Case Report
Introduction
Thrombotic complications may occur in neonates under intensive care who require prolonged hospitalization, central venous catheter, broad-spectrum antibiotic therapy, parenteral nutrition, and blood products. These thrombi are particularly associated with the use of central venous catheter and systemic infections. A careful differential diagnosis among intracardiac masses (thrombus, tumor, and vegetation) that includes clinical history, physical examination, laboratory tests (blood culture), and echocardiogram should be made1,2.
Both clinical and surgical intracardiac thrombosis management in neonates are controversial, since thus far there is little scientific evidence about which treatment is most effective3.
Owing to the sometimes fatal risk of thromboembolism in these patients, thrombolytic agents, especially recombinant tissue plasminogen activator (rTPA), are being successfully used in the pediatric population4. There are few reports describing
the use of this drug in neonates, particularly prematures with very low birth weight. The therapeutic range of this agent, therefore, remains unknown. Antiplatelet drugs (aspirin), considered adjuvants to antithrombotic therapy, have been
showing satisfactory results.
Case Report
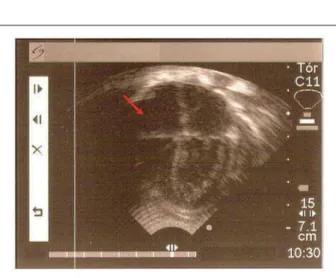
A female premature neonate (postnatal gestational age 34.4 weeks), the first twin delivered by cesarean section, with APGAR score 7/8, intact membranes, head circumference 29 cm; and length 40 cm was admitted to the Neonatal Intensive Care Unit (UTI da CRIANÇA) for early respiratory distress. At the beginning of the 75-day hospital stay, she had moderate hyaline membrane disease, early neonatal sepsis associated with meningitis, pneumonia, and jaundice. She was given exogenous surfactant, invasive and non-invasive ventilation (811 hours of oxygen exposure), broad-spectrum antibiotic therapy (covering anaerobic, fungal, Gram-positive and Gram-negative organisms), light therapy, cardiotonics, blood products, intravenous immunoglobulin (three days), and total parenteral nutrition (32 days). The baby girl developed necrotizing enterocolitis (Bell stage II), anemia, right pleural effusion, bronchopulmonary dysplasia; disseminated intravascular coagulation, gastroesophageal reflux, plus sucking and swallowing incoordination. Besides the peripheral vascular access, a peripherally inserted central catheter (PICC) was placed via the brachial vein and maintained for 17 days. Once her condition was clinically and surgically controlled (bowel resection and ileostomy), she showed C-reactive protein levels as high as >50 mg/dL (Reference value < 6mg/dL), despite negative cultures (blood, cerebrospinal fluid, urine, pleural fluid, catheter tip), normal blood count, and negative serological tests for syphilis, toxoplasmosis, hepatitis B, and cytomegalovirus, in addition to her mother being HIV-negative. By this time (49 days of life), the presence of an asymptomatic clinical infection was suspected (septic arthritis, osteomyelitis, endocarditis), and appropriate studies were conducted. Imaging studies (long-bone x-rays and joint ultrasonography) were unremarkable, but the two-dimensional Doppler echocardiogram revealed an irregularly-contoured intracavitary thrombus in the right atrium that protruded towards the right ventricle during atrial systole (Figure 1). After family consent was obtained, rTPA was administered in six-hour infusions for ten days, with daily dosage being progressively increased (0.2 mg to 0.5 mg/Kg/hour). Serial echocardiographic studies were performed throughout treatment to evaluate thrombus regression, which occurred at completion of the thrombolytic therapy (Figure 2).
Following the rTPA treatment, acetylsalicylic acid was given (3 mg/kg/day) for three months, with echocardiographic monitoring, leading to total thrombus dissolution (Figure 3). No adverse events were observed during the thrombolytic therapy.
Key words
Fibrinolytic agents; plasminogen; aspirin; thrombosis/ complications; platelet aggregation inhibitors.
We describe a case of a very low birth weight premature female twin with intracardiac thrombosis. Her condition was consistent with neonatal sepsis, and she was treated with advanced life support, antibiotic therapy, parenteral nutrition, blood transfusion, and central venous catheterization. Infective endocarditis was suspected, and a large intracavitary thrombus was detected by two-dimensional Doppler echocardiography. Surgical procedure was not only technically difficult but also highly lethal, being contraindicated in some cases. Consequently, the use of the thrombolytic recombinant tissue-plasminogen activator (rTPA) associated with aspirin was the treatment of choice, and complete dissolution of the thrombus was achieved without adverse effects.
Combined rTPA and Aspirin Therapy for Intracardiac Thrombosis in
Neonates
Fernanda Almeida Tardin, Antônio Carlos Avanza Júnior, Marcos Rogério Arantes Andião, Sônia Maria Alves Andrade
Rabello, Emília de Mattos Gouvêa Cristello, Edna Cellis Vaccari Baltan, Edelweiss Bussinguer Pereira Pegurin, Norma
Suely Oliveira
Santa Casa de Misericórdia de Vitória, UTI da Criança, Hospital Infantil Nossa Senhora da Glória – Vila Velha, ES - Brazil
Mailing address: Fernanda Almeida Tardin •
Rua Marechal Barbacena, 1088/42 – Vila Regente Feijó – 03333-000 – Vila Velha, ES - Brazil
E-mail: ferdialmeida@hotmail.com
Manuscript received August 17, 2006; revised received November 9, 2006; accepted December 14, 2006.
