www.jped.com.br
ORIGINAL
ARTICLE
Vitamin
D
deficiency
at
pediatric
intensive
care
admission
夽
Corsino
Rey
a,∗,
David
Sánchez-Arango
b,
Jesús
López-Herce
c,
Pablo
Martínez-Camblor
d,
Irene
García-Hernández
e,
Belén
Prieto
f,
Zamir
Pallavicini
gaPediatricIntensiveCareUnit,HospitalUniversitarioCentraldeAsturias,UniversidaddeOviedo,Oviedo,Spain bPediatricDayCareCenterofCulleredoandComplejoHospitalarioUniversitarioACoru˜na,ACoru˜na,Spain
cPediatricIntensiveCareDepartment,HospitalGeneralUniversitarioGregorioMara˜nón,InstitutodeInvestigaciónSanitaria
GregorioMara˜nón,UniversidadComplutensedeMadrid,Madrid,Spain
dOficinadeInvestigaciónBiosanitariaFICYT,UniversidaddeOviedo,Oviedo,Spain ePediatricService,ComplejoHospitalarioUniversitarioACoru˜na,ACoru˜na,Spain
fBiochemicalDepartment,HospitalUniversitarioCentraldeAsturias,UniversidaddeOviedo,Oviedo,Spain gPediatricService,HospitalUniversitarioCentraldeAsturias,Oviedo,Spain
Received22April2013;accepted7August2013 Availableonline30October2013
KEYWORDS
25hydroxivitaminD;
Critically-illchildren;
Criticalcare;
Prognosticmarkers;
Mortalityrisk
Abstract
Objective: toassesswhether25hydroxivitaminDor25(OH)vitDdeficiencyhasahighprevalence
atpediatricintensivecareunit(PICU)admission,andwhetheritisassociatedwithincreased
predictionofmortalityriskscores.
Method: prospectiveobservationalstudycomparing25(OH)vitDlevelsmeasuredin156patients
during the 12hours after critical careadmission with the25(OH)vitD levels of289 healthy
children.25(OH)vitDlevelswerealsocomparedbetweenPICUpatientswithpediatricriskof
mortalityIII(PRISMIII)orpediatricindexofmortality2(PIM2)>p75[(groupA;n=33)vs.the
others(groupB;n=123)].VitaminDdeficiencywasdefinedas<20ng/mLlevels.
Results: median(p25-p75)25(OH)vitDlevelwas 26.0ng/mL (19.2-35.8)inPICU patientsvs.
30.5ng/mL(23.2-38.6)inhealthychildren(p=0.007).Theprevalenceof25(OH)vitD<20ng/mL
was 29.5% (95% CI: 22.0-37.0) vs. 15.6% (95% CI: 12.2-20.0) (p=0.01). Pediatric intensive
carepatientspresentedanoddsratio(OR)forhypovitaminosisDof2.26(CI95%:1.41-3.61).
25(OH)vitD levels were 25.4ng/mL (CI 95%:15.5-36.0) in group A vs. 26.6ng/mL (CI 95%:
19.3-35.5)ingroupB(p=0.800).
Conclusions: hypovitaminosisDincidencewashighinPICUpatients.HypovitaminosisDwasnot
associatedwithhigherpredictionofriskmortalityscores.
©2013SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Allrightsreserved.
夽 Pleasecitethisarticleas:ReyC,Sánchez-ArangoD,López-HerceJ,Martínez-CamblorP,García-HernándezI,PrietoB,etal.VitaminD
deficiencyatpediatricintensivecareadmission.JPediatr(RioJ).2014;90:135---42.
∗Correspondingauthor.
E-mail:crey@uniovi.es(C.Rey).
0021-7557/$–seefrontmatter©2013SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Allrightsreserved.
PALAVRAS-CHAVE
25-hidroxivitaminaD;
Crianc¸asgravemente
doentes;
Terapiaintensiva;
Indicadores prognósticos;
Riscodemortalidade
DeficiênciadevitaminaDeminternac¸õesnaunidadedeterapiaintensivapediátrica
Resumo
Objetivo: avaliarseadeficiênciada25-hidroxivitaminaD,ou25(OH)vitD,temprevalência
elevadaeminternac¸õesnaunidadedeterapiaintensivapediátrica,eseestariarelacionadaà
previsãodeescoresderiscodemortalidade.
