REVISTA
PAULISTA
DE
PEDIATRIA
www.rpped.com.br
ORIGINAL
ARTICLE
Duration
of
breastfeeding
in
preterm
infants
followed
at
a
secondary
referral
service
Brunnella
Alcantara
Chagas
de
Freitas
a,∗,
Luciana
Moreira
Lima
a,
Carla
Fernanda
Lisboa
Valente
Carlos
b,
Silvia
Eloiza
Priore
a,
Sylvia
do
Carmo
Castro
Franceschini
aaUniversidadeFederaldeVic¸osa(UFV),Vic¸osa,MG,Brazil
bCentroVivaVidadeReferênciaSecundáriaVic¸osaeRegiãodeSaúde,Vic¸osa,MG,Brazil
Received8June2015;accepted27August2015 Availableonline5March2016
KEYWORDS
Preterminfant; Breastfeeding; Verylowbirthweight newborn;
Extremelypreterm infants
Abstract
Objective: Identifyandanalyzevariablesassociatedwithshorterdurationofbreastfeedingin preterminfants.
Methods: Retrospectivecohortofprematureinfantsfollowedupatsecondaryreferralservice intheperiodof2010---2015.Inclusion:firstappointmentinthefirstmonthofcorrectedageand haveundergonethreeormoreconsultations.Exclusion:diseasesthatimpairedoralfeeding. Outcome:durationofbreastfeeding.Atotalof103preterminfantswereevaluated,accounting for28.8%ofthepreterminfantsborninthemunicipalityinthatperiod,withapowerofstudy of80%.Descriptiveanalysis,t-test, chi-squaretest,Kaplan---Meiercurves andCoxregression wereused.p-values<0.05wereconsideredsignificant.
Results: Themediandurationofbreastfeedingamong preterminfantswas 5.0months.The riskofbreastfeedingdiscontinuation amongpreterm infantswithgestationalage<32weeks was 2.6-foldhigher thanfor thosebornat32 weeksormore andthe riskofbreastfeeding interruptioninpreterminfantswhowerereceivingbreastfeedingsupplementationinthefirst outpatientvisitwas3-foldhigherwhencomparedtothosewhowereexclusivelybreastfedin thefirstconsultation.
Conclusions: Themediandurationofbreastfeedinginpreterminfantswasbelowthe recom-mendedoneanddiscontinuationwasassociatedwithgestational<32weeksandthefactthatthe infantwasnolongerreceivingexclusivebreastfeedinginthefirstoutpatientvisit.Whenthese twovariableswereassociated,theirnegativeeffectonthemediandurationofbreastfeeding waspotentiated.
©2015SociedadedePediatriadeSãoPaulo.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBYlicense(https://creativecommons.org/licenses/by/4.0/).
∗Correspondingauthor.
E-mail:brunnella.freitas@ufv.br(B.A.C.Freitas).
http://dx.doi.org/10.1016/j.rppede.2016.02.010
2359-3482/©2015SociedadedePediatriadeSãoPaulo.PublishedbyElsevierEditoraLtda.ThisisanopenaccessarticleundertheCCBY
PALAVRAS-CHAVE
Lactenteprematuro; Aleitamento
materno;
Recém-nascidode muitobaixopeso; Prematuroextremo
Durac¸ãodoaleitamentomaternoemprematurosacompanhadosemservic¸ode referênciasecundário
Resumo
Objetivo: Identificareanalisarasvariáveisassociadasàmenordurac¸ãodoaleitamentomaterno emprematuros.
Métodos: Coorte retrospectiva de prematuros acompanhados em centro de referência secundária,de2010a2015.Inclusão:primeiraconsultanoprimeiromêsdeidadecorrigidapara prematuridadeeterfeitotrêsoumaisconsultas. Exclusão:doenc¸asqueimpossibilitassema alimentac¸ãoviaoral.Desfecho:durac¸ãodoaleitamentomaterno.Avaliaram-se103prematuros, 28,8%dosprematurosdomunicípionoperíodo,compoderdoestudode80%.Usaram-seanálise descritiva, teste t,qui-quadrado de Pearson, curvas de Kaplan---Meier e regressão de Cox. Considerou-sesignificativoop-valor<0,05.
Resultados: A durac¸ão mediana do aleitamento materno entre os prematuros foi de cinco meses.Oriscodeinterrupc¸ãodoaleitamentomaternoentreprematurosdeidadegestacional inferiora32semanasfoi2,6vezesmaioremrelac¸ãoaosquenasceramcom32semanasoumais eoriscodeinterrupc¸ãodoaleitamentomaternoemprematurosqueestavamemaleitamento maternocomplementadonaprimeiraconsultaambulatorialfoitrêsvezesmaioremrelac¸ãoaos queestavamemaleitamentomaternoexclusivonaprimeiraconsulta.
