www.jped.com.br
ORIGINAL
ARTICLE
Opinions
of
Brazilian
resuscitation
instructors
regarding
resuscitation
in
the
delivery
room
of
extremely
preterm
newborns
夽
,
夽夽
Cristiane
Ribeiro
Ambrósio
a,b,
Maria
Fernanda
Branco
de
Almeida
c,
Ruth
Guinsburg
c,∗aUniversidadeFederaldeSãoPaulo(UNIFESP),SãoPaulo,SP,Brazil
bUniversidadeFederaldeUberlândia(UFU),DepartamentodePediatria,Uberlândia,MG,Brazil
cUniversidadeFederaldeSãoPaulo(UNIFESP),EscolaPaulistadeMedicina,DivisãodeMedicinaNeonatal,SãoPaulo,SP,Brazil
Received2October2015;accepted5February2016 Availableonline31May2016
KEYWORDS
Newborninfant;
Bioethics;
Resuscitationorders; Cardiopulmonary resuscitation; Fetalviability
Abstract
Objective: TodescribetheopinionsofpediatricianswhoteachresuscitationinBrazilon
initi-atingandlimitingthedeliveryroomresuscitationofextremelypreterminfants.
Method: Cross-sectional study with electronic questionnaire (Dec/2011---Sep/2013) sent to
pediatricianswhoareinstructorsoftheNeonatalResuscitationProgramoftheBrazilianSociety ofPediatrics, containingthreehypothetical clinicalcases:(1) decisiontostartthe delivery roomresuscitation;(2)limitationofneonatalintensivecareafterdeliveryroomresuscitation; (3)limitationofadvancedresuscitationinthedeliveryroom.Foreachcase,itwasrequested thattheinstructorindicate thebestmanagementforeachgestational agebetween23 and 26weeks.Adescriptiveanalysiswasperformed.
Results: 560(82%)instructorsagreedtoparticipate.Only9%oftheinstructorsreportedthe
existenceofwrittenguidelinesattheirhospitalregardinglimitationsofdeliveryroom resuscita-tion.At23weeks,50%oftheinstructorswouldinitiatedeliveryroomresuscitationprocedures. At26weeks,2%woulddecidebasedonbirthweightand/orpresenceoffusedeyelids.Among the participants,38%wouldre-evaluatetheir deliveryroom decision andlimitthe carefor 23-weekneonatesintheneonatalintensivecareunit.Asforadvancedresuscitation,45%and 4%oftherespondents,at23and26weeks,respectively,wouldnotapplychestcompressions and/ormedications.
夽 Pleasecitethisarticleas:AmbrósioCR,deAlmeidaMF,GuinsburgR.OpinionsofBrazilianresuscitationinstructorsregardingresuscitation
inthedeliveryroomofextremelypretermnewborns.JPediatr(RioJ).2016;92:609---15.
夽夽StudycarriedoutattheDivisionofNeonatalMedicine,DepartmentofPediatrics,EscolaPaulistadeMedicina,UniversidadeFederalde
SãoPaulo,SãoPaulo,SP,Brazil;andNeonatalResuscitationProgram,SociedadeBrasileiradePediatria,SãoPaulo,SP,Brazil.
∗Correspondingauthor.
E-mail:ruthgbr@netpoint.com.br(R.Guinsburg).
http://dx.doi.org/10.1016/j.jped.2016.02.012
Conclusion: Difficultycan be observed regardingthe decision to not resuscitatea preterm infantwith23weeksofgestationalage.Atthesametime,asmallpercentageofpediatricians wouldnotresuscitateneonatesofunquestionableviabilityat26weeksofgestationalagein thedeliveryroom.
©2016SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/ 4.0/).
PALAVRAS-CHAVE
Recém-nascido; Bioética;
Ordensquanto
àConduta(Ética Médica); Ressuscitac¸ão Cardiopulmonar; ViabilidadeFetal
Opiniõesdosinstrutoresdereanimac¸ãobrasileirosquantoàreanimac¸ãoemsala departodeemrecém-nascidospré-termoextremos
Resumo
Objetivo: Descreveropiniõesdos pediatrasqueensinamreanimac¸ãonoBrasil arespeito de
iniciarelimitarareanimac¸ãoemsaladepartodeneonatospré-termoextremos.
