w w w . r b o . o r g . b r
Original
Article
Fasciocutaneous
flaps
for
covering
foot
and
ankle
injuries
夽,夽夽
Alexandre
Carvalho
Quirino
a,∗,
Karen
Cristina
Viegas
b aHandSurgeryService,HospitalSãoJoãodeDeus,Divinópolis,MG,BrazilbUniversidadeFederaldeSãoJoãoDelRei,SãoJoãoDelRei,MG,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received18January2012
Accepted27May2013
Availableonline18March2014
Keywords:
Surgicalflaps
Lowerextremity
Leginjuries/surgery
Reconstructivesurgicalprocedures
a
b
s
t
r
a
c
t
Objective:to presentsomecasesfromourserviceandtoconfirm thatsural andlateral
supramalleolarflapsaregoodoptionsforcoveringthesofttissuesofthefootandankle.
Methods:twenty-twoflapswereconstructedin21patientsofagesrangingfrom15to72
years.Malepatientspredominated(66.6%)andin47.6%ofthecasestheinjuryresulted
fromaccidentsinvolvingmotorcycles.
Results:amongthe22flaps,12weresuraland10werelateralsupramalleolar;inonecase,
twoflapswereused.Inallthecases,theinjuriesweresuccessfullycoveredandthepatients
recoveredwell.Duringthepostoperativefollow-up,thecommonestcomplicationwas
epi-dermolysis,occurringineightcases(threeinasuralflapandfiveinasupramalleolarflap),
amongwhichtwocasesprogressedtodistalnecrosisoftheflap(onesuralandtheother
supramalleolar).Onepatientwantedtheflapreviewedforestheticreasons.
Conclusions: suralandsupramalleolarflapsareveryreliable.Theypreservethemaintrunk
arteries,arequicklydissected,havelowhospitalcost,enablecoverageofextensiveareas,
presentestheticallyacceptabledamagetothedonorareaanddonotimpairmotorfunction.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora
Ltda.Allrightsreserved.
Retalhos
fasciocutâneos
para
cobertura
de
lesões
no
pé
e
tornozelo
Palavras-chave:
Retalhoscirúrgicos
Extremidadeinferior
Traumatismosdaperna/cirurgia
Procedimentoscirúrgicos
reconstrutivos
r
e
s
u
m
o
Objetivo:mostraralgunscasosdonossoservic¸o,alémdeconfirmarcomoboasopc¸õesos
retalhossuralesupramaleolarlateralnacoberturadepartesmolesdopéetornozelo.
Métodos:foramfeitos22retalhosem21pacientes,entre15e72anos.Houvepredomínio
dosexomasculino,com66,6%,eem47,6%aslesõesforamdecorrentesdeacidentesque
envolverammotocicletas.
Resultados: dos22retalhos,12foramdotiposurale10,supramaleolarlateral.Emumcaso
usaram-seosdoisretalhos.Emtodososcasoshouvesucessonacoberturadaslesões,com
boarecuperac¸ãodospacientes.Noseguimentopós-operatórioacomplicac¸ãomaiscomum
夽
Pleasecitethisarticleas:QuirinoAC,ViegasKC.Retalhosfasciocutâneosparacoberturadelesõesnopéetornozelo.RevBrasOrtop.
2014;49:183–188.
夽夽
WorkperformedatHospitalSãoJoãodeDeusandatHospitalSantaLúcia,Divinópolis,MG,Brazil.
∗ Correspondingauthor.
E-mail:alexandrequirino@uol.com.br(A.C.Quirino).
2255-4971/$–seefrontmatter©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditoraLtda.Allrightsreserved.
184
rev bras ortop.2014;49(2):183–188foi aepidermólise, comoitocasos, trêsnoretalhosural ecinconosupramaleolar, dos
quaisdoisprogrediramparapequenanecrosedistaldoretalho,umdelessuraleooutro
supramaleolar.Umpacientedesejoureveroretalhoporquestãoestética.