Conclusões: Adurac¸ãomedianadoaleitamentomaternoemprematurosencontrou-seaquém dopreconizadoesuainterrupc¸ãoseassociouàidadegestacionalinferiora32semanaseao fato de não estarmais em aleitamento maternoexclusivo na primeira consulta ambulato-rial.Quandoessasduasvariáveis seassociaram,potencializou-se suainterferência negativa nadurac¸ãomedianadoaleitamentomaterno.
©2015SociedadedePediatriadeSãoPaulo.PublicadoporElsevierEditoraLtda.Esteéumartigo OpenAccesssobalicençaCCBY(https://creativecommons.org/licenses/by/4.0/deed.pt).
Introduction
The increase in preterm infants’ survival rate has been observed in developed and developing countries. How-ever,theseinfants arevulnerabletoconditionsleadingto increasedmorbidityand mortalityandrequirespecialized follow-up.1
Decreasedinfantmortalityandbetterneurodevelopment areprovenbenefitsassociatedwithbreastfeeding.2,3Breast milkisrecommendedasidealfor feedingpreterm infants andtheuse offormulaisonlyindicatedwhen breastfeed-ingisimpossible.1,4,5However,pretermmothershavelower success rates inbreastfeeding, which reinforcesthe need toadoptpracticesaimedtopromotebreastfeedingatthe different levels of health care.1,5---7 In this context, the workdevelopedatCentroIntegradoVivaVidadeReferência SecundáriaVic¸osa,establishedin2010inthestateofMinas Gerais,ishighlighted;theserviceconsistsofan interdisci-plinaryteamandhasbecomeareferenceforthehealthcare ofpreterminfantsinthecity.
Basedonthesepremises,thisstudyaimedtoidentifyand analyzevariablesassociatedwithshorterdurationof breast-feedinginpreterminfantsfollowedupinanewlyimplanted secondaryreferralserviceinthemunicipality.
Method
This is aretrospective cohort study of datafrom medical recordsofallpreterminfantsfollowedatCentroIntegrado
Viva Vida de Referência Secundária Vic¸osa (Centro Viva Vida), in Minas Gerais, enrolled from September 2010 to June2015.ThemedicalrecordsofCentroVivaVidaare semi-structured,afactthatallowed obtainingreliabledatafor thisstudy.
HospitalSãoSebastião,thehospitalwhereallbirthstake placeinthemunicipalityofVic¸osa,isareferencefor high-risk pregnancy andhas hada milk banksince2009 and a neonatalintensivecareunitsince2004.CentroVivaVidais dedicatedtomaternalandchildren’shealthandistheonly preterminfants’referralserviceinthemunicipality, estab-lishedinSeptember2010.Intheservice,wherethehealth care ofpreterminfantsis beingimplementedand intensi-fied, the care is performed by the interdisciplinary team --- consisting of professionalsfrom thepediatrics, nursing, nutrition,psychology,physiotherapyandsocialwork areas ---andislinkedwithUniversidadeFederaldeVic¸osa.Atthe timeofthedischarge fromtheHospital SãoSebastião,all preterminfantsaresenttoCentroVivaVidaforoutpatient follow-up.
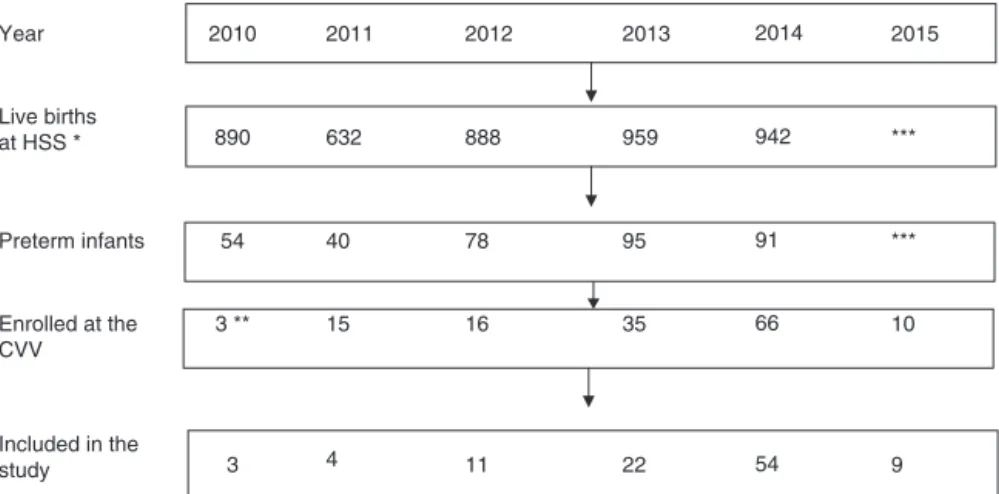
Duringthestudyperiod,theannualnumberoflivebirths in Hospital São Sebastião, municipality of Vic¸osa, ranged from632to959,withpretermbirthratesbetween6.1and 9.9%.Thedetailsofthenumberofbirthsandthetotal num-berwithlessthan37weekspereachyearofthestudyperiod areshowninFig.1.
