SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Original
Article
The
use
of
tranexamic
acid
in
patients
submitted
to
primary
total
hip
arthroplasty:
an
evaluation
of
its
impact
in
different
administration
protocols
夽
Gustavus
Lemos
Ribeiro
Melo
∗,
Daniel
Souza
Lages,
João
Lopo
Madureira
Junior,
Guilherme
de
Paula
Pellucci,
João
Wagner
Junqueira
Pellucci
RedeMaterDeideSaúde,BeloHorizonte,MG,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received30November2016 Accepted26January2017 Availableonline29July2017
Keywords: Hiparthroplasty Tranexamicacid Hemotransfusion
a
b
s
t
r
a
c
t
Objectives:Thereisstillnoconsensusastothebestformanddosagesofuseoftranexamic acid.Theaimofthisstudywastoevaluatetheuseoftranexamicacidintotalhip arthro-plasty,inordertoreducebloodlossanddecreasehemoglobin,takingintoaccountdifferent administrationprotocols.
Methods:42patientssubmittedtototalhiparthroplastyweredividedintothreegroups.The studywasprospectiveandrandomized.Group1receivedavenousdoseoftranexamicacid of15mg/kg,20minpriortobolusincision.Group2receivedanintravenousdoseof15mg/kg bolus,20minbeforetheincision,andanextradoseof10mg/kgbyinfusionpumpduringthe durationofthesurgicalprocedure.Patientsingroup3didnotreceivetranexamicacid,being thecontrolgroup.Pre-andpost-operativehemoglobinlevelsweremeasuredandbloodloss wasmeasured24haftersurgeryusingaPortovacdrain.
Results:TherewasasignificantreductionintheamountofbleedingthroughthePortovac drainandreductioninpostoperativehemoglobindropinpatientswhousedtranexamicacid. Therewasneithersignificantdifferenceinhemoglobindropbetweengroups1and2,nor wasthereaneedforhemotransfusion.Twopatientsingroup3requiredbloodtransfusion. Conclusions:Thefindings demonstrated thatthe useof intravenoustranexamicacidin totalhiparthroplastyreducedpostoperativebleedingratesandsignificantlyreducedserum hemoglobinwithout increasing thromboemboliceffects.The bolusandbolus+infusion pumpmethodswereshowntohaveasimilarinfluenceonhemoglobinandneedforblood transfusion.
©2017SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
夽
StudyconductedatRedeMaterDeideSaúde,BeloHorizonte,MG,Brazil. ∗ Correspondingauthor.
E-mail:gustavus.lemos@gmail.com(G.L.Melo). http://dx.doi.org/10.1016/j.rboe.2017.07.004
O
uso
do
ácido
tranexâmico
em
pacientes
submetidos
a
artroplastia
total
primária
do
quadril:
uma
avaliac¸ão
do
seu
impacto
em
diferentes
protocolos
de
administrac¸ão
Palavras-chave: Artroplastiadequadril Ácidotranexâmico Hemotransfusão
r
e
s
u
m
o
Objetivos: Aindanãoháconsensosobrequalamelhorformaequaisasdosagensdeuso doácidotranexâmico.Oobjetivodoestudofoiavaliarousodoácidotranexâmicona artro-plastiatotaldoquadrilquantoàreduc¸ãodaperdasanguíneaequedadehemoglobina. Levaram-seemconsiderac¸ãodiferentesprotocolosdeadministrac¸ão.
Métodos: Foramdivididosemtrêsgrupos42pacientessubmetidosàartroplastiatotaldo quadril.Oestudofoiprospectivoerandomizado.Ogrupo1recebeuumadosevenosade ácidotranexâmicode15mg/kg20minutosantesdeincisão,embólus.Ogrupo2recebeu umadoseendovenosade15mg/kgembólus,20minutosantesdaincisão,eumadoseextra de10mg/kgatravésdebombadeinfusãoduranteadurac¸ãodoprocedimentocirúrgico.Os pacientesdogrupo3–controle–nãoreceberamácidotranexâmico.Foramfeitasdosagens dehemoglobinapréepós-operatoriamenteefoimedidaaperdasanguíneaem24horas apósacirurgiaatravésdousodedrenoportovac.