Conclusões: osretalhossuralesupramaleolarsãobastanteconfiáveis,preservamostroncos
arteriaisprincipais,sãoderápidadissecc¸ão,têmbaixocustohospitalar,permitem
cober-turadeáreasextensaseapresentamdanoestéticoaceitávelnaáreadoadorasemprejuízo
funcionalmotor.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier
EditoraLtda.Todososdireitosreservados.
Introduction
Beforebeginningthisstudy,weobtainedapprovalfromthe
BrazilPlatform, anonline toolforregisteringresearchthat
involveshumanbeings,whichisaimedtowardthegeneral
publicandtowardaidingtheworkoftheResearch
Commit-teesystemandtheNationalResearchEthicsCommitteeofthe
NationalHealthCouncil(CEP/CONEP/CNS).
Today,withthesignificantlyincreasednumberofcarand
motorcycleaccidents,tissuelossesfrom thefootandankle
regionarebecomingincreasinglyfrequent.1Theseinjuriesare
dealtwithroutinelyatreferralservices,wherelabor,surgical
techniquesandspecializedtrainingareabundantlyavailable,
withthecapabilitytoresolvesuchlossesusingfreeflaps.
Ontheotherhand,manysuchservices,oftendistantfrom
themetropolises,alsoreceivesignificantnumbersofcasesof
theseinjuriesbutdonothavethesameconditionsasthe
refer-ral services. Thus, onevery reasonablechoicefor covering
these tissue losses in feet and ankles is sural
fasciocuta-neousandlateralsupramalleolarflaps.Thesetwoflapswere
describedbyMasqueletetal.in1992,2,3andtheyhavebecome
oneofthefewoptionsforcoveringtheseregions,whichhave
asparsevascularbed4inwhichbonesandtendonsareoften
foundtobeexposedinadditiontovesselsandnerves.
Suralandlateralsupramalleolarflapsareveryreliable5,6:
theypreservethemaintrunkarteries,canbedissectedrapidly
and,differentlyfromfreeflaps,havealowhospitalcost.They
makeit possibletocover largeareas,havealargerangeof
rotation,5,7presentedacceptableestheticdamageinthedonor
area without functional damageand are therefore a good
choiceforcoveringfootandankleinjuries.8
Thepresentstudyhadtheaimofshowingsomecasesfrom
ourservice,aswellasconfirmingthatsuralandlateral
supra-malleolarflapsaregoodoptionsforcoveringsofttissuesofthe
footandankle.Italsoconfirmsthatmanyinjuriesthat
for-merlywereonlycoveredwithfreeflapscanalsoberesolved
using fasciocutaneous flaps, withfaster and simpler
tech-niques,atservicesthatdonothavethehumanand/orsurgical
resourcesformicrosurgicalflapsofgreatersophistication.In
thismanner,freeflapsareleftasthelastoptionand/orfor
casesinwhichtherereallyisnootherchoice.
Materials
and
methods
Twenty-onepatients(22flaps)attendedatHospitalSãoJoão
deDeusandHospitalSantaLúciainDivinópolis,MinasGerais,
between2007 and 2012, were evaluated. Fourteen patients
Table1–Detailsofthepopulationstudied.
Variables N %
Sex
Male 14 66.67
Female 7 33.33
Causeofinjury
Motorcycleaccidents 10 47.62
Othertypes 11 52.38
Comorbidities
Yes 3(SAHa:2/DMb:1) 14.28
No 18 85.72
a Systemicarterialhypertension.
b Diabetesmellitus.
weremaleandsevenwerefemale,withameanageof37years
andarangefrom15to72.Thesideaffectedanddominantside
wereevenlybalancedamongthepatients.
In10patients(47.6%),theinjuriesresultedfrommotorcycle
accidents.Theinjurieswereobservedindifferentregionsof
thefootandankle,withninecasesintheankle,seveninthe
hindfoot(includingtheheel)andsixbetweenthemidfootand
forefoot.Thetimethathadelapsedbetweentheinjuryandthe
surgerytoprovidecoveragerangedfromtwoto264days,with
ameanof40.3.Therewerefourcontaminatedcases,which
weretheoneswiththelongestdelayinprovisionofcoverage,
withameanof116.5days.