Included in the
study 3 4 11 22 54 9
2015 2014
2013 2012
2011 2010
Year
Live births
at HSS * 890 632 888 959 942 ***
*** 91
95 78
40 54
Preterm infants
10 66
35 16
15 3 ** Enrolled at the
CVV
Figure1 Flowchartoftheofthestudypopulationselectionprocess.Vic¸osa-MG,2010---2015.
Note:theexclusion(differencebetweenpreterminfantsenrolledinCVVandincludedinthestudy)wasduetothefirstconsultation attheCVVoccurringafter44correctedweeksand/orhavinghadfewerthanthreeconsultations;nopretermhadanydiseasethat preventedoralfeeding.*AllbirthsinthemunicipalityoccurinHSS;**CVVwasestablishedinSeptember2010;***Dataarenotyet available(thestudywasextendedtoJuly2015).Sources:HospitalSãoSebastião(HSS)andCentroVivaVida(CVV).
follow-upperiod.Diseasesthatimpairedoralfeedingwere consideredexclusioncriteria.
The dependent variablefor the study wasduration of breastfeeding measured in months, according tothe cor-rectedage.8
Gestational age was defined as the best estimate obtained from early pregnancy ultrasound, date of last menstrual period,obstetric data andclinical examination according to the NewBallard score.9,10 Chronologicalage wasdefinedaspostnatalageandthecorrectedageasthe gestationalageatbirthplusthepostnatalage.11
Theassessedsociodemographicvariableswere:maternal andpaternal age,maternal andpaternalschooling (upto elementaryschoolandfurther),maternaloccupation(work outside or not), maternal maritalstatus (single/divorced, common-lawmarriage/married)andfamilyincomein mini-mumwages(MW;<2MWandMW≥2).12
The variables assessed in the prenatal and perinatal period were: type of delivery, gender, gestational age (weeks),birthweight(grams),stratificationbybirthweight andgestationalage,adequacyofbirthweightforgestational age,admissiontothe neonatalintensive care unitandits duration.Thebirthweightwascategorizedas<1.500gand
≥1.500g,andgestationalageas<32weeksand≥32weeks.13 ThesmallforgestationalagecriterionwasbasedonFenton andKim14curvesandwascharacterizedasvaluesbelowthe 10thpercentileofweightforgestationalage.
Thefirstconsultationwasdefinedasthefirstrecordinthe outpatientmedicalfileandthelastconsultationasthelast datarecordedinthemedicalfile,ofwhichlimitwastheend ofthestudyperiod.Theoccurrenceofhospitalizationand thetypeoffeedingweredocumentedatthefirst consulta-tion---categorizedasexclusivebreastfeeding,supplemented breastfeedingandartificialfeeding8---butforthebivariate andmultivariateanalysis,onlythetypeofbreastfeedingin thefirstconsultationwasconsidered (exclusiveor supple-mented).Anthropometricmeasurementsinthefirstandlast consultationswerealsorecordedandthecorrectedagewas alsoconsidered: weight,stature(length/height)and body
massindexforage.Theanthropometricmeasurementswere collectedbypediatricians ornutritionists during consulta-tionsusingdigitalscalesandanthropometer,andrecorded inthemedicalrecords.
The minimum sample size was definedusing the coef-ficient of variation obtained in the present study for the variabledurationofbreastfeeding(70%);considering20%of variationaroundthemean,weobtainedaminimumsample sizeof50individualssothatsignificantdifferencescouldbe observedwithasignificancelevelof5%andapowerofstudy of80%.15
For the descriptive analysis, means, standard devi-ations, medians, minimum and maximum values, fre-quencies and absolute numbers were determined. The Kolmogorov---Smirnov test was used for the continuous variables and the ones with parametric distribution were expressedasmeanandstandarddeviation,whilethosewith non-parametricdistributionwereexpressedasmediansand minimumandmaximumvalues.Thefrequenciesreferredto thetotal number of validresponses and the missingdata werenotconsidered.Acomparativeanalysisofthepreterm infants included and those not included in the study was performedbyttestandPearson’schi-squaretest.
duration.Thebivariateanalysiswasusedinthefirststage, whereweinvestigatedtheassociationbetweenindependent variablesandthedurationofbreastfeeding usingLogRank andBreslowtests,whichcomparethesurvivalcurvesineach categoryofthe independentvariable.The nullhypothesis inbothtestsistheequalityofsurvivalfunctions. TheCox regressionmodelwasusedtoanalyzebreastfeeding dura-tion,adjustedforcovariates.Allvariablesthathadap-value <0.20 in either of the two tests of the bivariateanalysis wereincludedinthemultivariateanalysis.Thefinalmodel includedsignificantvariablesatthe0.05level.The Statisti-calPackagefortheSocialSciences(SPSS)version20.0was usedforthestatisticalanalysis.