Resultados: Houveumareduc¸ãosignificativanaquantidadedesangramentoatravésdo dreno portovace reduc¸ãonaqueda da hemoglobinapós-operatórianospacientesque usaramácido tranexâmico.Nãohouvediferenc¸asignificativanaquedadehemoglobina entreosgrupos1e2,assimcomonãohouvenecessidadedehemotransfusão.Doispacientes dogrupo3necessitaramdehemotransfusão.
Conclusões: Osachadosdemonstraramqueousodoácidotranexâmicoporviaendovenosa naartroplastiatotaldoquadrilreduziuastaxasdesangramentonopós-operatórioequeda dahemoglobinaséricadeformasignificativa,semaumentarosefeitostromboembólicos. Osmétodosbólusebólus+bombadeinfusãodemonstraramterumainfluênciasemelhante quantoàhemoglobina,perdasanguíneaatravésdosdrenosenecessidadede hemotrans-fusão.
©2017SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Totalhiparthroplasty(THA)hasbecomeanexcellent treat-mentmethodforpainreliefandfunctionalimprovementin patientswithdegenerativehipjointdisease.Initially,its indi-cationwasrestrictedtoelderlypatientswithlowerfunctional demands.However,surgicaltechniqueimprovementsandthe evolutionofimplantsanditsfrictionsurfaces,whichprovide lesswearandtear,havewidenedtheuniverseofpatientswho couldbenefitfromthisprocedure.1
Perioperativebloodlossisacommoncauseof complica-tionsofthisprocedure.2Bleedingcomplicationsmayhinder thesuccessofanysurgery.3 Inrecentyears,severalauthors havereportedontheperioperativeadministrationof tranex-amicacid (TXA) and its beneficial effectin reducing blood loss.4
TXAhasbeenusedtoreducebloodlossandtheneedfor transfusionintotalhipandkneearthroplasty,withvarying results.5
TXA is a synthetic antifibrinolytic drug whose effect resultsfromthe formationofareversiblecomplex of plas-minogen and plasmin; it inhibits fibrinolysisand prevents lysis ofthe fibrin clot, and actsin the partial blockade of plasmin-induced platelet aggregation.6 TXA can provide a hemostaticbenefitinrecurrentorexcessivebleedingdueto
stabilizationoffibrinstructuresandpreventionofclot disso-lution,especiallywhenfibrinformationisimpaired.Itseffect onthepreservationofthefibrinmatrixcanfurtherenhance collagen synthesis and increase the elastic force of the tissue.7
TXAisquicklyabsorbed.Approximately90%ofanIVdose isexcreted intheurine within24h; theplasmahalf-life is of approximately 2h, and the therapeutic levelsare main-tainedfor6–8h.Itsactionpreservestheclotandmakesthe hemostaticmechanismmoreefficient,reducingtheintensity andriskofbleeding;itcanbeadministeredintravenouslyor topically.8
Currently,thereisenoughclinicalevidencetorecommend the use of TXAto reducepostoperative blood lossin total knee and hip arthroplasty. However, its optimal dose and regimensofadministrationareunknown.9Athigh concentra-tions,TXAcanbeadirectnoncompetitiveplasmininhibitor. Peak plasmalevelsare achieved5–15minafterintravenous administration.7 Duetoitslowcostandminorsideeffects, researchindifferentpartsoftheworldhasbeenconductedto assessTXA’seffectivenessincontrollingperioperative bleed-ingduringmajorsurgery.6
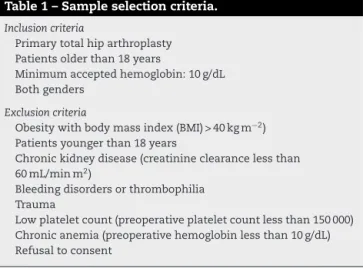
Table1–Sampleselectioncriteria.
