www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
The
learning
progression
of
diagnostic
sialendoscopy
夽
,
夽夽
José
Higino
Steck
a,∗,
Elaine
Stabenow
a,
Erivelto
Martinho
Volpi
b,
Evandro
Cezar
Guerreiro
Vasconcelos
aaCirurgiadeCabec¸aePescoc¸o,ClínicaONCCAPE,Campinas,SP,Brazil
bServic¸odeCirurgiadeCabec¸aePescoc¸odoHospitaldasClínicasdaFaculdadedeMedicinadaUniversidadedeSãoPaulo
(HCFM-USP),SãoPaulo,SP,Brazil
Received17September2014;accepted21February2015 Availableonline6November2015
KEYWORDS
Salivarygland diseases; Endoscopy; Diagnosis
Abstract
Introduction:Sialendoscopyisbecomingthegoldstandardprocedurefordiagnosisand
treat-mentofSalivaryGlandInflammatoryDiseases.
Objective:Toevaluatethelearningprogressionofasinglesurgeontoimplementandperform
diagnosticsialendoscopy:toestimatehowmanyprocedureswerenecessarytoachievebetter results;ifitwashigherrateofcomplicationsinthebeginning.
Methods:Retrospective analysis involving 113 consecutive sialendoscopies performed from
2010to2013. Accordingtoadescriptiveanalysisofthefactorsrelated tosurgeon’s experi-ence,thecasuisticwasdividedintotwogroups:group(A)comprisingthefirst50exams,and group(B)thelast63.Groupswerethencomparedconcerningdemographicandperi-operative aspects.
Results:InGroupA,failuretocatheterizepapillawere22%versus3%inB(p=0.001).Failure
tocompleteexaminationwas30%ingroupAversus6%inB(p=0.001),andnecessitytorepeat examswas22%ingroupAversus10%inB(p=0.058).Thecomplicationrateswere18%ingroup A,and10%inB(p=0.149).OperativetimewasslightlyshorteringroupB(56versus41min,
p=0.045).
Conclusion:Wefound betteroutcomesafterthefirst 50diagnosticsialendoscopies.
Compli-cation rateswere statistically the same between earlyandlate groups ofexperience with sialendoscopy.
© 2015 Associac¸ão Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial. Published by Elsevier Editora Ltda. This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/).
夽
Pleasecitethisarticleas:SteckJH,StabenowE,VolpiEM,VasconcelosECG.Thelearningprogressionofdiagnosticsialendoscopy.Braz JOtorhinolaryngol.2016;82:170---6.
夽夽Institution:ONCCAPE---Clinic---HeadandNeckSurgeryService. ∗Correspondingauthor.
E-mail:higinosteck@gmail.com(J.H.Steck). http://dx.doi.org/10.1016/j.bjorl.2015.10.007
PALAVRAS-CHAVE
Doenc¸asdaglândula salivar;
Endoscopia; Diagnóstico
Progressãodoaprendizadodasialoendoscopiadiagnóstica
Resumo
Introduc¸ão: Asialoendoscopiavemsetornandooprocedimentodereferênciaparaodiagnóstico
eotratamentodasdoenc¸asinflamatóriasdaglândulasalivar.
Objetivo: Avaliaraprogressãodeaprendizadodeummesmocirurgiãoparaimplementac¸ãoe
realizac¸ãodasialoendoscopiadiagnóstica:verificarquantosprocedimentosforamnecessários paraaobtenc¸ãoderesultadosmelhoresesehouveocorrênciademaiortaxadecomplicac¸ões noiníciodoaprendizado.
Método: Análise retrospectiva envolvendo 113 sialoendoscopias consecutivas realizadas de
2010 a2013. Deacordocom umaanálise descritivados fatoresrelacionados àexperiência docirurgião,acasuísticafoidivididaemdoisgrupos:grupo(A),compreendendoosprimeiros 50exames;egrupo(B),osúltimos63.Emseguida,osgruposforamcomparados,levandoem considerac¸ãoosaspectosdemográficoseperioperatórios.
