RevBrasAnestesiol.2018;68(1):87---90
REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
CLINICAL
INFORMATION
Difficult
fiberoptic
tracheal
intubation
in
1
month-old
infant
with
Treacher
Collins
Syndrome
Ricardo
Fuentes,
Juan
Carlos
De
la
Cuadra,
Hector
Lacassie,
Alejandro
González
∗PontificiaUniversidadCatólicadeChile,FacultaddeMedicina,DivisióndeAnestesiología,Santiago,Chile
Received12January2015;accepted11February2015 Availableonline1October2015
KEYWORDS
TreacherCollins Syndrome; Difficultairway; Fiberoptic bronchoscope; Laryngealmask airway; Infants
Abstract Neonatesandsmallinfantswithcraniofacialmalformationmaybeverydifficultor impossibletomaskventilateorintubate.Wewouldliketoreportthefiberopticintubationof asmallinfantwithTreacherCollinsSyndromeusingthetechniquedescribedbyEllisetal.
Casereport: An one month-old infant with Treacher Collins Syndrome was scheduled for mandibularsurgeryundergeneralendotrachealanesthesia.Directlaryngoscopyfororal intu-bationfailedtorevealtheglottis.Fiberopticintubationusingnasalapproach andusingoral approachthrougha1.5sizelaryngealmaskairwaywereperformed;however,bothapproach failedbecausethefiberscopeloadedwithaone3.5mmIDuncuffedtubewasstuckinsidethe nasalcavityorinsidethelaryngealmaskairwayrespectively. Therefore,thelaryngeal mask airwaywaskeepinplaceandthefiberopticintubationtechniquedescribedbyEllisetal.was planned:thetrachealtubewiththe15mmadapterremovedwasloadedproximallyoverthe fiberscope;thefiberscopewasadvancedundervideo-screenvisualizationintothetrachea;the laryngeal maskairwaywas removed,leaving thefiberscopeinplace; thetrachealtubewas passedcompletelythroughthelaryngealmaskairwayandadvanceddownoverthefiberscope intothetrachea;thefiberscopewasremovedandthe15mmadapterwasreattachedtothe trachealtube.
Conclusion: Thefiberopticintubationmethodthroughalaryngealmaskairwaydescribedby Ellisetal.canbesuccessfullyusedinsmallinfantswithTreacherCollinsSyndrome.
©2015SociedadeBrasileiradeAnestesiologia.Publishedby ElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
PALAVRAS-CHAVE
SíndromedeTreacher Collins;
Viaaéreadifícil; Broncoscópiodefibra óptica;
Intubac¸ãotraquealdifícilcomfibraópticaembebêdeummêsdeidade comsíndromedeTreacherCollins
Resumo Osrecém-nascidos ecrianc¸as pequenascommalformac¸ãocraniofacialpodem ser muitodifíceisouimpossíveisdeventilarpormáscaraoudeintubar.Gostaríamosderelatara intubac¸ão comfibra ópticadeum bebêcomsíndromedeTreacherCollinsusandoatécnica descritaporEllisetal.
∗Correspondingauthor.
E-mail:gonzalea@med.puc.cl(A.González).
https://doi.org/10.1016/j.bjane.2015.02.004
88 R.Fuentesetal.
Máscaralaríngea; Bebês
Relatodecaso:Umacrianc¸adeummêsdeidadecomsíndromedeTreacherCollinsfoi progra-madaparacirurgiamandibularsobanestesiageralendotraqueal.Alaringoscopiadiretapara intubac¸ãooralnãorevelouaglote.Aintubac¸ãocomfibraópticausandoasabordagensnasal eoralpormeiodemáscaralaríngeadetamanho1,5foitentada,masambas asabordagens falharamporqueofibroscópioportandoumtubosembalonetede3,5mmficoupresono inte-riordacavidadenasaloudentrodamáscaralaríngea,respectivamente.Portanto,amáscara laríngeafoimantidanolugareatécnicadeintubac¸ãocomfibraópticadescritoporEllisetal. foiplanejada: otubotraquealcomo adaptadorde15mmremovidofoi colocado proximal-mentesobreofibroscópio;ofibroscópiofoiavanc¸adonatraquéiasobvisualizac¸ãoemtelade vídeo;amáscaralaríngeafoiremovida,deixando ofibroscópionolugar;otubotraquealfoi passadocompletamenteatravésdamáscaralaríngeaeavanc¸adoparabaixosobreofibroscópio natraquéia;ofibroscópiofoiremovidoeoadaptadorde15mmfoirecolocadonotubotraqueal.