Método: Estudotransversalcomquestionárioeletrônico(Dez/11-Set/13)enviadoaos
instru-toresdoProgramadeReanimac¸ãoNeonataldaSociedadeBrasileiradePediatriacontendotrês casosclínicoshipotéticos:1)decisãodeiniciarounãoareanimac¸ão;2)limitac¸ãoounãodos cuidadosintensivosapósareanimac¸ãoemsaladeparto;3)limitac¸ãoounãodareanimac¸ão avanc¸adaemsaladeparto.Paracadacasofoisolicitadaaindicac¸ãodacondutaparacadaidade gestacionalentre23-26semanas.Aanálisefoidescritivapormeiodafrequênciadasrespostas.
Resultados: 560(82%)instrutoresconsentiramemparticipar.Apenas9%instrutoresafirmaram
existiremseuhospitalnormaescritasobrequandonãoiniciarareanimac¸ãoemsaladeparto. Com23semanas,50%dosinstrutoresfariamareanimac¸ãoemsaladepartoe,com26semanas, 2%baseariamsuadecisãonopesoaonascere/ounaaberturadafendapalpebral.Dos entrevis-tados,38%reavaliariamsuadecisãoelimitariamocuidadonaUTIamedidasdeconfortopara nascidosde23semanasreanimadosnasaladeparto.Quantoaosprocedimentosdereanimac¸ão avanc¸ada,45%e4%com23e26semanas,respectivamente,nãoindicariamtaismanobras.
Conclusão: Observa-se dificuldadenaopc¸ão denão reanimar neonatos com23 semanas de
gestac¸ãoe,aomesmotempo,umpequenopercentualdepediatrasnãoreanima,nasalade parto,neonatoscujaviabilidadenãoéquestionada(26semanas).
©2016SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Este ´eumartigo OpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4. 0/).
Introduction
Availabledataindicatethatinfantsatlessthan23weeksof gestationalagearetooimmaturetosurvivewiththecurrent
technology;ontheother hand,thosebornat 25weeksor
morehave significantsurvivalratesandalarge proportion ofthemsurvivewithoutseveresequelae.1---4Thus,usingas
guidethesurvivalratesofpretermneonates,theliterature, ingeneral,hasestablishedasthelimitofviabilitytheperiod between22 and 25 weeksof gestational age (GA),below whichthedegreeofbiologicalimmaturityisalimiting fac-tortolifeandabovewhichthebenefitoftreatmentisnot challenged.5,6
However,thereisgreatdifficultyindefiningtheproper managementforfetusesbornbetweentheselimits.During thisperiod,theuncertaintyoftheresultistherule,rather thantheexception,andisthereforereferredtoasthe‘‘gray area,’’ becausesurvival and prognosis areuncertain, and thereisdoubtaboutthebestapproachtobeusedandthe degreeofinvestmentandinterventiontobemade,sincethe dataavailablefordecision-makingarelimited,andalthough theyhelp,theydonotoverruletheuncertaintyorthe pos-sibility oferror. Forthe group ofinfants born in the gray area,twocoursesofactionarepossible:(1)restrictionof
life supportmeasures andthe possibilityof deathas out-come, orincreasein sequelaeifthepatientdoesnotdie; or(2)accesstoallavailabletechnology,havingaspossible outcomesdeathwithpainandsuffering, orthepossibility ofsurvivalwithhighratesofmajorsequelae,orthechance ofagoodclinicalevolution,withsurvivalwithoutsequelae orwithminorsequelae.5,7---10
Therefore, considering the multiple uncertainties, the NeonatalResuscitation Programof theBrazilianSociety of Pediatrics(ProgramadeReanimac¸ãoNeonataldaSociedade BrasileiradePediatria[PRN-SBP])recommendscautionand, considering the additionalinformation obtained after the birth,thedecisionnottoresuscitatemaybemadebythe medicalteaminthedeliveryroomor,ifdoubtsremain,the teammust resuscitate thepatient,take him tothe NICU, and then gather the necessary information, including the family’swishes,inordertoeventuallylimitthelifesupport measures.
whatBrazilianphysicians thinkabouttheseethicalissues. Thus,theaimofthisresearchwastodescribetheopinions ofpediatricianswhoteachresuscitationinBrazilregarding thedecisionstoinitiateandlimitresuscitationofextremely pretermnewbornsinthedeliveryroom,basedon hypotheti-calclinicalcases,comparingthemaccordingtotheBrazilian macro-regionwheretheprofessionalworks.