Resultados: No grupo A, a não realizac¸ão do cateterismo papilar foi de 22% vs. 3% em B
(p=0,001).Anãorealizac¸ãodeumexamecompletofoide30%nogrupoAvs.6%emB(p=0,001), eanecessidadederepetiroexamefoide22%nogrupoAvs.10%emB(p=0,058).Os percentu-ais de complicac¸ões foram18%no grupoA e 10%em B (p=0,149).Otempo operatóriofoi ligeiramentemenornogrupoB(56vs.41minutos,p=0,045).
Conclusão:Verificamosmelhoresdesfechosapósas50primeirassialoendoscopiasdiagnósticas.
Ospercentuaisdecomplicac¸õesforamestatisticamentesemelhantesentreosgruposiniciale avanc¸adodeexperiênciacomasialoendoscopia.
© 2015 Associac¸ão Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial. Publi-cado por Elsevier Editora Ltda. Este é um artigo Open Access sob a licença CC BY (https://creativecommons.org/licenses/by/4.0/deed.pt).
Introduction
Inthelast15 yearsthegold standardin thetreatmentof Salivary Gland Inflammatory Diseases (SGID) moved from open surgical resection to endoscopic treatment, with the obvious gain of avoiding complications from parotid and submandibular surgery, like scars and nerve injury, andpreservingsalivaryfunction.1,2Sialendoscopywasfirst
describedforthetreatmentofsialolithiasis.3,4 Rapidlythe
techniquegained spacein thediagnosis and treatmentof other SGID, like Radioiodine sialadenitis,Sjogrens disease and Juvenile recurrent parotiditis.5 However, the use of
verydelicateinstrumentsinverysmallanddelicate struc-turesasthesalivarypapillae andductsproved tobevery challenging.6 In2006,Marchaletal.7wereworking yetto
improve the sialendoscopy technique to enter the small branchesofthesalivaryducts.
Asthebenefitsofthesialendoscopyinregardtotheopen surgeries became evident,1,2 some training centers were
established, as the European Sialendoscopy Training Cen-ter,createdin2002byFrancisMarchal.1Despiteagrowing
experience about this procedure, some important doubts remain,suchaswhetherthecomplicationrateishigherat thebeginningofthelearningcurveandhowmanycasesare necessaryforasurgeontoperformasafesialendoscopy.8,9
Thus,theobjectiveofthispaperistoreviewandevaluate thelearning progressionofa singlesurgeontoimplement and performdiagnostic sialendoscopyin both parotid and submandibularglands,inordertoestimatehowmany pro-cedureswerenecessarytoachievegoodresultsandifthe rateofcomplicationswashigherinthebeginning.
Methods
Thisisaretrospective,transversal,consecutive-casesstudy. ItwasapprovedbytheInstitutionalReviewBoard(CO003), andallpatientsgavetheirinformedconsentpriortotheir inclusioninthestudy.
Allpatientssubmittedtosialendoscopyperformedbythe samesurgeonfromSeptember 2010toJanuary2013were included.Parotidorsubmandibularexamswereallincluded. Therewasnoexclusioncriterion.Accordingly,thecasuistic comprises113sialendoscopiesconcerning65patients(62% females)withameanageof46years(rangingfrom4to83). Concerningtheexaminedglands,45%wereparotidand55% submandibularglands.
Thesurgeonhadaninitialhands-ontrainingonfreshpig headspecimensattheESTC---EuropeanSialendoscopy Train-ingCentre,Geneva,Switzerland.
All patients initially undergone a diagnostic sialendo-scopy.