Conclusão:Ométododeintubac¸ãocomfibraópticaatravésdeumamáscaralaríngeadescrito porEllisetal.podeserusadocomsucessoembebêscomsíndromedeTreacherCollins. ©2015SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigoOpen Accesssobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
TreacherCollinsSyndromeisacongenitalcraniofacial mal-formation mainly characterized by bilateral hypoplasiaof facialbones(mandible,maxillaandzygoma),cleftpalate, ears and eyes deformities and temporomandibular joint abnormalities.Patientswiththissyndromemaybevery dif-ficultorimpossibletomaskventilateorintubate.1,2
Several techniques and deviceshave been successfully
used to intubate pediatric patients with Treacher Collins
Syndrome.1---10 InnewbornsandsmallinfantswithTreacher
Collins Syndrome only the use of laryngeal mask airway
(LMA),fiberopticbronchoscope(FB)and,morerecently,two
differentopticaldeviceshavebeendescribedtohandlethe
airway.11---15 We would like to report the tracheal
intuba-tionof1-month-oldinfantwithTreacherCollinsSyndrome,
undergoingmandibularsurgery,usingthefiberoptic
intuba-tionmethoddescribedbyEllisetal.16
Case
report
Consent for publication was obtained from the patient’s
father.A1monthold,5kgboy,withupperairway
obstruc-tionsecondarytoTreacherCollinsSyndromewasscheduled
formandibulardistractionosteogenesisundergeneral
endo-tracheal anesthesia. He had a significant micrognathia;
therefore difficult tracheal intubation wasanticipated. A
nasal intubation was planned using conventional direct
laryngoscopy or, in case of failure, using a pediatric FB
withnoworkingchannel(Fujinon120P,2.8mmOD;Fujinon
Corporation, Saitama, Japan). Fiberoptic oral intubation
throughaLMAwouldbethenextstepifpreviousapproaches
wereunsuccessful.Twoseniorpediatricanesthesiologists,a
senioranesthesiaregistrar andtwoseniorplasticsurgeons
werepresentintheoperatingroom,andwewereprepared
foratracheostomyifmentionedmethods were
unsuccess-ful.
Intheoperatingroom,beforetheanesthesiainduction,
the airway devices were checked and that the pediatric
FBwouldfit easily througha 3.5mm IDuncuffed tracheal
tube(RuschUruguayLtda.,Montevideo,Uruguay).Standard
monitoringwereappliedwhiletheinfantreceived100%O2
via facial mask. Atropine 0.01mg.kg−1 was administered
througha24gaugeintravenouscannulapreviouslyinserted.
In order to maintain spontaneous ventilation,
inhala-tion induction was performed with increasing doses of
sevoflurane in an air/O2 mixture to obtain 4% end tidal
concentration.Lungventilationwaseasilyassistedwithbag
andfacialmask.DirectlaryngoscopywithaMiller0blade
failedtorevealthevocalcords.Then,wemovedto
fiberop-tic nasal intubation. Maintaining an adequate anesthesia
depth and spontaneousventilation, a 3.5mm IDuncuffed
trachealtubewascarefullyinsertedthroughonenarisinto
thenasopharynxtoverifythatpassedeasilyacrossthenasal
cavityandtofacilitatethefiberopticintubation.However,
theFBwasstuckinsidethelumenofnasaltubeandcould
notmove further.Therefore,we wenttothenextstepto
securetheairway.
WeverifiedthataFBloadedwitha3.5mmIDuncuffed
trachealtube couldpass both togetherthroughasize 1.5
LMA (Unique, LMA NorthAmerica, San Diego, USA) lumen
that hadits grillbars previouslycut. The LMA wasgently
insertedanditscorrectpositionwasconfirmedbyendtidal
CO2 andtheabilitytoprovideassistedventilation.TheFB
wasthreadedthroughthetrachealtubeandbothtogether
were introducedand advanced intotheLMA lumen under
video-screenvisualization.However,thetrachealtubewith
the FBinitsinterior wasstuckinside the LMAlumen and
anyonecouldnotadvancefurther,andbothwereremoved
keepingtheLMAinplace.Atthattime,wedecidedtotry
thefiberopticintubatingmethodthroughLMAdescribedby
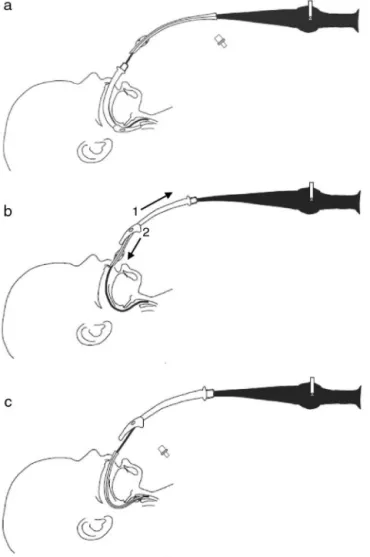
Ellisetal.16(Fig.1).