Method
After being approved by the Research Ethics Committee
of Universidade Federal de São Paulo and the Board of
theBrazilian Society of Pediatrics,a cross-sectionalstudy
was carried out from December 2011 to September 2013
with pediatricians who were active PRN-SBP instructors.
Sample size calculation was not performed, because the
study aimed to evaluate the universe of active PRN-SBP
instructors.
An electronic questionnaire wasdeveloped, using as a
basis the tool validated and utilized by Martinez et al.11
AllactivePRN-SBPinstructors receiveda linktothe ques-tionnaireby email anda personal password access. After enteringthepassword,theinstructorreceivedan explana-tionof theresearch,and afteragreeingtoparticipateby acceptingtheinformedconsent,accesstothequestionnaire wasprovided.
Thequestionnairehadthreeaxes.Thefirstaxisreferred to the characterization of the interviewee, with demo-graphic and professionaldata. The second axis contained 17 multiple-choice questions and an obligatory answer regarding the current practices on neonatal resuscitation andethicalissuesinvolvedintheresuscitationofextremely pretermneonates.Thelastaxisdiscussedthethreeclinical casesthatarethefocusofthisstudy.Theresponsecontrol foreachinstructorwasaccessibleonlytothemain investiga-tor,andanonymitywasguaranteedregardingthetabulation ofresults.
Asforthethreeclinicalcases,thefirstoneconcernedthe decisiontostartresuscitationinthedeliveryroom:Youare calledurgentlytothedeliveryroomtoassistavaginalbirth ofatwinpregnancy.Thefirsttwinwasbornwithirregular breathingandthesecondwasbornwithpoorvitality,with apneaand bradycardia.Therewasnotime totalktothe parentsaboutresuscitation.Indicate,foreachgestational age(23,24,25,and26weeks),thechoice regardingyour management:1)Youresuscitatethetwonewborns;2)You donotresuscitatethesecond,butresuscitatethefirst;3) Youdonotresuscitateeitherofthem;4)Youverifyifthe eyelidsarestillfusedineachnewbornandmakethe deci-siontoresuscitate;5)Youverifythebirthweightofeach patientandmakethedecision.
The second case concerned the limitation or not of neonatalintensive care afterresuscitation in thedelivery room:Assumingthatthetwonewbornsfrom Case1 were resuscitated in the delivery room by the on-duty pedia-trician,whoreferredthemtotheNICUwhereyouareon call.Currently,thepatientsareinthetransportincubator, receiving free flow oxygen and showing intense respira-toryeffort.Indicate,foreachgestationalage(23,24,25, and26weeks),thechoiceregardingyourmanagement:1) Providecomfortcare(heatandfreeflowoxygen);2)Provide
continuous positive airway pressure (CPAP) nasally; 3) Providemechanicalventilationandsurfactant.
The third case addressed the limitation of advanced resuscitation in the delivery room: You are called to the deliveryroomtoassistanextremelypretermneonateborn duetoplacentalabruption.Youtalkbrieflytothemother andexplain about the possibility ofthe child being born in critical condition and dying in the delivery room. The motherasksthateverythingbedonetosavethenewborn’s life.Thepatientisbornshowingapneaandsevere brady-cardia,isquicklyintubatedafterfailedmask ventilation, andremainswithheartrate(HR)<60bpmdespiteadequate ventilation.Indicate,foreachgestationalage(23,24,25, and26weeks),thechoiceregardingyourmanagement:1) Indicatechestcompressionsandadrenaline,andconsiders umbilicalcatheterizationforvolumeexpansion;2)Maintain onlyventilation,transferthepatienttotheNICU,andwait forthe newborn’sdeath;3)Suspendventilationandwait forthenewborn’sdeathtooccurinthedeliveryroom.
Thestatistical analysiswasdescriptive. Thequalitative variablesweredescribed by frequencyof events, andthe quantitative variables, by measures of central tendency. All answers were analyzed for the group as a whole and according tothe regionwhere instructors worked (North, Northeast,andMidwestvs.SouthandSoutheast).The com-parison of the responses according to the five Brazilian macro-regions where the interviewed instructors worked wascarriedoutbychi-squaredtest,withalevelof signifi-canceofp<0.05.
