From the Division of Respiratory Diseases – INCOR, University of São Paulo School of Medicine, São Paulo – Brazil.
EFFECTIVENESS OF SILVER NITRATE COMPARED
TO TALC SLURRY AS PLEURAL SCLEROSING
AGENT IN RABBITS. INFLUENCE OF CONCOMITANT
INTRAPLEURAL LIDOCAINE
Francisco S. Vargas, Alipio O. Carmo, Evaldo Marchi, Marcelo A.C. Vaz, Karine P. Ramos, Viviane C. Mattos and Lisete R. Teixeira
RHCFAP/2992 VARGAS, FS et al. - Effectiveness of silver nitrate compared to talc slurry as pleural sclerosing agent in rabbits. Influence of concomitant intrapleural
lidocaine. Rev. Hosp. Clín. Fac. Med. S. Paulo 54 (6):199-208, 1999.
SUMMARY: The ideal agent for producing pleurodesis has not been identified. Talc, the most commonly used, poses several problems. Another possibility is silver nitrate, which was widely used in the past.
Purpose: To determine the influence of the intrapleural instillation of lidocaine in producing a pleurodesis with silver nitrate, to define the effect of lidocaine in the maturation of the collagen fibers, and to confirm that the pleurodesis after silver nitrate is stronger than after talc.
Methods: We studied three groups of 8 rabbits. Two groups received 0.5% silver nitrate; in one we had previously injected 0.5 ml of 2% lidocaine. The third group received 400 mg/kg talc (2 ml). The animals were sacrificed 28 days after the injection, and the pleural spaces were assessed grossly for evidence of pleurodesis and microscopically for evidence of inflammation and fibrosis. The total amount of pleural collagen and the distribution of thick and thin collagen fibers were quantified. Collagen was identified using picrosirius red stain.
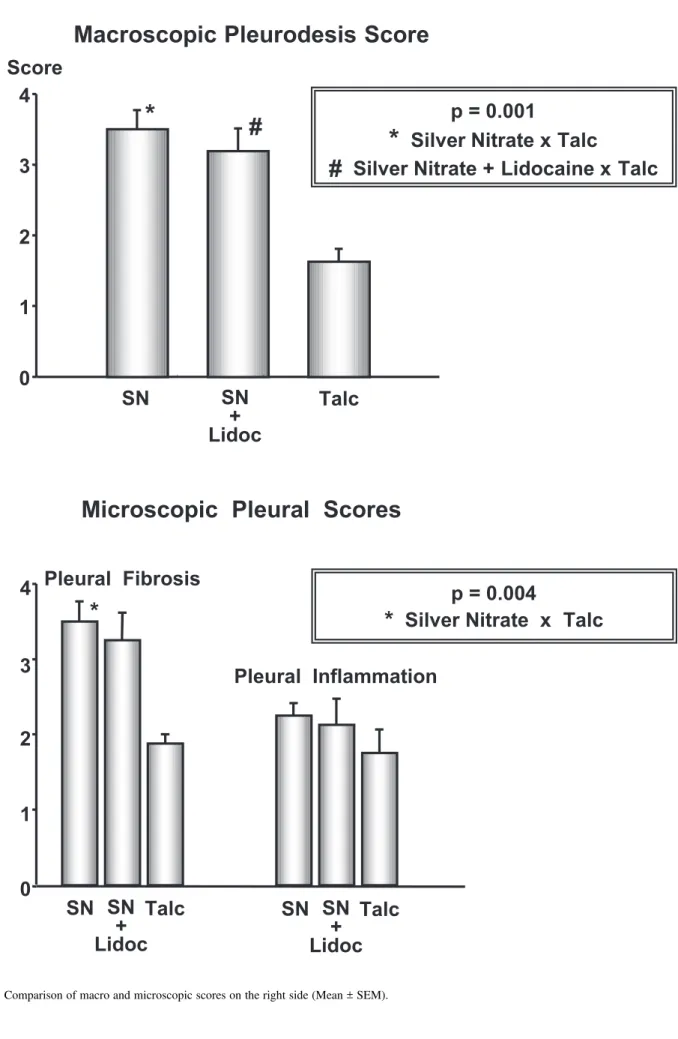
Results: In the two groups that received silver nitrate (without lidocaine: 3.5 + 03 and with lidocaine: 3.2 + 0.3), the macroscopic pleurodesis (scale 0 – 4) was significantly (p = 0.001) better than that resulting from talc (1.6 + 0.2). The mean degree of pleural fibrosis induced by silver nitrate (3.5 + 0.2) was significantly (p = 0.004) higher than that induced by talc (1.9 + 0.1). The previous instillation of lidocaine resulted in a tendency for decreased amounts of fibrosis (3.1 + 0.4). The mean amount (103mm2) of pleural collagen was significantly (p = 0.009) greater in the rabbits that received silver
nitrate (116.9 + 22.7) than in those that received talc (10.7 + 3.4). The injection of lidocaine slightly reduced the collagen (80.1 + 30.3). The distribution of collagen fibers did not differ among the groups.