Inclusioncriteria
Primarytotalhiparthroplasty Patientsolderthan18years
Minimumacceptedhemoglobin:10g/dL Bothgenders
Exclusioncriteria
Obesitywithbodymassindex(BMI)>40kgm−2) Patientsyoungerthan18years
Chronickidneydisease(creatinineclearancelessthan 60mL/minm2)
Bleedingdisordersorthrombophilia Trauma
Lowplateletcount(preoperativeplateletcountlessthan150000) Chronicanemia(preoperativehemoglobinlessthan10g/dL) Refusaltoconsent
theimmunomodulationrelatedtohomologous transfusion,
whichhasbeenofincreasingconcernespeciallyconsidering
theincreaseintheprevalenceofinfectionsinimplanted
pros-theses, immunosuppression, and the previously evidenced
associationwiththeappearanceofneoplasminpatientswho
receivethistypeoftransfusion.10
Perioperative bleeding may require blood transfusions, whichhavetheirowncomplicationsandrisks,andincrease thecostsofhealthcare.Amongotherpreventionmethods,the effectivenessoftreatmentwithTXAinreducingsurgicalblood losshasbeendemonstrated,especiallyintheimmediate post-operativeperiod.11
Thus,thisstudyaimedtoprovetheefficacyofTXAintotal hiparthroplastieswhencomparedwitha controlgroup, to identifypossiblecomplications,and toestablishacriterion fortheidealuseofTXA.
Material
and
methods
Thestudy included42 patientssubmitted toprimaryTHA, operated bythe same team of surgeons, from February to November 2016.In this prospectiveand randomizedstudy, patientsweredividedintothreegroups.Group1receivedTXA ina15mg/kgIVbolusdose20minbeforeincisionrespecting amaximumdoseof2g.Group2receivedTXAina15mg/kg IVbolus dose 20min before incision and an extra dose of 10mg/kg using an infusion pump throughout the surgical procedure.Group3,thecontrolgroup,didnotreceiveTXA. Pre- and postoperative hemoglobin levels were measured; blood losswas measured within24hafter surgeryusing a Portovacdrain.Themeanperi-andpostoperativebleeding, hemoglobindecrease,and needforblood transfusion were comparedamongthethreegroups.Table1presentsthe inclu-sionandexclusioncriteria.
Statisticalanalysis
Resultswereexpressedasmeans±standarddeviations(SD). One-wayANOVAwasusedforcomparingthemeans,asthis wasacomparisonofthreeindependentgroups.The normal-ityassumptionswereverifiedwiththeShapiro–Wilktest,and variancehomogeneity was assessedusing the Levenetest. Finally,theTukeytestwasusedtoassesswhichdifferences
were statisticallysignificant.Resultswere consideredtobe statisticallysignificantwhenp<0.05.Thestatisticalanalyses wereperformedwithIBMStatisticsSPSSversion19.
Results
According to the preoperative inclusion criteria (Table 1), patients in group 1 (bolus), group 2 (bolus and pump), and group 3 (control) had mean hemoglobin levels above 10g/dL:14.33mL/dL(95%CI:13.05–15.55),13.73mL/dL(95%CI: 11.97–15.49),and13.96mL/dL(95%CI:12.47–15.44;p=0.575), respectively. Therefore, the groups were homogeneous regardingpreoperativehemoglobin,withnostatistically sig-nificantdifference,whichreducedthechanceofinterference duetodiscrepantpreoperativehemoglobinvalues(Fig.1).
