtime 18.56±6.31 13.08±4.34 0.010*
Motorblockstarttime 13.04±7.10 6.04±2.30 0.000*
TimetoreachMBS0 170.28±51.32 186.04±35.13 0.211
Firstanalgesictime 268.88±94.52 253.60±92.46 0.566
* p<0.05(betweenGroupCSAandGroupSDSA).
timeintheSDSAgroupwassignificantlyshorterthaninthe CSA group. At thesame timethe twosegmentregression timewas significantlylonger in group SDSA than in group CSA(p<0.05)(Table2).Nosignificantdifferencewasfound
between the twogroups MBS0 and first use of analgesia times(p>0.05)(Table2).
GroupSDSAusedasignificantlyhigherdoseof levobupi-vacainethangroupCSA(p<0.05).Therewasnostatistically
p≤0.05 (between group CSA and group SDSA) Group CSA
Level
Th5
Th
L1
L5
S4
Time
Control 0. min 2.5. min 5. min 7.5 min 10. min 15 min 20 min 25 min 30 min 35 min 40 min 45 min 50 min 60 min 70 min 80 min 90 min 100 min 110 min 120 min 150 min 180 min
4 h 6 h 9 h
15 h
12 h
12.5 min
Group SDSA
Table3 Totaldrugsandliquidsgiven(mean±SD).
Totals GroupCSA(n=25) GroupSDSA(n=25) p
Totallevobupivacaine 8.70±1.63 12.50±0.00 0.000*
Totalmorphine 8.00±3.78 6.96±2.83 0.278
Totalephedrine 0.20±1.00 1.20±3.31 0.160
Totalatropine 0.02±0.1 0.04±0.13 0.561
Totalliquids 1290.20±180.01 1337.60±148.86 0.315
* p<0.05(betweenGroupCSAandGroupSDSA).
Table4 Preoperativeandpostoperativeadrenalinandcortisollevels(mean±SD).
Group GroupCSA(n=22) GroupSDSA(n=22) p
PreopAdrenalin 249.90±62.63 265.40±70.90 0.446
PostopAdrenalin 190.04±52.63† 180.76±54.77‡ 0.570
PreopCortisol 168.95±85.51 134.22±51.07 0.111
PostopCortisol 127.51±57.10† 89.37±32.98‡,* 0.010
* p<0.05(betweenGroupCSAandGroupSDSA).
† p<0.05(significantdifferencecomparedwithGroupCSAcontrolvalues).
‡ p<0.05(significantdifferencecomparedwithGroupSDSAcontrolvalues).
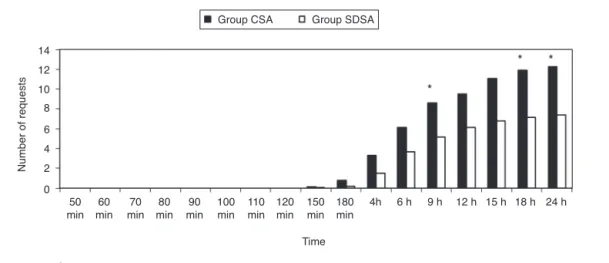
p≤0.05 (between group CSA and group SDSA) Group CSA
Number of requests
14
12
10
8
6
4
2
0 50 min
60 min
70 min
80 min
90 min
100 min
110 min
120 min
150 min
180 min
4h 6 h 9 h 12 h 15 h 18 h 24 h
Time Group SDSA
Figure5 AveragenumberofrequestsfromthePCAunit.*p<0.05(betweenGroupCSAandGroupSDSA).
significantdifferencebetweenthetwogroupsaverage con-sumption of morphine, ephedrine, atropine and liquids (p>0.05)(Table3).
Nodifference wasfound in thenumber of dosesgiven bythetwogroupsPCAmachines (p>0.05).Comparingthe numberofrequeststothePCA machinesat9,18and24h theCSA group requestswere significantlyhigher thanthe SDSAgroup(p<0.05)(Fig.5).
No significant difference was found between the two groupsplasmaadrenalinelevels(p>0.05)(Table4).
