w w w . j c o l . o r g . b r
Journal
of
Coloproctology
Original
Article
Ischemic
colitis:
risk
factors,
diagnosis
and
prognosis
in
patients
undergoing
surgery
Sara
Francisca
Ferreira
Fernandes
a,∗,
Laura
Elisabete
Ribeiro
Barbosa
baMedicineSchool,UniversidadedoPorto,Porto,Portugal
bServiceofGeneralSurgery,CentroHospitalarSãoJoão,EPE,Porto,Portugal
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received11May2015 Accepted28August2015
Availableonline25September2015
Keywords:
Ischemiccolitis Colitis Riskfactors Prognosis
a
b
s
t
r
a
c
t
Objective:Toidentifyriskfactors,diagnosisandprognosisassociatedwithischemiccolitis, focusingmainlyonpatientsundergoingsurgery.
Materialsandmethods:ThisretrospectivestudyincludedallpatientsadmittedtotheCentro HospitalardeSãoJoão–E.P.E.,diagnosedwithischemiccolitisduringtheperiodfrom2012 to2013.
Results:Thestudyincluded154patients;118wereundergoingmedicaltreatment,witha 12%mortalityrate,and36wereundergoingsurgery,witha61%associatedmortalityrate. Hypertensionwasthemostcommonriskfactorinbothgroups.Thepresenceofalarge num-berofcardiovascularriskfactorsinbothgroups,suchashypertensionanddyslipidemia, wasrecorded,butwestillfoundnodirectrelationshipwithdevelopmentofischemic coli-tis.Comorbiditiesthataffectbloodflow,suchasthepresenceofthrombioraneurysms,do provideaworseprognosisandthereforerequireamoreaggressivetreatment.
Conclusion: Thediagnosisofischemiccolitisisnotalwaysimmediatelyestablisheddueto anonspecificpresentation.Surgicaltreatmentshouldbereservedforseverecaseswitha worseprognosisassociated.
©2015SociedadeBrasileiradeColoproctologia.PublishedbyElsevierEditoraLtda.All rightsreserved.
Colite
isquémica:
fatores
de
risco,
diagnóstico
e
prognóstico
em
doentes
submetidos
a
cirurgia
Palavras-chave:
Coliteisquémica Colite
Fatoresderisco Prognóstico
r
e
s
u
m
o
Objetivos:Identificar fatores de risco, diagnóstico e prognóstico associados à colite isquémica,incidindomaisemdoentessubmetidosàcirurgia.
Materiaisemétodos:OestudoretrospetivoincluiutodososdoentesadmitidosnoCentro HospitalardeSãoJoão–E.P.E.comdiagnósticodecoliteisquémicaduranteoperíodode 2012a2013.
∗ Correspondingauthor.
E-mail:mimed09112@med.up.pt(S.F.F.Fernandes).
http://dx.doi.org/10.1016/j.jcol.2015.08.004
Resultados: Oestudoincluiu 154doentes; desses, 118foramsubmetidos a tratamento médico,comumataxademortalidadede12%,e36foramsubmetidosatratamento cirúr-gico,comumataxademortalidadeassociadade61%.Hipertensãoarterialfoiofatorderisco maiscomumemambososgrupos.Foiregistadaapresenc¸adegrandenúmerodefatores deriscocardiovascularesemambososgrupos,comohipertensãoarterialedislipidemia, masaindanãofoiencontradanenhumarelac¸ãodiretacomodesenvolvimentodecolite isquémica.Comorbilidadesqueafetamofluxosanguíneo,comoapresenc¸adetrombosou aneurismas,fazempreverumpiorprognósticoe,porisso,exigemmaioragressividadeno tratamento.
Conclusão: O diagnóstico de colite isquémica nem sempre é imediato, devido a uma apresentac¸ãopoucoespecífica.Otratamentocirúrgicodeveráserreservadoparacasosmais severos,tendopiorprognósticoassociado.
©2015SociedadeBrasileiradeColoproctologia.PublicadoporElsevierEditoraLtda. Todososdireitosreservados.
