r e v b r a s o r t o p . 2016;51(5):489–500
SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Review
article
Diagnosis
and
treatment
of
osteochondral
lesions
of
the
ankle:
current
concepts
夽
Marcelo
Pires
Prado
a,∗,
John
G.
Kennedy
b,
Fernando
Raduan
c,
Caio
Nery
daHospitalIsraelitaAlbertEinstein,SãoPaulo,SP,Brazil
bHospitalforSpecialSurgery,NewYork,UnitedStates
cUniversidadeFederaldeSãoPaulo,EscolaPaulistadeMedicina,DepartamentodeOrtopediaeTraumatologia,SãoPaulo,SP,Brazil
dUniversidadeFederaldeSãoPaulo,SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received29September2015 Accepted5October2015 Availableonline17August2016
Keywords:
Ankleinjuries/diagnosis Ankleinjuries/therapy Osteochondritis/diagnosis Osteochondritis/therapy Talus
a
b
s
t
r
a
c
t
Weconductedawide-rangingreviewoftheliteratureregardingosteochondrallesionsof theankle,withtheaimofpresentingthecurrentconcepts,treatmentoptions,trendsand futureperspectivesrelatingtothistopic.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http://
creativecommons.org/licenses/by-nc-nd/4.0/).
Diagnóstico
e
tratamento
das
lesões
osteocondrais
do
tornozelo:
conceitos
atuais
Palavras-chave: Traumatismosdo tornozelo/diagnóstico
Traumatismosdotornozelo/terapia Osteocondrite/diagnóstico Osteocondrite/terapia Tálus
r
e
s
u
m
o
Osautoresfazemumarevisãoampladaliteraturaarespeitodaslesõesosteocondraisdo tornozelo,comointuitodeexporosconceitosatuaissobreotema,asopc¸õesdetratamento, astendênciaseasperspectivas.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevierEditora Ltda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http://
creativecommons.org/licenses/by-nc-nd/4.0/).
夽
StudyconductedatHospitalIsraelitaAlbertEinstein,SãoPaulo,SP,Brazil,andHospitalforSpecialSurgery,NewYork,UnitedStates.
∗ Correspondingauthor.
E-mail:mpprado@einstein.br(M.P.Prado).
http://dx.doi.org/10.1016/j.rboe.2016.08.007
Introduction
Lesionsofchondralandosteochondraltissuesoftheankleare commonlyrelatedtoanklesprain,1whichaffectsoneinevery 10,000individualsintheUnitedStatesdaily.
Although there is relative agreement in the literature
regarding the microtraumatic etiology of osteochondral
lesionsofthetalus,whenthefocusofattentionshiftstothe diagnosis and treatment, thisbecomes acontroversialand extremelydynamicsubject,whichjustifytheinterestto elab-oratethepresentstudy,whosemainobjectivewastoupdate thediagnosticandtherapeuticapproachesoftheseinjuries.
Material
and
methods
Thisreviewandupdatearticleassessedstudiesrelatedtothe treatmentofosteochondrallesionsthataffecttheanklejoint. Prospectiveandrandomizedstudies,caseseries,and system-aticreviewswereincluded.
Diagnosis
Thesuspecteddiagnosisofosteochondrallesionsofthetalus startswithcomplaintsofpainrelatedtophysicalactivities, usually with a history of previous trauma. Joint swelling, sensationofinstability,jointblockage,or extremelypainful clampingmayoccur.
Despitetheaforementionedcomplaints,physical exami-nationisrathervagueandislimitedtodiffusetendernessof
thejointduringflexionandmaximumextension,and touch-sensitiveareasonthetibiotalarjointline.
Testinganklestabilityisessentialforthediagnosisof insta-bility,whichisfrequentlyassociatedwithoristhemaincause oftheosteochondralankleinjury.
Despitethegreatchanceoffalse-negativediagnoses, sim-pleankleradiographsinAP,lateral,andobliquearethefirst imagingtobeobtainedinthediagnosticprocessof osteochon-drallesionsofthetalus.2
Themostcommonfindinginsimpleradiologyisthe pres-ence ofpoorly definedradiolucent area in the talar dome,
in the place where the pathological process has become
installed.
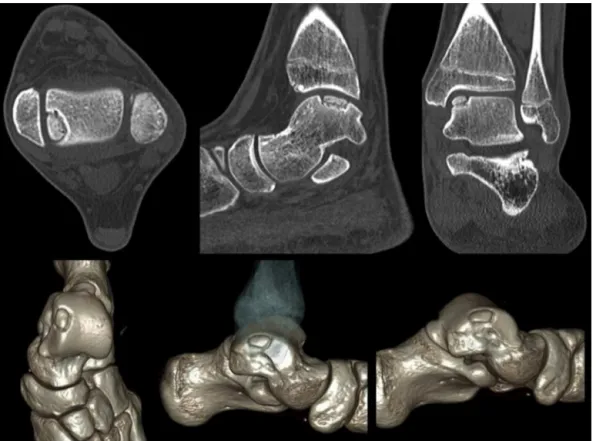
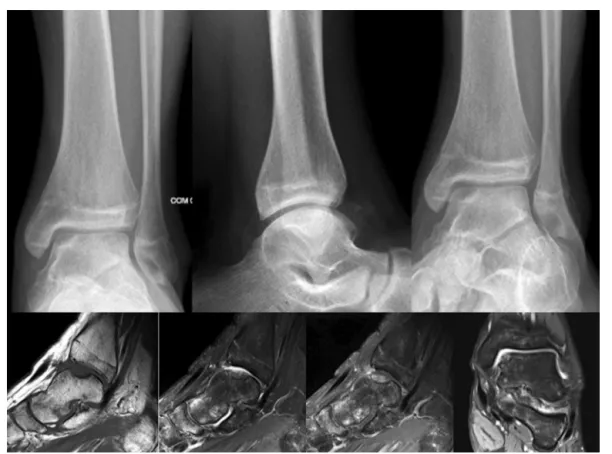
Themainlimitationofcomputedtomography(CT)isthe inabilitytoprovidedataonthequalityofthearticular carti-lage;however,itisthemainresourceintheevaluationofbone changesassociatedwithinjury,measurement,andlocation, aswellasinthedefinitionofthedeviationsofthefragments, andthereforeithastheabilitytoclassifythelesions3(Fig.1). Magneticresonanceimaging(MRI)providesinformation, allowingfortheassessmentofarticularcartilageandpresence ofsubchondralinflammatorychanges,aswellasforthe iden-tificationofthedepthofthechondrallesion.4,5Itistherefore regardedasthegoldstandardinthediagnosisof osteochon-drallesions6,7(Fig.2).