Withineachgrouppostoperativeplasmaadrenalinlevels weresignificantlylowerthanthepreoperativecontrollevels (p<0.05)(Table4).
Comparingthegroups’postoperativeserumcortisol lev-els,theSDSAgrouplevelsweresignificantlylowerthanthe CSAgrouplevels(p<0.05)(Table4).
Within both groups postoperativeserum cortisol levels were significantly lower than preoperative control levels (p<0.05)(Table4).
Comparingsideeffectsinbothgroups,whiletherewasno differencebetweenthegroupsintermsofnausea,vomiting, respiratorydepression,headacheandrash,lowerbackpain in group CSA wassignificantly greaterthan in group SDSA (p<0.05)(Table5).
Table5 Sideeffects(n,%).
Group GroupCSA
(n=25)
GroupSDSA (n=25)
p
Nausea: 0 2(8%) 0.153
Vomiting: 0 0 1.000
Respiratorydepression: 0 0 1.000
Headache: 0 1(4%) 0.317
Lowerbackpain: 9(36%) 2(8%) 0.018*
Rash: 0 0 1.000
Discussion
This study compared continuous spinal anesthesia with single-dose spinal anesthesia using levobupivacaine in geriatric patients undergoing transurethral urologic inter-ventions. We found that continuous spinal anesthesia provided better hemodynamic stability, shorter recovery periodsandequalanestheticquality.
Inolderpatientsincreasesinhealthproblemscombined with suppressed physiologic compensatory mechanisms meansthathemodynamic instabilitylinkedtospinal anes-thesia may bemore seriousand lastlonger. Rapid spread of sympathetic block in spinal anesthesia may cause an increase in morbidity, especially in older patients with reduced cardiovascular adaptation mechanisms.18 One of
the most important factors tobe awareof in patients of increased age and with accompanying diseases is hemo-dynamicstability. Inaprospective studyoncardiacarrest linkedtoanesthesiaBibouletetal.19 determinedthemost
importantfactorsincardiacarrestinpatientsover84and withan ASA risk factor of 3and above.They found inap-propriate anesthetic doses, hypovolemiaand hypoxia due todifficultykeepingtheairwayopen werethemost com-monreasonsfor cardiacarrest.Especiallyin patientswho are older, or have cardiovascular and respiratory system problems,evenlowdosesmayresultingreateranesthetic levels,sotechniquessuchasCSAwhichallowthepossibility of dose titrationshouldbe givenpreference comparedto SDSA.20
Favareletal.,21 inastudycomparingCSAandSDSAuse
of 0.5% hyperbaric bupivacaine, showed that blood pres-sure loweredlessin theCSA groupcomparedtotheSDSA group.The researchersfound thattheCSA grouphadless hemodynamicchangesandthattheslowerstartof segmen-talblockandslowdevelopmentofsympatheticblockmade adaptation easier.21 DeAndres etal.22 used 0.5% isobaric
bupivacaineintheircomparisonofCSAandSDSAandfound hypotensionduetotherepeateddoseintheCSAgroupdid notneedvasopressordrugswhiletheincidenceof hypoten-sionintheSDSAgroupwasgreater.
Klimschaetal.18 compared0.5%isobaricbupivacainein
CSA, SDSA and epiduralanesthesia. Bloodpressure in the CSAgroupdidnotreduce,incontinuousepidural anesthe-sia therewasa 15±3% reduction anda 19±2% decrease intheSDSAgroup.AcomparisonofSDSAwithCSAbyReisli etal.23foundasignificantreductioninbloodpressureinthe
SDSAgroupcomparedtotheCSAgroup.Labailleetal.24used
low dose 0.125% isobaric bupivacaine withCSA technique toprovideeffectiveanesthesiawithminimalhemodynamic changesinolderpatients. Minvilleetal.25 comparedSDSA
andCSA withlow dose bupivacaine in plannedhip opera-tionsinpatientsover75years.Occurrenceofhypotension intheCSA groupwas31%and68%intheSDSAgroup; seri-ous hypotensionwas 8% in the CSA group and 51% in the SDSA group. In the CSA group 4.5±2mg ephedrine was consumed, compared with 11±2mg in the SDSA group. TheyfoundtheCSAgroupwashemodynamicallymore sta-ble.
