REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Hyperglycemia
assessment
in
the
post-anesthesia
care
unit
Vinicius
Rodovalho
Pereira,
Rodrigo
Akio
Azuma,
Bruno
Emanuel
Oliva
Gatto,
João
Manoel
Silva
Junior
∗,
Maria
Jose
Carvalho
Carmona,
Luiz
Marcelo
Sá
Malbouisson
UniversidadedeSãoPaulo(USP),FaculdadedeMedicina,HospitaldasClínicasdeSãoPaulo,SãoPaulo,SP,Brazil
Received22February2015;accepted17August2015 Availableonline21September2017
KEYWORDS
Electivesurgery; Hyperglycemia; Prevalence; Riskfactors; Post-anestheticcare unit
Abstract
Backgroundandobjectives: Hyperglycemia insurgicalpatients may causeseriousproblems.
Analyzingthiscomplicationinthisscenariocontributestoimprovethemanagementofthese patients.Theaimofthisstudywastoevaluatetheprevalenceofhyperglycemiainthe post-anestheticcareunit(PACU)innon-diabeticpatientsundergoingelectivesurgeryandanalyze thepossibleriskfactorsassociatedwiththiscomplication.
Methods:We evaluatednon-diabeticpatientsundergoingelectivesurgeriesandadmittedin
thePACU.Datawerecollectedfrommedicalrecordsthroughprecodedquestionnaire. Hyper-glycemiawasconsideredwhenbloodglucosewas>120mg.dL−1.Patientswithhyperglycemia
were compared to normoglycemic ones toassess factorsassociated with theproblem. We excludedpatientswithendocrine-metabolicdisorders,diabetes,childrenunder18years,body massindex(BMI)below18orabove35,pregnancy,postpartumorbreastfeeding,historyofdrug use,andemergencysurgeries.
Results:Weevaluated837patients.Themeanagewas47.8±16.1years.Theprevalenceof
hyperglycemiainthepostoperativeperiodwas26.4%.Inmultivariateanalysis,age(OR=1.031, 95% CI1.017---1.045);BMI(OR=1.052,95%CI 1.005---1.101);durationofsurgery(OR=1.011, 95%CI1.008---1.014),historyofhypertension(OR=1.620,95%CI1.053---2.493),and intraoper-ativeuseofcorticosteroids(OR=5.465,95%CI3.421---8.731)wereindependentriskfactorsfor postoperativehyperglycemia.
Conclusion: TheprevalenceofhyperglycemiawashighinthePACU,andfactorssuchasage,
BMI, corticosteroids, blood pressure, and duration of surgery are strongly related to this complication.
©2016SociedadeBrasileiradeAnestesiologia.Publishedby ElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
∗Correspondingauthor.
E-mail:joao.s@globo.com(J.M.SilvaJunior).
http://dx.doi.org/10.1016/j.bjane.2015.08.005
PALAVRAS-CHAVE
Cirurgiaeletiva; Hiperglicemia; Prevalência; Fatoresderisco; Saladerecuperac¸ão anestésica
Avaliac¸ãodehiperglicemianasaladerecuperac¸ãopós-anestésica
Resumo
Justificativaeobjetivos: Hiperglicemiaem pacientescirúrgicospodeocasionargraves
prob-lemas. Nesse contexto, analisar essa complicac¸ão contribui para o melhor manejo desses pacientes. O objetivo do estudo foi avaliar a prevalência de hiperglicemia na sala de recuperac¸ãopós-anestésica(SRPA)empacientesnãodiabéticossubmetidosacirurgiaseletivas eanalisarospossíveisfatoresderiscoassociadosaessacomplicac¸ão.
Métodos: Foramavaliadospacientesnãodiabéticossubmetidosacirurgiaseletivaseadmitidos
naSRPA.Osdadosforamcoletadosdosprontuáriospormeiodequestionáriopré-codificado.Foi consideradahiperglicemiaquandoaglicemiaera>120mg.dL−1.Pacientescomhiperglicemia
foramcomparadoscomosnormoglicêmicosparaavaliarfatoresassociadosaoproblema.Foram excluídosospacientescomdistúrbiosendócrino-metabólicos,diabéticos,menoresde18anos, índicedemassacorpórea(IMC)menordoque18oumaiordoque35,gestac¸ão,puerpérioou aleitamentomaterno,antecedentedeusodedrogasecirurgiasdeurgência.