Conclusion: This rabbit model clearly confirms that intrapleural silver nitrate is more effective than talc for producing pleurodesis. The previous intrapleural instillation of lidocaine results in a decreasing trend in the amount of collagen, but does not change the effectiveness of the pleural fusion or modify the process of collagen maturation.
DESCRIPTORS: Pleurodesis. Talc. Silver nitrate. Pleural effusion. Lidocaine. Collagen.
Pleurodesis is observed when a fi-brotic process between the parietal and visceral pleura occurs as the response to a sclerosing agent injected into the pleural space1. Currently, talc is
ac-cepted by many as the agent of choice for patients with a malignant pleural ef-fusion. Talc is popular for several rea-sons: a) it is effective in the experimen-tal situation2, b) in humans it is
appar-ently more effective than tetracycline derivatives3, c) its administration did
not interfere with chemotherapy4, d) it
is widely available5, and e) it is less
ex-pensive than other sclerosing agents5.
However, there are concerns: a) acute respiratory distress syndrome develops in up to 8% of patients6,7,and b) the
mortality due to the intrapleural admin-istration is about 1%6,7.
Silver nitrate is also inexpensive and widely available. It was used in the past with success8-10 and abandoned in
the 1980s for no clear reasons,
prob-ably due to severe side effects, mainly chest pain requiring large doses of opi-ates11. The morbidity previously
en-countered apparently was due to the high concentrations used (1% – 10%). In experimental studies in rabbits, we demonstrated that the intrapleural ad-ministration of 0.5% silver nitrate pro-duces a pleurodesis that is comparable to that produced by tetracycline12 and
that is better than the pleural sclerosis produced by talc13.
into the pleural space has been sug-gested. However, in an experimental study in rabbits, we demonstrated that the intrapleural administration of lidocaine (Lido), reduces the effective-ness of pleurodesis when the scleros-ing agent is sodium hydroxide14.
The objectives of the present study are: a) to confirm the previous obser-vation13 that the pleurodesis obtained
with silver nitrate is stronger than that observed after talc and that the distri-bution of collagen fibers is similar with both agents and b) to assess whether lidocaine injected intrapleurally before silver nitrate has any effect on the sub-sequent pleurodesis.
METHODS
The methods have been described in previous studies12,15. New Zealand
white rabbits weighing 2.0 to 2.5 kg were anesthetized with an intramuscu-lar injection of ketamine hydrochloride (35 mg/kg) plus xylazine hydrochlo-ride (5 mg/kg). The thorax was pre-pared for aseptic surgery by shaving the right chest wall and then cleaning it with povidone-iodine. A 2-cm skin incision was made midway between the spine and the sternum. The muscles in the seventh or eighth intercostal space were bluntly dissected to allow visualization of the parietal pleura. The sclerosant was injected under direct vi-sualization. In sequence, the muscle and the skin were sutured. After the surgery, the rabbits were monitored for clinical evidence of pain (vocalization, tachypnea, and restlessness). Rabbits showing signs of distress were given buprenorphine hydrochloride 0.05 mg/ kg, subcutaneously. The study was ap-proved by the Ethics Committee of the Heart Institute (InCor), University of São Paulo Medical School, which over-sees research involving both animals and humans.
The rabbits were divided in three
groups of 8 animals. Two groups re-ceived 2 ml of 0.5% silver nitrate (SN, AgNO3 — Merck, Germany); in one of these two groups we injected 0.5 ml of 2% lidocaine hydrochloride 3–5 min-utes before receiving SN. The third group received 400 mg/kg of sterilized talc in 2 ml of saline. The talc was as-bestos free, with a mean particle size of 25.4 mm (90% percentile of 50.5 mm), contaminated with minute amounts of dolomite, kaolite, cholrite and forsterite (Xilolite, Brazil). The talc slurry was gently shaken immedi-ately before injection.