HoweverPitkanenetal.26comparedCSAandSDSA
tech-niquesinplannedhipandkneeoperationsin40patientsand foundnosignificantdifferenceinhemodynamicstabilityof thegroups.
This studyfound both groupshad lowerbloodpressure than the control values. In the CSA group 4% of patients developedhypotensioncomparedto12%intheSDSAgroup, subsequentlythedoseof ephedrineusedwaslowerinthe CSAgroup.ThelowerbloodpressureintheSDSAgroup com-paredtothe CSAgroup is similartoresults fromprevious studies. Results from the use of levobupivacaine for CSA showedthatit providesmore hemodynamic stabilitythan bupivacaineinCSA,inagreementwithpreviouslypublished research.
Patients under spinal anesthesia show a reduction in heartratedue topreganglion fiberblockage anda reduc-tionin left atriumpressure.8 Shenkman et al.27 usedlow
dosesoflocalanestheticwiththeCSAtechniquetoprovide goodcontrolofhemodynamicsandthisadvantageoverthe SDSAtechniquemadeitsuitableforuseinolderandmore highriskpatients.Theyfoundamaximumreductioninheart rateof7.2%using0.1%bupivacaineforCSAinASAIII---IVrisk grouppatients.The researchersfound thatusingCSA they couldmodifythesensoryblocklevelinacontrolledfashion andreduce the risk of hemodynamic instability.27 Favarel
etal.21 found nosignificantdifferencein heartrateusing
hyperbaricbupivacainefor CSAandSDSA.Similarresearch findingnosignificantdifferenceinheartratewhenusingCSA comparedtoSDSAisavailable.18,25,28Thisstudyfoundno
sig-nificantdifferenceinheartratebetweentheCSAandSDSA groupsatanytimeinterval,similartotheliterature.
Research evaluating CSA using levobupivacaine are limited. The only research in literature by Sell et al.14
foundtheminimumeffectivedose oflocalanestheticwas 11.7mgusinglevobupivacaine for CSA in hipreplacement operations.Ourstudyfoundanaveragedoseof8.7mg lev-obupivacaineprovidedsufficientanesthesia.Weareofthe opinionthat the differencemaybedue todemographics, position,intendedblocklevelandothersuchfactors.
This study found the time to reach dermatome T10 sensory block level was significantly longer in the CSA group than the SDSA group. This is similar to times to reachsensory block levels that allow surgery in previous research.21,22,29Whiletherewasnosignificantdifferencein
peakdermatome,thetimefortheCSAgrouptoreachpeak dermatome was significantly longer. This result conforms withpreviousstudies.18,28
Comparing Bromage scale evaluations of motor block leveltheCSA group wassignificantlylowerthan theSDSA group. While motor block is a desirable characteristic in surgeries suchas orthopedics, it delays neurologic evalu-ationpostoperatively and obstructs mobilization. Forthis reasonanearlyendtomotorblockisadesirableproperty. Thelowerdegree of,andearlyendto,motorblockinthe CSAgroupcouldbeseenasanadvantage.
SDSAgrouppatientsrequiredanaverageof12.5mg lev-obupivacainecomparedto8.7mgfortheCSAgroup.Though theCSA group usedless local anesthetic, sufficient anes-theticlevel,similartotheSDSAgroup,wasachieved.
groupcomparedtothe SDSAgroup.Itmayalsobedue to thelowerlocalanestheticdoseandlowernerveblocklevel intheCSAgroup.