Twenty-four hours after the primary THA procedure, a hemoglobindecreasewasobservedinthethreegroups, great-est in group 3 (Fig. 2). The mean hemoglobin level was 11.60mL/dL(95%CI:10.18–13.02)ingroup1;11.11mL/dL(95% CI:9.53–12.70)ingroup2;and10.37mL/dL(95%CI:8.67–12.07; p=0.130)ingroup3.Thesedatademonstrateastatistically sig-nificanthemoglobindecreaseingroup3inrelationtogroups 1and2,demonstratingthebeneficialeffectofTXAregarding hemoglobindecreaseinthefirst24hofthesurgicalprocedure. After 48hofthe primary THA procedure, ahemoglobin decreasewasagainobservedinthethreegroups,anditwas alsogreatestingroup3(Fig.2).Themeanhemoglobinlevel was10.92mL/dL(95%CI:9.53–12.30)ingroup1;10.89mL/dL (95% CI: 9.44–12.33) in group 2; and 9.70mL/dL (95% CI: 8.45–10.95;p=0.053)ingroup3.Thesedatademonstratea sta-tisticallysignificanthemoglobindecreaseingroup3inrelation togroups1and2,demonstratingthebenefitsofTXAregarding hemoglobindecreaseinthefirst48hofthesurgicalprocedure (Fig.3).
The mean blood loss through the Portovac were 289.69mL (95% CI: 146.90–432.48) in group 1; 250.00mL (95% CI:113.73–386.27) in group 2; and 437.92mL(95% CI: 218.40–657.44;p=0.017)ingroup3.
Group3presentedstatisticallysignificanthigherbloodloss throughthePortovacdrainwhencomparedtogroup1(bolus) andgroup2(bolusandpump),asshowninFig.4.Therefore, it canbeconcludedthattherewasasignificantincreasein the volumeofbleedingmeasuredinthePortovacdrainsof patients ingroup 3comparedtogroups1and 2,a statisti-callysignificantvalue.Itagainsuggestsabeneficialeffectof TXAregardingdecreasedbleeding.Nostatisticallysignificant differenceswereobservedbetweengroups1and2.
Discussion
Hemoglobina pré operatória por grupo
13,96
HG Pré
13,73
0,0 2,0 4,0 6,0 8,0 10,0 12,0 14,0 16,0
14,33
Controle Bolus e bomba
Bolus
16,0
15,0 17,0
14,0
13,0
12,0
11,0
Controle Bolus e bomba
Grupo Bolus
Fig.1–Comparisonofpreoperativehemoglobinbygroup.
Hemoglobina 24 horas por grupo
11,60
0,0 2,0 4,0 6,0 8,0 10,0 12,0 14,0 16,0
Controle Bolus e bomba
Bolus
HG 24h
14,0
12,0
10,0
8,0
Controle Bolus e bomba
Grupo Bolus
11,11
10,37
Fig.2–Comparisonof24-hhemoglobinbygroup.
Hemoglobina 48 horas por grupo
9,70 10,89
10,92
0,0 2,0 4,0 6,0 8,0 10,0 12,0 14,0 16,0
Controle Bolus e bomba
Bolus Bolus e bomba Controle
Grupo Bolus
HG 48h
14,0
12,0
10,0
8,0
33
Fig.3–Comparisonof48-hhemoglobinbygroup.
Dreno total por grupo
289,69
437,92
250,00
0,0 100,0 200,0 300,0 400,0 500,0
Controle Bolus e bomba
Bolus Bolus e bomba Controle
Grupo Bolus
1000
800
600
Dreno total
400
200
0
40
34
groupwassignificantlylowerthanthatofthecontrolgroup at2,4,6,8,10,and 12h.Regarding thetime ofalterations related to postoperative blood loss, asignificant reduction wasobservedinthefirst2haftersurgeryintheTXAgroup (p<0.001).After2h,nosignificantdifferenceswereobserved betweentheTXAgroupandthecontrolgroup.Preoperative administrationofTXAreducedpostoperativebloodlossatup to12h,aswellasthetotalbleedingincementedTHA,dueto thereductionofbloodlossduringthefirst2haftersurgery.