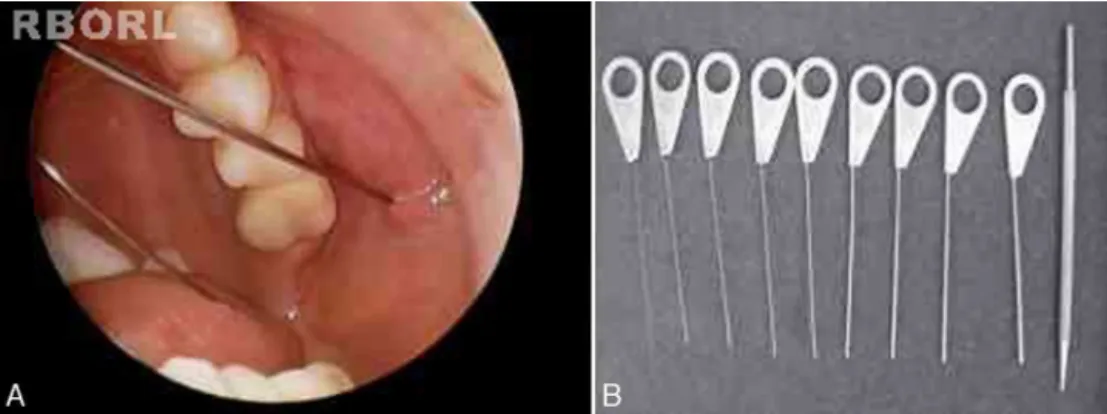
Patients were placed in supine or semi-seated posi-tion,underlocalorgeneralanesthesia.WeutilizedMarchal diagnostic and interventional miniature endoscopes (Karl StorzTM)withanexternaldiameter1.1or1.3mm,amicro
cameraandvideosystem.
Figure1 Papillacatheterizationofaleftparotidgland(A)andprobesutilizedtoperformpapilladilation(B).
Figure2 Sialendoscopicviewofastoneanditsremovalwith minibasketcatheter.
ductal stenosis, salivary stones, chronic sialadenitis signs (palemucosa,stenosisandplugsofmucus),acute sialadeni-tissigns(friableandreddish mucosawithpus)andductal plugsofmucusduetostasisofsalivaflow.
In some cases, treatment was performed in the same procedure,accordingtotheendoscopicfinding, likestone removalbybasket(Fig.2),fragmentationbylaserlithotripsy or both. Stenosis was treated with endoscopic dilation. Intraductalinstillationof100mgofhydrocortisonewas sys-tematicallydoneattheendoftheallprocedures.
Postoperativecare followeda FastTrackRehabilitation routineincluding opioids free analgesia, immediate post-operativefeedingandambulation.Allsialendoscopieswere executedinanoutpatientfashion.
In orderto estimate how many procedures were nec-essary to achieve good results, an initial analysis of surgeon-relatedoutcomeswasperformedbasedonmedical chartreview.Wesearchedcaracteristicsthatallowed divid-ingthecasuisticinearly andlategroups ofsialendoscopy experience.
Demographic and the following perioperative aspects were analyzed: (1) the duration time of sialendoscopies in minutes;(2) failure in papillacatheterization; (3) fail-uretocompletetheendoscopicexamination;(4)necessity to repeat sialendoscopy in the same patient; (5) failure toachievetherapeuticgoal;(6)perioperativecomplication rates.
Papillawasconsideredsuccessfullycatheterizedwhenit waspossible tofinditand introduceat leastone dilation probeinside.
Examinationwasconsideredsuccessfulwhenitachieved progression of the endoscope (external diameter 1.1 or 1.3mm) toat least one ramification of the main duct or untildiseasewasfound.
Treatmentwasconsideredsuccessfulwhenthe therapeu-ticgoalwasachieved,asstoneremovalorstenosisdilation.
Howgroupsweredefined
Visualanalysisofgraphicallydisplayeddatasuggestedthat surgeon-relatedoutcomesimprovedaroundthe50th sialen-doscopy.
Papillacatheterizationwasstronglyrelatedtosurgeon’s experienceandwasanimportantstepbecausethe diagnos-ticprocedureispossibleonlyifitisachieved.
The50thsialendoscopy(Fig.3)wasthelastoneofthe sequence when failure to achieve papilla catheterization wasfrequent(22%).
Afterthe50thsialendoscopy,onlyintwoprocedures(3%) papillacatheterizationwasnotachieved(Fig.3).Theywere performedinbilateralparotidglandsofa28year-oldwoman whoreceivedradioiodinetherapyforpapillarythyroid carci-noma.Therewasahugepapillastenosissuggestinganatomic difficultiesmorethananinexperiencedsurgeon.