The most widespread classification for osteochondral
lesionsofthetalusisthatproposedbyBerndtandHarty8in 1959;itisbasedonthedegreeofdisplacementofthe osteo-chondralfragmentandhasfourstages:StageI–smallfocal subchondraltrabecularcompressionarea;StageII–partially loosefragment(incompletefracture);StageIII–loosefragment
rev bras ortop.2 0 1 6;51(5):489–500
491
Fig.2–X-raysoftheankleandmagneticresonanceimagingofapatientwhounderwentarthroscopictreatmentwith debridementandmicrofractures.
(completefracture),but notdisplaced;andStageIV–loose fragment(completefracture)anddisplacedfromitsbed.
In2001,ScrantonandMcDermott9addedStageVtothe classificationofBerndt&Harty,characterizedbythepresence ofosteochondralcystswithasizecorrespondingtothatofthe originalinjury,justbelowthedamagedarticularsurface.
Mintzetal.4combinedarthroscopicobservationswithMRI todesigntheirratingforosteochondrallesionsofthetalus, followingthesamedynamicsoftheotherclassifications.Six differentstagesarepossible:Stage0–normalcartilage;Stage 1 – hypersignal cartilage on MRI, but normal arthroscopic appearance;Stage2–fibrillationandcracksthatdonotreach thebone;Stage3–presenceofcartilageflap,withexposureof thesubchondralbone;Stage4–loosefragment,non-diverted; Stage5–divertedfragment.
Despitetheknownpossibilityofoverestimationofinjuries, thereisaclearandwell-definedtrendintheliteraturetovalue imagesofosteochondrallesionsofthetalusobtainedbyMRI,10 especiallythoseofhigh-resolution,11 due totheirexcellent correlationwith arthroscopicfindings, afact whichgreatly helpsintherapyplanningandprognosis.
Prognostic
factors
Size
Currently, there appearsto be aconsensus on the indica-tion ofarthroscopic treatmentforosteochondrallesions of
thetalussmallerthan1.5cm2,evenforrecurrentlesions.11–13
Therecommendedarthroscopictreatmentisdebridementof
theinjuredarea,withresectionoffreeorpartially-detached osteochondralfragments,followedbystimulationofthebone marrowthroughdrillingormicrofracturesofthesubchondral bone.14,15
Location
The location ofthe lesions influences the prognosismuch
moreduetothereparativetissuestability(retention)thanto the areaorthe quadrantinwhichthelesion ispositioned. Itisknownthatlesionslocatedintheroundedareasofthe articularsurface,alsoknownastalarshoulders,offermore precariousconditionstostabilizetherepairtissue– uncon-tained injuries – and therefore they have a less favorable prognosis.12,16
Without good quality edges, the scar that formsis less stable, increasingthe chancesofmechanically unfavorable formationoffibrocartilage,17richintypeIcollagen.
Age
Thepatient’s ageattheonsetoftheinjuryisconsideredto beanimportantprognosticfactor.18 However,thereis con-troversyover thisclaim, assomeauthorsfailed toobserve
differences in results when considering only age, having
Subchondralcystsanddepth
Theoccurrenceofsubchondralcysticlesionsindicatespoor prognosis.9,20Poorresultscanbeexpectedin53%ofpatients inthisgroup.21–23
Otherpossibleprognosticfactors
Chondrallesionsvs.osteochondrallesions
Throughtheobservationof283patientsforanaverageof52 months,Choietal.24observednodifferencesintheprognosis ofinjuriesthatinvolvedonlythechondrallayersfromthose thatsurpassedthesubchondralboneplate.
Bodyweightloadsupport
Whilesomeauthorsbelievethatearlyloadingdoesnot inter-ferewiththefinalresultofsmallosteochondrallesions,25Gill etal.26histologicallydemonstratedthatmaintenanceofload limitationinthepostoperativeperioddefinitivelyinfluences thefillingspeedandthequalityoftherepairtissuein osteo-chondrallesions.
Spinalcordedema
Theclinicalpictureandtheprognosisofosteochondrallesions areinverselyrelatedtotheintensityofbonemarrowedema observedintheMRI.27
Jointinstabilityandtrauma28
Treatment. The treatment of osteochondral lesions of the
talus should be restricted to symptomatic lesions. The
occasional finding ofasymptomatic osteochondral lesions,
regardlessoflocation,type, and size,should be communi-catedtothepatientorhis/herrelatives;thecaseshouldbe followed-up at regular intervals in search of possiblejoint deterioration.29
Conservativetreatment. Thenon-surgicaltreatment modali-tiesavailableintheliteratureincludemodificationofactivities of daily living, intra-articular steroid infiltration, use of orthotics,loadsuppression,anduseofimmobilizingbootsand orthoses.8,11
Theresultsofthistypeoftreatmentdonotexceed45%30; itisneitherconsistentnorpredictable.31
TheplasmarichingrowthfactorsisaformofPRP con-sidered to be a biological carrier of a complex mixture of bioactiveproteinsessential to the normalhealing process, havingpotentialeffectsontherepairofosteochondrallesions andarthrosis.32,33Thesefindingsandtherapeuticapplications stillrequirefurtherstudiestoconsolidatetheirapplicabilityin dailypractice.
Surgical treatment. Surgical treatment of osteochondral
ankle injuries can be divided into five main groups of
procedures17,34:
1. Reductionandfixationofosteochondralfragments
2. Bonemarrowstimulation
3. Articularcartilagereplacement 4. Regenerativecelltherapy 5. Metalimplants
Reductionandfixationofosteochondralfragments
Acuteosteochondralfracturesareproducedmostlybyinjuries afterankleinversion.
Under these conditions, patient should be treated with urgencyand,whenfeasible,thefragmentsshouldbereduced
and set in their original bed. The procedure can be done
arthroscopicallyandthefragmentscanbefixedwithfixation dartsorabsorbablescrews,asbothofwhichprovideexcellent functionalresults.