It is known that epidural and spinal anesthesia at dif-ferentlevelssuppressestheneuroendocrinestressresponse better than general anesthetic. Highlevel spinal block is necessary to suppress the andrenergic response.30 Seitz
et al.31 found cortisol increased during surgery in lower
extremity operations using general anesthetic, while the epiduralanestheticgrouphadlowerlevelscomparedto val-uesfrombeforesurgery.Pfugetal.32foundhigherlevelsof
adrenalinpostoperativelycomparedtocontrolvalues.Low levelspinalanesthesiapreventsthisincrease,thehighlevel spinalanestheticgrouphadvalueslowerthanthecontrols. WhileMolleretal.33foundnodifferenceincortisollevelsin
thelatepostoperativeperiodcomparingspinalandgeneral anesthesia, during surgery and in the early postoperative periodcortisol levelswere lower in the spinal anesthesia group.Comparingthe postoperativeplasmaadrenalinand serumcortisollevelsinbothgroupsinthisstudy,bothgroups had lower levels compared to control values. The SDSA grouppostoperativeserumcortisollevelsweresignificantly lower.ThehighernerveblocklevelintheSDSAgroupmay be responsible for greater suppression of afferent neural impulsesoriginatinginthesplanchnicsympatheticnerves.
In conclusion continuous spinal anesthesia using 0.25% concentrationlevobupivacainetoprovideregional anesthe-siafortransurethralprostateresectionoperationsinolder patientscanbeusedsafely.
Conflict
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Kayhan Z. Bos¸altım Sistemi ve Anestezi, Klinik Anestezi. 3. Baskı. ˙IstanbulLogosYayıncılık.2004;15:388---405.
2.Morgan GE, Mikhail MS, Murray MJ. Genitoüriner Ameliyat-lardaAnestezi.KlinikAnesteziyoloji4Baskı ˙IstanbulGünes¸Tıp KitabevleriYayıncılık.2008;33:757---72.
3.Mebust WK, Holtgrewe HL, Cockett ATK, Peters PC. ve ark. Transurethral prostatectomy: immediate and postoperative complications----acooperativestudyof13participating institu-tionsevaluating3,885patients.JUrol.2002;167:5---9.
4.Dobson PM, Caldicott LD, Gerrish SP, Cole JR, Channer KS. Changesin haemodynamic variablesduring transurethral resection ofthe prostate: comparison of general and spinal anaesthesia.BrJAnaesth.1994;72:267---71.
5.MalhotraV,SudheendraV,DiwanS.Anesthesiaandtherenaland genitourinarysystems.In:MillerR,editor.Miller’sanesthesia, vol. 54,6thed.Philadelphia: ChurchillLivingstone;2005. p. 2175---208.
6.Rassweiler J,TeberD,Rainer KR,HofmannR. Complications oftransurethralresectionoftheprostate(TURP)----incidence. ManagePreventEurUrol.2006;50:969---80.
7.Cuvas O, Er AE, Ongen E, Basar H. Spinal anesthesia for transurethral resection operations:bupivacaine versus lev-obupivacaine.MinervaAnestesiol.2008;74:697---701.
8.KayhanZ.Lokal/BölgeselAnesteziYöntemleri.KlinikAnestezi 3Baskı ˙IstanbulLogosYayıncılık.2004;21:524---90.
9.BevacquaBK.Continuousspinalanaesthesia:what’snewand what’snot.BestPractResClinAnaesthesiol.2003;17:393---406.
10.DennyNM, Selander DE. Continuous spinalanaesthesia. Br J Anaesth.1998;81:590---7.
11.PitkanenM.Continuousspinalanesthesiaand analgesia.Tech RegAnesthPainManage.1998;2:96---102.
12.Erbüyün K, Ok G, Tekin ˙I. Sürekli Spinal ve Epidural AnesteziYöntemlerininAnestezik veHemodinamikEtkilerinin Kars¸ılas¸tırılması.FıratTıpDergisi.2007;12:201---5.
13.Yılmazlar A. Kontinü spinal anestezi. Anestezi Dergisi. 2002;10:12---7.
14.SellA,OlkkolaKT,JalonenJ,AantaaR.Minimumeffectivelocal anaestheticdoseofisobariclevobupivacaineand ropivacaine administeredviaaspinalcatheterforhipreplacementsurgery. BrJAnaesth.2005;94:239---42.
15.McLeod GA, Burke D. Levobupivacaine. Anaesthesia. 2001;56:331---41.
