Revista
Brasileira
de
Hematologia
e
Hemoterapia
Brazilian
Journal
of
Hematology
and
Hemotherapy
w w w . r b h h . o r g
Original
article
Sickle
cell
disease
and
pregnancy:
analysis
of
34
patients
followed
at
the
Regional
Blood
Center
of
Ribeirão
Preto,
Brazil
Ana
Cristina
Silva-Pinto
a,∗,
Simery
de
Oliveira
Domingues
Ladeira
b,
Denise
Menezes
Brunetta
a,
Gil
Cunha
De
Santis
a,
Ivan
de
Lucena
Angulo
a,
Dimas
Tadeu
Covas
a,baHemocentrodeRibeirãoPreto,FaculdadedeMedicinadeRibeirãoPreto,UniversidadedeSãoPaulo(USP),RibeirãoPreto,SP,Brazil
bFaculdadedeMedicinadeRibeirãoPreto,UniversidadedeSãoPaulo(USP),RibeirãoPreto,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received3September2013 Accepted9June2014 Availableonline16July2014
Keywords:
Anemia Sicklecell Pregnancy
Pregnancycomplications Bloodtransfusion
a
b
s
t
r
a
c
t
Objective:Theobjectiveofthisstudywastoverifytheevolutionofpregnanciesinsicklecell patientsfollowedatoneinstitutionoveraperiodof12years(January2000toJune2012).
Methods:Thestudyevaluated34pregnantwomenwithsicklecelldiseasewithameanage of23.9±5.3years.Theincidenceofobstetriccomplications,non-obstetriccomplications linkedtosicklecelldiseaseandcomplicationsinthenewbornwereanalyzed.
Results:A total of 26% of the cases reported previous miscarriages, 20% had preterm labor,10%hadpre-eclampsia,and5%hadgestationaldiabetes.Forty-onepercentofthe deliveries were cesarean sections and 29%of patients required blood transfusions. In respecttosicklecelldisease,62%ofpatientshadvaso-occlusivecrises,29%hadacutechest syndrome, 23%hadurinarytractinfection,15%hadimpairedcardiacfunctionand6% developedpulmonaryhypertension.Onlyonepatientdiedinthepostnatalperioddueto acutechestsyndrome.Themeangestationalagewas37.8±2.63weeks,andmeannewborn weightwas2.809±643.8g.Thereweresevenfetallosses,includingthreestillbirthsandfour miscarriages. The impact of transfusion therapy on the incidence of maternal–fetal complicationsduringpregnancywasevaluated.
Conclusions: Pregnancyinsicklecellpatientsisstillassociatedwithcomplications.Although no statisticaldifferencewasobservedbetweentransfusedandnon-transfused women, therewerenodeaths(fetalormaternal)intransfusedpatientswhereasonematernaldeath andthreestillbirthsoccurredinnon-transfusedwomen.Alargerstudyofsicklecellpregnant womenwillbenecessarytoelucidatetheactualroleoftransfusionduringpregnancyin sicklecelldisease.
©2014Associac¸ãoBrasileiradeHematologia,HemoterapiaeTerapiaCelular.Published byElsevierEditoraLtda.Allrightsreserved.
∗ Correspondingauthorat:HemocentrodeRibeirãoPreto,FaculdadedeMedicinadeRibeirãoPreto,UniversidadedeSãoPaulo(FMRP-USP),
RuaTenenteCatãoRoxo,2501,CampusUniversitário,MonteAlegre,14051-140RibeirãoPreto,SP,Brazil. E-mailaddress:acristina@hemocentro.fmrp.usp.br(A.C.Silva-Pinto).
http://dx.doi.org/10.1016/j.bjhh.2014.07.002
Introduction
Sicklecelldisease(SCD)comprisesagroupofdiseases char-acterizedbythepresenceofsicklehemoglobin(HbS). Itis classified as sickle cell anemia (Hb SS), hemoglobinopathy SC,hemoglobinopathySD,S-betathalassemia(HbS-beta)and otherassociationsofmutanthemoglobinswithHbS.