Smallerordevitalizedfragmentsareresected,andthebase ofthelesionistreatedbystimulatingthebonemarrow.
Despite the good prognosisfor fracture consolidation,a deteriorationofthecartilage thatcoversthefragmentscan beexpectedinone-thirdofthecases.
Bonemarrowstimulation
Ifthearticularcartilagehasonlysoftenedzones (chondroma-lacia)orfibrillationwithoutexposureofthesubchondralbone, andthereisgoodstabilityofthetissue,surfacedebridement and“chondralsealing”withtheuseofradiofrequencycanbe performed.35
Anterogradedrillingandmicrofractures
Therationalebehindmultidrillingormicrofracturesforthe treatmentofosteochondrallesionsofthetalusisbasedonthe perforationofthesubchondralbone,allowingthecontactof the bonemarrowwiththelesion.Inadditiontothe
migra-tion ofmultipotent mesenchymal cells into the bed ofthe
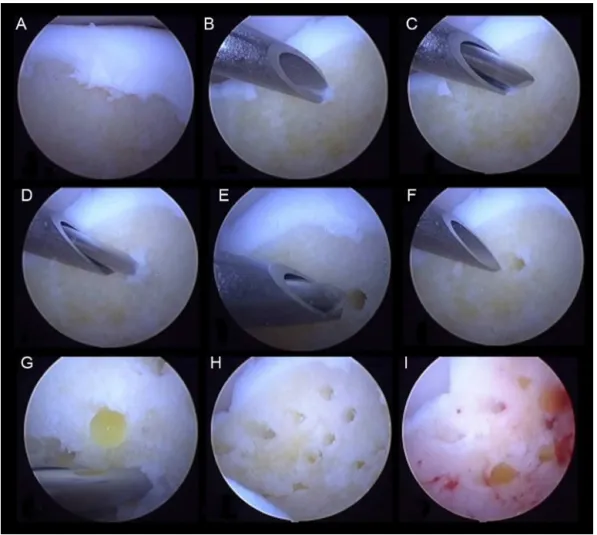
wound,localneovascularizationisalsoinduced,withcellular affluxtotherepairzone.Somebasicrulesmustbefollowed toensurethesuccessoftheseprocedures:(1)theedgesofthe lesionshouldbecurettedandthesoftenedtissueshouldbe removeduntilthehealthycartilage,firmlyadheredtothe sub-chondralbone,isreached;(2)theedgesshouldbeasregular andperpendicularaspossible;(3)drillingormicrofracturesin
thesubchondralbonemustbemadeperpendicularlytothe
surfaceat3–4-mmintervals;(4)thedepthshouldbeatleast 3mmtoensurethatthesubchondralbonehasbeencrossed; and(5)theprocedureshouldbestartedintheperipheryofthe lesionandfinishinthecenter29(Fig.3).Thefindingof bleed-inginthebaseoftheinjuryfromthesubchondralcapillaryis essential.Thebloodthatisdepositedinthebaseofthelesion containsprogenitorcellsandcytokinesresponsiblefor initi-atingthehealingprocess,whichinvolvestheformationofa fibrinclotandsubsequentformationoffibrousscartissuethat willundergometaplasiaintofibrocartilaginoustissue(Fig.4)
withlessresistancetocompressionandshearforceswhen
comparedwiththenormalarticularcartilagetissue.
Asystematicreviewdemonstratedtheconsistencyofthe resultsobtainedwiththetreatmentofosteochondrallesions
throughdebridementandmicrofractures,withmeanAOFAS
score of 86.8 points, achieving 80.2% excellent and good
results36; however, significant deterioration of results was observedafter4.2yearsoftheprocedure.17
In amorerecent meta-analysis,the successof combin-ingexcisionoffragments,curettageofthebaseoftheinjury,
andbonemarrowstimulationwas85%,comparedwith32%
rev bras ortop.2 0 1 6;51(5):489–500
493
Fig.3–Drillinginthebaseofosteochondrallesionsofthetalus.
resultsfromexcisioncombinedwithcurettageofthebaseof theinjury.37
Therepetitionofthedebridementprocess,curettage,and bonemarrowstimulationinpatientswithunfavorable evolu-tionreached92%goodresults,characterizedbyreturntoprior sportingactivities,includingprofessionalactivity.38
The result of microfractures can be enhanced by
hyaluronate intra-articular injection immediately after
surgery, with improved function and pain results when
comparedtopatientswhodidnotreceivesuchtreatment.39 Animalmodelsusingplatelet-richplasmainconjunction
with bone marrow stimulation procedures showed better
repairofthejointcartilagewhencomparedwithisolated sur-gicalprocedure,althoughhyalinecartilagewasnotobtainedin thefinalresult.40Thesameistruefortheuseofbonemarrow aspirateconcentrate.41
Retrogradedrilling
Retrogradedrillingwithradiographiccontrolisconsideredto beaveryeffectivetreatmentoptionforosteochondrallesions oftheintactjointcartilage.41Afterplacingaguidewireinthe lesionwiththeaidoffluoroscopyandarthroscopy,a cannu-lateddrillispassedoverthisguidewireandneverexceedsthe intactcartilage.Throughthetunnelformed,itispossibleto placethebonegrafttofillthelesion.Currently,various mod-elsofarticulatedandextremelyefficientguidinginstruments helpthesurgeontolocatethelesionandreachitsafely.
Articularcartilagereplacement
Autologousosteochondralgraft
The osteochondral autologous grafting system known as
mosaicplastyinvolvesobtainingcylindricalcartilageandbone grafts,mostcommonlyoriginatingfromthe lateralfemoral
condyles, and transferring them to areas of osteochondral
lesionintheloadingsurfaceofthetalardome.Thisprocedure presentsencouragingresults.
The indications for osteochondral grafting comprise
lesions largerthan 1.5cm2,recurrent orrefractorytomore
conservativetreatmentmethods,andespeciallylesions asso-ciatedwithsubchondralcysts.42
Mosaicoplastyhastechnicalstandardsthat mustbe fol-lowed inordertoachieve betterresults:(1) the donorarea canneverbealoadbearingregion;(2)osteochondralcylinders mustbeinsertedperpendicularlytothereceivingsurface;(3) thecartilageportionshouldhavetheshapeandcurvatureas closetothereceivingzoneaspossible;(4)thecylindermust beatleast15mminlengthforchondrallesionsand25mmin thepresenceofsubchondralcysts;(5)thecartilageplugmust remainperfectlyleveledwiththeedgesofthereceivingregion; stepsorunevennessregardingtheneighboringcartilageare notacceptable29,43(Fig.5).