Rabbits were sacrificed 28 days af-ter the procedure by a lethal injection of pentobarbital into the marginal ear vein. The thorax was removed en bloc. The
lung was expanded by the injection of 10% formalin intratracheally. Then the trachea was ligated, and the entire tho-rax was submerged in 10% neutral buff-ered formalin for at least 48 h.
Necropsy was performed by two of the investigators, who were blinded to the treatment group. Each pleural cav-ity was carefully exposed by making bilateral incisions through the dia-phragms and all the ribs in approxi-mately the midclavicular line. In this manner, the sternum and the medial portions of the anterior ribs were re-moved to allow evaluation of the pleu-ral cavities. The left hemithorax re-ceived no injection and was used as a control.
The macroscopic pleurodesis was graded according to the following scheme: 0 normal pleural space; 1 -less than three adhesions; 2 - more than three adhesions, but localized; 3 - gen-eralized scattered adhesions and 4 - complete obliteration of pleural space by adhesions.
The presence of hemothorax was graded on a zero to 4 scale; 0 meaning no hemothorax, 1 indicating a hemotho-rax involving less than 15% of the hemithorax, 2 indicating involvement of from 15% to 33%, 3 indicating
involve-ment of from 33 to 75%, and 4 indicat-ing greater than 75% involvement. At gross examination, the diagnosis of he-mothorax was made if there were blood clots in the pleural space. Atelectasis was classified as none (0), partial (1) or complete (2). Mediastinal shift was clas-sified as none (0), slight (1), moderate (2) or severe (3).
Samples of the visceral pleura and lung from each hemithorax were ob-tained and placed in neutral buffered 10% formalin. These tissue samples for histologic examination were processed routinely and stained with hematoxylin-eosin and picrosirius16,17. The degree of
microscopic inflammation and fibrosis was defined from the hematoxylin-eosin slides, and the total collagen was deter-mined from picrosirius red-stained slides. The microscopic slides were evaluated by two of the investigators who were blinded to the treatment. The inflammation and fibrosis were graded as none (0), equivocal (1), mild (2), moderate (3) or severe (4). Collagen fi-bers were subdivided into thick and thin fibers after picrosirius red staining16.
The enhancement of collagen birefrin-gence elicited by picrosirius staining is specific for collagen. Thin (immature) fibers are green and weakly birefrin-gent, while thick (mature) fibers are yel-low and strongly birefringent18.
Both collagen and fibers were mea-sured using a Leica Q500IW Imaging Workstation provided with an Image Processing and Analysis System (Leica Imaging Systems Ltd), which allows quantitative geometric and densitomet-ric measurements.
Statistical Analysis: All data are
ex-pressed as the mean + SEM. One-way analysis of variance (ANOVA) was used to compared the data among the groups (Sigma Stat; Jandel Scientific). Differences in the results were consid-ered significant when p < 0.05.
RESULTS
The intrapleural instillation of sil-ver nitrate with or without lidocaine resulted in a significantly greater de-gree of pleurodesis than did talc slurry (Table 1). The mean pleurodesis score after the intrapleural injection of 0.5% silver nitrate alone (3.5 + 0.3) or with lidocaine (3.2 + 0.3) was significantly higher (p = 0.001) than that obtained after talc (1.6 + 0.2) (Fig 1). Seven of eight rabbits (87.5%) that received sil-ver nitrate alone and five of eight (62.5%) that also received lidocaine had an effective pleurodesis (score 3 or 4), and no rabbit with talc had a score above 2. The scores on the left hemithorax were 0 for all the animals (Table 2).
The intrapleural injection of silver nitrate resulted in significantly (p =
0.004) more mediastinal shift (1.9 + 0.4) than the intrapleural injection of talc slurry (0.0 + 0.0). The mediastinal shift after the administration of silver nitrate and lidocaine (0.6 + 0.4) was minimal. There were two rabbits with hemothorax (grade 2 and 3) in the sil-ver nitrate group and two (grade 1) in the silver nitrate plus lidocaine group. Six of the eight (75%) rabbits that re-ceived silver nitrate and two of the eight (25%) that received silver nitrate plus lidocaine had grade 2 or higher atelectasis of the ipsilateral lung, while none of the rabbits that received talc had any atelectasis (Table 1). On the control side, no rabbit in either group developed mediastinal shift, atelectasis, or hemothorax (Table 2).