In situations of low oxygen tension, Hb S solubility decreases,resultinginthepolymerizationofthesemolecules. The intracellular formation of Hb S polymers affects the redcell structure,changingitinto asickle-shaped,thereby damaging the cell membrane, making it more rigid and exposing a greater number of adhesion molecules on the cell surface, thus increasing the adherence of red cells to thevascularendothelium.1 Thisphenomenon,named
sick-ling, is responsible for the premature destruction of red cells by the reticuloendothelial system, causing a chronic hemolytic anemia. Under stress situations, such as infec-tions, deoxygenation of Hb molecules and sickling of a large number ofred blood cells occur. These cells adhere tothevascularendotheliumwhichmaycausevessel occlu-sionand,consequently, tissueischemia causes thepainful crises that characterize one of the clinical features of thisdisease.Chronichemolyticanemia andfrequent vaso-occlusivecrisescausedamagetovariousorgansandimpair both the survival and the quality of life of patients with SCD.2
Until the 1970s,the management ofsickle cell patients was poor and pregnancy was associated with high mater-nalandfetalmortality.3Nowadays,withnewbornscreening
andpreventivemeasuressuchasvaccinationandantibiotic prophylaxissincebirth,patientsurvivalhasimproved.4
Fur-thermore,thequalityofobstetricandneonatalcarehasalso corroboratedtoasignificantreductioninthematernal mortal-ityrate(from4.1%to1.7%)andimprovedfetalsurvival(from 60to80%).4,5 However,despiteall themedicaladvancesin
recentdecades,pregnancyinsicklecellpatientsisstill associ-atedwithmanyclinicalandobstetriccomplicationscompared tothegeneralpopulation.6–8
Thephysiologicaladaptationsthatoccurinthecirculatory, hematologic,renal,andpulmonarysystemsduringpregnancy canoverburdenorgansthatalreadyhavechronicinjuries sec-ondarytoSCD,increasingtherateofobstetriccomplications suchaseclampsiaandpre-eclampsiaaswellasthe compli-cationsofthedisease,suchasworseningofvaso-occlusive crisesandacutechestsyndrome.7
Objective
Theaimofthis study wastoassess the evolutionof preg-nancyinsicklecellpatientsfollowedatoneinstitution,the FaculdadedeMedicinadeRibeirãoPreto,UniversidadedeSão Paulo (HC-FMRP-USP) in a 12-year period (January 2000 to June2012),anddiscuss theimpactofblood transfusionon pregnancy.
Thisstudywillcontributetotheknowledgeonthe preva-lenceofmaternalandfetalcomplicationsoccurringinthis populationandshowtheimpactoftherapeuticmeasuresused tocontrolthesecomplicationsduringpregnancy.
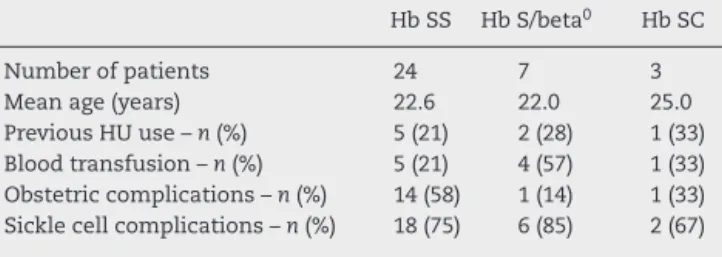
Table1–Characteristicsofthepatientsaccordingto theirsicklecellgenotype.
HbSS HbS/beta0 HbSC
Numberofpatients 24 7 3
Meanage(years) 22.6 22.0 25.0
PreviousHUuse–n(%) 5(21) 2(28) 1(33) Bloodtransfusion–n(%) 5(21) 4(57) 1(33) Obstetriccomplications–n(%) 14(58) 1(14) 1(33) Sicklecellcomplications–n(%) 18(75) 6(85) 2(67)
Methods
Thiswasaretrospectivestudythataimedatanalyzingthe evo-lutionofpregnanciesinsicklecellpatientsduringtheperiod coveredbythestudy(January2000toJune2012).
Studyparticipants
Thesubjects comprisedsickle cell patientsfollowed atthe Hospital das Clinicas, Universidade de São Paulo (USP) in RibeirãoPreto.Patientinclusioncriteriawerehavinga diag-nosis of SCD (Hb SS, Hb S-beta or Hb SC) by hemoglobin electrophoresisandhavinghadoneormorepregnanciesfrom January2000toJune2012.Thepatientswerethendividedin twogroupsinordertoevaluatetheimpactofblood transfu-sionsonsicklecellcomplicationsduringpregnancy.