Followingtheindicationsforeachprocedure,theresultsof osteochondralautologousgraftsaresuperiortothe combina-tionofdebridementandmicrofractures.44
Thenumberofgraftsused,previousprocedures,theneed
for osteotomy of the malleolus, and the presenceof mild
osteoarthritisoftheaffectedjointdonotinfluencethefinal outcomeofthisprocedure.
Regarding the donor area, the most frequent residual
symptomsareafeelingofinstabilityduringactivitiesofdaily
livingandpain, presentin11%ofpatientswho underwent
surgery.45Theoccurrenceofthesesymptomsisrelatedtovery largeparapatellarincisionsandexaggeratedtensioning
dur-ing the closure. Theknee prognosisdoes notappeartobe
affectedbythenumberofremovedgrafts,graftsize,orage ofthepatient.46
Osteochondralallograft
When osteochondrallesions exceed3cm2, become
uncon-tained,affecttheshoulderofthetalus,orareaccompanied
rev bras ortop.2 0 1 6;51(5):489–500
495
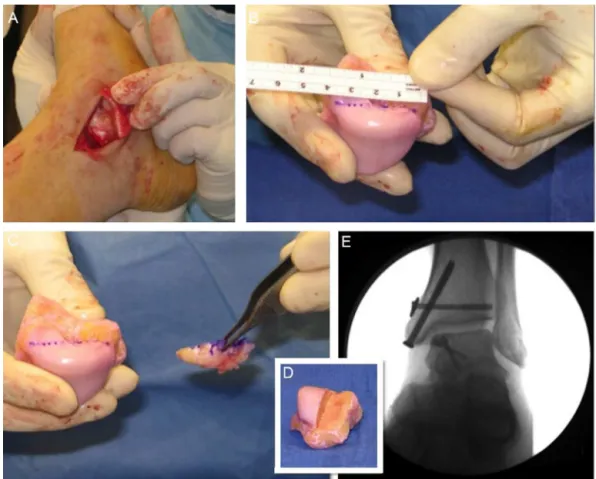
Fig.6–Osteochondralhomograftusedforthetreatmentofextensivemedialtalarshoulderinjury(TheauthorsthankDr. MarkS.Myersonfortheauthorizationtousethesefigures).
bylargesubchondralcysts,osteochondralautograftspresent technicaldifficulties,withagreater chanceofpoorresults. Insuchcases,freshcadaverallograft,withviable chondro-cytesandnormalsubchondralbone,appearsasaninteresting option, especiallybecauseit does notpresentmorbidity in thedonorareaorareaswithoutcoveragebetweenthegrafted plugs47(Fig.6).
Cryopreservationleadstoasignificantdeclineinthe num-berofviablechondrocytes.Thecellsurvivalfallsto20–30%in twoweeks,theperiodduringwhichtheprocedureshouldbe done.
Despitetheperspective ofgoodresults,the methodhas somemainobstacles:thetransmissionofdiseases,the pos-sibilityof adverse immunereaction, and difficulty in graft incorporationintothebed.
There is consensusamong the authors to consider the
osteochondralallograftasasalvagetreatmentforlargelesions
and for those where other methods have failed
repeat-edly.However,thehighincidenceofprocedurefailure(30%)
and of secondary procedures (40%) should be taken into
account.48,49
Regenerativecelltherapy
Autologouschondrocyteimplantation
The procedure begins by obtaining viable chondrocytes
throughresectionofasmallfragmentofthehealthycartilage tissuefromthejointtobetreatedorfromanotherjointfrom
thesameindividual.Thechondrocytesareisolatedand cul-turedforthreetosixweeksinordertomultiply.Thesecond partoftheprocedureisthepreparationofthereceivingarea and theimplantationofthe culturedcells.50 Curettageand debridement ofthe baseand edgesoftheinjuryuntilthey establishthelimitsofhealthycartilage,firmlyadheredtothe subchondralbone,areanintegralpartofthisprocess.Possible subchondralcystsarefilledwithcancellousgraftand perios-teumbladesintheappropriatedimensionswhicharesutured andgluedwithfibrintotheedgesofthelesion,inorderto createanairtightchamber,insidewhichtheculturedcellsare implanted(Fig.7).
Indicationsforthistherapyincluderecurrent osteochon-drallesionsofanysizeandprimarytreatmentoflargerlesions than 2.5cm2 withorwithoutsubchondralcysts inpatients
agedbetween15and55years,withoutdegenerativearthritis ormirror-imageosteochondrallesions,andwithoutinstability orchangesinjointalignment.51
Thecomplications,especiallythose relatedtoperiosteal
hypertrophy and delamination of the membranes used in
woundcoverage,reach18–33%ofcases.52
Inordertoreducemorbidityandthetechnicaldifficultyof autologouschondrocyteimplantation,variousattemptshave beenmaderegardingthecarrierforculturedchondralcells.
Acombinationoffibrinandthrombin(Chondron,Sewon
Fig.7–Autologouschondrocyteimplantation(sandwichtechnique).
Thesecond generationofautologouschondrocyte trans-plantsinvolvesthe useofcollagenmembranesforcarrying thecells,whicheliminatestheneedforobtainingthe perios-teumand allthe difficultiesand complicationsinherentto this period of the operation, and the results obtained are encouraging.54
The autologous chondrocyte implantation through an
arthroscopic procedure was a step forward. This
achieve-mentwasonlypossibleduetotheuseofaflexiblecollagen
membrane called matrix-induced autologous chondrocyte
implantation(MACI).55
Mesenchymalstemcells
Stemcelltherapyisbasedontwomechanismsofaction.At first,the cellsdifferentiateand mimicthefinalcells of tis-suesandorgans;then,thereistheproductionofsubstances (cytokinesand growth factors) that favorablyinfluencethe angiogenesisandthereductionofcellapoptosis,andinduce theendogenousregeneration.