Basedonthesefindings,twogroupsweredefined:early group(A)ofthesialendoscopysurgeon’sexperience, com-prisingthefirst50exams,andlategroup(B)withthelast 63sialendoscopies.
Statistics
StatisticalanalysiswasundertakenusingtheSPSSsoftware, version19.0(SPSS,Chicago,IL).
Papilla catheterization
Not achieved
Achieved
Sequence of sialoendoscopies
1 5 9 13 17 21 25 29 33 37 41 45 49 53 57 61 65 69 73 77 81 85 89 93 97 101 105 109 113
Figure3 Sequencechartof113consecutivesialendoscopies.Blackpointsatlowerhorizontalpositionrepresentproceduresin whichpapillacatheterizationwasachieved,whilethoseatupperpositionrepresentfailuretoachieveit.Verticaldashedlinemarks the50thprocedure.
0 1 2
Mild Moderate Strong
3 4 5 6 7 8 9 10
Figure 4 Visual color scale used to score the sialadenitis symptoms.
Ancillaryanalysis
It was also made a comparison between paired pre- and postoperativevisualcolorscalescoresofsialadenitis symp-tomsthatwerefilledoutby21latestpatients.Thosecases weresubmittedeithertodiagnosticordiagnosticand ther-apeuticsialendoscopies. Visual color scale scores zerofor absenceofsymptomsand10formaximalsymptomatic dis-ease(Fig.4).Visualcolorscalequestionnaireswereapplied inan outpatientfashion,beforesialendoscopyandaround the30thpostoperativeday.
Results
Comparingearlyandlategroupsofthe
sialendoscopyexperience
Thepatientsmeanagewassimilarbetweengroups:groupA 49±3,rangingfrom17to83yearsold;groupB43±4years old,rangingfrom4to75(p=0.21).
Femalesweremorefrequentinbothgroups:58%ingroup Aand65%ingroupB(p=0.38).
In group A submandibular gland sialendoscopies were morefrequent(74%)thaningroupB(40%;p=0.0001*).
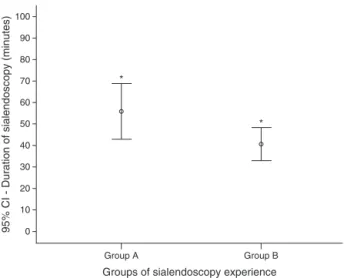
Sialadenitissymptomswithoutstonewerethemost fre-quent finding in both groups (Table 1). There was more salivarystoneingroupA.Group Bhadmorepatientswith historyofradioiodinetreatmentandwithrecurrentjuvenile parotitis.
Generalanesthesiawasperformedin80%ofgroupAand 89%ofgroupB(p=0.147).
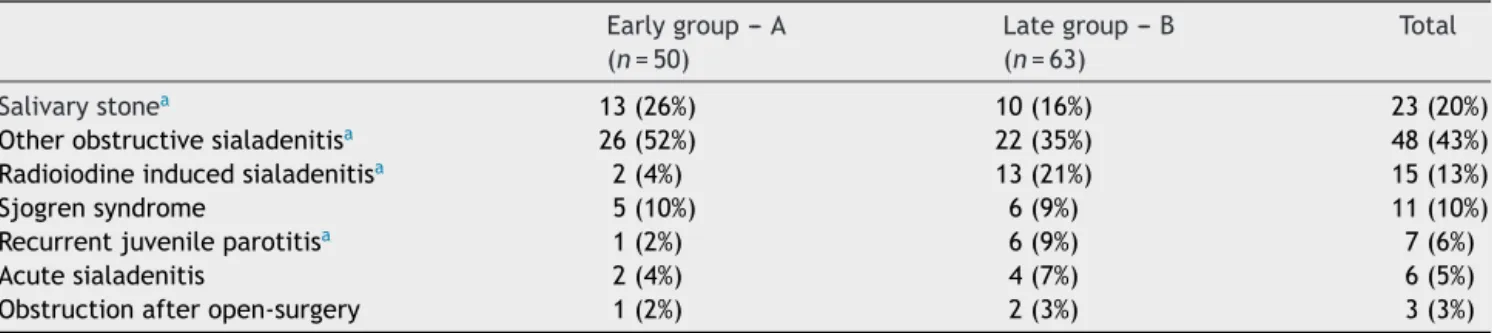
The duration time of sialendoscopies in group A was higher than group B:mean of 56min (ranging from20 to 160) against 41min (10---120) (p=0.045) (Fig. 5). To ana-lyze thesialendoscopy durationfor each examined gland,
100
90
80
70
60
50
40
30
20
10
Group A
Groups of sialendoscopy experience *
*
95% CI - Duration of sialendoscopy (minutes)
Group B 0
Figure5 Comparisonbetweenmeansofsialendoscopy dura-tion (min) according to early and late groups of surgeon experience(*Studentt-test,p=0.045).