Introduction
Ischemiccolitisisthemostcommoncauseofischemicchange ofthegastrointestinaltract.1Thisdiseasehasawide
distri-butionindifferentagegroups,withanincidencemainlyin olderpeople.Withtheprogressiveagingofthepopulation,itis estimatedafurtherincreaseofcases.Mortalityrates exceed-ing50%arefound.2Thesehighmortalityratesareinfluenced
byseveralfactors,suchastheexistenceofalargenumberof comorbidities,thelatediagnosisofthiscondition,and inap-propriatetreatment.3Itsincidenceisunknown.4
Ischemiccolitiscanresultfromaninadequateirrigation of the colon wall, with a local tissue hypoperfusion and hypoxia,5andusuallythisconditionhasasegmental
distri-butionaffectingmainlytheleftversusrightcolon(80%and 20%,respectively). Thecompromiseoftheentirecolonisa lessprevalentcondition,affectinglessthan10%ofcases.6
Ischemic colitis can be seen in an occlusive or non-occlusiveform,andinmostcasestheconditionispresentin thenon-occlusiveform,withaslowerflowstateanddecreased bloodperfusion.6–8
Thereareseveralriskfactorsassociatedwithischemic col-itis: age over 65 years, female gender, chronic obstructive pulmonarydisease,hypertension,typeII diabetesmellitus, dyslipidemia, cardiac arrhythmias (including atrial fibrilla-tion), coronary disease, heart failure, chronic obstipation, renal failure, peripheral arterial occlusive disease, among others.6,9,10 Some drugs are associated with ischemic
coli-tis;aspirinanddigitalisareindependentriskfactorsforthe development of this disease.11 Spasmolytic agents, proton
pumpinhibitorsandH2antagonistswerealsoassociatedwith ischemiccolitis.12,13
Inyoungerpatients,theassociatedriskfactorsmaybe dif-ferent,forinstance,vasculitis,pharmaceuticalsanddrugsof abuse,extremephysicalexerciseor airtravels. Contrary to whatoccursinadults,inyoungpeopletherightcolonisthe mostaffectedpart,andthereisstillnoexplanationforthis particularlocation.10,14,15
Theischemiamayhaveasymptomaticpresentationand can beoftransient nature.6 Acute abdominalpain,
vomit-ing, diarrhea and/or hematochezia are the most common
presentations. This more benign form of presentation respondswelltomedicaltreatment.However,anacute pre-sentationmayoccurinamoresevereform,requiringsurgical intervention. Systemic signs of sepsis, and signs of acute respiratorydistressandofperitonealirritation,mustprompt thedoctortosuspectofsevereischemiccolitis.Itisnotalways easytoestablishinafirstphasetheindicationformedicalor surgical treatment.Additionaldiagnostic means,for exam-ple,computedtomography, CTangiographyorcolonoscopy, are usedtoobtainamoreaccuratediagnosis,andphysical characteristicsarethecornerstoneofthisdiagnosis.16
Comparedtothemoresevereforms,atransientischemic colitisisassociatedwithabetterprognosis.Thesurgical mor-talityforpatientswithacuteischemiccolitisvariesbetween 10% and 65% of cases, and in patients with a total col-itis it can reach 75%.16 Risk factors that predict a worse
prognosisaremalegender,hypertension,renalfailure,right coloninvolvement,thepresenceofperitonealirritation,lack of hematochezia, and mesenteric atherosclerosis, among others.17–19
Theaimofthisstudyistoidentifyriskfactorsand eval-uatethediagnosisestablishedandtheassociatedprognosis, focusingmainlyonpatientsundergoingsurgery.
Materials
and
methods
Theretrospectivestudyincludedallpatientsadmittedtothe
CentroHospitalardeSãoJoão–EPEdiagnosedwithischemic col-itisduringtheperiodfrom2012to2013.Theidentificationof thosepatientswasbasedontheInternationalClassification ofDiseases.ThestudywasapprovedbytheEthics Commit-teeforHealthoftheCentroHospitalardeSãoJoão–EPE.Those patientsdiagnosedwithischemiccolitiscausedbyvolvulus, obstructionorherniawereexcludedfromthestudy.
