www.jped.com.br
ORIGINAL
ARTICLE
Prevalence
of
myocarditis
in
pediatric
intensive
care
unit
cases
presenting
with
other
system
involvement
夽
,
夽夽
Hanaa
Ibrahim
Rady
∗,
Hanan
Zekri
∗DepartmentofPediatrics,FacultyofMedicine,CairoUniversity,Cairo,Egypt
Received5December2013;accepted28May2014 Availableonline27September2014
KEYWORDS
Myocarditis; Cardiacenzymes; Troponin; Children;
Pediatricintensive careunit
Abstract
Objective: Toassesschildrenwithmyocarditis,thefrequencyofvariouspresentingsymptoms, andtheaccuracyofdifferentinvestigationsinthediagnosis.
Methods: Thiswasanobservationalstudyof63patientsadmittedtoPICUwithnon-cardiac diag-nosis.Cardiacenzymes,chest-Xray,echocardiography,andelectrocardiogramwereperformed todiagnosemyocarditisamongthosepatients.
Results: Therewere 16cases ofdefinite myocarditis.The agedistributionwas non-normal, withmedianof5.5months(3.25---21).Ofthe16patientswhowerediagnosedwithmyocarditis, 62.5%wereoriginallydiagnosedashavingrespiratoryproblems,andthereweremorefemales thanmales.Amongthepresentcases,theaccuracy ofcardiacenzymes(cardiac troponinT [cTn]andcreatinephosphokinaseMB[CKMB])inthediagnosisofmyocarditiswasonly63.5%, whiletheaccuracyoflowfractionalshorteningandofchest-Xraycardiomegalywas85.7and 80.9%;respectively.Cardiactroponinfolds2.02hadpositivepredictivevalueof100%,negative predictivevalueof88.7%,specificityof100%,sensitivityof62.5%,andaccuracyof90.5%.
Conclusions: Childrenwithmyocarditispresentwithsymptomsthatcanbemistakenforother typesofillnesses.Whenclinicalsuspicionofmyocarditisexists,chest-Xrayand echocardiogra-phyaresufficientasscreeningtests.Cardiactroponinsconfirmthediagnosisinscreenedcases, withspecificityof100%.
©2013SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Allrightsreserved.
夽 Pleasecitethisarticleas:RadyHI,ZekriH.Prevalenceofmyocarditisinpediatricintensivecareunitcasespresentingwithothersystem
involvement.JPediatr(RioJ).2015;91:93---7.
夽夽ThestudywasconductedonPICU,NewChildren’sHospital,CairoUniversity,Cairo,Egypt.
∗Correspondingauthors.
E-mail:hanaaarady@gmail.com(H.I.Rady),drksadek@yahoo.com(H.Zekri).
http://dx.doi.org/10.1016/j.jped.2014.05.011
PALAVRAS-CHAVE
Miocardite; Enzimascardíacas; Troponina; Crianc¸as;
Unidadedeterapia intensivapediátrica
Prevalênciademiocarditeemcasospediátricosnaunidadedeterapiaintensiva,com
envolvimentodeoutrossistemas
Resumo
Objetivo: Determinarascrianc¸ascommiocardite,afrequênciadeváriossintomasapresentados eaprecisãodediferentesinvestigac¸õesnodiagnóstico.
Métodos: Estudo observacional de 63 pacientes internados na UTIP com diagnóstico de problemas não cardíacos. Os exames de enzimas cardíacas, raio-X do tórax, ecocardio-grama e eletrocardiograma (ECG) foram realizados para diagnosticar miocardite dentre os pacientes.
Resultados: Houve16casosdemiocarditedefinida.Adistribuic¸ãoetárianãofoinormal,com médiade5,5meses(3,25-21).Dos16pacientesdiagnosticadoscommiocardite,62,5%foram originalmente diagnosticados como comproblemasrespiratórios, e amulheres estavam em maiornúmeroqueoshomens.Dentrenossoscasos,aprecisãodasenzimascardíacas(cTne CKMB)nodiagnósticodamiocarditefoideapenas63,5%,apesardeaprecisãodabaixafrac¸ãode encurtamento(FS)edoraio-Xdetóraxrevelandocardiomegaliatersido85,7%e80,9%; respec-tivamente.ATroponinaCardíacaem2,02vezesapresentouvalorpreditivopositivo=100%,valor preditivonegativo=88,7%,especificidade=100%,sensibilidade=62,5%eprecisão=90,5%.