The study was approved by the Institutional Review Board of Universidade Federal de Vic¸osa (CAAE 19676613.5.0000.5153), as part of the project ‘‘Growth, development and morbidities of preterm or low-birth weightinfantsandpreschoolchildren’’,whichcomprisesa doctoralthesis developed at the Postgraduate Programin ScienceofNutrition,DepartmentofNutritionandHealthof UFV.
Results
Themedicalrecordsof145preterminfantswereassessed and,afterapplyingtheinclusionandexclusioncriteria,the studypopulationincluded103subjects(Fig.1),28.8%ofthe preterminfantsofthe municipalityinthe period.As Cen-troVivaVida(CVV)wasestablishedinSeptember2010,one observesatendencytoanincreaseinthenumberofpreterm infants referred for outpatient follow-up after 2013. The exclusion of preterm infants was due to the first consul-tationatCVVafter44correctedweeksand/orhavinghad fewerthan threeconsultations, as nopreterm infanthad anydiseasethatpreventedoralfeeding.
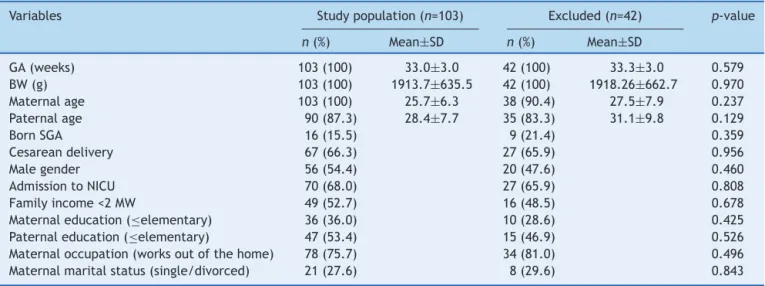
Sociodemographic and perinatal characteristics of the preterm infants are described in Table 1, as well as the
comparativeanalysisofthoseincludedandnotincludedin thestudy.Therewerenosignificantdifferencesbetweenthe characteristicsofthestudiedpopulationandtheexcluded preterminfants.
The population of preterm infants was distributed as follows: 31.1% had birthweight <1.500g (n=32) and 68.9%
≥1.500g(n=71);31.1%werebornwithgestationalage<32 weeks(n=32)and68.9%≥32weeks(n=71).Ofthe70preterm infants thatwereadmittedtotheneonatalintensive care unitintheneonatalperiod,themedianhospitalizationtime was26.8days(1---135days).
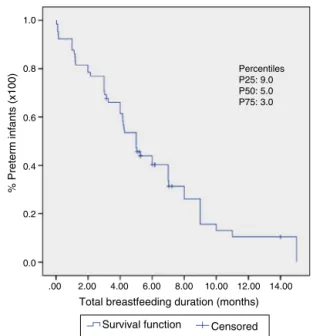
It wasobserved that 50% of the preterm infants were followeduntil11 monthsofcorrectedage (Fig.2).At the time of first consultation, 35.9% of the preterm infants were exclusively breastfed,39.8% received supplemented breastfeeding and 24.3% artificial feeding (Table 2), with median breastfeeding duration of five months (Fig. 3). Among preterm infants with less than 32 weeks, 10.8% receivedexclusivebreastfeeding(n=4),26.8%supplemented breastfeeding(n=11)and68%artificialfeeding(n=17).