Design
Clinicaldatawasobtainedthroughareviewofmedicalrecords from the hospital with the confidentiality of information beingpreserved.Theresultsoflaboratorytestswereobtained throughtheonlinehospitalsystemusingtheATHOSprogram. Theclinicalandlaboratorydatawererecordedonadata col-lectionformandlatercompiledforstatisticalanalysisofthe prevalenceofmaternalandfetalcomplications.
Statisticalanalysis
Dataarepresentedasdescriptivestatisticsincludingmeans and percentages. The Mann–Whitney non-parametric sta-tistical test was used to compare the transfused and non-transfusedgroupsasthesamplesdidnothaveaGaussian (normal)distribution.
Results
Thestudyevaluated34pregnantwomenwithSCD;24(70.5%) hadHbSS,seven(20.5%)HbSb0-thalassemiaandthree(8.8%) HbSC.Themeanagewas23.9±5.3yearsand20(59%)were followed fromthe firsttrimester ofpregnancyinthe High-riskPregnancyOutpatientServiceofthehospital,nine(25%) startedthisfollow-upinthelasttrimester,andfive(15%)did nothaveanyfollow-upinthisservice.Thecharacteristicsof thepatientsaccordingtothetypeofSCDareshowninTable1. Hb SS patients had more obstetric complications(three stillbirths,threemiscarriagesandeightpre-termlaborsand onematernaldeath)thantheother twogenotypes(S/beta0
Table2–Maternalobstetriccomplicationsduring pregnancy.
Obstetriccomplications n(%)
Previousmiscarriage 9(26.6)
Pretermlabor 8(23.5)
Pre-eclampsia 4(12.0)
Gestationaldiabetes 2(5.8)
Cesareansection 14(41.0)
Transfusioninperipartumperiod 10(29.4)
Table3–Non-obstetricmaternalcomplicationsduring pregnancy.
Non-obstetriccomplications n(%)
Vaso-occlusivecrises 21(61.7)
Acutechestsyndrome 10(29.4)
Urinarytractinfection 8(23.5)
Impairedcardiacfunction 5(14.7)
Maternaldeath 1(2.9)
ofthepatientsinallthreegroupsexperiencedcomplications relatedtoSCDduringpregnancy.
Obstetriccomplications
The patients had many obstetric complications, such as previousmiscarriage,pretermlabor,pre-eclampsia,and ges-tational diabetes (Table 2). Some patients required blood transfusionsintheperipartumperiodforclinical complica-tionssuchasacutechestsyndrome,recurrentvaso-occlusive crisesandonehadhyper-hemolyticsyndrome.
Non-obstetriccomplications
Theincidenceofsicklecellcomplicationsduringpregnancyis showninTable3.Onlyonepatientdiedtwodaysafterdelivery duetoacutechestsyndrome.
Characteristicsandcomplicationsofthenewborn
ThemaincharacteristicsofthenewbornsareshowninTable4. Thereweresevenfetallosses,includingthreestillbirthsand fourmiscarriages.
Table4–Analysisofthecharacteristicsofthenewborn infants.
Characteristic
Meangestationalage(weeks)–mean±SD 37.8±2.63 Averageweight(g)–mean±SD 2809±643.8 FirstminuteApgar<7–n(%) 11(27.5%)
Stillbirth–n(%) 3(7.7%)
Miscarriage–n(%) 4(10.2%)
SD:standarddeviation.
Theimpactoftransfusiontherapyduringpregnancywas also evaluated. The evolution of pregnancy, type of deliv-ery, fetal characteristics and maternal complications were comparedbetweentransfusedandnon-transfusedpregnant women.Approximatelyonethird(10/34)ofthepatientswere submittedtotransfusionduringpregnancyandtheresultsof thisanalysisarepresentedinTable5.
The indications fortransfusion during pregnancy were: acute chest syndrome (six patients), and repeated vaso-occlusivecrises(threepatients);onepatientwasalreadyon atransfusionprogramduetocerebralvasculopathy.
Discussion
Thisstudyshowsthatdespitethemedicaladvancesinrecent decades,pregnancyisstillassociatedwithmanyclinicaland obstetriccomplicationsinpatientswithSCD,resultingina highermaternaland infantmortalitythaninpatientswith thesicklecelltrait(Table6).Alldeaths(maternalandfetal) occurredinHbSSpatients,themostseveregenotypeofSCD. Itisknownthatpregnancyinducesanumberofphysiologic changesthataffectthehematologicindices,andpatientswith SCDmayexperienceworseningoftheanemiaandothersickle cellcomplications.9
Oxygen demandduring pregnancy increases tosupport the metabolic requirements of the placenta and fetus. As the maternaloxygen reservemay becompromised during pregnancy due to the increased oxygen consumption and decreasedfunctionalresidualcapacity,patientsmaybe pre-disposedtohypoxemia,withexacerbationofsicklingandits complications.10 These changesduringpregnancyhighlight
Table5–Comparisonofmaternal–fetalcharacteristicsbetweenpregnantwomenwithsicklecelldiseasetransfusedand non-transfusedduringpregnancy.