Case Report
Tardin et al Combined rTPA and aspirin therapy for intracardiac thrombosis in neonates
Arq Bras Cardiol 2007; 88(5) : e118-e120
Discussion
Preterm, very low birth weight neonates often develop severe cardiorespiratory and infectious complications, among them septic arthritis, osteomyelitis, and endocarditis. Some patients require central venous catheter, therefore complications secondary to this procedure are likely to occur. Central venous catheter and infective endocarditis are possible causes of thrombi formation6.
Based on this patient’s clinical and laboratory parameters, a treatment for infective endocarditis was offered as primary option, and appropriate studies were performed. Among the diagnostic possibilities, such as thrombus, tumor, and vegetation, the hypothesis of thrombosis was the most likely, considering the long-term use of central venous catheter, absence of cardiovascular symptoms, negative blood culture, echocardiographic images showing normal cardiac chambers, and the presence of a single, homogeneous, smooth-surfaced echodense mass in the right atrium, non-adherent to the wall or to the tricuspid valve.
Peripherally inserted central catheters are routinely used in neonates to optimize nutrition and provide stable infusion of medication into the central vascular system. Central catheters are associated with thromboembolic events and may be observed in 13% to 74% of pediatric patients. Among risk factors, no relationship was found with the type of catheter insertion (peripheral or central), its diameter or dwell time, but rather with its location (most frequently in the femoral and subclavian veins and less frequently in the brachial and jugular veins)9. Even though the route used in this patient was that of
lowest risk, thrombotic events may occur; however, neither the intracardiac location nor the large volume found is common.
Surgical approach in these cases is not only technically difficult but also associated with high mortality, especially in premature neonates, and may be contraindicated in thrombosis within right heart chambers6. In spite of the limited experience
with rTPA in neonates, some authors have successfully used this drug in pediatric patients. Although no double-blind, randomized clinical trial evaluating its therapeutic efficacy and side effects has yet been conducted, this agent is known to have low affinity for circulating plasminogen, which allows thrombus resolution without systemic repercussions and, thereby, supports its use. Combination therapy with this thrombolytic and aspirin yielded excellent results, with total thrombus dissolution and no complications, especially hemorrhagic, associated with other thrombolytics6. The fact that aspirin is an effective and
relatively safe antiplatelet agent, in addition to encouraging results from previous studies5, makes it a promising option for
treating intracavitary thrombus.
This study was intended to demonstrate that rTPA in combination with aspirin is an effective alternative for intracardiac thrombosis management in premature, very low birth weight neonates (<1500g), in whom surgical approach is technically difficult to perform and is associated with high mortality rates, and may be contraindicated. It also provides another piece of scientific evidence for refining the therapeutic modality in these cases, where no consensus exists in the literature.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Fig. 2 -Apical four-chamber view showing thrombus reduction (arrow) after ten days of rTPA therapy and two days of aspirin.
Fig. 1 - Apical four-chamber view suggesting the presence of thrombus/ vegetation in the right atrium protruding into the right ventricle (arrow), prior to treatment.
Fig. 3 -Apical four-chamber view showing total thrombus dissolution (arrow) after three months of therapy.
Case Report
Tardin et al
Combined rTPA and aspirin therapy for intracardiac thrombosis in neonates
Arq Bras Cardiol 2007; 88(5) : e118-e120
References
1. Silverman NH. Pediatric echocardiography. Baltimore, MD: Williams & Wilkins; 1993.
2. Dhahri K, Sandor G, Duncan W. Intra-atrial thrombus in a neonate with coarctation of the aorta. Cardiol Young. 2006;16: 392-4.
3. Schmidt B, Andrew M. Neonatal thrombosis: report of a prospective Canadian and international registry. Pediatrics. 1995; 96: 939-43.
4. Levitas A, Zucker N, Zalzstein E, Sofer S, Kapelushnik J, Marks A. Successful treatment of infective endocarditis with recombinant tissue plasminogen activator. J Pediatr. 2003; 143 (6): 649-52.
5. Adler A, Litmanovitz I, Bauer S, Dolfin T. Aspirin treatment for neonatal infectious endocarditis. Pediatric Cardiol. 2004; 25 (5): 562-4.
6. Andrew M, Brooker LA. Hemostatic disorders in newborns. In: Taeusch HW, Ballard RA. Avery’s diseases of the newborn. 7th ed. Philadelphia: WB Saunders Co; 1998. p. 1045-79.
7. Petti J. Assessment of infants with peripherally inserted central catheters: Part 2. Detecting less frequently occurring complications. Adv Neonatal Care. 2003;3(1):14-26.
8. Kuhle S, Massicotte P, Chan A, Adams M, Abdolell M, de Veber G, et al. Systemic thromboembolism in children: data from the 1800-NO-CLOTS consultation. Thromb Haemost. 2004;92(4):722-8.
9. Male C, Julian JA, Massicotte P, Gent M, Mitchell L. Significant association with location of central venous line placement and risk of venous thrombosis in children. Thromb Haemost. 2005; 94 (3): 516-22.