Gianniniet al.demonstrated theefficiencyofthe useof stemcellsobtainedfromconcentrationofaspiratedbone mar-roworbonemarrow-derivedcelltransplantation(BMDCT)in clinicaltrials,56albeitwithapossibletendencytoward deteri-orationoftheresults.57
Stem cells derived from fat have a better potential for chondrogenesis58;thoseobtainedfromthesynovium appar-entlyhavegooddifferentiationintochondrocytes,butonlyin animalstudies.59
Intra-articularinjectionofmesenchymalstemcells(MSC) favorablyinfluencedtheresultsoftreatmentofpatientsolder than 50 yearswith lesionslarger than 109mm2 associated
withsubchondralcysts,andmayhavesomebenefitin
low-eringthespeedofevolutiontodegenerativedisease.
Chondrogenesisinductionbyautologousmatrix
The use a combination of collagen membranes withMSC,
bonemarrowconcentrate(BMC),andbonemarrow-derived
rev bras ortop.2 0 1 6;51(5):489–500
497
MSC(BMSC)hasbeenshowntobemoreadvantageousthan
chondrocyteimplantation.57
Inthe matrix-induced chondrogenesis technique, autol-ogouschondrocytes(matrix-associatedautologous chondro-cytetransplantation/implantation[MACT/MACI])areseeded intoatypeIandIIIacellularcollagenmatrixthatisplaced intheclotformedaftermicrofracturetoprovideafavorable environmentforchondralregeneration.Clinicalresultswith fiveyearsoffollow-upareencouraging.60
Particulatedjuvenilearticularcartilage
Stimulation of osteochondral talar lesions repair can be
madefromthearticularcartilageofchildrenandadolescents
cadavers,particulatedinto1-mmcubesimplantedinthe pre-viously preparedbed ofthelesion (DeNovoNaturalTissue, ZimmerInc.,Warsaw,USA).Afterarthroscopicaldebridement andpreparationofthelesion,thesalineflowisinterrupted andtheinjuryisdried.Athinlayeroffibrin glueisapplied acrosstheextentofchondrallesionandtheparticulate carti-lageisinsertedtocoverthefullosteochondraldefect.Anew fibrin layerisappliedoverthe regionsoastoincrease the stabilityofthegraft.Studieswithanimalmodelsand short-termfollow-upinpatientshaveshowngoodresults,withthe formationofhyalinecartilageinthedefects(Fig.8).
Theinitialclinical resultsare good61; inlesions smaller than1.5cm2thesuccessratereaches92%goodresults.62
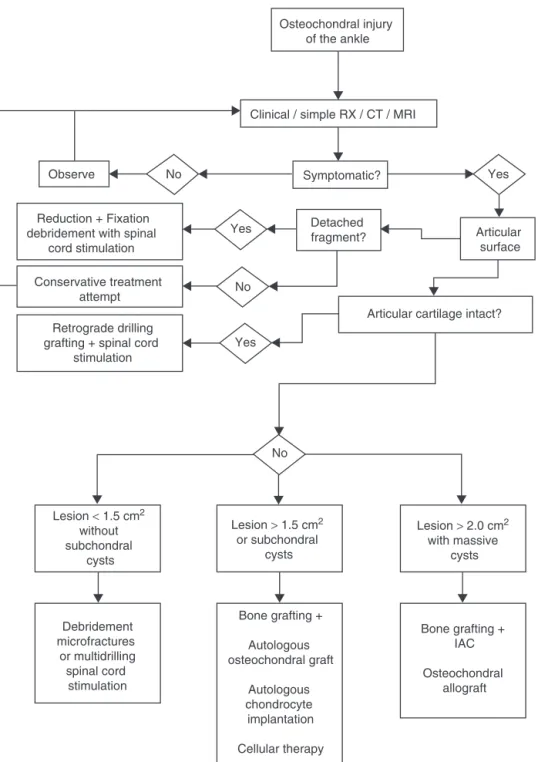
Osteochondral injury of the ankle
Clinical / simple RX / CT / MRI
Symptomatic?
Yes
Yes
Detached
fragment? Articular
surface
Articular cartilage intact?
Yes No
No
No Observe
Reduction + Fixation debridement with spinal
cord stimulation
Conservative treatment attempt
Retrograde drilling grafting + spinal cord
stimulation
Lesion < 1.5 cm2
without subchondral
cysts
Debridement microfractures
or multidrilling spinal cord
stimulation
Bone grafting +
Autologous osteochondral graft
Autologous chondrocyte
implantation
Cellular therapy
Bone grafting + IAC
Osteochondral allograft Lesion > 1.5 cm2
or subchondral cysts
Lesion > 2.0 cm2 with massive
cysts
Metalimplants
Filling ofthe talar osteochondrallesion area with the use ofmetallicimplants–surfaceprostheses–aimstoredothe contouroftheinjuredareaandenhancethedistributionof loadsontheanklejoint.Itisconsideredavalidmethodfor thetreatmentofosteochondrallesionsthatarerecurrentand refractorytootherformsoftreatment.63
Osteochondral
lesions
of
the
distal
tibia
Osteochondral lesions of the distal third of the tibia are unusualfindings,appearingin2.6%ofallosteochondralankle injuries.64
Thislowerincidencemayberelatedtotheconcaveshape oftheinferiorarticularsurfaceofthetibiaandtothegreater resistanceofthetibialcartilagetocompressionwhen com-paredwiththetalarcartilage.65,66
Thetreatmentoftheseinjuriesismorecomplexduetothe difficultyofaccessandtotheshapeofthearticularsurface ofthetibia. Curettage,excisionoffragments,thermal abla-tion,andstimulationofbonemarrowcanbedonethroughan arthroscopicapproach.
Whencystsarepresent,fillingwithbonegraftcanbedone throughthetransmalleolarapproach,witharthroscopic assis-tance.
The consensus among authors is that osteochondral
lesionsofthetibiahaveaworseprognosisthan osteochon-drallesionsofthetaluswhenconsideringthesamephysical characteristicsofthelesions.