When the pleura was examined mi-croscopically, the intrapleural adminis-tration of silver nitrate without lido-caine also resulted in more fibrosis (Table 1). The degree of pleural fibro-sis after the administration of 0.5% sil-ver nitrate alone (3.5 + 0.2) was sig-nificantly greater (p = 0.004) than that after talc (1.9 + 0.1). There was no sta-tistical differences after injection of sil-ver nitrate and lidocaine (3.1 + 0.4) (Fig 1). The degree of pleural
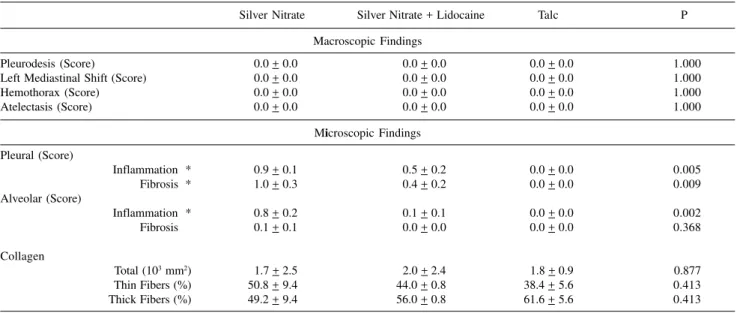
inflam-mation on the injected side (Table 1) was similar in all groups (p = 0.459). The mean degree of alveolar inflam-mation and fibrosis was also signifi-cantly higher in the silver nitrate group than in the talc group (Table 1). There was no statistical difference after silver nitrate with lidocaine. On the control side (Table 2), rabbits in the silver ni-trate group had significantly more pleural inflammation (p = 0.005) and fibrosis (p = 0.009) than those in the talc group; however, no differences were seen in the silver nitrate plus lidocaine group.
The total production of pleural col-lagen (Table 1, Fig 2) was higher (p = 0.009) after silver nitrate (116.9 + 22.7 103mm2) than after talc (10.7 + 3.4
103mm2); no statistical differences
were observed in the group that also received lidocaine, as compared to the talc group (80.1 + 30.3 103mm2). Thus,
previous intrapleural injection lido-caine resulted in a tendency for de-creased pleural fibrosis and deposition of collagen (Fig 3). After 28 days of the intrapleural injection of the scleros-ing agents, the pleurodesis observed showed the predominance of mature (thick) fibers in all groups. There were
Table 1 - Results from macroscopic and microscopic examination of the right side after the intrapleural instillation of the sclerosant (Mean + SEM).
Silver Nitrate Silver Nitrate + Lidocaine Talc P
Macroscopic Findings
Pleurodesis (Score) # * 3.5 + 0.3 3.2 + 0.3 1.6 + 0.2 0.001
Right Mediastinal Shift (Score) * 1.9 + 0.4 0.6 + 0.4 0.0 + 0.0 0.004
Hemothorax (Score) 0.6 + 0.4 0.1 + 0.1 0.0 + 0.0 0.305
Atelectasis (Score) * 2.4 + 0.5 0.9 + 0.5 0.0 + 0.0 0.003
Microscopic Findings Pleural (Score)
Inflammation 2.2 + 0.1 2.1 + 0.4 1.7 + 0.3 0.459
Fibrosis * 3.5 + 0.2 3.1 + 0.4 1.9 + 0.1 0.004
Alveolar (Score)
Inflammation * 2.2 + 0.3 1.6 + 0.4 0.1 + 0.1 0.001
Fibrosis * 1.2 + 0.1 0.7 + 0.1 0.0 + 0.0 <0.001
Collagen
Total (103 mm2) * 116.9 + 22.7 80.1 + 30.3 10.7 + 3.4 0.009
Thin Fibers (%) 33.4 + 3.7 35.6 + 5.1 46.5 + 5.9 0.165
Thick Fibers (%) 66.6 + 3.6 64.4 + 15.4 53.5 + 5.8 0.165
Figure 2 - Comparison of pleural fibrosis and pleural inflammation on right side in the studied groups: talc, silver nitrate and silver nitrate plus lidocaine (Mean + SEM).
Total Collagen
SN
SN
+
Lido
Talc
50
100
150
10
3µ
m
20
p = 0.009
*
Silver Nitrate x Talc
*
Collagen Fibers
0
100
Thin
Thick
50
SN
Talc
%
Figure 3 - Photomicrografs of tissue sections obtained from the pleural fibrosis stained with picrosirius and observed under conventional ilumination and polarized light.