Threepatientspresentedcomorbidities:twowithsystemic
arterialhypertension (SAH)andonewithdiabetes mellitus
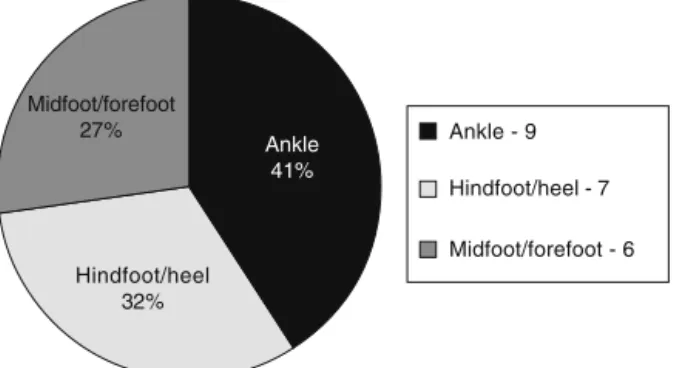
(DM)(Table1andFig.1).
Thesurgical optionsforcovering thetissue losses were
chosenbetweensuralflaps(constructedin12patients)and
Hindfoot/heel 32%
Ankle - 9
Hindfoot/heel - 7
Midfoot/forefoot - 6 Ankle
41% Midfoot/forefoot
27%
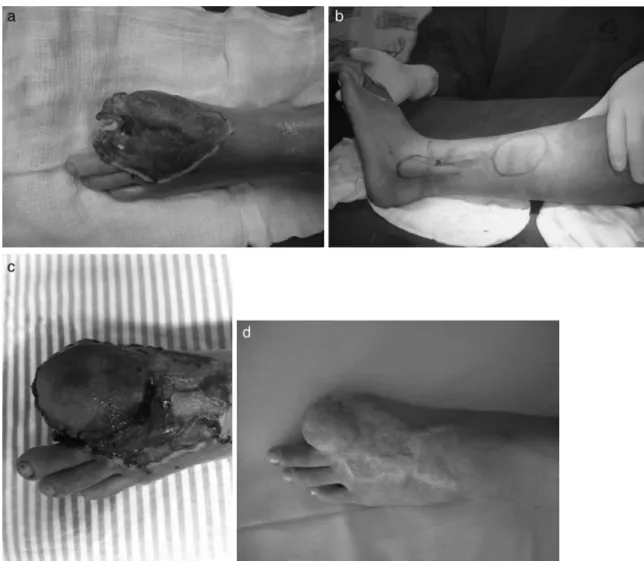
Fig.2–Case1,rightfoot.(a)Lossofskinandbonetissueattheleveloftheheel;contaminatedwound;(b)markingforthe suralflapwithstartofthedissectionandapivotpoint5cmabovethelateralmalleolus;(c)finalresultafter18monthsof evolution,withoutinfection.
lateralsupramalleolarflaps(in10patients).Bothflapswere
usedinonepatient.
Bothofthesearefasciocutaneousflaps,composedofskin,
subcutaneoustissueandfascia.Suralflapscontainthesural
nerveand,forthisreason,theyarealsoneurocutaneousflaps
withirrigationthroughabranchofthefibularartery,thesural
artery.9,10Meanwhile,supramalleolarflapsaresuppliedbyan
anastomoticnetworkfromtheankle.11
Theflapisonlyconstructedafterrigorousdebridementin
oneormoresurgicalprocedures,depending onthetypeof
woundandthe degreeofcontamination.Thepositionwas
chosenaccordingtothechoiceofflap:ventraldecubitusfor
thesuralflapandlateraldecubitusof50◦forthe
supramalle-olarflap.Bothofthesewereconstructedusingapneumatic
tourniquet.