Assessment
of
the
repaired
cartilage
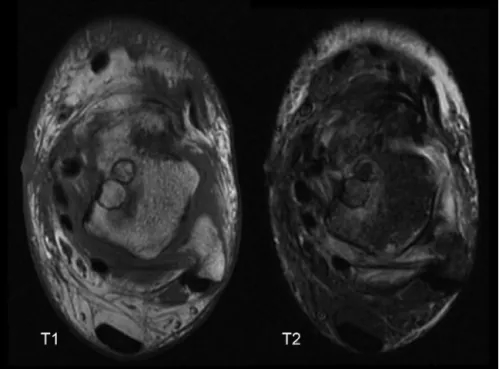
T2-weightedMRImappingisbecomingthemostusefuland
popularresource for the assessment ofthe repaired artic-ular cartilage, as an important alternative to arthroscopy, whichisaninvasiveprocedurenotfreefromcomplications. Asanaddedadvantage,MRIassessmentsincludetherepaired regionasawhole,whilearthroscopyhasamorerestrictedand superficialfieldofvisionthanalocalbiopsywouldprovide.67 TheintegrationoftheMocartmorphologicalscale
param-etersandbiochemicalmappingthroughT2-weightedMRIis
essentialforacompleteandaccuratenoninvasiveassessment oftherepairedcartilage,improvingtheinterpretationofthe clinicalscales.Mapping issuitableforaqualitative assess-mentofcartilage,beingabletodistinguishhyalinecartilage fromfibrocartilageandtocorrelatewithclinicaloutcomes.67
Theflowchart(Fig.9)presents themostcommon occur-rences,aswellassolutionsthataresupportedintheliterature. SomeofthesolutionspresentedarenotavailableinBrazil,
which does notpreclude knowledgeofthem and research
optionsforpatientswhopresenttheproblemslistedinthis article.
Final
remarks
Systematicreviewsoftheliterature,duetothe heterogene-ityoftheavailablestudies,donotallowforthedefinitionof
absolutestandardsofconduct.41However,thereisimportant
informationabout the efficiencyofthe treatmentmethods
with their respective success rates. With this information, orthopedists are able tosupport their choices, despite the lackofmathematicalconfirmation,untilthemuch-expected prospective, comparative, well-controlled studies are con-ducted.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.BaltzerAW,ArnoldJP.Bone-cartilagetransplantationfrom
theipsilateralkneeforchondrallesionsofthetalus.
Arthroscopy.2005;21(2):159–66.
2.DheerS,KhanM,ZogaAC,MorrisonWB.Limitationsof
radiographsinevaluatingnon-displacedosteochondral
lesionsofthetalus.SkeletalRadiol.2012;41(4):415–21.
3.FerkelRD,FlanniganBD,ElkinsBS.Magneticresonance
imagingofthefootandankle:correlationofnormalanatomy
withpathologicconditions.FootAnkle.1991;11(5):289–305.
4.MintzDN,TashjianGS,ConnellDA,DelandJT,O’MalleyM,
PotterHG.Osteochondrallesionsofthetalus:anewmagnetic
resonancegradingsystemwitharthroscopiccorrelation.
Arthroscopy.2003;19(4):353–9.
5.LüsseS,ClaassenH,GehrkeT,HassenpflugJ,SchünkeM,
HellerM,etal.Evaluationofwatercontentbyspatially
resolvedtransverserelaxationtimesofhumanarticular
cartilage.MagnResonImaging.2000;18(4):423–30.
6.CutticaDJ,SmithWB,HyerCF,PhilbinTM,BerletGC.
Osteochondrallesionsofthetalus:predictorsofclinical
outcome.FootAnkleInt.2011;32(11):1045–51.
7.O’LoughlinPF,HeyworthBE,KennedyJG.Currentconceptsin
thediagnosisandtreatmentofosteochondrallesionsofthe
ankle.AmJSportsMed.2010;38(2):392–404.
8.BerndtAL,HartyM.Transchondralfractures(osteochondritis
dissecans)ofthetalus.JBoneJointSurgAm.
1959;41-A:988–1020.
9.ScrantonPEJr,McDermottJE.TreatmentoftypeV
osteochondrallesionsofthetaluswithipsilateralknee
osteochondralautografts.FootAnkleInt.2001;22(5):380–4.
10.BaeS,LeeHK,LeeK,LimS,RimNJ,KimJS,etal.Comparison
ofarthroscopicandmagneticresonanceimagingfindingsin
osteochondrallesionsofthetalus.FootAnkleInt.
2012;33(12):1058–62.
11.GriffithJF,LauDT,YeungDK,WongMW.High-resolutionMR
imagingoftalarosteochondrallesionswithnew
classification.SkeletalRadiol.2012;41(4):387–99.
12.ChuckpaiwongB,BerksonEM,TheodoreGH.Microfracturefor
osteochondrallesionsoftheankle:outcomeanalysisand
outcomepredictorsof105cases.Arthroscopy.
2008;24(1):106–12.
13.ChoiWJ,ParkKK,KimBS,LeeJW.Osteochondrallesionofthe
talus:isthereacriticaldefectsizeforpooroutcome?AmJ
SportsMed.2009;37(10):1974–80.
14.ChristensenJC,DriscollHL,TencerAF,WilliamJ.StickelGold
Award.Contactcharacteristicsoftheanklejoint.Part2.The
effectsoftalardomecartilagedefects.JAmPediatrMed
Assoc.1994;84(11):537–47.
15.GianniniS,CeccarelliF,GirolamiM,CoppolaG,FerrariA.
Biologicalosteosynthesisinosteochondrallesionsofthe
rev bras ortop.2 0 1 6;51(5):489–500
499
16.FurukawaT,EyreDR,KoideS,GlimcherMJ.Biochemical
studiesonrepaircartilageresurfacingexperimentaldefects
intherabbitknee.JBoneJointSurgAm.1980;62(1):79–89.
17.ChoiWJ,ChoiGW,KimJS,LeeJW.Prognosticsignificanceof
thecontainmentandlocationofosteochondrallesionsofthe
talus:independentadverseoutcomesassociatedwith
uncontainedlesionsofthetalarshoulder.AmJSportsMed.
2013;41(1):126–33.
18.BecherC,ThermannH.Resultsofmicrofractureinthe
treatmentofarticularcartilagedefectsofthetalus.Foot
AnkleInt.2005;26(8):583–9.
19.ChoiWJ,KimBS,LeeJW.Osteochondrallesionofthetalus:
couldagebeanindicationforarthroscopictreatment?AmJ
SportsMed.2012;40(2):419–24.