Conclusões: Ascrianc¸ascommiocarditeapresentamsintomasquepodemserconfundidoscom outrostiposdedoenc¸as.Quandohásuspeitaclínicademiocardite,raio-Xdetóraxe ecocardio-grafiasãotestesderastreamentosuficientes.AsTroponinasCardíacasconfirmamodiagnóstico emcasosexaminados,comespecificidadede100%.
©2013SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Todososdireitos reservados.
Introduction
Myocarditisisaninflammatoryconditionofthemyocardium characterized by leukocyte infiltration and subsequent fibrosis and necrosis.1---4 However, because children with myocarditis may be asymptomatic, the true incidence is unknown,5---7withanestimateofaround0.05%.8---10
It is a potentially life-threatening condition,9 caus-ing significant morbidity and mortality with long-term sequelae, including congestive heart failure (CHF) and cardiomyopathy.4,9Sincethemortalityratesforinfantsand children withmyocarditis may be ashigh as75 and 25%, respectively, and early initiation of therapy is potentially beneficial,promptdiagnosisisimperative.11,12
Myocarditis in children is a challenging diagnosis to make.10 They have awide rangeofnon-specific signsand symptoms,overlapping withmore commondisorderssuch as respiratory distress and gastrointestinal disease.10,13,14 Mostcases of myocarditis are preceded by a viralor flu-likeillness,15 butbacteria,fungi,protozoa,parasites,and rickettsiaearealsocausativeagents.16Theuseofavariety ofinvasiveandnon-invasivemethodsisusuallymandatory, mainlybasedonhistoryandclinicalfeatures.17Itisclearly importantto have a high degree of suspicionto diagnose myocarditis.18
Historically,thegoldstandardforthediagnosisofacute myocarditis required an endomyocardial biopsy according totheDallascriteria.19,20Morerecentlyancillarydiagnostic modalitieshavebeenusedtohelpmakethediagnosisless invasiveandmorerapid.Theuseoflaboratorytesting (car-diactroponinT,I[cTnTandcTnI,respectively]andcreatine phosphokinaseMB[CKMB]),echocardiography,andcardiac
magnetic resonanceimaging(MRI)can makethediagnosis intheabsenceofinvasivebiopsy.21
High-doseintravenousimmunoglobulinhasbeen proven toimprovetherecoveryoftheleftventricularfunction,with atendencytopresentbettersurvivalrateinacute myocardi-tis.Consideringthecostofthisregimen,theaccuracyofthe diagnosisis essential,especiallyindevelopingcountriesin whichthehighcostofhealthcareisaconcern.20
This study aimed to determine the prevalence of myocarditis in association with other systems involved in critically illcases andtotest the use of cardiacenzymes (cTnT,cTnI,andCKMB),chestX-ray(CXR),and echocardio-gramforscreeningofthosecases.
Methods
Thiswasanobservationalstudy,inwhichallchildren admit-tedtoCairouniversityHospitalPediatricIntensiveCareUnit (PICU)wereenrolledbasedonthefollowinginclusion crite-ria:
• Allpatientspresentingwithrespiratorydistress;
• Symptomsandsignsofheartfailure;
• Anyinfectiouslesions,eitherfocalorsepticemia;
• Multipleorgansystemfailure.
Theexclusioncriteriawerechildrenwithknowncardiac lesions,eithercongenitaloracquired,andpresentingwith heartfailure.
respiratorydistressandneed forrespiratorysupport (oxy-genormechanicalventilation[MV]);assessmentofcardiac decompensation and need for cardiac support (inotropes or antifailure drugs); routine laboratorial exams (com-plete blood count, erythrocyte sedimentation rate (ESR), C-reactiveprotein(CRP),cultures);CXR;cardiacenzymes: TroponinT,Troponin I,andCKMB; electrocardiogram;and detailedechocardiographicexaminationincludingM-mode, 2-dimensional, and Dopplerechocardiography (echo) with color-codingcharacter.