Sural flaps were marked out starting at a point 5cm
abovethelateralmalleolus,atthesitewherethesuralartery
emerges,whichwasthepivotpoint.Alinewastracedout
lon-gitudinallyintheproximaldirection,betweenthispointand
theAchillestendon.Followingthis,amoldoftheinjurywas
madeusingacompress andmethyleneblue, soastothen
projectthemoldcorrespondingtotheareaoftheinjury,from
thepivotpointtothelocationforraisingtheflap,onthe
pos-teriorfaceofthelowerleg.Raisingtheflapbeganproximally,
withtheaidofamagnifyingglassof3.5×magnification,and
thesuralnerveandarterywerelocatedsoastoformpartofthe
flap.Theflapwascarefullyliftedfromasubfasciallayerand
thebranchesofthesuralarterytotheadjacentmuscleswere
cauterized.Thepedicleoftheflapshouldalwaysbe
accom-paniedbyabout2–3cmoffattytissuesurroundingit,sothat
thereisnoriskofdistressandtominimizecongestionofthe
flap(Fig.2a–c).
In the supramalleolar flap, a point was marked in the
depressionofthelower part ofthelocaltibiofibular space,
wheretheperforatingbranchofthefibulararterypenetrates
theinterosseousmembrane,around5cmfromthetipofthe
lateralmalleolus.Thisbranchisanastomosedwiththe
ante-riorlateralmalleolararteryandthenwiththelateraltarsal
arteryinthelateraledgeofthefoot.Theflapcanbe
peninsu-larorpedunculate,inanislandwithadistalbase,depending
ontheareaofcoverage.
Thesuralflapneededtobedesignedtobelocated2–3cm
distally tothe abovementionedpoint and,asdescribed for
suralflaps,thesupramalleolarflapwasalsodesigned
start-ing from the pivotpoint, with the mold ofthe injury, and
wasraisedwithabroadpedicleforsecurity.Thedissection
wasstartedontheanteriorfaceofthedesignandproceeded
proximally.Atthislocation,thesuperficialfibularnervewas
encountered andwas cauterized.Theflapwas raisedfrom
a subfascialplaneand was extendedto the periosteumof
thefibula.Iftherewasaneedforverydistalcoverageofthe
foot,thedissectionbecameslightlymorelaboriousandthere
was aneed todissect thepedicle beyondthe tarsal canal.
Atthislocation,thepediclewassubdermalandtherewasa
greaterriskofinjurytothepedicleandalsoofflapdistress
(Fig.3a–d).
Amongthesuralflapcases,flaprotationpassingthrougha
tunnelwasperformedinfivepatientsandtheskinwasopened
fortheflaptopassbyinsevenpatients.Elevenpatientsfirstly
underwentgraftinginthedonorarea.
Amongthesupramalleolarcases,theflapwasrotatedand
theskinwasopened(withoutatunnel)infivepatients,while
theflappassedthroughatunnelinfourpatientsandtheflap
waspeninsularinonepatient.Inallthesetenpatients,the
donorareafirstlyunderwentgrafting.
Outofthe21patients,thewoundswerecleanin17cases
and contaminated in four cases: three with osteomyelitis
and onewith pyoarthritis.Thirteenpatients camethrough
SUS,seventhroughcontractedservicesandoneasaprivate
patient.
All the patients were operatedunder spinalanesthesia.
Dopplerultrasoundwasnotusedinanyofthecases.