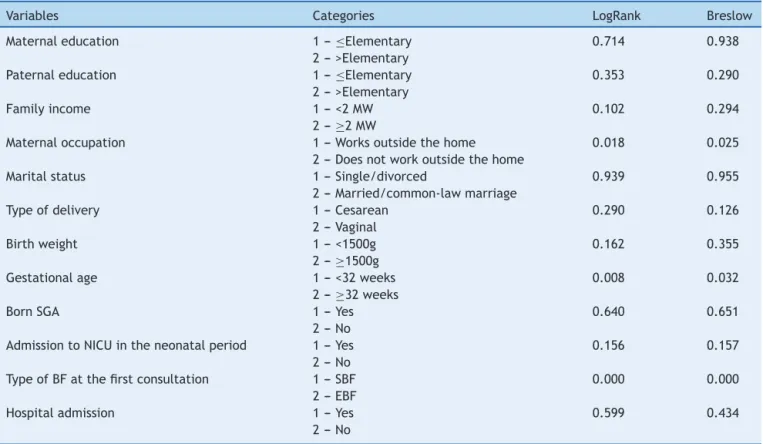
Atthebivariateanalysisfor thebreastfeedingduration outcome, throughtheresults of theLogRank andBreslow tests, the variables family income, maternal occupation, type of delivery, birth weight,gestational age, admission attheneonatalintensivecareunitandtypeof breastfeed-ingatthefirstconsultationhadap<0.20andwereincluded foranalysisintheCoxregressionmodel(Table3).
Thefinalmodelforthebreastfeedingdurationoutcome had two explanatory variables, gestational age and type of breastfeeding in the first consultation (Table 4). The adequacy of the model was verified by the development of charts involving thelogarithm of therisk function ver-sus time,andtheassumptionof proportionalhazardswas proven.
AccordingtotheLogRankandBreslowtests,themedian breastfeedingdurationaccordingtothetypeof breastfeed-inginthefirstconsultation(exclusiveorsupplemented)and adjustedforgestationalage(<32weeksor≥32weeks)was
Table1 Comparativeanalysisofsociodemographicandperinatalcharacteristicsofpreterminfantsincludedandnotincluded inthestudy.Vic¸osa-MG,2010---2015.
Variables Studypopulation(n=103) Excluded(n=42) p-value
n(%) Mean±SD n(%) Mean±SD
GA(weeks) 103(100) 33.0±3.0 42(100) 33.3±3.0 0.579
BW(g) 103(100) 1913.7±635.5 42(100) 1918.26±662.7 0.970
Maternalage 103(100) 25.7±6.3 38(90.4) 27.5±7.9 0.237
Paternalage 90(87.3) 28.4±7.7 35(83.3) 31.1±9.8 0.129
BornSGA 16(15.5) 9(21.4) 0.359
Cesareandelivery 67(66.3) 27(65.9) 0.956
Malegender 56(54.4) 20(47.6) 0.460
AdmissiontoNICU 70(68.0) 27(65.9) 0.808
Familyincome<2MW 49(52.7) 16(48.5) 0.678
Maternaleducation(≤elementary) 36(36.0) 10(28.6) 0.425
Paternaleducation(≤elementary) 47(53.4) 15(46.9) 0.526
Maternaloccupation(worksoutofthehome) 78(75.7) 34(81.0) 0.496
Maternalmaritalstatus(single/divorced) 21(27.6) 8(29.6) 0.843
1.0
0.8
0.6
0.4
0.2
0.0
.00
% Preterm infants (x100)
10.00 20.00
Outpatient follow-up duration (months)
30.00 40.00 50.00 Percentiles P25: 17.0 P50: 11.0 P75: 5.27
Figure2 Kaplan---Meiercurvewiththeestimateofthetotal timeofoutpatientfollow-upofpreterminfants(n=103).Vic ¸osa-MG,2010---2015.Itcanbeobservedthat50%ofpreterminfants werefolloweduntil11monthsofcorrectedage.The25thand 75thpercentilesarealsodemonstrated.
asfollows:exclusivebreastfeedinginthefirstconsultation andgestationalage<32weeks,4.2months;supplemented breastfeedingin thefirstconsultationand gestationalage <32 weeks, 1.2 months; exclusive breastfeeding in the firstconsultationandgestationalage≥32weeks,9months; supplemented breastfeeding in the first consultation and gestational age≥32 weeks, 4 months. The respective p-valueswerep<0.001andp=0.001.
According to the Cox regression model, the follow-ing associations were found: the risk of interruption of
1.0
0.8
0.6
0.4
0.2
0.0
.00 2.00 4.00
Total breastfeeding duration (months) 6.00 8.00 10.00 12.00 14.00
Survival function
% Preterm infants (x100)
Censored Percentiles P25: 9.0 P50: 5.0 P75: 3.0
Figure3 Kaplan---Meiercurvewithestimatesof breastfeed-ingdurationinpreterminfants(n=71).Vic¸osa-MG,2010---2015. Amedianoffivemonths canbeobserved.The25thand75th percentilesarealsodemonstrated.
breastfeeding among preterm gestational age <32 weeks was 2.6-fold higher when compared to those born at 32 weeksor moreand the risk of breastfeeding interruption amongpreterm infants that were receiving breastfeeding supplementationinthefirstoutpatientconsultationwas 3-foldhigherwhencomparedtothosewhowereexclusively breastfedinthefirstconsultation.