Results
During the study period, there were 829 instructors, of
whom130wereinactiveand14refusedtoparticipate.Thus,
the final target population of the study consisted of 685
activePRN-SBPinstructors.Ofthese,560instructors(82%) answeredthequestionnaire.Thedistributionofinstructors
whoansweredthequestionnaireperstaterangedfrom76%
(São Paulo) to 100% (Amazonas, Rondônia, Roraima, and
EspíritoSanto).
Thegeneralcharacteristicsoftherespondentsareshown inTable1.Themeanageoftherespondentswas45±9years (range:27---67). As for religion, of the 517 whoprofessed theChristianfaith,68%wereCatholics,15%Spiritualists,7% wereevangelicalProtestants,and2%professedother Protes-tantbeliefs.Intermsofplaceofresidence,theinstructors weredistributedasfollows:68(12%)intheNorth,179(32%) intheNortheast,36(6%)intheMidwest,208(37%)inthe Southeast,and 69 (12%) in theSouth, with363 (65%) liv-inginthestate capitalsand197(35%)inthecountryside. Regardingtrainingandprofessionalperformance,thetime sincegraduationfrommedicalschoolwasonaverage22±9
years(range:4---45)andthetimeworkinginneonatologywas 16±8years(range:1---40).
Table1 Generalcharacteristicsofthe560instructorsof theNeonatalResuscitationProgramoftheBrazilianSociety ofPediatricswhoparticipatedinthestudy.
Variable Number Percentage
Age≥45years 296 53
Femalegender 440 79
Stablerelationship 435 78
Haschildren 443 80
Christian 517 92
Religionisveryimportant 349 62 BoardCertificationin
Pediatrics
467 83
BoardCertificationin Neonatology
306 55
Neonatologypractice ≥10years
403 73
Worksinadeliveryroom 490 88 Worksinapublichospital 419 75 Worksinauniversityhospital 243 43 WorksinaNeonatalICU 452 81 Personalexperiencewith
end-of-lifedecisions
226 40
ICU,intensivecareunit.
weightby 299(67%),with33%reportingthatthey
consid-eredgestationalageasthesolecriterionforthedecision,5% reportedconsideringonlybirthweight,and62%considered bothcriteria.For355(80%)respondents,thereported ges-tationalageusedtolimitresuscitationwasbelow24weeks,
andfor263(59%)pediatricians,thebirthweightlimitwas 500g.
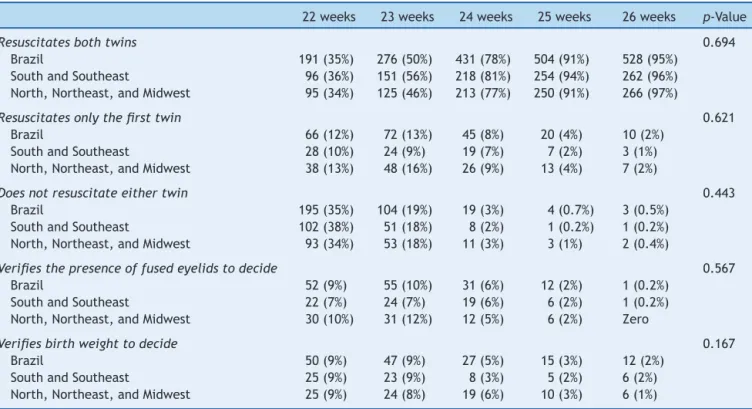
Table 2 shows the percentage of answers to the alternatives related to Case Study 1, according to the gestacionalage(GA)ofeach patient.The greatertheGA, the greaterthe chance theinterviewee wouldresuscitate the two twins. However, even at 23 weeks, 50% of the assessedresuscitationinstructorswouldresuscitatethetwo neonates; at 26 weeks, 2% would base their decision on thebirthweightand/orthepresenceoffusedeyelids.This behavior wasobserved for the instructors asawhole and alsoaccordingtotheirworkarea(chi-squared:p=0.694).