Medical treatment
118/154 (76.6%)
Surgical treatment
36/154 (23.4%)
Survival
14/36 (38.9%)
Death
22/36 (61.1%) Survival
104/118 (88.1%)
Death
14/118 (11.9%) Ischemic colitis
154
Fig.1–Resultsof154patientswithischemiccolitis.
wereanalyzed.Thisinformationwasprovidedbyasearchof eachmedicalrecordbySClinicprogram.
AllvariableswereanalyzedusingSPSS22.0forWindows (SPSS,Chicago,IL).Inthefaceofthesmallnumberofcasesin oursample,onlyadescriptiveanalysiswascarriedout.
Thestudywascomplementedbyabriefreviewofthetopic basedonasearchinPubMed,usingkeywordssuchas“COLITE ISQUÊMICA/ISCHEMICCOLITIS”,andpaperspublishedsince 1985.
Results
Thestudyincluded154patients.Thegroupundergoing med-icaltreatment(groupM)consistedof118patients(39 men and79 women)and thegroupofsurgicaltreatment(group S)consistedof36patients(20menand16women)(Fig.1).The meanageofMandCgroupswere74.3and70.9years, respec-tively.Ameanof10.5(SD±12.4)daysofadmissionforMgroup and25.2(SD±24.3)daysforgroupC(Table1)wasobtained.
Hypertensionwasthemostcommoncomorbidityinboth groups(groupM,61.0%andgroupS,58.3%).IntheMgroup,
Table1–Patientcharacteristics.
Patients,n(%)
Medicalt. Surgicalt.
Meanage±SD 74.3±13.1 70.9±13.6 Daysofhospitalization,mean±SD 10.5±12.4 25.2±24.3 Gender
Male 39(33.1) 20(55.6)
Female 79(66.9) 16(44.4)
Comorbidities
DiabetesmellitusII 26(22.0) 10(27.8) Dyslipidemia 50(42.4) 10(27.8) Hypertension 72(61.0) 21(58.3) Coronarydisease 31(26.3) 8(22.2) Inf.mesent.a.thrombus 0(0.0) 1(2.8) Sup.mesent.a.thrombus 6(5.1) 3(8.3) Abdominalaortathrombus 0(0.0) 1(2.8) Abdominalaortaaneurism 1(0.8) 5(13.9) Commoniliaca.aneurism 0(0.0) 2(5.6) Chronicrenalfailure 21(17.8) 8(22.2) Colonneoplasm 2(1.7) 1(2.8) Auricularfibrillation 15(12.7) 5(13.9) Habitualmedication
ASA 17(14.4) 9(25.0)
Statins 26(22.0) 2(5.6)
ASAandstatins 26(22.0) 4(11.1)
we foundthat dyslipidemia waspresent in42.4% ofcases andingroupCin27.8%ofcases.Welookedatother comor-bidities present at diagnosis:diabetes mellitus II, coronary disease, presenceof thrombus in the superior mesenteric, inferiormesenteric,andabdominalaorticarteries,aneurysm oftheabdominalaortaandcommoniliacartery,diagnosticof chronickidneyfailure,coloncancerhistoryanddiagnosisof atrialfibrillation(Table1).
Comparedtostandardmedicationtakenbypatients,we observedthatthegroupthatunderwentmedicaltreatment usesaspirin(14.4%)andstatins(22%)withregularity.Inthe groupundergoingsurgery,25%ofthepatientsuseaspirin,and 5.6%usestatins(Table1).
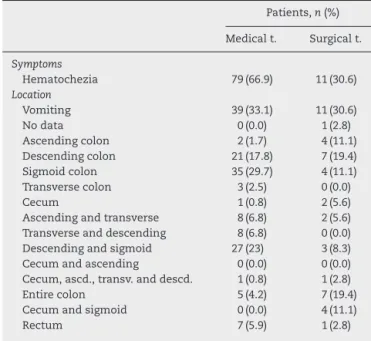
Amongsymptomsonadmissionofpatients,wefoundthat 66.9%ofthoseinMgrouphadhematocheziaand33.1%were admittedwithvomiting.IngroupS,30.6%hadhematochezia and30.6%ofcaseswereadmittedwithvomiting(Table2).