Resultados: Foramavaliados837pacientes.Amédiadeidadefoi47,8±16,1anos.A
prevalên-ciadehiperglicemianopós-operatóriofoide26,4%.Naanálisemultivariada,idade(OR=1,031; IC95%1,017-1,045);IMC(OR=1,052;IC95%1,005-1,101);tempocirúrgico(OR=1,011;IC95% 1,008-1,014);antecedentedehipertensão(OR=1,620;IC95%1,053-2,493)eusodecorticoides intraoperatório(OR=5,465;IC95%3,421-8,731)representaramfatoresderiscoindependentes parahiperglicemianopós-operatório.
Conclusão:Hiperglicemia apresentou alta prevalência na SRPA e fatores como idade, IMC,
corticoides, hipertensão arterial e tempo de cirurgia são fortemente relacionados a essa complicac¸ão.
©2016SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigoOpen Accesssobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Althoughglycemiclevelsupto220mg.dL−1werepreviously consideredacceptable incritically illpatients,1 infectious
and metabolic complications were reported as a conse-quenceofhyperglycemia.2,3
Hyperglycemia resulting from surgical stress has long beenconsideredanadaptiveandbeneficialresponse.1
How-ever,the surgicalwound triggersaseriesofother events, whichin association withhyperglycemia maybe deleteri-ous.Insurgicalpatient,neuroendocrineresponses suchas releaseofcatecholamines,stress hormones,inflammatory cascade activation, and systemic inflammatory response resultinincreasedproteincatabolism,adiposetissue mobi-lization,gluconeogenesis,andglycogenolysis.
Another centralphenomenon in the incidence of post-operative hyperglycemia is the development of insulin resistance induced by surgical stress.4 The sum of these
effectsleadstoprolongedpostoperativerecovery,increased metabolicstress,andriskofcomplications.4Inearly
postop-erativeperiod,adequatecontrolofhyperglycemiaresultsin fastersurgicalrecovery,withlessincidenceofcomplications and lower hospital costs in patients undergoing major surgeries.5---8
The relationship between hyperglycemia and progno-sis has recently been investigated in patients with acute neurological disease,9,10 acute myocardial infarction,11,12
trauma,13 andperipheral arterialdisease.14 Intraoperative
hyperglycemia is correlated with death and signifi-cant organic dysfunction in patients undergoing heart
surgery.15---17However,thereisashortageofdatasenttothe
post-anesthetic care unit (PACU) onnon-diabetic patients undergoingelectivesurgeries.
Therefore, the aim of this paper wasto evaluate the prevalenceofhyperglycemiainnon-diabeticpatients under-goingelectivesurgeriessenttothePACUandassesstherisk factorsforthisseriouscomplication.
Material
and
methods
After approval by the Ethics Committee of the HCFMUSP, which waived the consent term as this is a non-interventionalstudy,weretrospectivelyevaluatedpatients whounderwentelective surgerybetweenAugust2012and September2014attheHospitaldasClínicas,Faculdadede Medicina da Universidade de Sao Paulo. All patients who wereadmittedtothePostAnesthesiaCareUnit(PACU)and hadabloodglucosetestwereincludedinthestudy.
According to a protocol previously established in the institution, all patients have their capillary glucose mea-suredandiftwomeasurementshavechangedvalues,serum glucoseismeasuredtoconfirmtheresults.Avaluegreater than 120mg.dL−1 is used as a cut-off point for hyper-glycemia, according to the literature,18 and a value of
orbreastfeeding),endocrine-metabolicdisorders,previous diagnosisofdiabetes,andaknownorsuspectedhistoryof drugabuse.