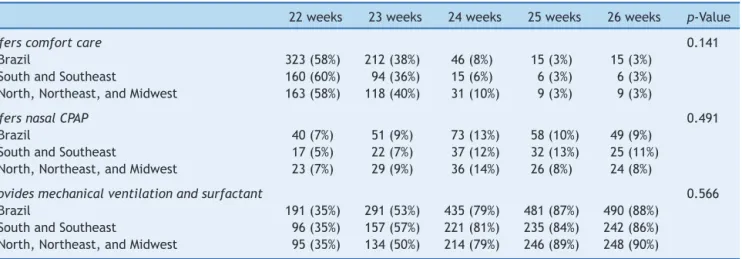
Table 3 shows the percentage of answers for the alternativesrelatedtoCase2accordingtotheGAofeach patient. The greater the GA, the greater the chance the respondentwouldoffer fullintensive care, i.e., mechani-calventilationandexogenoussurfactantreplacement.Part oftherespondentsconsideredthepossibilitythatoncethe neonatewasresuscitatedinthedeliveryroom,theywould reviewthedecisionandprovidecomfortcareintheNICU, as38%oftheassessedpediatricianswouldlimittheICUcare tocomfortmeasuresfornewbornsat23weekofGA effec-tively resuscitated in the delivery room, the same being mentionedby3%ofrespondentsforneonatesat26weeks. Suchbehaviorisobservedfortheinstructorsasawholeand alsoaccordingtotheirareaofwork(chi-squared:p=0.141). Table 4 shows the percentage of answers for the alternatives relatedtoCaseStudy 3,according tothe GA of eachpatient.It isobserved onceagainthat thehigher theGA,thegreaterthechancethattheintervieweewould offer advanced resuscitation, starting chest compressions andmedicationstoresuscitatethenewborn.At23weeks,
Table2 Decisiontostartresuscitationintwinswhenthefirsttwinhad,soonafterbirth,irregularbreathingandthesecond twinhadapnea,accordingtogestationalageandtheBrazilianregionwherethepediatricianworks.
22weeks 23weeks 24weeks 25weeks 26weeks p-Value
Resuscitatesbothtwins 0.694
Brazil 191(35%) 276(50%) 431(78%) 504(91%) 528(95%) SouthandSoutheast 96(36%) 151(56%) 218(81%) 254(94%) 262(96%) North,Northeast,andMidwest 95(34%) 125(46%) 213(77%) 250(91%) 266(97%)
Resuscitatesonlythefirsttwin 0.621
Brazil 66(12%) 72(13%) 45(8%) 20(4%) 10(2%) SouthandSoutheast 28(10%) 24(9%) 19(7%) 7(2%) 3(1%) North,Northeast,andMidwest 38(13%) 48(16%) 26(9%) 13(4%) 7(2%)
Doesnotresuscitateeithertwin 0.443
Brazil 195(35%) 104(19%) 19(3%) 4(0.7%) 3(0.5%) SouthandSoutheast 102(38%) 51(18%) 8(2%) 1(0.2%) 1(0.2%) North,Northeast,andMidwest 93(34%) 53(18%) 11(3%) 3(1%) 2(0.4%)
Verifiesthepresenceoffusedeyelidstodecide 0.567
Brazil 52(9%) 55(10%) 31(6%) 12(2%) 1(0.2%) SouthandSoutheast 22(7%) 24(7%) 19(6%) 6(2%) 1(0.2%) North,Northeast,andMidwest 30(10%) 31(12%) 12(5%) 6(2%) Zero
Verifiesbirthweighttodecide 0.167
Brazil 50(9%) 47(9%) 27(5%) 15(3%) 12(2%)
SouthandSoutheast 25(9%) 23(9%) 8(3%) 5(2%) 6(2%) North,Northeast,andMidwest 25(9%) 24(8%) 19(6%) 10(3%) 6(1%)
Table3 TypeofcareprovidedtothetwinsinCase1attheneonatalintensivecareunitifthosepatientshadbeenresuscitated, accordingtogestationalageandBrazilianregionwheretheinterviewedpediatricianswork.
22weeks 23weeks 24weeks 25weeks 26weeks p-Value
Offerscomfortcare 0.141
Brazil 323(58%) 212(38%) 46(8%) 15(3%) 15(3%) SouthandSoutheast 160(60%) 94(36%) 15(6%) 6(3%) 6(3%) North,Northeast,andMidwest 163(58%) 118(40%) 31(10%) 9(3%) 9(3%)
OffersnasalCPAP 0.491
Brazil 40(7%) 51(9%) 73(13%) 58(10%) 49(9%) SouthandSoutheast 17(5%) 22(7%) 37(12%) 32(13%) 25(11%) North,Northeast,andMidwest 23(7%) 29(9%) 36(14%) 26(8%) 24(8%)
Providesmechanicalventilationandsurfactant 0.566
Brazil 191(35%) 291(53%) 435(79%) 481(87%) 490(88%) SouthandSoutheast 96(35%) 157(57%) 221(81%) 235(84%) 242(86%) North,Northeast,andMidwest 95(35%) 134(50%) 214(79%) 246(89%) 248(90%)
p-Value,significancelevelaccordingtothechi-squaredtest.