ExaminationswereperformedusingaPhilipsequipment withan 8MHztransducer.The followingstandardwindows wereused:
1. Subxiphoid 2. Apical
3. Longandshortparasternal 4. Longandshortsuprasternal.
Measurementofcardiacdimensions:
TheM-modeechocardiographictracingsderivedfromthe two-dimensionalechocardiographywereused.It is gener-atedfromtheparasternallongaxisview.TheM-modecursor linewaspositionedperpendiculartothemajoraxisofthe left ventricle at the level of the posterior mitral valve leaflet.
The calculation ofthe fractionalshortening(FS%) from thedataobtainedfromM-modemeasurementfollowedthe equation:
FS%=
LVIDd− LVIDs
LVIDd
×100
LVIDd,internaldimensionofthediastolicLV(leftventricle). LVIDs,internaldimensionofthesystolicLV.22
Children with suspected cardiac affection (myocardi-tis) by cardiac enzymes, echocardiography, or ECG were treatedwithintravenousimmunoglobulin2mg/kgover48h, inaccordancewiththeusualprotocolofthisPICU.
Patientswerecategorizedashavingprobablemyocarditis (diagnosismadebyapediatriccardiologistbasedonmedical history, physical examination, and investigation results in theabsenceofanendomyocardialbiopsyornomyocarditis). Theinvestigationsconsideredwere:
• ECGcriteriaofsinustachycardiadisproportionatetothe feverorageofthepatient.
• Cardiomegalyinchestradiograph.
• Dilated leftventricleor both ventriclesduring echocar-diography associated withimpaired systolic or diastolic functionandassociatedmitralvalveregurgitation(MR). • Cardiacenzymesmostlycardiactroponinselevatedmore
than2.02foldsofthenormalleveloftheenzyme.
Echocardiographicfindings(fractionalshortening)or ele-vatedcardiacenzymeswereconsideredasthemostreliable keysfordiagnosisofmyocarditis.
Theoutcomewasevaluatedby:
• LengthofPICUstay, • Survivaltodischarge, • Follow-upecho.
This study was approved by Cairo University Ethics Committee, and was conducted in accordance with the guidelinesforhumanresearch.
Statisticalanalysis
Nominaldatawereexpressedasfrequencyandpercentage andwerecomparedusingchi-squaredtest.Numericaldata wereexpressedasmedianandrange(25th---75th),andwere comparedusingStudent’st-test.Non-parametricdatawere comparedusingtheMann---Whitneytest.Pearson’s correla-tionswereusedtoexploreassociationsbetweennumerical variables. A p-value <0.05 was considered asstatistically significant.
Results
This studycomprised 63 critically-illchildren admitted to thePICU,followingtheinclusionandexclusioncriteria.
Regarding theiradmission diagnosis,they weredivided into respiratory infections (41 cases), encephalitis (12 cases), and others (ten cases; diabetic ketoacidosis, enterocolitis, Guillain-Barré syndrome, septicemia, and multisystemorganfailure).
Sixteen(25.3%)ofthemwerediagnosedwith myocardi-tis.Amongthose,62.5%(10/16)hadrespiratoryinfectionsas thediagnosisatadmission,12.5%(2/16)hadencephalitisas thediagnosis atadmission,and25%(4/16)hadeither dia-beticketoacidosis,enterocolitis,Guillain-Barrésyndrome, septicemia,ormultisystemorganfailureasthediagnosisat admission.
Althoughtherewasdifferenceinthenumberoffemales (62.5%)versusmales(37.5%)withmyocarditis,this differ-encewasstatisticallyinsignificant(p=0.126).The median age for those diagnosed myocarditis was 5.5 months (3.25---21),andforthosewithnegativemyocarditismedian was9months(4---17;p=0.618).
Asignificantassociationwasobservedbetweenpatients withmyocarditisandthefollowinginvestigations:CXR car-diomegaly,lowFS,andelevatedcardiacenzymes(Table1). Amongthecases,theaccuracyofcardiacenzymes(cTnand CKMB)inthediagnosisofmyocarditiswasonly63.5%,while theaccuracyof lowFSandofCXR cardiomegalywas85.7 and80.9%,respectively.