Table2 Characteristicsofpreterminfantsattheoutpatientfollow-up(n=103).Vic¸osa-MG,2010---2015.
Variables n(%) Mean(±SD) Median(min---max)
Firstconsultation 103(100)
CAP(weeks,days) 40.0(2.2)
---Weight(g) 3124.8(764.5)
---Length(cm) 49.1(3.0)
---Lastconsultation 103(100)
CA(months,days) 12.1(8.8)
---Weight(g) 8903.0(2411.0)
---Height(cm) 73.6(9.9)
---BMI 16.2(1.6)
---Numberofconsultations 103(100) --- 6.0(3.0---16.0)
Feedingatthefirstconsultation
EBF 37(35.9)
---SBF 41(39.8)
AF 25(24.3)
Hospitaladmission ---
---Yes 12(12.0)
No 88(88.0)
Table3 Associationbetweenindependentvariablesandbreastfeedingduration,accordingtothep-valuefoundinthebivariate analysisbyLogRankandBreslowtests.Preterminfants,Vic¸osa-MG,2010---2015.
Variables Categories LogRank Breslow
Maternaleducation 1---≤Elementary
2--->Elementary
0.714 0.938
Paternaleducation 1---≤Elementary
2--->Elementary
0.353 0.290
Familyincome 1---<2MW
2---≥2MW
0.102 0.294
Maternaloccupation 1---Worksoutsidethehome
2--- Doesnotworkoutsidethehome
0.018 0.025
Maritalstatus 1--- Single/divorced
2--- Married/common-lawmarriage
0.939 0.955
Typeofdelivery 1---Cesarean
2---Vaginal
0.290 0.126
Birthweight 1---<1500g
2---≥1500g
0.162 0.355
Gestationalage 1---<32weeks
2---≥32weeks
0.008 0.032
BornSGA 1---Yes
2---No
0.640 0.651
AdmissiontoNICUintheneonatalperiod 1---Yes 2---No
0.156 0.157
TypeofBFatthefirstconsultation 1---SBF 2---EBF
0.000 0.000
Hospitaladmission 1--- Yes
2---No
0.599 0.434
MW,minimumwage;BF,breastfeeding;SBF,supplementedbreastfeeding;EBF,exclusivebreastfeeding;SGA,smallforgestationalage; NICU,neonatalintensivecareunit.
Table4 Variablesassociatedwithbreastfeedingduration,accordingtotheresultsobtainedinthemultivariateanalysisbyCox regressionmodel.Preterminfants,Vic¸osa-MG2010---2015.
Covariate Coefficient Standarderror p-value Hazardratios(95%CI)
GA 0.948 0.369 0.010 2.581(1.253---5.317)
TypeofBFatthefirstconsultation 1.100 0.331 0.001 3.005(1.571---5.749)
GA,gestationalage;BF,breastfeeding;CI,confidenceinterval.
Discussion
Inthisstudy,themedian durationof breastfeedingamong theassessedpreterminfantswasfivemonths,whichisbelow the recommended duration.5 Factors related to shorter breastfeeding duration were gestational age <32 weeks and supplemented breastfeeding at the first outpatient consultation. When these two variables were associated, their negative effect on the median breastfeeding dura-tionwaspotentiated,whichwasonly1.2months,compared withtheassociationofexclusivebreastfeedingat thefirst consultation and gestational age≥32 weeks, leading to a medianofbreastfeedingduration ofninemonths. Corrob-oratingthisassociation,thehazardratiosforbreastfeeding interruptionwere2.6-foldhigherfor preterminfants with gestationalage<32weeksand3-foldhigherforthose receiv-ing supplemented breastfeeding at the first consultation. Moreover,asnegativeaspects,itshouldbehighlightedthat 39.8%ofpreterminfantsinthefirstoutpatientconsultation werereceivingbreastfeedingsupplementationand24.3%no
longerreceivedbreastmilk.Thestudyresultsindicatethe needtoadoptstrategiestoestablishandincreaseexclusive breastfeedingduration,especiallyof preterminfantswith <32weeksofgestationalage.