55% of the assessedinstructors would offer full advanced
resuscitation to the patient and, at 26 weeks, 4% would
interruptresuscitationeffortsinthissituation.Such behav-iorisobservedforinstructorsasawholeandalsoaccording totheirregion(chi-squared:p=0.738).
Discussion
Themostimportantfindingsofthisstudyare:thesignificant
response rate (82%), which allows us toknow anddepict
the practices of professionals who teach resuscitation in
thedeliveryroominBrazil;thedifficultyinchoosingnotto resuscitatechildrenatthelowerlimitofthegrayzone,at 23weeksofgestation;thepresenceofasmallpercentageof pediatricianswhodonotresuscitateneonatesinthedelivery roomwhoseviabilityisnotquestioned(26weeksgestation);
the extreme difficulty in the delivery room management
for neonates with24---25 weeksof gestation,with hetero-geneousandnotnecessarilyconsistentopinions;andfinally,
thefactthatthereportedneonatalresuscitationpractices arerelativelyuniforminBrazilfromaregionalpointofview. Inasimilarquestionnaireondecisionsmadeinthe
deliv-ery room sent to neonatologists in the state of Illinois,
UnitedStates,theresponseratewas66%.Amongthe
neona-tologists who answered the questionnaire, 55% said they
wouldnot resuscitatea neonate bornat 22 weeksof GA,
astheupperresuscitationlimitfor85%ofthese profession-alswouldbe23---25weeks.12 Thoseauthorsconcludedthat
physicians,todecideonresuscitationinthedeliveryroom, areinfluencedbytheparents’opinionaswellastheirown experienceandopinion.Moreover,thefearofbeingsuedand theethicalteachingsduringmedicaleducationalsoplayan importantroleinthisdecision.Peerzadaetal.,13 in2006,
reportedthat94%ofSwedishneonatologistswhoanswered aquestionnaireconsideredfutileanytreatmentinneonates below23weeksofgestationandthatresuscitationofthose at23weekshaduncertainbenefits,statingtheywouldnot followtheparents’wishesiftheywantedresuscitation.The findingsof this study show a very differentprofile of the
Table4 Managementofaborninpoorconditionduetoplacentalabruption,thatmaintainsheartrate<60bpm,evenafter intubation,whenthemotherhasrequestedthateverythingshouldbedonetosavethenewborn’slife,accordingtogestational ageandBrazilianregionwheretheinterviewedpediatricianswork.
22weeks 23weeks 24weeks 25weeks 26weeks p-Value
Offersadvancedresuscitation 0.738
Brazil 230(41%) 307(55%) 455(82%) 522(94%) 534(96%) SouthandSoutheast 106(37%) 157(57%) 226(81%) 261(96%) 266(98%) North,Northeast,andMidwest 124(44%) 150(55%) 229(81%) 261(95%) 268(96%)
InterruptsPPV,transferstoICU,andwaitsfordeath 0.576
Brazil 170(31%) 158(29%) 74(13%) 20(4%) 4(1%) SouthandSoutheast 88(34%) 76(28%) 35(15%) 8(3%) 0(0%) North,Northeast,andMidwest 82(26%) 82(26%) 39(16%) 12(3%) 4(2%)
InterruptsPPVandwaitsfordeathinthedeliveryroom 0.811
Brazil 155(28%) 90(16%) 26(5%) 13(2%) 17(3%) SouthandSoutheast 80(30%) 41(15%) 13(4%) 5(2%) 8(2%) North,Northeast,andMidwest 75(30%) 49(19%) 13(4%) 8(2%) 9(2%)
assessedpediatricians. Brazilian physicians have difficulty
in making the decision not to start resuscitation, as 50%
of resuscitation instructors would start resuscitation in a patientat 23 weeks, a fact that is in opposition totheir
own opinions, since 88% of them have previously
consid-eredthattheGAlimitforresuscitationshouldbearound24
weeks.Thismismatchbetweenwhatpediatricianssaythey
practiceandwhatthey thinkis theidealinvolves several issues,especiallythe lack of clear guidelinesand criteria forthelimitationoftherapeuticefforts,inadditiontothe
misperceptionsthatpermeateanswersthatdependon
con-ceptsrelatedtowhatisethical,whatismoral,andwhatis legal.Suchbehavioralsoseemstobethereality in South America,asFajardoetal.14 showedin2012that, inLatin
Americancountries,theusualpracticeistoprovide inten-sivecareandnottolimitlifesupport,differentlyfromwhat ispracticedinNorthAmericaandEurope.