Fig.1 presentsthe ROCcurve of elevated cardiac tro-poninvaluesrepresentedinfoldsofincrease.Becausenot allpatients hadthe cTn levelmeasured at the same lab-oratory,weconsidered thecTnasfoldsofincrease rather thanabsolutevalueinordertocomparethem,dueto ref-erence ranges variability between different laboratories. TheAreaunderthecurve(AUC)was0.936(95%CI:0.85---1,
p=0.0001).Cardiactroponinfolds2.02hadapositive pre-dictive value (PPV) of 100%, negativepredictive value of negative(NPV)of 88.7%,specificityof 100%,sensitivityof 62.5%,andaccuracyof90.5%.
NegativeCRPwasmoreoftenfoundinpatientsdiagnosed asmyocarditis(62.5%;p=0.955).Fiftypercentofpatients diagnosedmyocarditishadbandemia(p=0.412).
Table1 Relationbetweendifferentinvestigationsandmyocarditis.
Myocarditis p-value RR/OR(95%CI)
Yes No
CXRshowingcardiomegaly 9 5 0.001 10.8(2.8---41.8)
LowFS 12 5 0.0001 25(5.8---108.8)
ECG(sinustachycardia/arrhythmias) 16 0 0.317
Elevatedcardiacenzymes 16 23 0.001 0.59(0.45---0.76)
RR,relativerisk;OR,oddsratio;CI,confidenceinterval;CXR,chest-Xray;FS,fractionalshortening;ECG,electrocardiogram.
Table2 Relationbetweengivensupport,lengthofstay,outcome,andmyocarditis.
Myocarditis Yes(n=16)
Myocarditis No(n=47)
p-value OR(95%CI)
Inotropicsupport(n=25) 11(68.8%) 14(29.8%) 0.006 5.1(1.5---17.7)
Mechanicalventilation(n=31) 13(81.2%) 18(38.3%) 0.003 6.9(1.7---27.9)
LOSdays 9 6 0.277
Death 8(50%) 14(29.8) 0.143
OR,oddsratio;LOS,lengthofstay.
1.0
0.8
0.6
0.4
0.2
0.0
0.0 0.2 0.4 0.6 0.8 1.0
1 - specificity
Diagonal segments are produced by ties ROC curve
Sensitivity
Figure 1 Showing ROC curve of cardiac troponin-folds,
p=0.001.
withmyocarditis had almost five times increasedodds of MRwhencomparedwithnon-myocarditispatients.
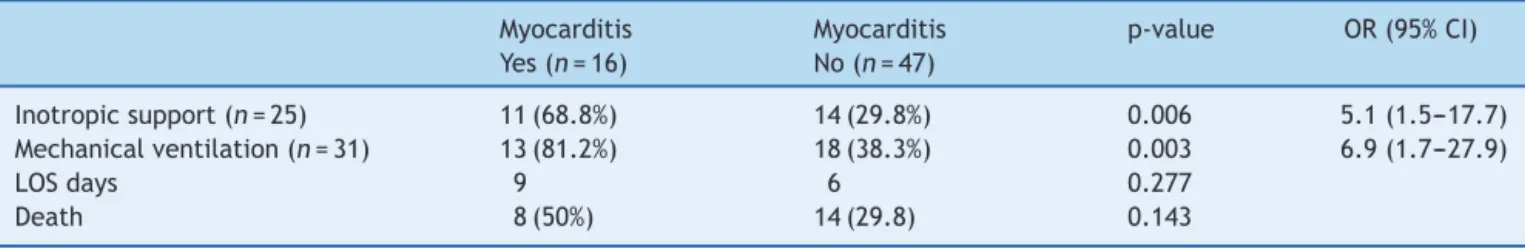
Patientswithmyocarditishadalmostfive-foldincreased odds of inotropic support, and seven-fold increased odds of MV when compared with patients withno myocarditis (Table2).
Median hospitalization of those diagnosed myocarditis wasninedays (3.24---14.5)compared to6 days(5---10) for thosewithnegativemyocarditis,p=0.277.
There was no significant difference regarding survival to discharge between those diagnosed myocarditis (eight
cases,50%)andthosewithnegativemyocarditis(33cases, 70.2%;p=0.143;Table2).