Sigmoidcolonwasthemostaffectedinthegroup under-goingmedicaltreatment;thislocationwasnotedin35cases (29.7%), followed by descending and sigmoid colon in 27 patients(23%),descendingcolonin21(17.8%),ascendingand transversecolonsandtransverseanddescendingcolons,both with8cases(6.8%each),rectumin7cases(5.9%),involvement oftheentirecolonin5cases(4.2%),transversecolonin3cases
Table2–Symptomspresentedandlocationofischemic colitis.
Patients,n(%)
Medicalt. Surgicalt.
Symptoms
Hematochezia 79(66.9) 11(30.6) Location
Vomiting 39(33.1) 11(30.6)
Nodata 0(0.0) 1(2.8)
Ascendingcolon 2(1.7) 4(11.1) Descendingcolon 21(17.8) 7(19.4) Sigmoidcolon 35(29.7) 4(11.1) Transversecolon 3(2.5) 0(0.0)
Cecum 1(0.8) 2(5.6)
Ascendingandtransverse 8(6.8) 2(5.6) Transverseanddescending 8(6.8) 0(0.0) Descendingandsigmoid 27(23) 3(8.3) Cecumandascending 0(0.0) 0(0.0) Cecum,ascd.,transv.anddescd. 1(0.8) 1(2.8)
Entirecolon 5(4.2) 7(19.4)
Cecumandsigmoid 0(0.0) 4(11.1)
0 2 4 6 8 10 12 14 16
Male Female
Ischemic colitis
Shock
AAA rupture
Iliac a. rupture
CRF
Dermatological disorder Hematological disorder
Knife wound
Fig.2–Reasonofhospitalizationinpatientsundergoing surgery.
(2.5%),ascendingcolonin2cases(1.7%)andcecumandblind, ascending,transverseanddescendingcolons,in1case(0.8%), respectively(Table2).
In the group undergoing surgery, the descending colon was the most affected;this location was noted in7 cases (19.4%),followedbytheentirecolonalsoin7cases(19.4%), ascendingcolon,sigmoidandcecumandsigmoidin4cases, respectively (11.1%), descending and sigmoid colons in 3 cases(8.3%),transverseandblindcolonswith2cases(5.6%), respectively,rectumandblind,ascending,transverseand des-cendingcolonsin1case(2.8%),respectively(Table2).
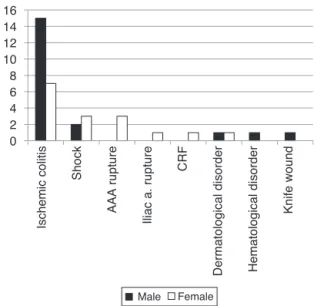
Aseriesofanalyseswascarriedoutfocusingonlyinthe group undergoing surgery, including reason for admission (Fig.2),imagingchangesinabdominal-pelvicCTand rectosig-moidoscopythatledtothediagnosisofischemiccolitisand typeofsurgeryperformedandassociatedmortality(Table3). Ischemic colitis was notthe onlycause for hospitaliza-tioninthegroupsubmittedtosurgery.Twenty-twoadmitted patients had ischemic colitis, including 15 males and 7 females.Shockwasalsooneoftheadmissiondiagnoses,with developmentofischemiccolitisfollowingtheclinicalpicture
Table3–Mortalityassociatedwithdifferenttypesof surgery.
Mortality Total
Yes No
Procedure
Righthemicolectomy 3 3 6
Lefthemicolectomy 2 5 7
Totalcolectomy 4 2 6
Sigmoidectomy 4 1 5
Subtotalcolectomy 2 1 3
Ileocecalremoval 0 1 1
Arteriography 0 1 1
Exploratorylaparotomy 7 0 7
in5patients(2malesand3females).Otheradmission diag-noseswerenoted,suchasabdominalaorticaneurysmrupture (3 cases,100% female patients), ruptured aneurysmof the commoniliacartery(1female),acuterenalfailure(1female), dermatologicalpathology(1maleand1female),a hematolog-icaldisorder(1male)andaknifeinjury(1male)(Fig.2).