The primary objective of this study was to assess the prevalence of hyperglycemia in PACU and the secondary wastoassesstheriskfactorsforhyperglycemia.Inorderto findarepresentativesampleandcometoanagreementfor thesamplecalculationthathyperglycemiacanaffectabout 4---5%ofthepopulation,19 withan estimatetypeIerrorof
5%and95%power,weconsideredasanoptionalhypothesis 5%ofpatientswithhyperglycemiaadmittedtothePACUand 2%asanullhypothesis.Thus,atleast446patientswouldbe requiredfor thestudy.However,asapprovedbythe insti-tution’scommittee,datacouldbecollectedforaperiodof twoyears,sothestudywasonlystoppedaftercompleting thisperiod.
The assesseddataweresex,age,BMI,anesthetic tech-nique,durationofsurgery,glucoseuse,corticoiduse,need fortransfusionorintraoperativeuseofvasopressors, comor-bidities,typeofsurgery,andglycemicvalueobtainedfrom thechartsofpatientsadmittedtoPACU.
Inordertofindfactorsrelatedtohyperglycemia,patients withhigh blood glucose levelswerecompared withthose considerednormoglycemic,andlogisticregressionwasalso performedwiththemostrelevantdatafromthisevaluation. Statistical analysis was performed using the SPSS 15.0 software (SPSS Inc.,USA). Chi-square test, Fisher’s exact test, and likelihood ratio test were used for assessing qualitativevariables.Parametriccontinuousvariableswere testedusingStudent’st-test.Subsequently,thedatawere submittedtothelogisticregressiontest.
A p-value<0.05 was considered significant in bivariate analysisforinclusionofvariablesinthelogisticregression model.Multivariateanalysiswasusedtoidentify indepen-dentpredictorsofhyperglycemiainPACU.
Results
During the study period, 1000 patients were eligible for analysis;however,16.3% wereexcluded becausetheyhad diabetes.Thus, 837patientswere enrolled:326maleand 511female,meanagesof47.8±16.1years.Meanblood glu-cosevalueswere108.6mg.dL−1.Onaverage, patientshad BMIof26.2kgm−2.Durationofsurgerywas137.2
±76.5min (Table1).
The incidence of hyperglycemia in the postoperative periodwas26.4%.
Arterialhypertensionwasseeninpatientswithglucose concentrationgreaterthan120mg.dL−1.Moreover,patients who hadhyperglycemia in the early postoperative period havereceivedmoreintraoperativegeneralanesthesia, cor-ticosteroidsorvasopressors(Table2).
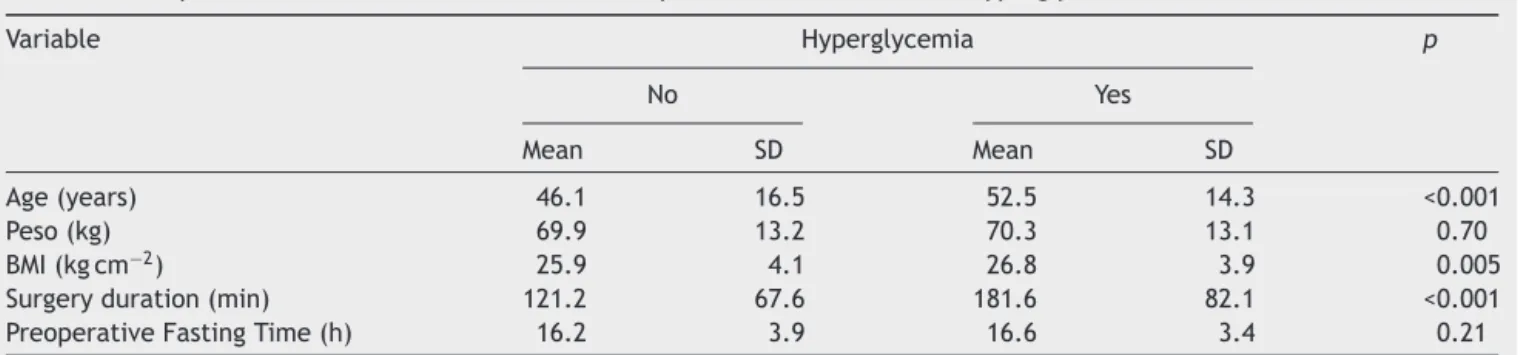
Inaddition,olderpatients,thosewithahigherBMIand longer durationof surgery presented more hyperglycemia postoperatively(Table3).