16.Mc Clellan KJ, Spencer CM. Levobupivacaine. Drugs. 1998;56:355---62.
17.MazoitJX,BoicoO,SamiiK.Myocardialuptakeofbupivacaine: II. Pharmacokinetics and pharmacodynamics of bupivacaine enantiomersintheisolatedperfusedrabbitheart.AnestAnalg. 1993;77:477---82.
18.Klimscha W, Weinstabl C, Ilias W, Mayer N, Kashanipour A, SchneiderB,etal.Continuousspinalanesthesiawitha micro-catheterandlow-dosebupivacainedecreasesthehemodynamic effects of centroneuraxisblocks in elderly patients. Anesth Analg.1993;77:275---80.
19.BibouletP,AubasP,DubourdieuJ,RubenovitchJ,CapdevilaX, d’AthisF.Fatalandnonfatalcardiacarrestsrelatedto anes-thesia.CanJAnaesth.2001;48:326---32.
20.BibouletPh,DeschadtJ,AubasP,VacherA,ChauvetPH. Con-tinuousspinal anesthesia:does lowdose plain or hyperbaric bupivacaineallowtheperformanceofhipsurgeryintheelderly? RegAnesth.1993;18:170---5.
21.Favarel-GarriguesJF,SztarkF,PetitjeanME,ThicoipeM,Lassie P,DabadieP.Hemodynamiceffectsofspinalanesthesiainthe elderly:singledoseversustitrationthroughacatheter.Anesth Analg.1996;82:312---6.
22.DeAndresJ,BeliverJ,BaluichesR.Comparisonofcontinuous spinalanaesthesiausinga32Gcatheterwithanaesthesiausing asingle24Gatraumaticneedleinyoungpatients.BrJAnaesth. 1994;73:747---50.
23.Reisli R, Horasanlı E, Demirbilek S, Dikmen B, Yi˘gitbas¸ B, Gö˘güs¸N. Tekdoz ve sürekli spinal anestezininhemodinamik veanesteziketkilerininkars¸ılas¸tırılması.TürkAnestReanCem Mecmuası.1999;27:21---6.
24.LabailleT,BenhamouD,WestermannJ.Hemodynamiceffects ofcontinuousspinalanesthesia:acomparativestudybetween low and high doses of bupivacaine. Reg Anesth. 1992;17: 193---6.
25.Minville V, Fourcade O, Grousset D, Chassery C, Nguyen L, Asehnoune K, et al. Spinal anesthesia using single injection small-dose bupivacaine versus continuous catheter injection techniquesforsurgicalrepairofhipfractureinelderlypatients. AnesthAnalg.2006;102:1559---63.
26.Pitkanen M, Rosenberg P, Silvanto M, Tuominen M. Haemodynamic changes during spinal anaesthesia with slowcontinuousinfusionorsingledose ofplainbupivacaine. ActaAnaesthesiolScand.1992;36:526---9.
27.ShenkmanZ,EidelmanLA,CotevS.Continuousspinal anaesthe-siausingastandardepiduralsetforextracorporealshockwave lithotripsy.CanJAnaesth.1997;44:1042---6.
29.SchniderTW,Mueller-DuysingS,JohrM,GerberH.Incremental dosingversussingle-dosespinalanesthesiaand hemodynamic stability.AnesthAnalg.1993;77:1174---8.
30.KehletH.ModificationsofresponsestosurgerybyNeural Block-ade.In:CousinsMJ,BridenbaughPO,editors.Neuralblockedin clinicalanesthesiaandmanagementofpain,vol.5. Lippincot-Raven;1998.p.129---75.
31.Seitz W, Luebbe N, Bechstein W, Fritz K, Kırchner E. A Comparison of two types of anaesthesia on the endocrine andmetabolic responsesto anaesthesiaand surgery.EuropJ Anaesth.1986;3:283---94.
32.Pflug AE, HalterJB. Effect of spinal anesthesia on adrener-gic toneand theneuroendocrineresponsestosurgical stress inhumans.Anesthesiology.1981;55:120126.