Zhouet al.13 have shown that TXA reduced blood loss and transfusion requirements inpatients undergoingTHA. Theuse ofTXAsignificantlyreducedmeantotalblood loss onameanvolumeof305.27mL(95%CI:−397.66to−212.89; p<0.001);being86.33mLmeanintraoperativebloodloss(95% CI:−152.29to−20.37;p=0.01);176.79mLmeanpostoperative blood (95%CI:−236.78to−116.39; p<0.001); and152.70mL meanoccultbloodloss(95%CI:−187.98to−117.42;p<0.001). Thisresultedinasignificantreductionintheproportionof patientswhoneededbloodtransfusions(oddsratio0.28;95% CI:0.19–0.42;p<0.001). There was nosignificant difference in the occurrence of deep venous thrombosis, pulmonary embolism,orothercomplicationsbetweenstudygroups,or thecostordurationofhospitalization.
Rochaetal.6reportedaprotocolinwhichTXAwasusedat aloadingdoseof10mg/kgbodyweight,administeredduring the30minpriortoskinincision.Themaximumdoseof2gof drugwasobserved.Aftertheincisionwasmade,continuous infusionofTXAwasmaintainedatarateof30mg/kg/huntil theskinwassutured.Theseauthorsalsoreportedthatthis protocolhasbeensafelyusedinothercenters.
In a randomized controlled trial comparing the effect of TXA and fibrin spray on blood loss in cemented THA, McConnelletal.14administeredasingle10mg/kgbolusdose ofintravenous TXAduringanesthesiainduction.According totheseauthors,themanufacturerdidnotspecifya recom-mendeddose forthis surgery,thereforethe dose andtime werechosenbythem,basedonpreviousstudies,whichhave demonstratedtheeffectivenessofabolusdoseof10mg/kg duringinductioninhiparthroplasty.Arandomized, double-blindedstudyassessedtheeffectofTXAonbloodlossand blood transfusions in 40 primary THAs. TXA at a dose of 10mg/kgbodyweight,or placebo,wereadministered intra-venouslyshortlybeforesurgery.Bloodlossduringoperation andpostoperativedrainageweremeasured,aswellasserum hemoglobin concentrations. An ultrasound scan was per-formedoneweekpostoperativelytoestimatebloodlossdue toremaininghematomas.Totalbloodloss(surgery+drainage) was0.76(95%CI:0.63–0.89)intheTXAgroup,and1.0(95%CI: 0.81–1.2)intheplacebogroup(p=0.03).Thenumberofblood transfusionsonthedayofsurgerywas2vs.10(p=0.07)and totalnumberofbloodtransfusionsduringthehospitalization periodwas5vs.13(p=0.2).Onepatient ineach grouphad pulmonaryembolism.15
In a prospective, randomized, double-blinded study, Husted et al.16 studied 40 patients scheduled for primary THA to determine the effect of TXA on perioperative and postoperativebloodlossandonthenumberofblood trans-fusionsrequired.Thesepatientswererandomizedtoreceive TXA(10mg/kgadministered asanintravenousbolus injec-tion,followedbyacontinuousinfusionof1mg/kg/hfor10h)
orplacebo(20mLsalinesolution,intravenously)15minbefore incision.Peri-andpostoperativebloodloss(recordedatdrain removal,24haftertheoperation)were recorded,aswellas thenumberofbloodtransfusions.PatientswhoreceivedTXA hadameanperioperativebloodlossof480mLvs.622mLin patientsreceivingplacebo(p=0.3);meanpostoperativeblood loss of 334mLvs. 609mL (p=0.001);mean total blood loss of814mLvs.1231mL(p=0.001),and atotalneedforblood transfusionsof4vs.25(p=0.04).Nopatientinanygrouphad deepvenousthrombosis,pulmonaryembolism,orprolonged wounddrainage.