20.FerkelRD,ZanottiRM,KomendaGA,SgaglioneNA,Cheng
MS,ApplegateGR,etal.Arthroscopictreatmentofchronic
osteochondrallesionsofthetalus:long-termresults.AmJ
SportsMed.2008;36(9):1750–62.
21.RobinsonDE,WinsonIG,HarriesWJ,KellyAJ.Arthroscopic
treatmentofosteochondrallesionsofthetalus.JBoneJoint
SurgBr.2003;85(7):989–93.
22.HanSH,LeeJW,LeeDY,KangES.Radiographicchangesand
clinicalresultsofosteochondraldefectsofthetaluswithand
withoutsubchondralcysts.FootAnkleInt.
2006;27(12):1109–14.
23.YoshimuraI,KanazawaK,TakeyamaA,AngthongC,IdaT,
HagioT,etal.Arthroscopicbonemarrowstimulation
techniquesforosteochondrallesionsofthetalus:prognostic
factorsforsmalllesions.AmJSportsMed.2013;41(3):528–34.
24.ChoiGW,ChoiWJ,YounHK,ParkYJ,LeeJW.Osteochondral
lesionsofthetalus:arethereanydifferencesbetween
osteochondralandchondraltypes?AmJSportsMed.
2013;41(3):504–10.
25.LeeDH,LeeKB,JungST,SeonJK,KimMS,SungIH.
Comparisonofearlyversusdelayedweightbearingoutcomes
aftermicrofractureforsmalltomidsizedosteochondral
lesionsofthetalus.AmJSportsMed.2012;40(9):2023–8.
26.GillTJ,McCullochPC,GlassonSS,BlanchetT,MorrisEA.
Chondraldefectrepairafterthemicrofractureprocedure:a
nonhumanprimatemodel.AmJSportsMed.2005;33(5):680–5.
27.CutticaDJ,ShockleyJA,HyerCF,BerletGC.CorrelationofMRI
edemaandclinicaloutcomesfollowingmicrofractureof
osteochondrallesionsofthetalus.FootAnkleSpec.
2011;4(5):274–9.
28.GoldstoneRA,PisaniAJ.Osteochondritisdissecansofthe
talus.NYStateJMed.1965;65(19):2487–94.
29.EasleyME,LattLD,SantangeloJR,Merian-GenastM,Nunley
JA2nd.Osteochondrallesionsofthetalus.JAmAcadOrthop
Surg.2010;18(10):616–30.
30.Mei-DanO,MaozG,SwartzonM,OnelE,KishB,NyskaM,
etal.Treatmentofosteochondritisdissecansoftheankle
withhyaluronicacidinjections:aprospectivestudy.Foot
AnkleInt.2008;29(12):1171–8.
31.SánchezM,AnituaE,AzofraJ,AguirreJJ,AndiaI.
Intra-articularinjectionofanautologouspreparationrichin
growthfactorsforthetreatmentofkneeOA:aretrospective
cohortstudy.ClinExpRheumatol.2008;26(5):910–3.
32.DeolPP,CutticaDJ,SmithWB,BerletGC.Osteochondral
lesionsofthetalus:size,age,andpredictorsofoutcomes.
FootAnkleClin.2013;18(1):13–34.
33.DavidTS,ShieldsCL.Radiofrequencyandarticularcartilage.
TechKneeSurg.2004;3(3):193–7.
34.VerhagenRA,StruijsPA,BossuytPM,vanDijkCN.Systematic
reviewoftreatmentstrategiesforosteochondraldefectsof
thetalardome.FootAnkleClin.2003;8(2):233–42.
35.ZengerinkM,StruijsPA,TolJL,vanDijkCN.Treatmentof
osteochondrallesionsofthetalus:asystematicreview.Knee
SurgSportsTraumatolArthrosc.2010;18(2):238–46.
36.SavvaN,JaburM,DaviesM,SaxbyT.Osteochondrallesionsof
thetalus:resultsofrepeatarthroscopicdebridement.Foot
AnkleInt.2007;28(6):669–73.
37.DoralMN,BilgeO,BatmazG,DonmezG,TurhanE,DemirelM,
etal.Treatmentofosteochondrallesionsofthetaluswith
microfracturetechniqueandpostoperativehyaluronan
injection.KneeSurgSportsTraumatolArthrosc.
2012;20(7):1398–403.
38.MilanoG,SannaPassinoE,DeriuL,CaredduG,ManuntaL,
ManuntaA,etal.Theeffectofplateletrichplasmacombined
withmicrofracturesonthetreatmentofchondraldefects:an
experimentalstudyinasheepmodel.Osteoarthritis
Cartilage.2010;18(7):971–80.
39.FortierLA,PotterHG,RickeyEJ,SchnabelLV,FooLF,ChongLR,
etal.Concentratedbonemarrowaspirateimproves
full-thicknesscartilagerepaircomparedwithmicrofracture
intheequinemodel.JBoneJointSurgAm.2010;92(10):
1927–37.
40.AndersS,LechlerP,RacklW,GrifkaJ,SchaumburgerJ.
Fluoroscopy-guidedretrogradecoredrillingandcancellous
bonegraftinginosteochondraldefectsofthetalus.Int
Orthop.2012;36(8):1635–40.
41.EmreTY,EgeT,CiftHT,Demircio ˘gluDT,SeyhanB,UzunM.
Openmosaicplastyinosteochondrallesionsofthetalus:a
prospectivestudy.JFootAnkleSurg.2012;51(5):556–60.
42.LattLD,GlissonRR,MontijoHE,UsuelliFG,EasleyME.Effect
ofgraftheightmismatchoncontactpressureswith
osteochondralgraftingofthetalus.AmJSportsMed.
2011;39(12):2662–9.
43.GobbiA,FranciscoRA,LubowitzJH,AllegraF,CanataG.
Osteochondrallesionsofthetalus:randomizedcontrolled
trialcomparingchondroplasty,microfracture,and
osteochondralautografttransplantation.Arthroscopy.
2006;22(10):1085–92.
44.WoelfleJV,ReichelH,NelitzM.Indicationsandlimitationsof
osteochondralautologoustransplantationinosteochondritis
dissecansofthetalus.KneeSurgSportsTraumatolArthrosc.