Table 2 - Results from macroscopic and microscopic examination of the left side after the intrapleural instillation of the sclerosant (Mean + SEM).
Silver Nitrate Silver Nitrate + Lidocaine Talc P
Macroscopic Findings
Pleurodesis (Score) 0.0 + 0.0 0.0 + 0.0 0.0 + 0.0 1.000
Left Mediastinal Shift (Score) 0.0 + 0.0 0.0 + 0.0 0.0 + 0.0 1.000
Hemothorax (Score) 0.0 + 0.0 0.0 + 0.0 0.0 + 0.0 1.000
Atelectasis (Score) 0.0 + 0.0 0.0 + 0.0 0.0 + 0.0 1.000
Microscopic Findings Pleural (Score)
Inflammation * 0.9 + 0.1 0.5 + 0.2 0.0 + 0.0 0.005
Fibrosis * 1.0 + 0.3 0.4 + 0.2 0.0 + 0.0 0.009
Alveolar (Score)
Inflammation * 0.8 + 0.2 0.1 + 0.1 0.0 + 0.0 0.002
Fibrosis * 0.1 + 0.1 0.0 + 0.0 0.0 + 0.0 0.368
Collagen
Total (103 mm2) 1.7 + 2.5 2.0 + 2.4 1.8 + 0.9 0.877
Thin Fibers (%) 50.8 + 9.4 44.0 + 0.8 38.4 + 5.6 0.413
Thick Fibers (%) 49.2 + 9.4 56.0 + 0.8 61.6 + 5.6 0.413
no statistical differences (p = 0.165) regarding the distribution between thin or thick fibers among the groups (Fig 2). On the left side, the amount of col-lagen was minimal with no statistical differences.
The intrapleural administration of silver nitrate (with or without lidocaine) or talc slurry was well tolerated; distress was not observed in any of the animals. Only one rabbit in the silver nitrate group died during the anesthesia. After the intrapleural injection of the scleros-ing agent, the animals maintained nor-mal feeding and activities. The rabbits did not require medication for vocaliza-tion, tachypnea, or restlessness.
DISCUSSION
This study confirms that in the rab-bit model, 0.5% silver nitrate (2 ml) is more effective than 2 ml of talc slurry (400 mg/kg) in producing a pleuro-desis13. The study also shows that
pre-vious intrapleural injection (0.5 ml) of 2% lidocaine results in a tendency for decreasing pleural fibrosis and deposi-tion of collagen. However, local anes-thesia does not modify the macro-scopic fusion between the visceral and parietal pleura or the maturation of col-lagen represented by the proportion between thin and thick fibers.
The ideal agent for producing pleurodesis has not been identified. Talc appears to be the most effective agent, but recently it has been associ-ated with ARDS19,20. Bleomycin is
ex-pensive and less effective than the other agents. Tetracycline is unavailable, and the tetracycline derivatives are expen-sive, painful, and not available throughout the world3.
Silver nitrate was one of the first agents used for pleurodesis; more than 50 years ago, Brock21 proposed its use
to create an aseptic obliterative pleuro-desis. Since then, there have been sev-eral reports with contradictory results.
Previous studies in the rabbit model have shown that silver nitrate is as ef-fective as tetracycline22 and more
effec-tive than talc13 in producing
pleuro-desis. The primary advantages of silver nitrate are its low cost and wide acces-sibility; the disadvantages are the se-verity of the side effects, mainly chest pain and pleural exudation.
The mechanism responsible for the pleurodesis that follows intrapleural ad-ministration of the sclerosing agents is incompletely understood. The first event between the intrapleural injection and the fusion of the visceral and parietal pleura appears to be the injury mani-fested by the denudation of mesothelial cells23 and the development of an
exu-dative pleural effusion24. The reparation
of pleural tissue involves several pro-cesses: acute inflammation (day 1), re-generation of the damaged cells, migra-tion of connective tissue cells to the damaged area (days 3–5), synthesis of extracellular matrix (ECM) proteins (days to weeks), and deposition of col-lagen (1st week to several weeks)25.
Collagen is the most important pro-tein in the production of pleurodesis. The first step in the synthesis of col-lagen occurs in the fibroblasts and is represented by the synthesis of propep-tides; while intracellular they aggregate to form procollagen molecules25. These
molecules are subsequently secreted, and in the extracellular space, they ag-gregate to form fibrils called tropocol-lagen. The next step is the oxidation of tropocollagen molecules25 and
forma-tion of thin immature collagen fibers16.