Withregardtoimagingchangesthatledtothediagnosisof ischemiccolitisinpatientsundergoingsurgery,wesoughtthe presenceofairand/orfluidintheabdominal–pelviccomputed tomography.Aerocoliawasobservedin1patient,presenceof freeliquidin24patients,andthecommonpresenceofairand liquidin3patients.Intheremaining8patientsinthisgroup, thesechangeswerenotobserved.
Regardingthetypeofsurgeryperformed,hemicolectomy was carried out in 6patients with50% ofassociated mor-tality,lefthemicolectomyin7patientswithamortalityrate of2/7(28.6%), totalcolectomy in6patientswitha mortal-ity rate of 66.6%,sigmoidectomy in5 cases, ofwhich 80% died, subtotalcolectomy in3cases witha 66.7%mortality rate,andileum–cecalremovalinonly1patientwhosurvived. Arteriographywaseffectivein1patient,andlaparotomywas performedin7cases,withanassociatedmortalityrateof100% (Table3).
Discussion
Ourretrospectivestudyfoundsimilarresultstothoseof pre-viousstudiesshowinghigherprevalenceoffemalegender.20
However,wehavenotedmoremenundergoingsurgery, com-paredtowomen,althoughwithoutstatisticalsignificance.The incidencealsowashigherintheleftcolon,namely: descen-dingcolon(inthegroupthatunderwentmedicaltreatment) andsigmoid(inthegroupundergoingsurgery),whichisinline withwhatisdescribedinliterature.10Thisoccursbecauseof
ananatomicaldecrease ofblood flow,especiallyinthe sig-moidcolon–anareawheretheinferiormesentericarteryand rectalarteriesmeet,andthisexposesthecolontoamore sen-sitiveareaofischemia.Contrarytowhatisdescribed,namely, thattherectumisoneofthemostrichlyirrigatedareas(and thereforelessaffectedbyischemia),10inourstudythatwas
nottheplaceleastaffectedbyischemicrectitis.Thisis prob-ably becausethenumber ofsampleswasnotlargeenough to observethis fact. Inthe medicaland surgicaltreatment groups,themeanageswere74.3and70,9years,respectively. Withincreasingage,colicarteriesbegintoexhibitmore tortu-osity,thusreducingthelocalbloodflow.Inthisstudy,wedid notobserveischemiccolitisinyoungpeople.
Withregard toriskfactors,ourfindings areinlinewith whatisdescribedintheliterature.Wenotedthepresenceof alargenumberofcardiovascularriskfactors,suchas hyper-tensionanddyslipidemia;yetnoassociationbetweenthese factors and ischemiccolitis –anessentiallyfatalcondition – was found.11 It was noted that those comorbidities that
prognosis.21Inourstudy,wenotedthatthiscomorbidityis
moreoftenpresentinthegroupthatrequiredsurgery,which supportsthehypothesisofthegreaterseverityofthedisease andofmoreaggressivenessinthetreatment.Historyofcolon neoplasmwasalsorecorded,whichcanbeexplainedbythe changeofmorphologyandincolonicirrigation,inthe pres-enceofaneoplasticprocess,withcolicobstructionanda con-sequentdecreaseinperfusion,distensionandcolicmotility.22
Studieshaveshownthatatrialfibrillationisanindependent riskfactorforischemiccolitis.23Inourstudy,wefoundthat
thiscomorbidityispresent bothinthegroupthatreceived medicaltreatmentasinthesurgicalgroupatsimilarrates, whichmaysuggestthatthecomorbidityhasnoimpactonthe severityofthediseaseandonthetreatmenttobeadopted.
Wehavefoundthataportionofoursamplehad,as nor-malmedication,acetylsalicylicacid,whichcorroboratesthe relationshipofanti-inflammatoryagentswithlesionsofthe colon,includingthedevelopmentoferosionsorulcerations, which may lead to an infectious process and to ischemic necrosis.24 Several adverse effects of statins already were
described,includingacaseofischemiccolitis.25Inourstudy,
weobservedthatstatinsarepartofthenormal pharmacolog-icalprofileofpatients.