Sutur-ingwasperformedusingmononylon4.0and5.0andwasleft
quite slackwhen above the pedicle. Long gauze was used
extensively forthe dressings,withcareregarding
186
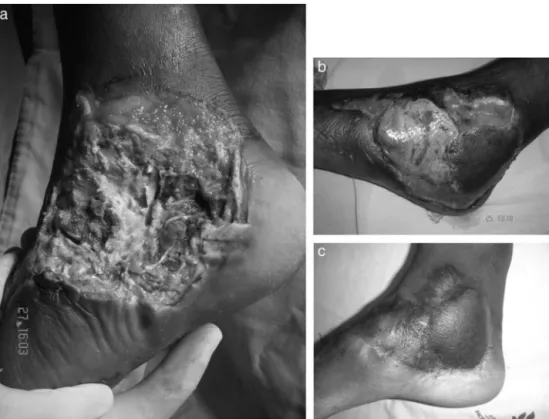
rev bras ortop.2014;49(2):183–188Fig.3–Case2,leftfoot.(a)Lossofskinandbonematerialattheleveloftheforefoot,withexposureofthephalanxboneand thesesamoidsofthehallux;(b)markingofthelateralsupramalleolarflapwiththepivotpointinthedepressioninthelower partofthetibiofibularspace,thelocationwheretheperforatingbranchofthefibulararterypenetratestheinterosseous membranearound5cmfromthetipofthelateralmalleolus;(c)7thpostoperativeday,showinggraftedareaaroundtheflap, andflapwithepidermolysis;(d)finalresultafter10monthsofevolution,showinggoodcoverageoftheinjury.
Results
Inallcases,theinjuriesweresuccessfullycovered,withgood
recoveryamongthepatients.However,somecomplications
wereobserved.Thecommonestofthesewasepidermolysis,
ineightcases(36.3%):threeinsuralflapsandfivein
supra-malleolarflaps.Ofthesepatients,two(onesuralandtheother
supramalleolar)progressedtoslightdistalnecrosisoftheflap.
Thesupramalleolarcaserequiredanewintervention, with
subsequentskingraftingatthesite.Inonepatientwhohad
alreadyundergonereconstructionwithasuralflap,theburn
injuryprogressed,withnewboneexposure.Itwasdecidedto
constructanewflap,choosingthelateralsupramalleolartype
(Fig.4a–c).
Amongthe four contaminated cases, oneof them
pre-sented recurrence of secretion drainage, even with the
treatment. Another two interventions were needed, with
debridementandcurettage.
Out ofthe21 patients operated,20 were notconcerned
regardingtheissueofestheticsandonlyonewishedtoreview
theflap.Fateliminationwasperformedoneyearafterthefirst
surgicalapproach.
Noneuromaswereobservedintheflapdonorareas,
nei-therinthesuralnorinthefibularnerve.Noneofthepatients
suffered gaitalterations consequenttoundergoingthe flap
surgery.Whenasked,allthepatientsreportedparesthesiaon
thelateralfaceofthefootincasesofsuralflapsorthemedial
andintermediatefacesofthemidfootandforefootincasesof
lateralsupramalleolarflaps.However,theydidnotplaceany
importanceonthissymptom.
Discussion
Flapsforprovidingskincoverageforfeetandankleshavebeen
described.6,12–17 However,inmost injuriesinvolvinglossof
tissue,itisnotpossibletoachievecoverageusingonlythe
sur-roundingtissue.Distantflapshavetobechosen,whichcould
befasciocutaneousorfreeflaps.6,13–17
Becausethesearepoorly vascularizedregions4 thatalso
Fig.4–Case3,rightfoot:suralandlateralsupramalleolarflaps.(a)Lossofskintissuewithboneexposureinthemidfoot andhindfootandpartoftheankle,secondarytoburnsafteranaccidentinvolvingamotorcycleexhaust;(b)suralflap integratedinthehindfootandlateralsupramalleolarflapwithepidermolysisinthemidfoot;(c)finalresultaftertwoyears ofevolution.
tendons,arteries,veins,nervesand,justbelow,bones,
cover-ageusingskingraftsisnotachievedinmostoftheseinjuries.
Thesesegmentsrequirestablecoveragesoastoenable
bet-terjointmobilityandmakeitpossibleforthetendonstoslide
well,forgaittooccurwithaminimumofclaudicationandfor
theretobeasfewfunctionalsequelaeaspossible.