Anew3.5mmIDuncuffedtrachealtubewiththe15mm
adapterremovedwasloadedproximally overthe
broncho-scope. The FB wasintroduced easily throughthe size 1.5
LMAandadvancedundervideo-screenvisualizationintothe
trachea until the carina was visualized (Fig. 1A). Then,
theLMA wasdeflatedandremoved fromthe mouth,
Difficultintubationin1month-oldinfant 89
Figure1 Fiberopticintubationmethod throughalaryngeal maskairway(LMA)describedbyEllisetal.16(A)Thefiberoptic
brochoscope(FB)loadedproximallywithatracehaltube with-out15mmadapterisintroducedandadvancedthroughtheLMA intothetrachea.(B)TheLMAisremovedfromthemouthand pulledup,andthetracheal tubeispasseddown throughthe LMAlumen.(C)Thetrachealtubeisadvanceddownoverthe FBintothetrachea.
passedcompletelythroughtheremoved LMA(Fig.1B)and
advanceddownoverFBintothetrachea(Fig.1C).TheFB
wasremoved,the15mmtubeadapterwasreattachedand
thepropertrachealtubepositionwasconfirmedbyendtidal
CO2andtheauscultationofbilateralbreathingsound.The
patientwasconnectedtomechanicalventilation.The
over-all airwaymanagement procedure lastedfor 1h and vital
signs were always within normal range. Surgery and the
postoperativeperiodinintensivecareunitwereuneventful.
One month later, thesmall infantwasscheduled for a
laparoscopic Nissenfundoplication. Again, visualizationof
thevocalcordsduringlaryngoscopywithMiller0bladewas
notpossibleandthe oraltrachealintubation was
success-fullyperformedwiththemethoddescribedpreviously.
Discussion
Difficult intubation in pediatric patients is usually
antici-patedandgivesussometimetobeprepared.Nevertheless,
it is always challenging and it requires experience in
handledifficultpediatricairwayanddiverseairway
instru-ments available. Several airway management techniques
havebeendescribedinpediatricpatientswithcraniofacial
malformation.1---17 However,there areonly few devices in
sizesthatfitneonatesandsmallinfants,andthathavebeen
successfullyusedto secure theairwayin TreacherCollins
Syndrome;1,11---13,16wehaveonlyavailableLMAandpediatric
FBsuitable for thosepatients. In the patient reported,a
nasotrachealintubation wasourfirstchoice, becausethis
airway approach is more appropriate for surgical access
in mandibular distraction osteogenesis. Nevertheless, the
nasaltubeprobablybentinside thenasalcavitynarrowed
bythefacialhypoplasia,reducingitslumenandmakingfail
thefiberopticnasalintubation.
The use of aLMA in infants withdifficult intubation is
an establishedmeans for securingthe airway: it provides
apatentairway, itallowsassisted ventilationofthe
anes-thetized child and it serves as a conduit for intubation.
Theproblemwiththisoralintubationtechnique ishowto
removethe LMAand FBwithout dislodging thetube from
thetrachea.18---20 Therearealternativestosolvethisissue
suchastoleave the LMA inplaceif it does notinterfere
withsurgery18,19;toextendthelengthoftrachealtubewith
anothertubeofsimilarsizeandthreadingbothonthe
bron-choscopeusingtheproximaltoholdthedistaltube,3,13,18,19
allowingalsouninterruptedventilationduringwithdrawalof
LMA,20andtoplaceawirethroughthebronchoscopeandto
advanceatubeoverthewire.18,19Inthiscase,ourapproach
wasto use two tracheal tubes, the proximal end of one
wedgedintothedistalendoftheother,toremovetheFBand
LMA.Duetothefailureofnasalintubation,wedecidedfirst
tobesurethatthetrachealtubewiththeFBinsidecould
passthroughtheLMAalreadyinplace.Wethinkthata
simi-larphenomenonofthenasalintubationcouldhappeninthe
oralcavityanditwouldexplainthattheFBloadedwiththe
trachealtubewasstuckinsidetheLMAlumen.The
cranio-facialabnormalitiesofTreacherCollinsSyndromeprobably
reduceanddeformthenasalandoralcavities;inaddition,
thetongue(duetomandibularhypoplasia)protrude
poste-riorlyand may displace and deform the shaft of the LMA
asreportedbyInadaetal.4intheirpediatricpatientswith
TreacherCollinsSyndrome.Theseeventswouldexplainthe
failureofbothfiberopticintubationapproaches.
The LMA left in placeallowed us toventilate, to
oxy-genate and to keep the infant adequately anaesthetized
while we decidedhowto solvethis problem.Afterwards,
weusethefiberopticoral intubationmethodinwhichthe
trachealtubewasadvancedeasilyoverdeFBaftertheLMA
wasremoved.ThismethodwasdescribedbyEllisetal.16to
handletheairwayinaneonatewithanasarcaandlaryngeal
edemaand,astheauthorsmention,isanalternativeoforal
intubationthroughaLMAinsituationswherethelaryngeal
maskitmustberemoved.Tothebestofourknowledgethere
arenopreviousreportsofthesuccessfuluseofthis
intuba-tionmethod ina1 month-oldinfantwithTreacherCollins
Syndrome.