Discussion
While pediatricmyocarditis presentswithsignificant mor-bidity and mortality, data onthe prevalence are limited, andthediagnosisremainschallenging.10
Thisstudyprovidesanalysisofchildrenadmittedtothe PICU ofCairo University andwhen screenedthrough CXR, echo, ECG, and cardiac enzymes (cTn and CKMB) it was found that the prevalence ofmyocarditis was25.3%. In a
post-mortemstudyof childrenwhodiedwithout ahistory suggestive of myocarditis, researchers found evidence of activeorhealedmyocarditisin17of138cases(12.3%).3
Fromthosediagnosedasprobablemyocarditis,62.5%had admission presentation relatedto the respiratory system. Freedmanetal.foundthat32%oftheircasespresentedwith respiratorysymptoms.12Thepresentfindingsshouldremind clinicians that pulmonary complaintsmay be commonfor childrenwithmyocardialdysfunction,whereascardiac find-ingsmaybeminimal.23Inflammationplaysanimportantrole incardiacdysfunctionunderdifferentsituations.Acute sys-temicinflammationoccurringinpatientswithsevereburns, trauma,andinflammatorydiseasescausescardiac dysfunc-tion, which is one of the leading causes of mortality in thesepatients.Acutesepsisdecreasescardiaccontractility andimpairsmyocardialcompliance.24Althoughbothusually haveaviralcause,acutemyocarditisandacutepericarditis arenotalways associated(inthe samewaythat meningi-tisandencephalitisdonotalwaysoccurtogether),andthe clinicalemphasisisusuallyononeortheother.25
Themedianageofthepresentmyocarditiscaseswas5.5 months(3.25---21),withinsignificantdifferencecomparedto non-myocarditispatients.Soongswangetal.detectedacute myocarditisamongpatientswithmeanage5.4±5.1years,
Amongtheexaminationsperformed,itwasobservedthat echo(lowFS)andCXRhadanaccuracyof85.7and80.9%, respectively;hence,theycanbeusedasscreeningfor sus-pectedmyocarditiscases.
Cardiac enzymescTn-foldsofincreasemorethan 2.02, hadahighspecificity100%,butalowsensitivity,of62.5%. SimilarresultswerefoundinthestudyperformedbyBohn andBenson.14AnotherstudyfoundthatacTnTcutoffpoint of0.052ng/mlhadasensitivityof71%andspecificityof86% fordiagnosisofmyocarditis,withafalsenegativecTnTrate of44%.19
In general, cardiac enzymesareelevated in myocardi-tis, but their reliability to detect myocarditis has been repeatedlyquestioned.SerumlevelsofcTnaremore sensi-tivein patients withclinicallysuspectedmyocarditis than conventional determination of CKMB levels, and indicate myocyte injury. Cardiac troponin was mainly elevated in patientswithacute,early-onsetmyocarditis, whereasthe absenceofincreasedlevelssuggestsalong-termpresence ofmyocarditis.26 Thusthedifferenceinthepresentresults comparedtootherscanbeduetothetimingofbloodsample collection.
Regarding the support offered to myocarditis cases, 81.2%required MV, while,in thestudy byKlugman etal., only37.5% requiredMV.10 Moreover,inotropicsupportwas offeredto68.8%ofthepresentmyocarditiscases,compared toaround35%inKlugmanetal.’sstudy.10
The mortality rate among myocarditis cases was high (50%).Previousreportsrangedfrom13to38%.19,27
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Batra AS, Lewis AB. Acute myocarditis. Curr Opin Pediatr. 2001;13:234---9.
2.Corrado D, Basso C, Thiene G. Sudden cardiac death in youngpeople withapparentlynormal heart.Cardiovasc Res. 2001;50:399---408.
3.Feldman AM, McNamara D. Myocarditis. N Engl J Med. 2000;343:1388---98.
4.McCarthy3rdRE,BoehmerJP,HrubanRH,HutchinsGM,Kasper EK,HareJM,etal.Long-termoutcomeoffulminantmyocarditis ascomparedwithacute(nonfulminant)myocarditis.NEnglJ Med.2000;342:690---5.
5.Amabile N, Fraisse A, Bouvenot J, Chetaille P, Ovaert C. Outcome ofacute fulminant myocarditis in children. Heart. 2006;92:1269---73.
6.English RF, Janosky JE, Ettedgui JA, Webber SA. Out-comes for children with acute myocarditis. Cardiol Young. 2004;14:488---93.