Within the symptoms most often presented, we found that it was not always easy to diagnose ischemic colitis basedonthese symptoms,because theyareoften nonspe-cific. The group that was submitted to medical treatment showedahigherprevalenceofhematocheziaatadmission; andinthegroupthatunderwentsurgery,hematocheziaand vomitinghadthesamepercentageatpresentation.Itmaybe worthrememberingthatpatientswhowereadmittedwithout thesetwosymptomsweresubsequentlysubmittedtosurgery, whichmayindicatethatthesymptomsdidnotpredict treat-mentortheprognosis.
With a higher incidence in the group that underwent surgery,wefoundthatischemiccolitiswasthemostfrequent reasonforhospitalization,butnottheonlyone.Ischemic col-itis followed admissionsfor septicshock, according tothe expected,becausewithasystemicimbalanceinthepresence ofshock,thebodyundergoeschanges,particularlyinterms ofirrigation,andtheischemiceventsoccuratthelevelofthe colon,mainlyduetoamesentericvasospasm.Thispictureof colitisaftershockisdescribedintheliteratureasarare rela-tionship,andthatprimarilyinvolvestherightcolon,26which
wasnotthecaseinourstudy.Onecanexpectthatthe rup-tureofaneurysmsintheabdominalaortacanlatercausean ischemiceventinthecolon,byincreasingthesusceptibilityto hemodynamicimbalance.
Giventhetypeofsurgeryperformedandthemortalityrate, wefoundthatmostoftheprocedureshadapoorprognosis associated,resultinginthedeathofthepatient.Incasesof moreaggressiveness, forinstance,atotalorsubtotal colec-tomy,wefoundthatthemortalityrateishigher,whichisto beexpected.Incaseswherethepatientwenttotheoperating roomandunderwentlaparotomywithoutanyinterventionby otherprohibitiveconditions,themortalityratewastotal.We onlyobservedasinglecaseinwhichthesurgeondecidedin favorofanarteriography,witha100%successrate.We antici-patethatlessinvasivetechniquesforthepatient,andapplied attherighttime,canhaveabetterprognosis.
Overall,themortalityratewaslowerincasesthat under-wentmedicaltreatment,whichisexplainedbythefactthat thereisnonecrosis;besides,thediseasehasamorebenign natureandachancetoevolvemorefavorably.
Incasesofsevereischemiccolitis,surgicaltreatmentisthe bestoptiontoconsider,inordertonottoworsenorpreventa clinicaldeteriorationofthepatient.27
Ourstudyhaslimitations,especiallyasregardstoan insuf-ficientsamplesizetoallowanextrapolationofresults.Ina futurestudy,morefactorspresentinbothgroupswillbe stud-ied.
Conclusion
Ischemiccolitisisacommoncauseofischemiaofthe gastroin-testinaltract,accountingforasignificantnumberofhospital admissions.Thisdiseaseisassociatedwithwell-definedrisk factors.Thediagnosisisnotalwaysimmediatelyestablished, due to some unspecific presentations, and in many cases thisresultsinadiagnosisbasedonsuspicion.Lowdigestive endoscopyandangiotomographyarecriticalstudiesthathelp inthediagnosisandtherapeuticdecision.Medicaltreatment isthebestchoiceforpatientswithalessseverediseaseand amorefavorableprognosis.Surgicaltreatmentisreservedfor patientswhopresentwithirreversibleischemiaorforthose whodidnotrespondtomedicaltreatment.Themortalityrate ishigherinthegroupsubmittedtosurgery.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.ScharffR,LongoE,VartanianM,JacobsL,BahadursinghN, KaminskiL.Ischemiccolitis:spectrumofdiseaseand outcome.Surgery.2003;134:624–30.
2.GuttormsonL,BubrickP.Mortalityfromischemiccolitis.Dis ColonRectum.1989;32:469–72.
3.PaternoF,McGillicuddyE,SchusterK,LongoW.Ischemic colitis:riskfactorsforeventualsurgery.AmJSurg. 2010;200:646–50.