Método: estudoobservacionalprospectivocomparandoníveisde25(OH)vitDde156pacientes,
mensuradosnasprimeiras12horasdainternac¸ãoemterapiaintensiva,comníveisde25(OH)
vitDde289 crianc¸assaudáveis. Osníveisde 25(OH) vitDtambémforamcomparadosentre
pacientesnaUTIPcomescorePRISMIIIouPIM2>p75(GrupoA;n=33),eorestante,(Grupo
B;n=123).AdeficiênciadevitaminaDfoidefinidacomoníveis<20ng/mL.
Resultados: onívelmédio(p25-p75)de25(OH)vitDfoi26,0ng/mL(19,2-35,8)empacientes
internadosnaUTIP,emcomparac¸ãoa30,5ng/mL(23,2-38,6)emcrianc¸assaudáveis(p=0,007).
Aprevalênciade25(OH)vitD<20ng/mLfoide29,5%(IC95%,22,0-37,0),emcomparac¸ãoa
15,6%(IC95%,12,2-20,0)(p=0,01).Ospacientesemterapiaintensivapediátricaapresentaram
umarazãodechance(RC)parahipovitaminoseDde2,26(IC95%,1,41-3,61).Osníveisde25
(OH)vitDforam25,4ng/mL(IC95%,15,5-36,0)nogrupoA,emcomparac¸ãoa26,6ng/mL(IC
95%,19,3-35,5)nogrupoB(p=0,800).
Conclusões: aincidênciadehipovitaminoseDfoielevadaempacientesemterapiaintensiva
pediátrica,masnãofoiassociadaàmaiorprevisãodeescoresderiscodemortalidade.
©2013SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Todososdireitos
reservados.
Introduction
Low levels of vitamin D are common in adult and
pedi-atricpopulations.1VitaminDdeficiencyhasbeenclassically
related with osseous illness, such as rickets. Currently, vitaminDdeficiencyisconsideredtoberelatedwith over-allmortality,2 prevention of infections, innate immunity,3 hypertension,4hypertriglyceridemia,type1and2diabetes mellitus,5neoplasms,6andautoimmunedisorders.7In chil-dren, it has been related to severe asthma, bronchiolitis episodes,andlowerresponsetocorticoids.8
The most important source of vitamin D is the skin, through the action of ultraviolet B radiation on
7dehy-drocholesterol. Vitamin D must be metabolized to 25
hydroxivitaminD(25(OH)vitD)intheliver,whichisan inac-tiveprecursorwithahalf-lifeofapproximatelytwotothree weeks. The half-life of the active form (1,25(OH)vitD) is onlyfourto24hours.9Forthatreason,25(OH)vitDhasbeen themostcommonformofvitaminDmeasured inprevious studies10Inhealthychildren,age,skinpigmentation,season oftheyear,sunexposure,anddietarycalciumintake influ-ence25(OH)vitDconcentrations.Moststudieshaveadopted thedefinitionofvitaminDinsufficiencyas25(OH)vitD con-centrationslowerthan30ng/mL,andvitaminDdeficiency asconcentrationsbelow20ng/mL.10
Recently,vitaminDdeficiencyhasbeenassociatedwith higherillnessseverityuponadmission,mortality,andworse shortandlongtermoutcomesinadultintensivecareunits (ICU)patients.11---13Severalstudies14---16providednew infor-mationregardingtherelationshipbetweenvitaminDstatus andcriticalillnessesinchildrenadmittedtopediatricICUs (PICUs).ItwasobservedthathypovitaminosisDisacommon findingincritically-illchildren.McNallyetal.16alsoreported thatvitaminDdeficiencywasassociatedwithgreater sever-ityofcriticalillness.However,Rippeletal.14didnotfindan
association between hypovitaminosisD and length ofstay orhospitalsurvival.VitaminDstatusmayplayanimportant rolein acutestress andcriticalillness, butitspleiotropic effectsinacuteillnessarenotcompletelyunderstood.Many confounding factors (hemodilution, interstitial extravasa-tion,decreasedsynthesisofbindingproteins,renalwasting of25(OH)vitD,pH, underlyingdisease,seasonofthe year, age,anddietarysupplementation,amongothers)influence vitamin D status during critical illness.17 To date, there is noconsensus regarding the optimal definitions of vita-minD deficiency,northethresholdlevelstodefinehealth benefits.17,18
Therefore,thisstudyaimedtoinvestigatewhether vita-minDdeficiencyishighlyprevalentinpatientsadmittedtoa PICU.Thesecondaryobjectivewastoverifywhethervitamin Ddeficiency wouldbeassociatedwithincreasedmortality riskscoresandillnessseverityatPICUadmission.