The useof formula is onlyindicated when feeding the infant breast milk is impossible1,4 and, for a successful breastfeeding after discharge, it is important that the preterminfantreceiveexclusivebreastfeedingatthetime ofdischarge.16 Thereisevidencethatmothersof preterm infantshavelowersuccessratesinbreastfeeding,andthus the adoptionof practicesthat aimtoestablish and main-tain the supply of breast milk as first choice for feeding preterminfants,consideredavulnerablepopulation,must becontinuallysupportedandreviewed.1,5---7,17
34 weeks)and preparationof the preterminfant and the family to hospital discharge. These practices are recom-mended in literature.1,16,18 Nevertheless, lower rates of exclusive breastfeedingwereobserved amongthestudied preterm infants in the start of the outpatient follow up, whencomparedwithsupplementedbreastfeedingand arti-ficial feeding rates. There is an association between the preterm receiving supplemented breastfeeding from the firstweekoflifeandashorterdurationofbreastfeeding.19
All preterm infants born with <32 weeks of gesta-tional age were admitted to the neonatal intensive care unit. It is known that the health status of the preterm infant duringthe perinatalperiod is adetermining factor of breastfeeding duration,20 but there are other factors involved,suchastheinsufficientstimulationofthebreast andtheunderlying causesofpreterm birth(hypertension, diabetes and maternal obesity), all of them negatively influencing breast milk production.21 On the other hand, studies show that maternal motivation and the support receivedtobreastfeed areabletoincrease breastfeeding duration.3,22
The presence of human milk banks in hospitals where preterminfants areadmitted isan important toolto pro-motebreastfeeding.23 Aseffective strategiesinpromoting breastfeedingonecanmention:providinginformationtothe family;helping themother to establish and maintain the milksupply;ensuringpropertechniquesforhandlingbreast milk (storage and handling); development of procedures andapproaches tofeedpreterm infants withbreastmilk; promoting skin-to-skin contact and nonnutritive sucking opportunitiesat thebreast;managementof thetransition tobreastfeeding;preparationofthepreterminfantandthe family to hospital discharge and appropriate follow-up.18 However,theestablishment of theidealtimetostart the transitiontobreastfeedinginpreterminfantsisstilla chal-lengeforhealthprofessionals.Frequently,unjustifieddelays andsuctionrestrictionsmayoccurduetoopinionsnotbased onevidence.24
AstudybyWilsonetal.21showsthatmostofthemother’s breastmilksupplyinthefirstweekoflifeofpreterminfants <32weeksisassociatedwitha55%rateofexclusive breast-feeding ratesat 36 corrected weeksfor prematurity. This confirmsthatitispossibletoachievehighratesofexclusive breastfeedinginpreterminfants<32weeks.
Althoughthisstudyshowednoassociationbetween hospi-talreadmissionandbreastfeedingduration,preterminfants aremoresusceptibletoreadmissionsandtheirhealthstatus affectsbreastfeedingduration.20,25
Decreased infant morbidity, mortality and better neurodevelopment are proven benefits associated with breastfeeding.2,3,26Thus,offeringfollow-upandsupportto preterminfantsandtheirfamilies,especiallythosebornat lessthan32weeks,focusingonthepromotion,protection and supportof breastfeeding, in order toincrease exclu-sivebreastfeedingrates,areanimportantissueandshould be carried out in all health care levels, beginning during the hospitalization period and extending throughout the outpatientfollow-upperiod.20,27---30 Asstudylimitation,we mentiontheretrospectivecohortdesign, subjectto infor-mation biases (a fact minimized by the semi-structured modeloftheservicemedicalrecords,whichalloweda bet-terqualityof information)andchangesinthesample size
over time (minimized by the appropriate methodological design).
Itcanbeconcludedthat,inthestudy,themedian breast-feeding duration among preterm infants was below the recommendedperiodanditsdiscontinuationwasassociated withlessthan32weeksofgestationalageandwiththefact thatthepretermwasnolongerreceivingexclusive breast-feeding at the first outpatient consultation. When these two variables were associated, their negative effect on themedianbreastfeedingdurationwaspotentiated.These resultsemphasizetheneedofadoptingstrategiesto estab-lishandincrease the durationof exclusive breastfeeding, especiallyamongpreterminfantslessthan32weeksof ges-tationalage.
Funding
Thisstudydidnotreceivefunding.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Brasil---MinistériodaSaúde.SecretariadeAtenc¸ãoàSaúde ---DepartamentodeAc¸õesProgramáticaseEstratégicas.Atenc¸ão àsaúdedorecém-nascido:guiaparaosprofissionaisdesaúde. Brasília:MinistériodaSaúde;2011.
2.SchanlerRJ.Outcomesofhumanmilk-fedprematureinfants. SeminPerinatol.2011;35:29---33.
3.Forcada-GuexM,Pierrehumbert B, BorghiniA,Moessinger A, Muller-NixC.Earlydyadicpatternsofmother---infant interac-tionsand outcomesofprematurity at18months.Pediatrics. 2006;118:e107---14.
4.Aggett PJ, Agostoni C, Axelsson I, De Curtis M, Goulet O, et al. ESPGHAN Committee on Nutrition. Feeding preterm infants after hospital discharge: a commentary by the ESPGHANCommitteeonNutrition.JPediatrGastroenterolNutr. 2006;42:596---603.