Non-transfused(n=24) Transfused(n=10) p-value
Medianage(years)–mean(range) 23(19–37) 22(18–32) 0.79
Pre-gestationalHb(g/dL)–mean(range) 8.45(6.6–10.0) 8.2(7.6–11.6) 1
Meangest.age(weeks) 39.6 37.5 0.87
Mean1stminuteApgarscore 7.3 7.8 0.79
Meanweightatbirth(g) 2850(1415–3063) 2710(1745–3335) 0.22
Meanweightofplacenta(g) 512.5 450.0 0.25
C.section/normaldelivery 6/15 5/6a 0.47
Miscarriage–n(%) 3(12.5) 1(10.0) 0.68
Stillbirth–n(%) 3(12.5) – 0.14
Maternaldeath–n(%) 1(2.9) – 0.25
Totaldeaths(maternalandfetal) 4/48 0/20 0.31
Table6–Comparisonofmaternal–fetalcharacteristicsbetweentwopublishedstudiesandthecurrentstudy.
Koshyetal.11 Nomuraetal.8 Currentstudy
HbSS HbSS+HbSC Sicklecelltrait HbSS+HbS/beta+HbSC
Numberofpatients 100 51 56 34
Gestationalage(weeks) 37.5 35.2 37.9 37.8
Weight<2500g(%) 41.7 62.7 17.9 25.0
Previousmiscarriage(%) 36.0 25.5 25.0 26.6
Perinataldeath(%) 7.6 11.8 1.8 7.7
Cesareansection(%) – 84.3 73.2 41.1
Pre-eclampsia(%) 18.0 21.6 14.3 12.0
Gestationaldiabetes(%) – 2.0 12.5 6.0
Maternaldeath(%) 1.7 3.9 0 2.9
theneedforamultidisciplinaryteamofexpertstomonitor pregnantsicklecellwomeninatertiaryhospital.
WhenourresultsarecomparedtoaBrazilianstudy pub-lishedin2010byNomuraetal.(Table6),thematernaldeath ratewassimilardespitedifferencesintheobstetric compli-cationrate(pre-eclampsia,gestationaldiabetesandcesarean section).8 Thelargestdifferenceoccurred intheanalysisof
fetalcharacteristicssuchasgestationalageatdelivery,weight lowerthan2500gatbirthandperinataldeath.Thegestational ageandperinataldeathrateinthisstudyweresimilartothe publicationbyKoshyetal.11
In another recently published retrospective study, the authorsanalyzed68SCDpatients.Almostallofthepatients hadatleastonesicklecellcomplicationduringpregnancy,but alowerrateofobstetriccomplications(15/68)comparedtothe currentstudy.12Inrelationtonewbornoutcomes,astudy
per-formedatauniversityhospitalintheWestIndiesanalyzed perinataloutcomessuchasadmissiontoanurseryward,birth weightlessthan2.5kg,5-minApgarscorelessthan7,cesarean sectionforfetaldistress,andperinataldeathordeathbefore dischargefromnurserywardof19newbornbabies.Atotalof 47%ofthesubjectshadadverseoutcomes.13
Theneedfortransfusionduringpregnancyforeitheracute anemiaorobstetricemergenciesiscommoninSCDpatients. Ontheotherhand,theuseofprophylactictransfusionsisstill polemic.14AccordingtoKoshyetal.,thereisnoneedfor
pro-phylactictransfusionsduringanon-complicatedpregnancy.15
Theauthorsperformedarandomizedcontrolledtrial evaluat-ingthebenefitsofprophylactictransfusionsduringpregnancy and found that maternal and fetal outcomes were simi-larinthetransfusedandnon-transfusedgroup.Subsequent retrospectivecohortstudiesevaluatingtheefficacyof prophy-lactictransfusionsalsofailedtoshowasubstantialdecrease inobstetricandfetalcomplications.16,17Conversely,
prophy-lactic erythrocytapheresis in the third trimester has been associatedwitha reductioninadverse maternaland fetus outcomes.18
Althoughnostatisticaldifferencewasobservedbetween transfusedandnon-transfusedpatients,therewerenodeaths (fetal or maternal) intransfused women, whereas in non-transfusedpatients,therewasonematernaldeathandthree stillbirths.This observationleads ustoquestion again the roleoftransfusionsinsicklecellpatientsduringpregnancy,a periodpronetoanincreaseinthepercentageofmaternaland fetalcomplications.Perhapsthecurrentstudydidnotdetect anystatisticalsignificancebetweenthetwogroupsduetothe
limitednumberofpregnantwomenanalyzed.Arandomized multicenterstudyshouldbeperformedurgentlytoevaluatea largernumberofpregnantsicklecellwomeninordertobetter elucidatethisissue.