When usingthelogistic regressionmodel,at each one-yearincreaseinage,thereisa3.1%increaseinthechance ofhyperglycemia(OR=1.031),anda1kgm−2increaseinBMI leadstoanincreaseof5.2%inthechanceofhyperglycemia (OR=1.052). Furthermore, duration of surgery presented a statistically significant correlation with hyperglycemia.
Finally,intraoperativeuseofcorticosteroidsincreasedthe risk of postoperative hyperglycemia by 5.46 (OR=5.465) (Table4).
Interestingly,intraoperativeglucoseadministrationwas observedin14.1%of thesample, therewasnocorrelation withhyperglycemia.
In general, 11 patients (1.2% of sample) had hypo-glycemia, ranging from46 to60mg.dL−1, requiring treat-ment,andninepatients(0.9%ofsample)hadglucosevalues between200and299andrequiredinsulintherapyinPACU.
Discussion
The main findings of this study were the high prevalence ofhyperglycemia intheadmissionofpatientstoPACUand thefactthatage,BMI,arterialhypertension,intraoperative corticoiduse,anddurationofsurgerywereindependentrisk factorsfortheoccurrenceofhyperglycemiainthe immedi-atepostoperativeperiod.
An assessment of the impact of hyperglycemia on admission to intensive care units found an incidence of hyperglycemia in 27.5% of the 2713 patients included in the study. However, the study population consisted of critically ill patients with indication for intensive care hospitalization.19 Thus, the present study is one of the
fewthatevaluatedthiscomplicationinpatientsofelective surgerieswhowereadmittedtoPACU.
Overall, 26.4% of patients had hyperglycemia in this study. The cut-off point was greater than 120mg.dL−1, which is compatiblewiththat used by the American Dia-betesAssociation18andbystudiesthatseektojustifystrict
glycemiccontrolinpostoperativepatients.20,21
Hyperglycemiaispotentiallydeleteriousbecauseitacts asa procoagulant,22 changes neutrophil functions,
stimu-latesthereleaseofinflammatory cytokines,increasesthe risk of infections, changes healing, and may be associ-atedwithincreasedmortality.23,24Therefore,evaluatingthis
complicationandassociatedfactorsisimportanttoimprove thisproblemmanagement.
It wasalso observed in this study that age is an inde-pendentrisk factor for hyperglycemia in this population. Thismaybeexplainedbythefactthatwithagingthereare changesininsulinsecretionandincreasedperipheral resis-tancetoitseffects,whichcantriggerhyperglycemia.25After
theageof50,thefastingbloodglucoselevel increasesby 6---14mg.dL−1every10years.26
Additionally, the increase in BMIwasalso a risk factor forthe postoperativeincidenceof hyperglycemia,leading toa5.2%increaseinriskforeach1kgcm−2increaseinBMI. Obesepatients haveahigh incidenceof diabetesand glu-coseintolerance.Themuscularandadiposetissueofobese patientsresponds lesstoinsulin action due toadecrease inthe numberof receptors anda lowerresponse created bytheinsulin---receptorinteraction.27Inobesepatients,the
cortisolproduction is also altered, increasingthe periph-eralresistancetoinsulin.Inastudywith50,905adults,it wasshown that BMI is an independent predictor for dia-betes,withthreetimeshigherprevalenceinpatientswith BMI>24.28
Table1 Characteristicsofpatients.
Variable Mean SD Median Minimum Maximum
Age(years) 47.8 16.1 47 18 90
Weight(kg) 70.0 13.1 69 42 120
Height(cm) 163.4 9.4 163 140 199
BMI(kgcm−2) 26.2 4.1 26.0 17 35
Surgeryduration(min) 137.2 76.5 120 10 555 Anesthesiatime(min) 210.9 89.7 195 40 610 Glycemia(mg.dL−1) 108.7 29.7 105 46 299
SD,standarddeviation;BMI,bodymassindex.
Table2 Comparisonofcategoricalvariablesbetweenpatientswithandwithouthyperglycemia.