5.SociedadeBrasileiradePediatria.DepartamentoCientíficode Neonatologia,editor. SeguimentoAmbulatorial doPrematuro deRisco.1ed.RiodeJaneiro:SBP;2012.
6.UnderwoodMA.Humanmilkfortheprematureinfant.Pediatr ClinNorthAm.2013;60:189---207.
7.Tudehope DI.Human milk. Thenutritional needsofpreterm infants.JPediatr.2013;162:S17---25.
8.WorldHealthOrganization.Indicatorsforassessinginfantand youngchildfeedingpractices:conclusionsofaconsensus meet-ingheld6---8November2007inWashingtonD.C.,USA;2008.
9.TheAmericanCongressofObstetriciansandGynecologists[page ontheInternet].CommitteeonObstetricPractice;American InstituteofUltrasoundinMedicine;SocietyforMaternal-Fetal Medicine. Method for Estimating Due Date. Available from:
http://www.acog.org/Resources-And-Publications/Committee- Opinions/Committee-on-Obstetric-Practice/Method-for-Estimating-Due-Date[accessed04.06.15].
10.RegoMA,FrancaEB,TravassosAP,BarrosFC.Assessmentofthe profileofbirthsanddeathsinareferralhospital.JPediatr(Rio J).2010;86:295---302.
12.InstitutoBrasileirodeGeografiaeEstatística(IBGE)[pageonthe
Internet]. Available from: http://www.ibge.gov.br [accessed
18.10.14].
13.IOM.Pretermbirth:causes,consequences,andprevention
insti-tuteofmedicine.NationalAcademyofSciences;2007.Available
from:http://www.nap.edu/catalog/11622.html
14.FentonTR,KimJH.Asystematicreviewandmeta-analysisto revisetheFentongrowthchartforpreterminfants.BMCPediatr. 2013;13:59.
15.Hulley SB,Cummings SR. Estimating samplesize and power. In: Designing clinical research. Baltimore, MD: Williams and Wilkins;1988.p.148.Appendix13A,215.
16.SantoroJúniorW, Martinez FE.Effectofinterventiononthe rates ofbreastfeedingof verylowbirth weight newborns. J Pediatr(RioJ).2007;83:541---6.
17.Nazareth R, Goncalves-Pereira J, Tavares A, Miragaia M, de Lencastre H, Silvestre J, et al. Community-associated methicillin-resistantStaphylococcusaureusinfectionin Portu-gal.RevPortPneumol.2012;18:34---8.
18.Spatz DL. Ten steps for promoting and protecting breast-feeding for vulnerable infants. J Perinat Neonatal Nurs. 2004;18:385---96.
19.HolmesAV,AuingerP,HowardCR.Combinationfeedingofbreast milkandformula:evidenceforshorterbreast-feedingduration fromtheNationalHealthandNutritionExaminationSurvey.J Pediatr.2011;159:186---91.
20.Espy KA, Senn TE. Incidence and correlates of breast milk feeding in hospitalized preterm infants. Soc Sci Med. 2003;57:1421---8.
21.Wilson E, Christensson K, Brandt L, Altman M, Bonamy AK. Earlyprovisionofmother’sownmilkand otherpredictorsof
successful breast milk feeding after very preterm birth: a regionalobservationalstudy.JHumLact.2015.
22.Buarque V, Lima M de C, Scott RP, Vasconcelos MG. The influence of support groups on the family of risk newborns and on neonatal unit workers. J Pediatr (Rio J). 2006;82: 295---301.
23.EdwardsTM,SpatzDL.Makingthecaseforusingdonorhuman milkinvulnerableinfants.AdvNeonatalCare.2012;12:273---8, quiz9---80.
24.DavanzoR,StrajnT,KennedyJ,CrocettaA,DeCuntoA.From tubetobreast:thebridgingroleofsemi-demandbreastfeeding. JHumLact.2014;30:405---9.
25.Underwood MA, Danielsen B, Gilbert WM. Cost,causes, and rates of rehospitalization of preterm infants. J Perinatol. 2007;27:614---9.
26.Tarrant M, Kwok MK, Lam TH, Leung GM, Schooling CM. Breast-feeding and childhood hospitalizations for infections. Epidemiology.2010;21:847---54.
27.HallowellSG,SpatzDL.Therelationshipofbraindevelopment andbreastfeedinginthelate-preterminfant.JPediatrNurs. 2012;27:154---62.
28.GeddesD,HartmannP,JonesE.Pretermbirth:strategiesfor
establishingadequatemilkproductionandsuccessfullactation.
SeminFetalNeonatalMed[epub25.04.13].
29.WhyteRK. Neonatalmanagement and safedischargeof late and moderate preterm infants. Semin Fetal Neonatal Med. 2012;17:153---8.