Regarding advanced resuscitation, there seems to be great dissent among the instructors who participated in the study in relation to providing chest compressions and medications to extreme preterm infants, as 45% of respondents wouldnot perform advanced resuscitation in 23-weekneonates,while55%wouldperformtheadvanced procedures.Extremelypretermnewbornswhoreceive car-diopulmonaryresuscitationinthedeliveryroomhavea 2.9-to3.7-foldhigherriskofdeathand1.5-to2.3-foldhigher riskofsevereneurologicaldamageinrelationthegroupof patientswhodonotneed thisinterventioninthedelivery room.15,16
Itis alsoworthmentioningthat, althoughthereareno recommendations in this respect, fused eyelids and birth weightalsoguided the decisionregarding resuscitation in the delivery room for several interviewees. Perhaps this is due tothe fact that, in practice, GA is not accurately knownin asignificant numberofcases,which meansthat pediatricians try to estimate it throughparameters that, althoughinaccurate,approximatelyreflectextreme prema-turity. Fusedeyelids are present in approximately 20% of livebirthswithGAbetween24and27weeks,andthus,this conditionisnotagoodparameterfordecision-makinginthe deliveryroom.17Birthweightshouldalsobeconsideredwith
caution,asthereis nodirect association between weight andmaturityofthenewborn,withtheobstetricestimateof fetalweightbeingaccurateinonly15---20%ofcases.18,19
Another interesting point observed in this study was relatedtowhere oneshouldwait forthe deathof infants forwhomthedecisionnottoresuscitatewasmade.There is some difficulty for Brazilian pediatricians in keeping the newborn together with the parents in the delivery room, which is a guideline of the American Academy of Pediatrics.20SuchconductmaybedueinparttothePRN-SBP
guidelines,whichrecommend,whenindoubtorwhenthere isscarcedatatomakeadecision,andespeciallywhenthe GAisnotknown,thatitisbettertoresuscitateinthe deliv-eryroomandpostpone thedecisiontolimit therapyuntil later,when more datacan be obtained tobetter support thedecision.
Despitethewealthofinformation,thestudyhas limita-tions,especiallythe factthat it isbased onanswerstoa questionnaireandonhypotheticalclinicalcases,whichmay significantlydifferfromtheprofessional’sperformanceina real-lifescenario.Anotherissueisrelatedtothechoiceofa
questionnairewithclosedanswersonasubjectinwhichthe subtletyofspeechmayreflectwidevariationsinpractice. Despitetheselimitations,thisisthefirststudythatdiscloses the opinionsof Brazilian pediatricians regarding interven-tionsearlyinlife.
Moreover, even in the international scenario, the extremelyhighpercentageofquestionnaire responsesand thefactthattherespondentsrepresenttheentire popula-tionofopinionmakersregardingneonatalresuscitationare points to be highlighted, and can be usedfor the devel-opmentof clearerguidelinesonthe ethicaldilemmas the pediatrician faces when treating newbornsat the limit of viability.
This study represents an initial step to understand whatpediatricians thinkandhowtheyactin thedelivery room.Thequestionnaireindicatesthattheresuscitationof extremelypretermnewbornsispermeatedbyambivalence andcontradictions. Afrank andcomprehensive debateon thesubjectduringmedicalgraduation,pediatricresidency and neonatal fellowshipis essential toprovide a broader basis for the discussionand supportof resuscitation deci-sions related to the beginning of life in the presence of borderlinematurityconditionsforextrauterinesurvival.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
The authors would like to thank the PRN-SBP instructors
fortheirimportantcollaboration;theStateCoordinatorsof PRN-SBPforencouraginglocalparticipation;andthe Brazil-ianSocietyofPediatricsforsupportingtheresearchinthe contextoftheNeonatalResuscitationProgram.