These thin collagen fibers will mature reacting with other collagen fibers to become thick mature collagen fibers16
responsible for the resistance of the visceral pleura to stretching26.
Several factors should be consid-ered regarding the process occurring from the instillation of the sclerosing agent to the tissue repair or the devel-opment of a pleurodesis. The mesothe-lial cell is crucial: the injury represents
the first step—the greater the injury, the more likely is the probability of de-veloping a pleurodesis12; the
mesothe-lial cell is also involved in the repair process27. Mesothelial cells secrete
col-lagen and enzymes such as metallopro-teinases, which degrade collagen, and inhibitors of the metalloproteinases27.
Pleurodesis or tissue repair depends on the balance between the pro-collagen and the anti-collagen factors, if pro-collagen factors are predominant, pleurodesis will occur.
In the development of this study, we planned to confirm that the pleuro-desis with silver nitrate is stronger than that with talc and to clarify whether there is a similar percentage of mature and immature collagen fibers in both silver nitrate and the talc pleurodesis. We also hypothesized that previous in-trapleural injection of lidocaine would decrease the effectiveness of pleuro-desis and that lidocaine would impair the maturation of the collagen fibers.
This research ratifies that a low concentration of silver nitrate (0.5%) is more effective than talc (400 mg/kg) in producing a pleurodesis in rabbits. Sil-ver nitrate produces a greater degree of macro- and microscopic fibrosis. The research also confirms that the pleuro-desis following intrapleural injection of either silver nitrate or talc is character-ized by a similar distribution of col-lagen fiber types. Although the total amount of collagen fibers was signifi-cantly greater after silver nitrate (116.9 mm2) than after talc (10.7 mm2), the
higher inflammation (2.2) and fibrosis (1.2) after silver nitrate; after talc, the lung was normal.
The effect of lidocaine in the pro-duction of a pleurodesis is interesting. The previous intrapleural instillation of 0.5 ml of 2% lidocaine resulted in a strong tendency for a decrease in the degree of macro- and microscopic pleurodesis, but the change did not reach statistical significance. The pro-portion of thin to thick collagen fibers was not modified.
Several mechanisms should be con-sidered to explain these effects. Lido-caine hydrochloride combines chemi-cally with silver nitrate to form AgCl and lidocaine. When lidocaine hydro-chloride and silver nitrate are mixed in a test tube in the proportions used in this protocol, a white salt settles out in the bottom of the mixture. This cer-tainly indicates that some of the silver nitrate is being deactivated, and the amount of the active sclerosant is de-creasing. As this study only shows a tendency to decrease the effectiveness, we believe that the injection of larger volumes of lidocaine would reduce the degree of pleurodesis.
Another possibility is that lidocaine might influence the results by increas-ing the total volume injected and dilut-ing the silver nitrate. This possibility is unlikely since the volume of lidocaine injected was only 0.5 ml and since pre-vious studies with minocycline showed that at the same dose, the pleurodesis
with larger volumes was stronger28.
Finally, the combination of lido-caine with silver nitrate may change the pH. However, the addition of lidocaine hydrochloride to silver nitrate does not affect the pH very much. The pH of silver nitrate is 5.32 and of lidocaine 6.73. When 0.5 ml of lido-caine hydrochloride is mixed with 2 ml of 0.5% silver nitrate, the pH changes to 5.68, and no significant changes in the serial pH measurements are ob-served in this mixture over a 60-minute period. It should be mentioned that Sahn and Good could not demonstrate a relationship between the pH of the sclerosing agent and its effectiveness as a sclerosant24.
Silver nitrate was used in the 1980s to induce pleurodesis and abandoned due to severe side effects including se-vere chest pain and the formation of a large pleural exudation. This study sug-gests that the intrapleural administra-tion of 2 ml of 0.5% silver nitrate pro-duces few side effects. None of the rab-bits appeared distressed after receiving silver nitrate, and all of them resumed a normal feeding pattern and normal activities after administration of silver nitrate.
The local side effects represented by mediastinal shift, presence of atelecta-sis, and the occurrence of hemothoraces in the silver nitrate group are not discon-certing; these changes are less than those observed after the intrapleural ad-ministration of the tetracycline
deriva-tives12. With the tetracycline derivatives,
these complications can be prevented by inserting a chest tube. Our animals did not receive chest tubes.