Conclusions
Thisstudyshowsthatpregnancyisstillassociatedwithmany clinicalandobstetriccomplicationsinpatientswithSCDand sopatientsshouldbefollowedbyamultidisciplinaryteamin atertiaryhospital.
Theactual role oftransfusion during pregnancyin SCD remainstobedeterminedhoweveritseemsthatitshouldbe adoptedmoreliberally.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.SteinbergMH.Pathophysiologyofsicklecelldisease. BaillieresClinHaematol.1998;11(1):163–84.
2.BallasSK.Sicklecelldisease:clinicalmanagement.Baillieres ClinHaematol.1998;11(1):185–214.
3.PowarsDR,SandhuM,Niland-WeissJ,JohnsonC,BruceS, ManningPR.Pregnancyinsicklecelldisease.ObstetGynecol. 1986;67(2):217–28.
4.Platt1OS,BrambillaDJ,RosseWF,MilnerPF,CastroO, SteinbergMH,etal.Mortalityinsicklecelldisease.Life expectancyandriskfactorsforearlydeath.NEnglJMed. 1994;330(23):1639–44.
5.HoyertDL.Maternalmortalityandrelatedconcepts.Vital HealthStat.2007;3(33):1–13.
6.RogersDT1,MolokieR,MolokieR.Sicklecelldiseasein pregnancy.ObstetGynecolClinNorthAm.2010;37(2):223–37.
7.KoshyM,BurdL.Managementofpregnancyinsicklecell syndromes.HematolOncolClinNorthAm.1991;5(3):585–96.
8.NomuraRM,IgaiAM,TostaK,daFonsecaGH,GualandroSF, ZugaibM.Maternalandperinataloutcomesinpregnancies complicatedbysicklecelldiseases.RevBrasGinecolObstet. 2010;32(8):405–11.
9.TownsleyDM.Hematologiccomplicationsofpregnancy. SeminHematol.2013;50:222–31.
11.KoshyM,ChisumD,BurdL,OrlinaA,HowH.Managementof sicklecellanemiaandpregnancy.JClinApher.1991;6(4): 230–3.
12.Al-FarsiSH,Al-RiyamiNM,Al-KhaboriMK,Al-HunainiMN. Maternalcomplicationsandtheassociationwithbaseline variablesinpregnantwomenwithsicklecelldisease. Hemoglobin.2013;37(3):219–26.
13.PeppleDJ,MullingsAM,ReidHL.Maternalbloodviscosityand perinataloutcomeinsteady-statehomozygoussicklecell disease.NigerJPhysiolSci.2013;28(1):69–71.
14.NaikRP,LanzkronS.Babyonboard:whatyouneedtoknow aboutpregnancyinthehemoglobinopathies.HematolAm SocHematolEducProgram.2012;2012:208–14.
15.KoshyM,BurdL,WallaceD,MoawadA,BaronJ.Prophylactic red-celltransfusionsinpregnantpatientswithsicklecell
disease.Arandomizedcooperativestudy.NEnglJMed. 1988;319(22):1447–52.
16.HowardRJ,TuckSM,PearsonTC.Pregnancyinsicklecell diseaseintheUK:resultsofamulticentresurveyofthe effectofprophylacticbloodtransfusiononmaternaland fetaloutcome.BrJObstetGynaecol.1995;102(12): 947–51.
17.GrossettiE,CarlesG,ElGuindiW,SeveB,MontoyaY, CreveuilC,etal.Selectiveprophylactictransfusioninsickle celldisease.ActaObstetGynecolScand.2009;88(10): 1090–4.