Variable Hyperglycemia Total p
No Yes n %
n % n %
Sex 0.51
Female 372 60.4 139 62.9 511 61.1
Male 244 39.6 82 37.1 326 38.9
Typeofsurgery 0.78
Abdominal 281 45.6 105 47.5 386 46.1 Headandneck 88 14.3 37 16.7 125 14.9 Ophthalmic 86 14.0 32 14.5 118 14.1 Urological 85 13.8 25 11.3 110 13.1
Plastic 56 9.1 17 7.7 73 8.7
Other 20 3.2 5.0 2.3 25 3.0
Intraoperativeglucoseuse 84 13.6 34 15.4 118 14.1 0.52
Intraoperativecorticoiduse 339 55.1 193 87.3 532 63.6 <0.001
Anesthesia 0.01
General 401 65.1 164 74.2 565 67.5 Neuraxial 215 34.9 57 25.8 272 32.5
Intraoperativevasopressor 41 6.7 25 11.3 66 7.9 0.03
Intraoperativetransfusion 2.0 0.3 0.0 0.0 2.0 0.2 0.54a
Comorbidities
Arterialhypertension 169 27.4 93 42.1 262 31.3 <0.001
Dyslipidemia 36 5.8 16 7.2 52 6.2 0.46
Asthma 12 1.9 9 4.1 21 2.5 0.08
Kidneyfailure 15 2.4 9 4.1 24 2.9 0.21
Cirrhosis 2.0 0.3 0.0 0.0 2.0 0.2 0.54a
Crohn’sdisease 3.0 0.5 2.0 0.9 5.0 0.6 0.40a
CHF 3.0 0.5 2.0 0.9 5 0.6 0.40a
COPD 5.0 0.8 5.0 2.3 10.0 1.2 0.09a
Hypothyroidism 36 5.8 12.0 5.4 48 5.7 0.82
Hyperthyroidism 3.0 0.5 4.0 1.8 7.0 0.8 0.83a
Chi-squaretest.
aFisherexacttest;Other:neurosurgery,thoracic,vascular.
Dexamethasoneis oftenusedduring anestheticprocedure as adjunctive treatment to prevent nausea and vomiting andinhibitinflammatoryresponse.However,itsuse, even in a single dose, may trigger hyperglycemia by stimulat-ingneoglucogenesisandinhibitingperipheralinsulinaction. One study29 showed that intraoperative dexamethasone
(10mg) given to patients undergoing abdominal surgery
increased glycemia in both diabetic and non-diabetic patients. Several other studies have also demonstrated theseeffectstriggeredbytheuseofcorticosteroids.30,31
Table3 Comparisonofcontinuousvariablesbetweenpatientswithandwithouthyperglycemia.
Variable Hyperglycemia p
No Yes
Mean SD Mean SD
Age(years) 46.1 16.5 52.5 14.3 <0.001
Peso(kg) 69.9 13.2 70.3 13.1 0.70
BMI(kgcm−2) 25.9 4.1 26.8 3.9 0.005
Surgeryduration(min) 121.2 67.6 181.6 82.1 <0.001 PreoperativeFastingTime(h) 16.2 3.9 16.6 3.4 0.21
BMI,bodymassindex;SD,standarddeviation.
Table4 Multiplelogisticregression.
Variable OR 95%CI p
Inferior Superior
Age(peryear) 1.031 1.017 1.045 <0.001 BMI(perkgm−2) 1.052 1.005 1.101 0.03
Intraoperativeuseofcorticosteroids(perunit) 5.465 3.421 8.731 <0.001 Generalanesthesia(perunit) 1.330 0.883 2.002 0.172
SAH(perunit) 1.620 1.053 2.493 0.028
Intraoperativeuseofvasopressor(perunit) 1.238 0.678 2.258 0.487 Durationofsurgery(permin) 1.011 1.008 1.014 <0.001
BMI,bodymassindex;SAH,systemicarterialhypertension.
lowerinsulin secretionandperipheral tissueresistanceto theactionofinsulinandproducehyperglycemia.Thelength anddurationofthesurgicalinterventiondetermineagreat variationinthecontributionofcounterregulatoryhormones, suchasglucagon,epinephrine,norepinephrine,cortisoland GH,inordertoinfluenceglycemichomeostasis.32---34
Itisimportanttonotethatinthepresentstudy,incidence of hypoglycemia was observed in 1.2% of patients, which makes intraoperative glycemic control essential, as anes-thesia masksthe hypoglycemiasymptoms. Alarge study35
drewattentiontotheproblemrelatedtohypoglycemiaand associatedcomplications.