2013;21(8):1925–30.
45.FraserE,HarrisMC,PradpMP,KennedyJG.Autologous
osteochondraltransplantationforosteochondrallesionsof
thetalusinanathleticpopulation.KneeSurgSports
TraumatolArthrosc.2016;24(4):1272–9.
46.GianniniS,BudaR,GrigoloB,VanniniF,DeFranceschiL,
FacchiniA.Thedetachedosteochondralfragmentasasource
ofcellsforautologouschondrocyteimplantation(ACI)inthe
anklejoint.OsteoarthritisCartilage.2005;13(7):601–7.
47.WoelfleJV,ReichelH,Javaheripour-OttoK,NelitzM.Clinical
outcomeandmagneticresonanceimagingafter
osteochondralautologoustransplantationinosteochondritis
dissecansofthetalus.FootAnkleInt.2013;34(2):173–9.
48.PaulJ,SagstetterA,KrinerM,ImhoffAB,SpangJ,
HinterwimmerS.Donor-sitemorbidityafterosteochondral
autologoustransplantationforlesionsofthetalus.JBone
JointSurgAm.2009;91(7):1683–8.
49.HaeneR,QamiraniE,StoryRA,PinskerE,DanielsTR.
Intermediateoutcomesoffreshtalarosteochondralallografts
fortreatmentoflargeosteochondrallesionsofthetalus.J
BoneJointSurgAm.2012;94(12):1105–10.
50.BugbeeWD,KhannaG,CavalloM,McCauleyJC,GörtzS,Brage
ME.Bipolarfreshosteochondralallograftingofthetibiotalar
joint.JBoneJointSurgAm.2013;95(5):426–32.
51.JohnsonB,LeverC,RobertsS,RichardsonJ,McCarthyH,
HarrisonP,etal.Cellculturedchondrocyteimplantationand
scaffoldtechniquesforosteochondraltalarlesions.Foot
AnkleClin.2013;18(1):135–50.
52.NiemeyerP,SalzmannG,SchmalH,MayrH,SüdkampNP.
Autologouschondrocyteimplantationforthetreatmentof
meta-analysisofavailableevidence.KneeSurgSports
TraumatolArthrosc.2012;20(9):1696–703.
53.LeeKT,KimJS,YoungKW,LeeYK,ParkYU,KimYH,etal.
Theuseoffibrinmatrix-mixedgel-typeautologous
chondrocyteimplantationinthetreatmentforosteochondral
lesionsofthetalus.KneeSurgSportsTraumatolArthrosc.
2013;21(6):1251–60.
54.AndersS,GoetzJ,SchubertT,GrifkaJ,SchaumburgerJ.
Treatmentofdeeparticulartaluslesionsbymatrixassociated
autologouschondrocyteimplantation–resultsatfiveyears.
IntOrthop(SICOT).2012;36:2279–85.
55.AurichM,BediHS,SmithPJ,RolauffsB,MückleyT,ClaytonJ,
etal.Arthroscopictreatmentofosteochondrallesionsofthe
anklewithmatrix-associatedchondrocyteimplantation:
earlyclinicalandmagneticresonanceimagingresults.AmJ
SportsMed.2011;39(2):311–9.
56.GianniniS,BudaR,CavalloM,RuffilliA,CenacchiA,Cavallo
C,etal.Cartilagerepairevolutioninpost-traumatic
osteochondrallesionsofthetalus:fromopenfieldautologous
chondrocytetobone-marrow-derivedcellstransplantation.
Injury.2010;41(11):1196–203.
57.GianniniS,BudaR,BattagliaM,CavalloM,RuffilliA,Ramponi
L,etal.One-steprepairintalarosteochondrallesions:
4-yearclinicalresultsandt2-mappingcapabilityin
outcomeprediction.AmJSportsMed.2013;41(3):
511–8.
58.KimYS,ParkEH,KimYC,KohYG.Clinicaloutcomesof
mesenchymalstemcellinjectionwitharthroscopic
treatmentinolderpatientswithosteochondrallesionsofthe
talus.AmJSportsMed.2013;41(5):1090–9.
59.SakaguchiY,SekiyaI,YagishitaK,MunetaT.Comparisonof
humanstemcellsderivedfromvariousmesenchymal
tissues:superiorityofsynoviumasacellsource.Arthritis
Rheum.2005;52(8):2521–9.
60.ValderrabanoV,MiskaM,LeumannA,WiewiorskiM.
Reconstructionofosteochondrallesionsofthetaluswith
autologousspongiosagraftsandautologousmatrix-induced
chondrogenesis.AmJSportsMed.2013;41(3):519–27.
61.AdamsSB,YaoJQ,SchonLC.Particulatedjuvenilearticular
cartilageallografttransplantationforosteochondrallesions
ofthetalus.TechFootAnkleSurg.2011;10(2):92–8.
62.CoetzeeJC,GizaE,SchonLC,BerletGC,NeufeldS,StoneRM,
etal.Treatmentofosteochondrallesionsofthetaluswith
particulatedjuvenilecartilage.FootAnkleInt.
2013;34(9):1205–11.
63.vanBergenCJ,ReilinghML,vanDijkCN.Tertiary
osteochondraldefectofthetalustreatedbyanovel
contouredmetalimplant.KneeSurgSportsTraumatol
Arthrosc.2011;19(6):999–1003.
64.MologneTS,FerkelRD.Arthroscopictreatmentof
osteochondrallesionsofthedistaltibia.FootAnkleInt.
2007;28(8):865–72.
65.CutticaDJ,SmithWB,HyerCF,PhilbinTM,BerletGC.
Arthroscopictreatmentofosteochondrallesionsofthetibial
plafond.FootAnkleInt.2012;33(8):662–8.
66.BattagliaM,VanniniF,BudaR,CavalloM,RuffilliA,MontiC,
etal.Arthroscopicautologouschondrocyteimplantationin
osteochondrallesionsofthetalus:mid-termT2-mappingMRI
evaluation.KneeSurgSportsTraumatolArthrosc.
2011;19(8):1376–84.
67.ZwingmannJ,SüdkampNP,SchmalH,NiemeyerP.Surgical
treatmentofosteochondritisdissecansofthetalus:a
systematicreview.ArchOrthopTraumaSurg.