Suraland lateral supramalleolarflapsare reliable, allow
coverage of extensive areas and have a large arc of
rotation.5,6,18,19Thus,theyareanexcellentchoiceforcoverage
ofinjuriestofeetandankles.6,20–22Eventhoughtheseflapsare
differentregardingtheirdissection,suchthatsupramalleolar
flapstakelonger,withgreatertechnicaldifficulty,wedidnot
observeanysignificantdifferencesregardingcomplications.
OurexperiencedifferedfromthatofTouametal.,whofound
agreaternumberofcomplications,suchasflapnecrosis,when
lateralsupramalleolarflapswerechosen.23
Thefirst-choiceflapwasthesuralflap,becauseitisthe
simplerofthetwo.Whatmattersisnotthesizeoftheinjury
but,rather,itslocation.Incasesofverydistalinjuriestothe
forefootandmidfoot,andinpatientswithscarsinthearea
wherethesuralflapwouldberaised,thelateral
supramalle-olarflapwaschosen.Inoursample,wecould seethatthe
greater timerequiredand thedifficulty citedin relationto
lateralsupramalleolarflapsonlyoccurredwhentherewasa
needtoextendthe flapbeyondthe pointcorresponding to
thedepressioninthelowerpartofthetibiofibularspace,the
locationwheretheperforatingbranchofthefibularartery
pen-etratestheinterosseousmembrane.Webelievethattheseare
thecasesinwhichtherearemorefailuresinraisingthisflap.
Withregardtotunnelconstruction,thereisdivergencein
theliteratureanditisbelievedthatthisincreasestheriskof
flapdistress,duetovesselcompression,24aswellastheriskof
distressduetotraction.Inthepresentstudy,wedonothave
sufficientcomparativedatatodecidebetweenopenor
tun-neledapproaches.However,incasesinwhichthetunnelwas
long,suchasinforefootinjuries,andinthoseinwhichthe
flapwasextensive,wepreferredtoopentheskinand
subcu-taneoustissue,ratherthanrunningtheriskofcompression
andtractionofthepedicle.
Conclusion
Suralandsupramalleolarflapsareverysafe,withreliable
pedi-cles, agood cost/benefitrelationship and acceptabletissue
damageintheregion.Theydonotcausefunctionaldamage,
thedurationofthesurgeryisshort,theyareeasytodissect,
importantvesselsintheregionarepreservedandthereisa
lowcomplicationrate.
They are options for providing coverage for extensive
injuries to the hindfoot, midfoot, forefoot and ankle; they
canbeperformedatmediumandhigh-complexityservices,
andcanbeconsideredtobeoneofthefirstchoicesforthese
injuries.
Conflicts
of
interest
188
rev bras ortop.2014;49(2):183–188Acknowledgement
Theauthors are gratefultoProf.Dr.ArlindoGomesPardini
Júnior.
r
e
f
e
r
e
n
c
e
s
1. MinistériodaSaúde–SistemasdeInformac¸õesHospitalares
doSUS(SIH-SUS).MorbidadeHospitalardoSUSpor
AcidentesdeTransporteporLocaldeInternac¸ãode
2008–2010.Availablefrom:http://tabnet.datasus.gov.br/
cgi/tabcgi.exe?sih/cnv/fiuf.def[accessed2012].
2. MasqueletAC,BeveridgeJ,RomanaC,GerberC.Thelateral supramalleolarflap.PlastReconstrSurg.1988;81(1):74–81.
3. MasqueletAC,RomanaMC,WolfG.Skinislandflapssupplied bythevascularaxisofthesensitivesuperficialnerves: anatomicstudyandclinicalexperienceintheleg.Plast ReconstrSurg.1992;89(6):1115–21.
4. Buluc¸L,TosunB,SenC,SarlakAY.Amodifiedtechniquefor transpositionofthereversesuralarteryflap.PlastReconstr Surg.2006;117(7):2488–92.