References
1.SereniusF,KallenK,BlennowM,EwaldU,FellmanV,Holmstrom G,etal.Neurodevelopmentaloutcomeinextremelypreterm infantsat2.5yearsafteractiveperinatalcareinSweden.JAMA. 2013;309:1810---20.
2.Moore GP, LemyreB, Barrowman N, Daboval T. Neurodevel-opmental outcomes at 4 to 8 years of children born at 22 to25weeks’ gestationalage:ameta-analysis.JAMA Pediatr. 2013;167:967---74.
3.deWaalCG,Weisglas-KuperusN,vanGoudoeverJB,Walther FJ,NeoNedStudyGroup,LNFStudyGroup.Mortality,neonatal morbidityandtwo-yearfollow-upofextremelypreterminfants bornintheNetherlandsin2007.PLoSONE.2012;7:e41302.
4.García-Mu˜nozRodrigoF,DíezRecinosAL,García-AlixPérezA, FiguerasAloyJ,VentoTorresM.Changesinperinatalcareand outcomesinnewbornsatthelimitofviabilityinSpain:the EPI-SENStudy.Neonatology.2015;107:120---9.
5.SeriI,EvansJ.Limitsofviability:definitionofthegrayzone.J Perinatol.2008;28:S4---8.
6.BlackmonLR.Biologiclimitsofviability:implicationsforclinical decision-making.NeoReviews.2003;4:e140---6.
8.GriswoldKJ,FanaroffJM.Anevidence-basedoverviewof pre-natalconsultationwithafocusoninfantsbornatthelimitsof viability.Pediatrics.2010;125:e931---7.
9.Haward MF, Kirshenbaum NW, Campbell DE. Care at the edgeof viability:medical and ethical issues. ClinPerinatol. 2011;38:471---92.
10.Cúneo MM. Limitación del esfuerzo terapéutico en terapia intensivaneonatal.Elcasodelosextremadamenteprematuros. Roma:LateranUniversityPress;2012.
11.Martinez AM, Partridge JC, Yu V, Tan KW, Yeung CY, Lu JH, etal.Physiciancounsellingpracticesanddecision-makingfor extremelypreterminfantsinthepacificrim.JPaediatrChild Health.2005;41:209---14.
12.WeissAR,BinnsHJ,CollinsJWJr,deRegnierRA.Decision-making inthedeliveryroom:asurveyofneonatologists.JPerinatol. 2007;27:754---60.
13.PeerzadaJM,SchollinJ,HåkanssonS.Deliveryroom decision-makingfor extremelypreterminfantsinSweden. Pediatrics. 2006;117:1988---95.
14.FajardoCA,GonzálezS,ZamboscoG,CancelaMJ,ForeroLV, Venegas M, et al. End of life, death and dying in neona-tal intensive care units in Latin America. Acta Paediatr. 2012;101:609---13.
15.ShahPS,Sankaran K,AzizK, AllenAC,Seshia M,OhlssonA, etal.Outcomesofpreterminfants<29weeksgestationover
10year period in Canada:a cause for concern?J Perinatol. 2012;32:132---8.
16.WyckoffMH,SalhabWA,HeyneRJ,KendrickDE,StollBJ, Lap-tookAR,etal.Outcomeofextremelylowbirthweightinfants whoreceiveddeliveryroomcardiopulmonaryresuscitation.J Pediatr.2012;160:239---44.
17.BallardJL,KhouryJC,WedigK,WangL,Eilers-WalsmanBL,Lipp R.NewBallardscore,expandedtoincludeextremelypremature infants.JPediatr.1991;119:417---23.
18.Tyson JE, Parikh NA, Langer J, Green C, Higgins RD. National Institute of Child Health and Human Develop-mentNeonatalResearchNetwork.Intensivecareforextreme prematurity-moving beyond gestational age. N Engl J Med. 2008;358:1672---81.
19.Almeida MF, Guinsburg R. Reanimac¸ão neonatal em sala de parto:documentocientíficodoprogramadereanimac¸ão neona-taldaSociedadeBrasileiradePediatria;2013.Availablefrom:
http://www.sbp.com.br/pdfs/PRN-SBP-Reanima%C3%A7%C3% A3oNeonatal-atualiza%C3%A7%C3%A3o-1abr2013.pdf [cited 09.03.15].