weexcludedcasesinwhichpapillacatheterizationwasnot achieved.
Table 2 displays the comparison of perioperative out-comesbetweengroupsAandB.Therewashigherfrequency offailureofdiagnosticsialendoscopyingroupAmainlydue tofailureofpapillacatheterizationinthisgroup.Whenthe papillawassuccessfully catheterized,failure tocomplete endoscopicexaminationwashigheringroupAtoo. There-fore,necessitytorepeatthisprocedureinthesamepatient ingroupAwasmorefrequent.
Group A sialendoscopies with failure to complete examination included the 11 procedures where papilla catheterizationwasnotachievedand4others;falsepassage of the endoscope due to duct perforation; sialendoscopy underlocalanesthesiainterruptedbypain;twoothersdue toanatomicdifficulties.
Table1 Sialendoscopyindicationsofearlyandlategroupsofsialendoscopyexperience. Earlygroup---A
(n=50)
Lategroup---B (n=63)
Total
Salivarystonea 13(26%) 10(16%) 23(20%)
Otherobstructivesialadenitisa 26(52%) 22(35%) 48(43%)
Radioiodineinducedsialadenitisa 2(4%) 13(21%) 15(13%)
Sjogrensyndrome 5(10%) 6(9%) 11(10%)
Recurrentjuvenileparotitisa 1(2%) 6(9%) 7(6%)
Acutesialadenitis 2(4%) 4(7%) 6(5%)
Obstructionafteropen-surgery 1(2%) 2(3%) 3(3%)
US,ultrasonography.
aFisher’sexacttest,p≤0,05.
Table2 Comparisonofperioperativeoutcomesbetweengroupsofearlyandlatesialendoscopyexperience. Earlygroup---A
(n=50)
Lategroup---B (n=63)
Total p
Failureofdiagnosticsialendoscopy 15(30%) 4(6%) 19(17%) 0.001a
Failureofpapillacatheterization 11(22%) 2(3%) Failuretocompleteexamination 4(8%) 2(3%)
Necessitytorepeatsialendoscopy 11(22%) 6(10%) 17(15%) 0.058
Perioperativecomplication 9(18%) 6(10%) 15(13%) 0.149
aFisher’sexactteststatisticallysignificant.
AsingroupAsubmandibularglandsialendoscopieswere morefrequent, we performed a multivariate analysisand foundthat,independentoftheglandtype,sialendoscopies ofgroupAwererelatedtomorefailurestocomplete exam-ination(multivariatetest,p=0.02).
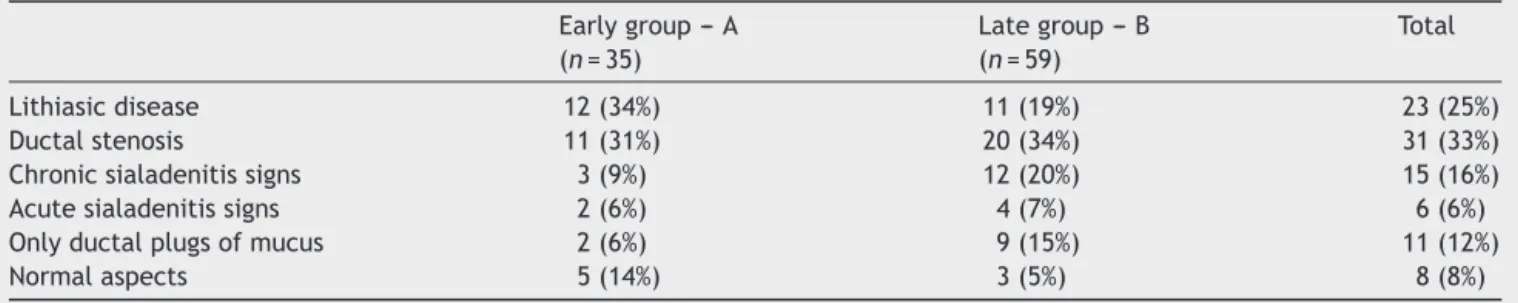
Endoscopicfindingsofthesialendoscopiesaredisplayed inTable3.