In conclusion, the present study confirms that 0.5% silver nitrate is more effective than 400 mg/kg of talc in producing a pleurodesis in rabbits. The intrapleural administration of sil-ver nitrate produced a greater degree of macroscopic pleurodesis with a greater amount of microscopic fibrosis and collagen formation. A previous intra-pleural injection of 0.5 ml lidocaine re-sulted in a tendency for decreased the fibrosis and collagen formation. The proportion between thin and thick col-lagen fibers is similar with either talc or silver nitrate. The previous intra-pleural administration of lidocaine did not change the proportion of the col-lagen fibers.
Considering that silver nitrate is in-expensive, widely available and pro-duces an effective pleurodesis without significant side effects in rabbits, we suggest that an evaluation in humans should be undertaken. However intra-pleural anesthesia with lidocaine should be avoided.
ACKNOWLEDGEMENTS: This study was supported by CNPq and FAPESP. The authors would like to thank the assistance of Dr. Roberto Onishi and Solange Aparecida Consorti.
RESUMO RHCFAP/2992
VARGAS, FS e col. – A eficiência da injeção intrapleural de lidocaina na produção de pleurodese com nitrato de prata. Uma comparação entre a pleurodese produzida pelo nitrato de prata e a injeção intrapleural de talco. Rev. Hosp. Clín. Fac. Med. S. Paulo 54 (6):199-208, 1999.
Não está ainda definido, qual o agente ideal para a produção de uma pleurodese efetiva. O talco é o agente mais freqüentemente utilizado apesar de suas manifestações colaterais. Ou-tra possibilidade é o niOu-trato de prata, largamente usado no passado.
Objetivos: Determinar a influência
Métodos: Foram estudados três
gru-pos de 8 coelhos. Dois receberam ni-trato de prata a 0,5%; em um deles, foi injetado previamente 0,5 ml de lido-caina a 2%. O terceiro grupo recebeu 2 ml de talco (400 mg/kg). Os animais foram sacrificados após 28 dias da in-jeção intrapleural e as cavidades pleurais examinadas macroscopica-mente, analisando-se a presença de fu-são entre os folhetos pleurais e micros-copicamente avaliando-se a inflamação e a fibrose. Quantificou-se o total de colágeno na pleura e a distribuição de fibras finas e grossas, utilizando-se a coloração de pricrosirius.
Resultados: Nos dois grupos em
que se injetou nitrato de prata (s/
lidocaina: 3.5 + 0.3 e com lidocaina: 3.2 + 0.3), a pleurodese macroscópica (scala 0 - 4) foi significantemente (p = 0.001) melhor do que a pleurodese re-sultante do talco (1.6 + 0.2). A média da fibrose pleural induzida pelo nitra-to de prata (3.5 + 0.2) foi significan-temente (p = 0.004) mais acentuada do que a produzida por talco (1.9 + 0.1). A instilação prévia de lidocaina deter-minou tendência a diminuir a quanti-dade de fibrose (3.1 + 0.4). A média (103mm2) do colágeno pleural foi
significantemente (p = 0.009) maior nos coelhos que receberam nitrato de prata (116.9 + 22.7) do que naqueles que receberam talco (10.7 + 3.4). A
in-jeção de lidocaina reduziu discreta-mente o colágeno (80.1 + 30.3). A dis-tribuição das fibras colágenas não foi diferente entre os grupos estudados.
Conclusão: Este modelo animal
confirma que, o nitrato de prata inje-tado no espaço pleural mais efetivo do que o talco na produção de pleurodese. A injeção intrapleural de lidocaina de-termina uma tendência a reduzir a quantidade de colágeno, mas não muda a efetividade da sínfise pleural ou mo-difica a maturação do colágeno.
DESCRITORES: Pleurodese. Talco. Nitrato de prata. Efusão Pleu-ral. Lidocaina. Colágeno.
REFERENCES
1. LIGHT RW & VARGAS FS - Pleural sclerosis for the treatment of pneumothorax and pleuraleffusion. Lung 1997; 175:213-223. 2. XIE C, TEIXEIRA LR, WANG N et al. - Serial observations after high
dose talc slurry in the rabbit model for pleurodesis. Lung 1998; 176:299-307.
3. WALKER-RENARD PB, VAUGHAN LM & SAHN SA - Chemical pleurodesis for malignant pleural effusions. Ann Intern Med. 1994; 120:56-64.
4. ADLER RH & SAYER I - Treatment of malignant pleural effusion: a method using tube thoracostomy and talc. Ann Thorac Surg 1976; 22:8-15.
