Arq Neuropsiquiatr 2009;67(2-A):305-307
305
Clinical / Scientiic note
OCulOCerebrOrenal SyndrOme Of lOwe
Magnetic resonance imaging indings in the irst six years of life
Arnolfo de Carvalho-Neto
1, Sergio Eiji Ono
1, Georgina de Melo Cardoso
1,
Mara Lucia Schmitz Ferreira Santos
2, Izabela Celidonio
3SíndrOme OCulOCerebrOrrenal de lOwe: aChadOS evOlutivOS de imagem de reSSOnânCia magnétiCa nOS primeirOS SeiS anOS de vida
Imaging Center: DAPI – Diagnóstico Avançado por Imagem, Curitiba PR, Brazil: 1Radiologist, Medical Center: Hospital Pequeno Príncipe, Curitiba PR,
Brazil: 2Child Neurologist; 3Child Neurologist Resident.
Received 5 August 2008, received in inal form 9 December 2008. Accepted 2 March 2009.
Dr. Sergio Eiji Ono – Rua Brigadeiro Franco 122 - 80430-120 Curitiba PR - Brasil. E-mail: ono.sergio@gmail.com The oculocerebrorenal syndrome of Lowe (OCRL), was
irst recognized as a distinct disease in 1952 by Drs. Lowe, Terrey and MacLachlan at Massachusetts General Hospi-tal, in Boston, USA, describing three male children with or-ganic aciduria, decreased renal ammonia production, hy-drophtalmos and mental retardation1. The X-linked
reces-sive inheritance pattern was recognized irst by LeFebvre2.
It is present in all races, with a predominance in those of Caucasian and Asian ancestries. Rarely females are affect-ed3. It is a very rare disease, with estimated prevalence in
the general population of 1 in 500,000. In USA the Lowe Syndrome Association (LSA) documented 190 living pa-tients in the year 2000 (0.67 × million inhabitants)4.
It is caused by a mutation in the gene encoding oc-ulocerebrorenal-Lowe protein (OCRL1), isolated in 1992, linked to the Xq24–q26 region of the X chromosome2,4-6.
Approximately 60% of OCRL patients demonstrate a loss of OCRL1 gene expression2, and the deinitive
laborato-ry test, that can be used for prenatal diagnosis, is the bio-chemical assay for deiciency of phosphatidylinositol 4,5-biphosphate 5-phosphate in cultured ibroblasts3.
The classic triad of eye, central nervous system, and kidney involvement are required for the diagnosis of Lowe’s syndrome4. Cataract is present at birth in all
pa-tients and glaucoma is detected within the irst year of life. Hypotonia compromises suction and causes serious respiratory problems in the irst period of life. Motor de-velopment is retarded and mental retardation is moderate or severe in almost all cases. Obsessivecompulsive behav-ior is typical. Seizure is seen in approximately 50% of the patients over 18 years old. Renal disease is primarily char-acterized by renal Fanconi syndrome but many children are asymptomatic at birth. Renal involvement is initially related to bicarbonate, salt and water wasting, causing fail-ure to thrive. Later, a signiicant number of patients
devel-op chronic renal failure. The treatment includes cataract extraction, glaucoma control, physical and speech ther-apy, drugs addressed to behavioral problems and correc-tion of the renal (tubular acidosis) and consequent bone diseases (rickets). Life span rarely exceeds 40 years4.
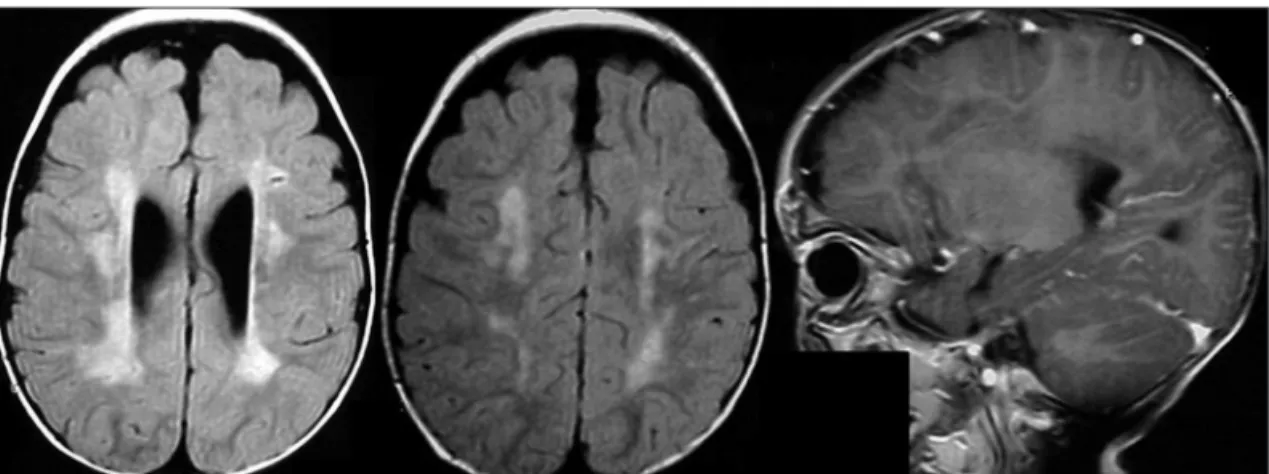
Brain magnetic resonance imaging (MRI) may show two patterns of lesions: hyperintensities on T2-weighted imag-es, and periventricular cystic lesions2,4-9. The present case
reports these indings in a time interval of 4 years, show-ing that initially the hyperintensities are seen, and after-wards, the cystic images. This pattern would help the ra-diologist and pediatric neurologist to reinforce the clin-ical diagnosis, as these patterns of images can be seen in other conditions.