5. KneserU,BachAD,PolykandriotisE,KoppJ,HorchRE. Delayedreversesuralflapforstagedreconstructionofthe footandlowerleg.PlastReconstrSurg.2005;116(7):1910–7.
6. FollmarKE,BaccaraniA,BaumeisterSP,LevinLS,ErdmannD. Thedistallybasedsuralflap.PlastReconstrSurg.
2007;119(6):138e–48e.
7. GarciaAMC.Retalhosuralreversoparareconstruc¸ãodistalda perna,tornozelo,calcanharedopé.RevBrasCirPlast. 2009;24(1):96–103.
8. WeberES,FranciosiLF,MuellerSF,DalponteM,HeurichNR, Gonc¸alvesSC.Retalhosuralparareconstruc¸ãodopé.ACM ArqCatarinMed.2007;36Suppl.1:1–4.
9. AlmeidaMF,daCostaPR,OkawaRY.Reverse-flowislandsural flap.PlastReconstrSurg.2002;109(2):583–91.
10.VendraminFS.Retalhosuraldefluxoreverso:10anosde experiênciaclínicaemodificac¸ões.RevBrasCirPlast. 2012;27(2):309–15.
11.TorresCB.Elcolgajosupramaleolarlateral:uncolgajode excepción.RevColombOrtopTraumatol.2011;25(1):40–9.
12.MartinsGB,MoreiraAA,VianaFO.Reconstruc¸ãodelesõesde partesmolesdocalcanharcomousoderetalhos
fasciocutâneos.RevBrasCirPlast.2009;24(1):104–9.
13.MasqueletAC,GilbertA.Atlascoloridoderetalhosna reconstruc¸ãodosmembros.RiodeJaneiro:Revinter;1997.
14.KarkiD,NarayanRP.Theversatilityofperforator-based propellerflapforreconstructionofdistallegandankle defects.PlastSurgInt.2012;2012:303247.
15.RezendeMR,RabeloNTA,BenabouJE,WeiTH,MattarJR, ZumiottiAV,etal.Coberturadoterc¸odistaldapernacom retalhosdeperfurantespediculados.ActaOrtopBras. 2008;16(4):223–9.
16.LazoDA,ZatitiSCA,ColicchioO,AlvarezDM,MazzerN, AlvarezIM,etal.Oempregodosretalhoslivresempacientes queimados:experiênciade58retalhosem46pacientes.Rev BrasCirPlast.2009;24(2):138–44.
17.HellerL,LevinS.LowerExtremitymicrosurgical reconstruction.PlastReconstrSurg.2001;108(4):1029–41.
18.CheemaTA,SalehES,CarvalhoAF.Thedistallybasedsural arteryflapforankleandfootcoverage.JFootAnkleSurg. 2007;46(1):40–7.
19.All-QattanMM.Thereversesuralfasciomusculocutaneous “megahigh”flap:astudyof20consecutiveflapsfor lower-limbreconstruction.AnnPlastSurg.2007;58(5):513–6.
20.SugaH,OshimaY,HariiK,AsatoH,TakushimaA. Distally-basedsuralflapforreconstructionofthelowerleg andfoot.ScandJPlastReconstrSurgHandSurg.
2004;38(1):16–20.
21.AkhtarS,HameedA.Versatilityofthesuralfasciocutaneous flapinthecoverageoflowerthirdlegandhindfootdefects.J PlastReconstrAesthetSurg.2006;59(8):839–45.
22.DemiriE,ForoglouP,DionyssiouD,KakasAAP,PavlidisL, LazaridisL.Ourexperiencewiththelateralsupramalleolar islandflapforreconstructionofthedistallegandfoot:a reviewof20cases.ScandJPlasticReconstrSurgHandSurg. 2006;40(2):106–10.
23.TouamC,RostoucherP,BhatiaA,OberlinC.Comparative studyoftwoseriesofdistallybasedfasciocutaneousflapsfor coverageofthelowerone-fourthoftheleg,theankle,andthe foot.PlastReconstrSurg.2001;107(2):383–92.