7.KühnB,ShapiroED,WallsTA,FriedmanAH.Predictorsof out-comeofmyocarditis.PediatrCardiol.2004;25:379---84.
8.LipshultzSE,SleeperLA,TowbinJA,LoweAM,OravEJ,CoxGF, etal.Theincidenceofpediatriccardiomyopathyintworegions oftheUnitedStates.NEnglJMed.2003;348:1647---55.
9.TowbinJA,LoweAM,ColanSD,SleeperLA,OravEJ,ClunieS, etal.Incidence,causes,andoutcomesofdilated cardiomyopa-thyinchildren.JAMA.2006;296:1867---76.
10.KlugmanD,BergerJT,SableCA,HeJ,KhandelwalSG,Slonim AD.Pediatricpatientshospitalizedwithmyocarditis:a multi-institutionalanalysis.PediatrCardiol.2010;31:222---8.
11.DanceaAB.Myocarditisininfantsandchildren:areviewforthe paediatrician.PaediatrChildHealth.2001;6:543---5.
12.Freedman SB, Haladyn JK, Floh A, Kirsh JA, Taylor G, Thull-Freedman J. Pediatricmyocarditis: emergency depart-ment clinical findings and diagnostic evaluation. Pediatrics. 2007;120:1278---85.
13.ChangYJ,ChaoHC,HsiaSH,YanDC.Myocarditispresentingas gastritisinchildren.PediatrEmergCare.2006;22:439---40.
14.Bohn D, Benson L. Diagnosis and management of pediatric myocarditis.PaediatrDrugs.2002;4:171---81.
15.CalabreseF,RigoE,MilanesiO,BoffaGM,AngeliniA,ValenteM, etal.Moleculardiagnosisofmyocarditisanddilated cardiomy-opathyinchildren: clinicopathologicfeatures and prognostic implications.DiagnMolPathol.2002;11:212---21.
16.BaboonianC,McKennaW.Eradicationofviralmyocarditis:is therehope?JAmCollCardiol.2003;42:473---6.
17.Al-Biltagi M,IssaM, HagarHA, Abdel-HafezM,AzizNA. Cir-culating cardiac troponins levels and cardiac dysfunction in childrenwithacuteandfulminantviralmyocarditis.Acta Pae-diatr.2010;99:1510---6.
18.ChecchiaPA,KulikTJ.Acuteviralmyocarditis:diagnosis. Pedi-atrCritCareMed.2006;7:S8---11.
19.SoongswangJ,DurongpisitkulK,NanaA,LaohaprasittipornD, KangkagateC,PunleeK,etal.CardiactroponinT:amarkerin thediagnosisofacutemyocarditisinchildren.PediatrCardiol. 2005;26:45---9.
20.SoongswangJ,DurongpisitkulK,RatanarapeeS,LeowattanaW, NanaA,LaohaprasitipornD,etal.CardiactroponinT:itsrole inthediagnosisofclinicallysuspectedacutemyocarditisand chronic dilated cardiomyopathy inchildren. Pediatr Cardiol. 2002;23:531---5.
21.LevineMC,KlugmanD,TeachSJ.Updateonmyocarditisin chil-dren.CurrOpinPediatr.2010;22:278---83.
22.Schiller NB, Shah PM,Crawford M, DeMaria A, Devereux R, FeigenbaumH,etal.Recommendationsforquantitationofthe leftventriclebytwo-dimensionalechocardiography.American SocietyofEchocardiographyCommitteeonStandards, Subcom-mitteeonQuantitationofTwo-DimensionalEchocardiograms.J AmSocEchocardiogr.1989;2:358---67.
23.Alpern ER, Stevens MW. An offbeat wheezer. Pediatr Ann. 2000;29:97---101.
24.LiY,GeS,PengY,ChenX.Inflammationandcardiac dysfunc-tionduringsepsis, musculardystrophy,andmyocarditis.Burn Trauma.2013;1:109---21.
25.OakleyCM.Myocarditis,pericarditisandotherpericardial dis-eases.Heart.2000;84:449---54.
26.DennertR,CrijnsHJ,HeymansS.Acuteviralmyocarditis.Eur HeartJ.2008;29:2073---82.