Inelectivesurgery,TXAreducestheneedforblood trans-fusionbyapproximately30%,withoutaffectingmortalityor increasingpostoperativecomplications.Intrauma,TXAwas recently associated with a reduction in the mortality rate inalargenumber oftrauma patientswithbleeding.17 TXA significantlydecreasespostoperativebloodlossina remark-abledifference(50–460mL).Totalperioperativebloodlosswas reduced by 440mL on average.18 Drugs such as TXA and aminocaproicacidhavebeenusedinlargeelectivesurgeries topreventfibrinolysisbyreducingthenumberofblood trans-fusions.However,althoughtheiruseisveryattractiveforthe coagulopathyoftrauma,therearecurrentlynodatafrom stud-iesinhumansthatsupportitsroutineapplicationintrauma.19 IntravenousTXAcanreducebloodloss13,20 andtheneedfor transfusioninpatientsundergoingTHA,withoutincreasing theriskofcomplications.13Thereislittledataregardingthe adverseeffectsofthisdrug.Itrarelycauseshypotensionand retinalalteration.Itsprolongedsystemicuseincreasestherisk ofthromboembolicphenomena;itiscontraindicatedinacute thrombopathiesandshouldbeusedwithcautioninpatients withaknowntendencyforthrombosis.21Studiesontheuse ofTXAshowedinterestingresults,butitsbenefitsinTHAhave notbeenwellestablished.22
Conclusion
Thefindingsofthepresentstudydemonstratedthattheuse ofintravenousTXAinTHAreducedtheratesofpostoperative bleeding and,consequently,significant decreasedin serum hemoglobinwasobservedingroups1(bolus)and2(bolusand infusionpump)whencomparedtogroup3(control:didnot receiveTXA).Therefore,therewasareductionintheneedfor bloodtransfusion,whichwasrequiredfortwopatientsinthe controlgroup.Patientsingroups1and2didnotrequireblood transfusion.Regardingthedifferentadministrationprotocols, theuseofbolusandbolusaddedtoinfusionpumpmethods haveshown averysimilarinfluenceonserum hemoglobin and the amountofblood lossthroughPortovacdrains; the differenceswerenotstatisticallysignificant.
Nothromboemboliceffectswereobservedinthepatients ofthisstudy.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. RabelloBT,CabralFP,FreitasE,PenedoJ,CuryMB,RinaldiER, etal.Artroplastiatotaldoquadrilnãocimentadaem pacientescomartritereumatoide.RevBrasOrtop. 2008;43(8):336–42.
2. ClavéA,FazilleauF,DumserD,LacroixJ.Efficacyof
tranexamicacidonbloodlossafterprimarycementlesstotal hipreplacementwithrivaroxabanthromboprophylaxis:a case–controlstudyin70patients.OrthopTraumatolSurgRes. 2012;98(5):484–90.
3. MoreiraNetoFF(Dissertac¸ão)Usoprofiláticodoacido tranexamicoemcirurgiacardíacafeitacomauxílioda circulac¸ãoextracorpórea.Campinas:UniversidadeEstadual deCampinas;2000.
4. deJongeT.Pharmacologicalreductionofbleedingduringhip endoprostheticreplacement.OrvHetil.2012;153(41):1607–12. 5. HoKM,IsmailH.Usodeácidotranexâmicoporvia
intravenosaparareduziratransfusãodesanguealogênico emtotaldequadrileartroplastiadojoelho:umametanálise. AnaesthIntensiveCare.2003;31(5):529–37.
6. RochaVM,BarrosAGC,GomesNL,SilvaLEC,SchettinoLCV, LoboJC,etal.Usodoácidotranexâmiconocontroledo sangramentodecirurgiasdeescoliosetoracolombarcom instrumentac¸ãoposterior.RevBrasOrtop.2015;50(2):226–31. 7. PradoTD,RibeiroRG,DamascenoAD,NardiAB.Hemostasiae
procedimentosanti-hemorrágicos.Agrarianacademy– centrocientificoconhecer,vol.1(1);2014.p.214.Available from:
http://www.conhecer.org.br/agrarian%20academy/2014a/ Hemostasis.pdf[accessed01.2016].