4.GandhiS,HansonM,VernavaM,KaminskiL,LongoE. Ischemiccolitis.DisColonRectum.1996;39:88–100.
5.BarbagelattaM.Anatomic-pathologicdiagnosisofischemic colitis.JChir.1997;1347:97–102.
6.MoszkowiczD,MarianiA,TrésalletC,MenegauxF.Ischemic colitis:theABCsofdiagnosisandsurgicalmanagement.J VisceralSurg.2013;150:19–28.
7.TheodoropoulouA,KoutroubakisI.Ischemiccolitis:clinical practiceindiagnosisandtreatment.WorldJGastroenterol. 2008;14:7302–8.
8.ReillyM,WilkinsB,FuhC,HaglundU,BulkleyB.The mesenterichemodynamicresponsetocirculatoryshock:an overview.Shock.2001;15:329–43.
9.HigginsD,DavisJ,LaineL.Systematicreview:the
epidemiologyofischaemiccolitis.AlimentPharmacolTher. 2004;19:729–38.
11.CubiellaJ,NunezL,GonzalezE.Riskfactorsassociatedwith thedevelopmentofischemiccolitis.WorldJGastroenterol. 2010;16:4564–9.
12.WalkerM,BohnL,CaliC,CookF,AjeneN,SandsE.Risk factorsforcolonischemia.AmJGastroenterol. 2004;99:1333–7.
13.MosliM,ParfitJ,GregorJ.Retrospectiveanalysisofdisease associationandoutcomeinhistologicallyconfirmedischemic colitis.JDigDis.2013;14:238–43.
14.HoS,TheB,GohS.Ischemiccolitisinsystemiclupus erythematosus-reportofacaseandreviewoftheliterature. AnnAcadMedSingap.1987;16:501–3.
15.BrownN,RosenholtzJ,MarshallB.Ischemiccolitisrelatedto cocaineabuse.AmJGastroenterol.1994;89:1558–61.
16.BeckD,Aguilar-NascimentoJ.Surgicalmanagementand outcomeinacuteischemiccolitis.OchsnerJ.2011;11:282–5.
17.A ˜nónR,BoscáMM,SanchizV,ToscaJ,AlmelaP,AmorósC, etal.Factorspredictingpoorprognosisinischemiscolitis. WorldJGastroenterol.2006;98:2018–22.
18.FeuerstadtP,BrandtL.Colonischemia:recentinsightsand advances.CurrGastroenterolRep.2010;12:383–90.
19.ReissfelderC,SweitiH,AntolovicD,RahbariNN,HoferS, BüchlerMW,etal.Ischemiccolitis:whowillsurvive?Surgery. 2011;149:585–92.
20.ChangL,KahlerL,SarawateC,QuimboR,KralsteinJ. Assessmentofpotentialriskfactorsassociatedwith ischaemiccolitis.NeurogastroenterolMotil.2008;20: 36–42.
21.AhnS,LeeH,ChoS,YoonJH,LeeOY,YoonBC,etal.Isend stagerenaldiseaseapoorprognosisfactorofischemiccolitis. KoreanJGastroenterol.2009;53:235–8.
22.ChiuH,ChenC,MoL,ChaoT.GastrointestinalIschemic colitisassociatedwithcoloncancer.JGastroenterolHepatol. 2005;20:1458.
23.SadotE,TelemD,CohenL,AroraM,DivinoC.Nonocclusive ischemiccolitis:analysisofriskfactorsforseverity.AmSurg. 2014;80:454–60.
24.ViethM.NSAID-colonopathy.Pathologe.2006;27:65–72.
25.TanJ,PretoriusC,FlanaganP,PaisA.Adversedrugreaction: rosuvastatinasacauseforischaemiccolitisina64-year-old woman.BMJCaseRep.2012;28.
26.LevandoskiG,DeitrickJ,BrotmanS.Necrosisofthecolonasa complicationofshock.AmSurg.1988;54:621–6.
27.RyooS,OhH,HaH,MoonS,ChoeE,ParkK.Theoutcomes andprognosticfactorsofsurgicaltreatmentforischemic colitis:whatcanwedoforabetteroutcome.