Insummary,wehaveshownthatthemethoddescribedby
Ellisetal.16canbesuccessfullyusedforfiberopticoral
intu-bationthroughtheLMAinsmallinfantswithTreacherCollins
Syndrome.Inouropinion,thekeypointsof difficult
90 R.Fuentesetal.
anesthesia,tomaintainspontaneousventilationandtohave
experienceindifferentintubationtechniques.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.HoskingJ,ZoanettiD,CarlyleA,etal.AnesthesiaforTreacher Collinssyndrome:areviewofairwaymanagementin240 pedi-atriccases.PediatrAnesth.2012;22:752---8.
2.FrawleyG,EspenellA,HoweP,etal.Anestheticimplications ofinfantswithmandibularhypoplasiatreatedwithmandibular distractionosteogenesis.PediatrAnesth.2013;23:342---8.
3.MuraikaL,HeymanJS,ShevchenkoY.Fiberoptictracheal intu-bationthroughalaryngealmaskairwayinachildwithTreacher Collinssyndrome.AnesthAnalg.2003;97:1298---9.
4.InadaT, FujiseK, TachibanaK,et al.Orotrachealintubation throughthelaryngealmaskairwayinpaediatricpatientswith TreacherCollinssyndrome.PaediatrAnaesth.1995;5:129---32.
5.BishopS,ClementsP,KaleK,etal.UseofGlideScopeRangerin themanagementofachildwithTreacherCollinssyndromeina developingworldsetting.PediatrAnesth.2009;19:695---6.
6.PéanD,DesdoitsA,AsehnouneK,etal.Airtraq laryngoscope for intubation in TreacherCollins syndrome. Pediatr Anesth. 2009;19:698---9.
7.Hirabayashi Y, Shimada N, Nagashima S. Tracheal intubation usingpediatricAirtraq®opticallaryngoscopeinapatientwith TreacherCollinssyndrome.PediatrAnesth.2009;19:915---6.
8.SugawaraY,InagawaG,SatohK,etal.Successfulintubation using a simple fiberoptic assisted laryngoscope for Treacher Collinssyndrome.PediatrAnesth.2009;19:1031---3.
9.Ebata T, Nishiki S, Masuda A, et al.Anesthesia for Treacher Collinssyndromeusinglaryngealmaskairway.CanJAnaesth. 1991;38:1043---5.
10.Jagannathan N, Roth AG, Sohn LE, et al. The new air-QTM intubatinglaryngealairwayfortrachealintubationinchildren withanticipateddifficultairway:acaseseries.PediatrAnesth. 2009;19:618---22.
11.Bucx MJL, Grolman W, Kruisinga FH, et al. The prolonged use ofthe laryngeal mask airway in a neonate withairway obstructionandTreacherCollinssyndrome.PaediatrAnaesth. 2003;13:530---3.
12.NilssonE,IngvarssonL,IsernE.TreacherCollinssyndromewith choanalatresia:onewaytohandletheairway.PediatrAnesth. 2004;14:700---1.
13.AsaiT,NagataA,ShinguK.Awaketrachealintubationthrough thelaryngealmaskinneonateswithupperairwayobstruction. PediatrAnesth.2008;18:77---80.
14.Gómez-Rios MA, Serradilla LN, Alvarez AE. Use of the TruView EVO2 laryngoscope in Treacher Collins syndrome after unplanned extubation. J Clin Anesth. 2012;24: 257---8.
15.ShurryM,HansonRD,KoveleskieJR,etal.Managementofthe difficultpediatricairwaywithShikaniOpticalStyletTM.Pediatr Anesth.2005;15:342---5.
16.Ellis DS, Potluri PK, O’Flaherty JE, et al. Difficult airway management intheneonate: a simplemethod ofintubating through a laryngeal mask airway. Paediatr Anaesth. 1999;9: 460---2.
17.Holm-KnudsenR.Thedifficultpediatricairway---areviewof newdevicesforindirectlaryngoscopyinchildrenyoungerthan twoyearsofage.PediatrAnesth.2011;21:98---103.
18.WalkerRW,EllwoodJ.Themanagementofdifficultintubation inchildren.PediatrAnesth.2009;19:77---87.
19.WheelerM,CotéCJ,TodresD.Thepediatricairway.In:CotéCJ, LermanJ,TodresD,editors.Practiceofanesthesiaininfants andchildren.4thed.Philadelphia,PA:SaundersElseiver;2009. p.237---78.