However, some limitations in this study should be reported, such as lack of informationon some variables. First, it was not possible to distinguish transient eleva-tionofblood glucoseor glucoseintolerance.Glycosylated hemoglobin(A1Ctest)couldhelpinthisdifferentiation.19
Furthermore,inthisstudy,nooutpatientcontrol medica-tionswereevaluatedinasthmaticpatients,mainlyregarding theuseofinhaledorsystemiccorticosteroids,andthe sever-ityprofileofpatients.
Regarding intraoperative use of corticosteroids, there wasnodistinctionbetweenthetypeofcorticosteroidused (dexamethasoneorhydrocortisone)orcorrelationbetween theuseddoseandriskofhyperglycemia.
Evaluationregardingthe typeof anesthesiaandsizeof surgerywasverybroad,withoutdetailsontheeffectofeach anestheticagentandthecorrelationbetweenthedoseused andduration time.These limitations, however,are inher-ent tothis type of study, which is an analysis withmany variables.
However,wenotethehighprevalenceofhyperglycemia in PACU, so measurement of glycemia either capillary or anothermethod is crucialdue to the great rangeof fac-torscorrelatedwiththeoccurrenceof thisprobleminthe postoperativeperiod.Ontheotherhand,thedatashowed anincreasedprevalenceofhyperglycemiainolderpatients with high BMI. These findings are significant and suggest theneedfor furtherstudiesonthesubject,mainly focus-ingonstrictglycemiccontrolinthistypeofpatientsfrom intraoperativeperiodtohospitaldischarge.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Vanhorebeek I, Langouche L, Van den Berghe G. Tight bloodglucose control:what isthe evidence? CritCareMed. 2007;35:S496---502.
2.McCowen KC, MalhotraA, BistrianBR. Stress-induced hyper-glycemia.CritCareClin.2001;17:107---24.
3.PozzilliP,LeslieRD.Infectionsanddiabetes:mechanismsand prospectsforprevention.DiabetMed.1994;11:935---41.
4.Ljungqvist O, Nygren J, Soop M, et al. Metabolic periop-erative management: novel concepts. Curr Opin Crit Care. 2005;11:295---9.
6.ThorellA,NygrenJ,HirshmanMF,etal.Surgery-inducedinsulin resistanceinhumanpatients:relationtoglucosetransportand utilization.AmJPhysiol.1999;276:E754---61.
7.ThorellA,NygrenJ,LjungqvistO.Insulinresistance:amarkerof surgicalstress.CurrOpinClinNutrMetabCare.1999;2:69---78.
8.Van den Berghe G, Wouters P, Weekers F, et al. Inten-sive insulin therapy in critically ill patients. NEngl J Med. 2001;345:1359---67.
9.Alvarez-SabinJ, MolinaCA, Ribo M,et al. Impactof admis-sion hyperglycemia on stroke outcome after thrombolysis: risk stratification inrelation to timeto reperfusion. Stroke. 2004;35:2493---8.
10.Juvela S, Siironen J, Kuhmonen J. Hyperglycemia, excess weight,andhistoryofhypertensionasriskfactorsforpoor out-come and cerebralinfarction afteraneurysmal subarachnoid hemorrhage.JNeurosurg.2005;102:998---1003.
11.Suleiman M,HammermanH, BoulosM,etal.Fastingglucose isanimportantindependentriskfactorfor30-daymortalityin patientswithacutemyocardialinfarction:aprospectivestudy. Circulation.2005;111:754---60.
12.TimmerJR,vanderHorst IC,OttervangerJP, etal. Prognos-tic value ofadmission glucose in non-diabetic patients with myocardialinfarction.AmHeartJ.2004;148:399---404.
13.Laird AM, Miller PR, Kilgo PD, et al. Relationship of early hyperglycemia to mortality in trauma patients. J Trauma. 2004;56:1058---62.