Treatmentwasintendedin70%(36/50)oftheprocedures ingroupAandin91%(57/63)ingroupB(p=0.006).Failure toachievetreatment in group Ahappened in 25%(9/36), andingroupBin5%(3/57)(p=0.008).
Therewasnostatisticallysignificantdifferencein peri-operative complications between groups (Table 2). The complicationswerethefollowing:
Falsepassageoftheendoscopeduetoductperforation:3 ingroupAand4ingroupB;
Papillaavulsion:2ingroupAand1ingroupB;
Severe swellingandpainsymptomsassociatedwith glan-dularinfectionin1caseofeachgroup;
Salivaryfistulain1caseofgroupA;
Salivaryductrestenosisin2casesofgroupA.
Ancillaryanalysis
Preoperative median score of the visual color scale of sialadenitissymptoms(9ranging from5 to10) washigher thanthepostoperativeone(2rangingfrom0to9)(Wilcoxon Test,p=0.001).Evenpatientssubmittedtodiagnostic sia-lendoscopy without a treatment procedure presented a reliefofsialadenitissymptoms duetopapilladilationand steroidsinstilation.
Discussion
Sialendoscopyisarelativelynewprocedureforthediagnosis andtreatmentofsalivaryductdiseases.Itwasintroduced intoclinicalpracticeinthelate1990s,andcausedan expres-sivechangeinthediagnosticandtherapeuticmanagement ofsialolithiasis.3Oneofthemajorchangeswasthe
reduc-tionof thenumberof salivaryglandsremoved becauseof salivaryglandstones.4
Untilrecently,themainuseofsialendoscopywasto con-firmthediagnosisofobstructionsandtoremovesialoliths, butitsusewasextendedtootherinflammatorypathologies like radioiodine sialadenitis, juvenile recurrent parotitis, Sjogren’sdiseaseandductstenosis.10---13
Sialendoscopyisveryhelpful asa diagnosticmethodin theinvestigationofinflammatorydiseasesofunknownorigin within salivaryglands.14 Despite itsconceptual simplicity,
sialendoscopy is a challenging procedure, particularly the therapeutic ones,requiring skilledand experiencedhands giventhepotentialriskofperforationofthesalivaryduct.2
Obstaclestoimplementthisprocedureincludetheinitial costoftheequipmentandtheassociatedlearningcurveof usingameticulousnewtechnique.6
Inthisstudy,mostofendoscopies(85%)wereperformed undergeneralanesthesiainanoutpatientfashion,butthe procedurecanbeperformedunderlocalanesthesiatoo.The typeofanesthesiacanbeamatterofchoiceforthepatient or thesurgical team,but itseemsthatgeneralanesthesia canbebettersuitableforthebeginningofthelearningcurve andforcomplexcasestoo.
Table3 Endoscopicfindings inearlyandlategroupsofsialendoscopyexperience(excludedcaseswithfailuretocomplete sialendoscopy).