8. SadigurskiD,AndionD,BoureauP,FerreiraMC,CarneiroRJF, ColavolpePO.Effectoftranexamicacidonbleedingcontrolin totalkneearthroplasty.ActaOrtopBras.2016;24(3):131–6. 9. Castro-MenéndezM,Pena-PazS,Rocha-GarcíaF,
Rodríguez-CasasN,Huici-IzcoR,Montero-ViéitesA.Efficacy of2grammesofintravenoustransexamicacidinthe reductionofpost-surgicalbleedingaftertotalhipandknee replacement.RevEspCirOrtopTraumatol.2016;60(5):315–24.
10.VolquindD,ZardoRA,WinklerBC,LonderoBB,ZanelattoN, LeichtweisGP.Usodoácidotranexâmicoemartroplastiatotal primáriadejoelho:repercussõesnaperdasanguínea perioperatória.RevBrasAnestesiol.2015;66:254–8. 11.Aguilera-RoigX,Jordán-SalesM,Natera-CisnerosL,
Monllau-GarcíaJC,Martínez-ZapataMJ.Tranexamicacidin orthopedicsurgery.RevEspCirOrtopTraumatol.
2014;58(1):52–6.
12.YamasakiS,MasuharaK,FujiT.Tranexamicacidreduces bloodlossaftercementlesstotalhiparthroplasty-prospective randomizedstudyin40cases.IntOrthop.2004;28(2): 69–73.
13.ZhouXD,TaoLJ,LiJ,WuLD.Dowereallyneedtranexamic acidintotalhiparthroplasty?Ameta-analysisofnineteen randomizedcontrolledtrials.ArchOrthopTraumaSurg. 2013;133(7):1017–27.
14.McConnellJS,ShewaleS,MunroNA,ShahK,DeakinAH, KinninmonthAW.Reductionofbloodlossinprimaryhip arthroplastywithtranexamicacidorfibrinspray.Acta Orthop.2011;82(6):660–3.
15.BenoniG,FredinH,KnebelR,NilssonP.Bloodconservation withtranexamicacidintotalhiparthroplasty:arandomized, double-blindstudyin40primaryoperations.ActaOrthop Scand.2001;72(5):442–8.
16.HustedH,BløndL,Sonne-HolmS,HolmG,JacobsenTW, GebuhrP.Tranexamicacidreducesbloodlossandblood transfusionsinprimarytotalhiparthroplasty:aprospective randomizeddouble-blindstudyin40patients.ActaOrthop Scand.2003;74(6):665–9.
17.LuzL,SankarankuttyA,PassosE,RizoliS,FragaGP,
NascimentoBJr.Tranexamicacidfortraumatichemorrhage. RevColBrasCir.2012;39(1):77–80.
18.RamosMFW,MoraisAC,SantanaJA,ChavesRA,SeiberlichE. Antifibrinolíticoemcirurgiacardíaca:comoequandousar? RevMedMinasGerais.2011;212Suppl.3:S3–8.
19.NascimentoBJr,ScarpeliniS,RizoliS.Coagulopatiano trauma.Medicina(RibeirãoPreto).2007;40(4):509–17.
20.TsutsumimotoT,ShimogataM,OhtaH,YuiM,YodaI,Misawa H.Tranexamicacidreducesperioperativebloodlossin cervicallaminoplasty:aprospectiverandomizedstudy.Spine (PhilaPa1976).2011;36(23):1913–8.
21.AlbuquerqueGC,CarvalhoCRS,OliveiraCR,TerraDP,Quinete SS.Telangiectasiahemorrágicahereditária:ácido
tranexâmiconotratamentodeúlceraplantar.AnBras Dermatol.2005;80Suppl.3:S373–5.
22.JohanssonT,PetterssonLG,LisanderB.Tranexamicacidin totalhiparthroplastysavesbloodandmoney:arandomized, double-blindstudyin100patients.ActaOrthop.