14.Vriesendorp TM, Morelis QJ, Devries JH, et al. Early post-operative glucose levels are an independent risk factor for infection after peripheral vascular surgery. A retrospective study.EurJVascEndovascSurg.2004;28:520---5.
15.FurnaryAP,GaoG,GrunkemeierGL,etal.Continuousinsulin infusionreducesmortalityinpatientswithdiabetes undergo-ingcoronaryarterybypassgrafting.JThoracCardiovascSurg. 2003;125:1007---21.
16.Furnary AP, Wu Y, Bookin SO. Effect of hyperglycemia and continuous intravenousinsulin infusionson outcomes of car-diacsurgicalprocedures:thePortlandDiabeticProject.Endocr Pract.2004;Suppl.2:21---33.
17.Gandhi GY,NuttallGA,AbelMD, etal.Intraoperative hyper-glycemia and perioperative outcomes in cardiac surgery patients.MayoClinProc.2005;80:862---6.
18.American Diabetes A. Standards ofmedical care in diabetes 2013.DiabetesCare.2013;Suppl.1:S11---66.
19.AldamP,LevyN,HallGM.Perioperativemanagementofdiabetic patients:newcontroversies.BrJAnaesth.2014;113:906---9.
20.MalerbiDA,FrancoLJ.Multicenterstudyoftheprevalenceof diabetesmellitusandimpairedglucosetoleranceintheurban
Brazilianpopulationaged30---69yr.TheBrazilianCooperative Group on the Study of Diabetes Prevalence. Diabetes Care. 1992;15:1509---16.
21.VandenBergheG,WilmerA,MilantsI,etal.Intensiveinsulin therapyinmixedmedical/surgicalintensivecareunits:benefit versusharm.Diabetes.2006;55:3151---9.
22.CarrME.Diabetesmellitus:ahypercoagulablestate.JDiabetes Complicat.2001;15:44---54.
23.BlondetJJ, BeilmanGJ. Glycemiccontrol and preventionof perioperativeinfection.CurrOpinCritCare.2007;13:421---7.
24.TurinaM,MillerFN,TuckerCF,etal.Short-termhyperglycemia insurgicalpatientsandastudyofrelatedcellularmechanisms. AnnSurg.2006;243:845---51,discussion51---3.
25.Mooradian AD. Mechanisms of age-related endocrine alter-ations.PartII.DrugsAging.1993;3:131---46.
26.Mooradian AD. Mechanisms of age-related endocrine alter-ations.PartI.DrugsAging.1993;3:81---97.
27.LorentzMN,AlbergariaVF,LimaFASd.Anestesiaparaobesidade mórbida.RevBrasAnestesiol.2007;57:199---213.
28.HeY,ZhaiF,MaG,etal.Abdominalobesityandtheprevalence ofdiabetesandintermediatehyperglycaemiainChineseadults. PublicHealthNutr.2009;12:1078---84.
29.HansP,VanthuyneA,DewandrePY,etal.Bloodglucose concen-trationprofileafter10mgdexamethasoneinnon-diabeticand type2 diabeticpatients undergoing abdominalsurgery. Br J Anaesth.2006;97:164---70.
30.GulcanE, BulutI, TokerA, etal. Evaluation ofglucose tol-erancestatus inpatientswithasthmabronchiale.JAsthma. 2009;46:207---9.
31.KoskelaHO, SalonenPH, NiskanenL. Hyperglycaemia during exacerbationsofasthmaandchronicobstructivepulmonary dis-ease.ClinRespirJ.2013;7:382---9.
32.GiuriniJM,CookEA, CookJJ.Diabetes:the latesttrendsin glycemiccontrol.ClinPodiatrMedSurg.2007;24:159---89.
33.Gottschalk A, Rink B, Smektala R, et al. Spinal anesthesia protectsagainstperioperativehyperglycemiainpatients under-goinghiparthroplasty.JClinAnesth.2014;26:455---60.
34.Kilickan L, Yumuk Z, Bayindir O. The effect of combined preinductionthoracicepiduralanaesthesiaandglucocorticoid administrationonperioperativeinterleukin-10levelsand hyper-glycemia. A randomized controlled trial. J Cardiovasc Surg (Torino).2008;49:87---93.