Earlygroup---A (n=35)
Lategroup---B (n=59)
Total
Lithiasicdisease 12(34%) 11(19%) 23(25%)
Ductalstenosis 11(31%) 20(34%) 31(33%)
Chronicsialadenitissigns 3(9%) 12(20%) 15(16%)
Acutesialadenitissigns 2(6%) 4(7%) 6(6%)
Onlyductalplugsofmucus 2(6%) 9(15%) 11(12%)
Normalaspects 5(14%) 3(5%) 8(8%)
cause (23%). One of the reasons for that is the presence of other common causes of obstructive sialadenitis less described in literature series but common in our clini-cal practice, like radioiodine induced sialadenitis (13%), because we are a reference center for thyroid cancer treatment. Stenosis without lithiasis is a common cause of obstruction in ourexperience (31%),sometimes with a knowncause(likeradioiodineorSjogrendisease),and some-times withno apparent cause (idiopathic).The literature considers stenosis as the second cause of obstruction.13
With the development of the sialendoscopy technique, probablyindications other than lithiasis will bemore and morefrequent.Accordingly,inourexperienceRITinduced sialadenitis was more frequent in group B. Despite the variability of causes for indication of sialendoscopy, the techniqueforthediagnosticexamisthesame,soour anal-ysisofthelearningprogressioncanbeextrapolated.
Alltheprocedureswereperformedbythesamesurgeon withthesameequipmentafterinitialrecognizedhandson training.Postoperativeoutcomesthatwerebetterafter50 sialendoscopies arelinked todirect surgeonability, espe-ciallysalivarypapillacatheterization.
Analyzing interquartile charts of sialendoscopies sequence, itwasnoticed that thefirst twoquartiles con-centratedmorecasesoffailuresinpapillacatheterization, casesoffailureincompletingtheexaminationand achiev-ingtreatment goal whencomparedto latequartiles.This improvement was statistically confirmed by comparisons between early and late groups, both in univariate and multivariateanalysis.Thisdatasuggeststhat50procedures couldbeconsidered asanacceptable limitinthelearning curve for sialendoscopy. After the first 50 exams papilla catheterizationwasnot achievedonlyin bilateral parotid glandsofthesamepatient,suggestingaspecificanatomical variation,ratherthananunexperiencedsurgeon.
In the literature, Danquart et al.15 described that the
successratesrosefromthefirst25procedurestothefinal 25procedures,althoughnotsignificantly. Soitseemsthat thelearningcurveeffectisreallyobtainedaftermorethan 25procedures,aswefound.
The groups’ demographic and clinical features were homogeneous, but more frequent submandibular endo-scopies were found in the initial group. We asked if the worstoutcomesinthebeginningcouldbeduetothis find-ingandnotduetolearningcurve.Toanswer thisquestion amultivariateanalysiswasperformed.Resultsshowed bet-teroutcomes withthelearningprogressionindependently ofthefrequencyoftheexaminedgland.Thesubmandibular
endoscopy was only associated with more complications thanparotidgland,whilethelearningcurvedidnotaffect thecomplicationrates.
The operative time wasshorter in group B, even with more complete exams and more therapeutic procedures, which demand more time. In group A the sialendoscopy mean duration was 56min, and in group B 41min. The literature describes that the mean duration of diagnostic and operative sialendoscopy is, respectively, 26±14 and 73±43min.16
Papillacatheterizationwasachievedin 89%ofthe pro-cedures, similarto literature.15 More experienced groups
describesuccessratesfrom96%to98%17,18toachieve
ther-apeuticgoal,thesameasgroupB(95%),whilegroupAhad only75%.
Despitethe surgeonlearningcurve,the overall rateof complicationswaslow,comparablewithliterature.19
The most frequent effectof sialendoscopy is the tran-sitoryglandular swelling due to irrigation.The frequency in ourstudy was61%, and literature describes ashigh as 80---100%.13
Majorcomplicationsasductperforationwithfalse pas-sagewererarelydescribedintheliterature.Ourincidence was documented as 8%, all with spontaneous resolution. Danquart15reported6%.Mostofourcomplicationswerein
submandibularexams.We alsohadtwocases ofinfection andwedecidedtosystematicallyprescribeantibioticsafter that.Intheliteraturethefrequency describedwas1.6%.1
Other complications described in literature1 like bleeding
andnerveinjurywerenotobservedinourcasuistic. Steno-sisoccurredasarecurrenceofsomecasestreatedinitially asstenosis,soitisnotreallyacomplicationoftheprocedure butanevolutionofthepathology.