CaSe
The present case report was approved by the Ethics Com-mittee of the Medical Center and has an informed consent giv-en by the pargiv-ents of the child. The patigiv-ent had conggiv-enital bilat-eral cataracts and underwent surgery at the age of 4 months. Afterwards he developed psychomotor retardation, hypotonia, hypoglicemia, dysmorphic facial features, dificulty in swallow-ing and severe behavior disturbances (irritability and self-muti-lation), which progressively worsened. Although he never had seizures, his electroencephalogram exam showed frontal lobe discharges. Renal impairment was detected at the age of 4 when laboratory tests revealed urinary calcium wasting. On the basis of the clinical course and the laboratory parameters, Lowe syn-drome was diagnosed.
diSCuSSiOn
bilat-Arq Neuropsiquiatr 2009;67(2-A)
306
Oculocerebrorenal syndrome of Lowe: MRI Carvalho-Neto et al.
eral hyperintensities seen on T2-weighted images in the periventricular white matter and in the centrum semio-vale. These are nonspeciic indings, but in the context of OCRL syndrome, this is considered gliosis8. The second
examination (Fig 2), done four years later, at six years of age, showed the appearance of cysts in the periventric-ular white matter that corresponds to perivascperiventric-ular lacu-nes in OCRL.
Reports in the past attributed the hyperintensities to demyelination6,7 or gliosis8, and not necessarily
correlat-ed with the severity of clinical manifestations7. Recent
studies and neurophatological data show evidences that these are due to gliosis. Schneider and Sener2,8 described
cases with proton MR spectroscopy reporting prominent myoinositol peaks, a glial marker, suggesting the presence of gliosis. But at the same time, it is not clear if these peaks could represent accumulation of phosphatidylinos-itol 4,5-biphosphate, a metabolite which is not degraded in patients with Lowe syndrome2. The gene product
do-main affected in OCRL patients is an inositol
polyphos-phate 5-phosphatase, located in the Golgi apparatus, that catalyzes the hydrolysis of the 5-position phosphate and controls cellular levels of phosphatidylinositol 4,5-biphos-phate (PtdIns 4,5-P2), a metabolite involved in Golgi vesic-ular transport. It has been postulated that the enzymatic deiciency lead the accumulation of PtdIns 4,5-P2 in lyso-somal membranes and therefore increased extracellular release of lysosomal enzymes. This would cause develop-mental defects in the lens and abnormal renal and neu-rological functions. In CNS the accumulation of lysosom-al products can lead to dilatation of perivascular spaces, whereas extracellular release of lysosomal enzymes can lead to toxic gliotic reactions2.
Neuropathological findings are limited, describing brain weight usually below normal, atrophy, ventricular enlargement and thinning of the corpus calosum. The me-ninges are diffusely ibrotic without inlammatory chang-es. The most frequent inding in the white matter is gliosis, mainly in the centrum semiovale and in the periventricu-lar region. Spongy changes have been observed, frequently Fig 1. MRI examination at 21 months of age. Axial FLAIR (luid-attenuated inversion recovery) and sagital
T1-weight-ed post gadolinium (MR contrast agent). T2 weightT1-weight-ed images show white matter hyperintensities in the periventricu-lar and centrum semiovale regions.
Arq Neuropsiquiatr 2009;67(2-A)
307
Oculocerebrorenal syndrome of Lowe: MRI Carvalho-Neto et al.
associated with perivascular lacunes. Active myelin break-down (demyelination) has never been reported3.
MR findings alone are sometimes nonspecific, and without clinical data the radiologist’s report could be mis-leading. Diffuse white matter abnormalities can be attrib-uted to several diseases and conditions. The OCRL syn-drome is diagnosed based on clinical and laboratory data, but this article may help the neuroradiologist to reinforce the diagnosis. The two MR indings seen in OCRL patients – hyperintensities and cysts – are well described in the literature, but to the best of our knowledge, there are vir-tually no reports describing the sequential appearance of these indings on MRI.
referenCeS
1. Lowe CU, Terrey M, MacLachan EA. Organic-aciduria, de-creased renal ammonia production, hydrophthalmos, and men-tal retardation; a clinical entity. Am J Dis Child 1952;83:164-184. 2. Schneider JF, Boltshauser E, Neuhaus TJ, Rauscher C, Martin
E. MRI and proton spectroscopy in Lowe syndrome. Neuro-pediatrics 2001;32:45-48.
3. Knaap MS, Valk J. Lowe syndrome. Magnetic resonance of myelination and myelin disorders. Third edition. New York: Springer 2005:387-391.
4. Loi M. Lowe syndrome. Orphanet J Rare Dis 2006;1:16. 5. Pueschel SM, Brem AS, Nittoli P. Central nervous system and
renal investigations in patients with Lowe syndrome. Child’s Nerv System 1992;8:45-48.
6. Carroll WJ, Woodruff WW, Cadman TE. MR indings in ocu -locerebrorenal syndrome. AJNR 1993;14:449-451.
7. Ono J, Harada K, Mano T, Yamamoto T, Okada S. MR ind -ings and neurological manifestations in Lowe oculocerebro-renal syndrome. Pediatr Neurol 1996;4:162-164.
8. Sener RN. Lowe syndrome: proton MR spectroscopy, and dif-fusion MR imaging. J Neuroradiol 2004; 31:238-240.