5. KENNEDY L, RUSH VW, STRANGE C et al. Pleurodesis using talc slurry. Chest 1994; 106:342-346.
6. MILANEZ CAMPOS JR, WEREBE EC, VARGAS FS et al. Respiratory failure due to insufflated talc. Lancet 1997; 349:251-252.
7. REHSE DH, AYE RW & FLORENCE MG - Respiratory failure following talc pleurodesis. Am J Surg. 1999; 177:437-440. 8. WIED U, ANDERSEN K, SCHULTZ A et al. - Silver nitrate pleurodesis
in spontaneous pneumothorax. Scand J Thor Cardiovasc Surg 1981; 15:305-307.
9. WIED U, HALKIER E, HOEIER-MADSEN K et al. Tetracycline versus silver nitrate in pleurodesis in spontaneous pneumothorax. J Thorac Cardiovasc Surg 1983; 86:591-593.
10. ANDERSEN J & NISSEN H - Results of silver nitrate pleurodesis in spontaneous pneumothorax. Chest 1968; 54:230-233.
11. WIED U, HALKIER E, HOEIER-MADSEN K et al. - Tetracycline versus silver nitrate pleurodesis in spontaneous pneumothorax. J Thorac Cardiovasc Surg 1983; 86:591-593.
12. VARGAS FS, TEIXEIRA LR, SILVA LM et al. - Comparison of silver nitrate and tetracycline as pleural sclerosing agents in rabbits. Chest 1995; 108:1080-1083.
13. VARGAS FS, TEIXEIRA LR, LIGHT RW, et al. - Silver nitrate is superior to talc slurry in producing pleurodesis in rabbits. Chest (in press).
14. TEIXEIRA LR, VARGAS FS, CARMO AO et al. - Effectiveness of sodium hydroxide as a pleural sclerosing agent in rabbits: influence of concomitant intrapleural lidocaine. Lung 1996; 174:325-332. 15. ROGERS JT, CHENG D, WHEELER A et al. - The effects of tumor
necrosis factor alpha (TNF) blocking antibody on pleurodesis in rabbits. Chest 1998; 114:260S.
16. ANDRADE GB, RIET-CORREA F, MONTES GS et al. - Dating of fibrotic lesions by the picrosirius-polarization method. An application using the lesions of Lechiguana (bovine focal proliferative fibrogranulomatous panniculitis). Eur J Histochem 1997; 41: 203-209.
18. JUNQUEIRA LC & MONTES GS - Biology of collagen-proteoglycan interaction. Arch Histol Jap 1983; 46:589-629.
19. RINALDO JE, OWENS GR & ROGERS RM - Adult Respiratory distress syndrome following intrapleural instillation of talc. J Thorac Cardiovasc Surg 1983; 85:523-526.
20. BOUCHAMA A, CHASTRE J, GAUDICHET A et al. - Acute pneumonitis with bilateral effusion after talc pleurodesis. Chest 1984; 86:795-797.
21. BROCK RC. The use of silver nitrate in the production of aseptic obliterative pleuritis. Guys Hosp Rep 1942; 91:99-103. 22.VARGAS FS, TEIXEIRA LR, SILVA LM et al. - Comparison of silver
nitrate and tetracycline as pleural sclerosing agents in rabbits. Chest 1995; 108:1080-1083.
23. KENNEDY L, HARLEY LA, SHAN SA et al. - Talc slurry pleurodesis. Pleural fluid and histologic analysis. Chest 1995; 107: 1707-1712.
24. SHAN AS & GOOD JT - The effect of common sclerosing agents on the rabbit pleura space. Am Rev Respir Dis 1981; 124:65-67. 25. COTRAN R, KUMAR V & COLLINS T - Robbins Pathologic Basis
of Disease, 6th ed. Pennsylvania, Saunders,1999. p.89-134.
26. LEMOS M, POZO RMK, SANTIAGO G et al. - Organization of collagen and elastic fibers studied in stretch preparations of whole mounts of human visceral pleura. Ann Anat 1997; 179:447-452. 27. MARSHALL BC, SANTANA A, XU QP et al. - Metalloproteinases
and tissue inhibitor of metalloproteinases in mesothelial cells – cellular differentiation influences expression. J Clin Invest 1993; 91:1792-1799.
28. LIGHT RW, WANG NS, SASSOON NS et al. - Comparison of the effectiveness of tetracycline and minocycline as pleural sclerosing agents in rabbits. Chest 1994;106:577-582.