Thiswasalsothefirstpaperthatanalyzedinanobjective waytheevolutionofpatients’symptomswithsialendoscopy. Even if not being used for all cases yet, ancillary analy-sisshowedanaverageimprovementinvisualcolorscaleof symptomsfrom9to2,andthiswasstatisticallysignificant. Welookforwardtocontinuingthisanalysistoevaluatelater outcomesinfurtherstudies.
Conclusions
The complication rate wasnot affected by the learn-ingprogression,withstatisticallythesameresultsbetween earlyandlategroupsofsialendoscopyexperience.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.MarchalF,Dulguerov P, Lehmann W. Interventional sialendo-scopy.NEnglJMed.1999;341:1242---3.
2.BaptistaPM,VilarCG,MartínezJAR,FalconeMC.Sialendoscopy: anewalternativeforthetreatmentofsalivarypathology.Our experience.ActaOtorrinolaringolEsp.2008;59:120---3. 3.LuersJC,GroshevaM,ReifferscheidV,StennerM,BeutnerD.
Sialendoscopy for sialolithiasis: early treatment,better out-come.HeadNeck.2012;34:499---504.
4.IroH,DlugaiczykJ,ZenkJ.Currentconceptsindiagnosisand treatmentofsialolithiasis.BrJHospMed.2006;67:24---8. 5.ArdekianL,KleinH,AbrilR,MarchalF.Sialendoscopyforthe
diagnosisandtreatmentofjuvenilerecurrentparotiditis.Rev StomatolChirMaxillofacChirOrale.2014;115:17---21.
6.Maresh A, Kutler DI, Kacker A. Sialendoscopy inthe diagno-sisandmanagementofobstructivesialadenitis.Laryngoscope. 2011;121:495---500.
7.Marchal F,Chossegros C, GuyotL. A technical improvement in sialendoscopy to enter the salivary ducts. Laryngoscope. 2006;116:842---4.
8.VairelB, DeBonnecazeG, AlShehriS.Learningcurve in sia-lendoscopy:ourfirst101procedures.RevLaringolOtolRhinol. 2012;133:177---81.
9.WalvekarRR,RazfarA, CarrauRL.Sialendoscopyand associ-atedcomplications: a preliminaryexperience.Laryngoscope. 2008;118:776---9.
10.NahlieliO,NazarianY.Sialadenitisfollowingradioiodine ther-apy --- a new diagnostic and treatment modality. Oral Dis. 2006;12:476---9.
11.Capaccio P,Sigismund PE, LucaN, Marchisio P, Pignataro L. Modernmanagementofjuvenilerecurrentparotitis.JLaryngol Otol.2012;126:1254---60.
12.Shacham R, Puterman MB, Ohana N, Nahlieli O. Endoscopic treatmentofsalivaryglandsaffectedbyautoimmunediseases. JOralMaxillofacSurg.2011;69:476---81.
13.Capaccio P, Torretta S, Ottavian F, Sambataro G, Pignataro L.Modernmanagementofobstructivesalivarydiseases.Acta OtorhinolaryngolItal.2007;27:161---72.
14.NahlieliO,BaruchinA.Long-termexperiencewithendoscopic diagnosis and treatment of salivary gland inflammatory dis-eases.Laryngoscope.2000;110:988---93.
15.DanquartJ,Wagner N,ArndalH,HomøeP.Sialendoscopyfor diagnosisand treatmentofnon-neoplasticobstructioninthe salivaryglands.DanMedBull.2011;58:A4232.
16.Marchal F, Dulguerov P, Becker M, Barki G, Disant F, Lehmann W. Specificity for parotid sialendoscopy. Laryngo-scope.2001;111:264---71.
17.MarchalF,DuelguerovP.Sialolithiasismanagement:thestate of the art. Arch Otolaryngol Head Neck Surg. 2003;29: 951---6.
18.NahlieliO,NakarLH,NazarianY,TurnerMD.Sialendoscopy:a newapproachtosalivaryglandobstructivepathology.JAmDent Assoc.2006;137:1394---400.