Patients
and
methods
This studywasasecondaryanalysisof dataandbiological
samples collected aspart of the new prognosis
biomark-ers investigation,a prospective observationalstudy set in
theeight-bedPICUoftheHospitalUniversitarioCentralde
Asturias,inOviedo,Spain.Thestudyprotocolwasapproved
bytheHospitalEthicsCommittee.Thestudywasconducted
in 156 patients admitted to the PICU and agedless than
16 years.The exclusion criteriawereno blood extraction
during the first 12hours after admission; lack of consent
to participate by parents or by children older than 12
years;known or suspectedadrenal, pituitary, or
hypotha-lamicdisease;anduse ofsystemicsteroids for >tendays
intheprevious month,ormorethanonedose ofsystemic
steroidswithin24hoursofadmission(exceptfor
On every blood test sampledin the first12hoursafter
admission, the following variables were recorded: age,
weight,underlyingdisease,anddiagnosis.Respiratoryrate,
heart rate,blood pressure,O2 saturation, urinerate, and
administrationofvasopressoragentswererecordedhourly.
Radiographicandmicrobiologicdiagnosticswereperformed
whenindicated.Bloodcultureswereperformedwhenthere
was clinical suspicion of infection or when the patient’s
temperature was > 38◦C. The pediatric index of
mortal-ity 2 (PIM 2) value was calculated at admission, and the
pediatric risk of mortality III (PRISM III) value was
calcu-lated during the first 12h after admission, as it was the
normalclinicalpractice.Routinebiochemicalassays,
includ-ingC-reactiveprotein(CRP)andprocalcitonin(PCT),were
performedduringthefirst12hoursafteradmission.Venous
bloodsampleswerecollectedintubescontaining
ethylene-diamine-tetra-acetic acid (EDTA). A plasma aliquot was
frozen and stored at -80◦C for further determination of
25(OH)vitD,mid-regionalpro-adrenomedullin(MR-proADM),
andcarboxy-terminalpro-endothelin-1(CT-proET-1).
Healthychildren
The25(OH)vitDlevelsofthePICUpatientswerecompared
withthe 25(OH)vitD levels that were obtained aspart of
astudy onvitaminD statusthat iscurrently under
devel-opment in a population of healthy children fromthe city
ofOviedo(Asturias,Spain).Datafrom289healthychildren
wereobtained.
DefinitionofhypovitaminosisD
VitaminDdeficiencywasdefinedas<20ng/mL25(OH)vitD
levels.10
Mortality
risk
groups
Patientsweredividedintwogroupsaccordingtomortality
riskscores. Higherrisk mortalitygroup(groupA)included
patientswithaPIM2orPRISMIIIscore>p75(n=33);lower
risk mortality group (group B) comprised the remaining
patients(n=123).
Measurementof25(OH)vitD,CRP,PCT, MR-proADM,andCT-proET-1
Serum25(OH)vitDwasmeasuredusingadirectcompetitive
chemiluminescenceimmunoassay(LIAISON®Analyzer).The
assayrangeis4.0to150ng/mL.PlasmaCRPwasmeasured
onaModularAnalyticsCobacs6000(RocheDiagnostics-IN,
USA)usinganimmunoturbidimetrictechnique.The
analyti-caldetectionlimitwas0.07mg/dL.
MR-proADM,CT-proET-1,andPCTweremeasuredinEDTA
plasmausingasandwichimmunoassay(TRACEtechnology;
Brahms-Hennigsdorf,Germany).Analyticaldetectionlimits
were0.08nmol/Lforpro-ADM,0.4pmol/Lfor CT-proET-1,
and0.02ng/mLforPCT.
Statisticalanalysis
Patients’clinicalandbiologicalparametersweredescribed
usingfrequencies,percentages,means,medians,andranges
(p25-p75). Groups of patients were compared using the
Mann---Whitney U-test for continuous variables, and cross
tablesandexactchi-squaredtestwereusedforcategorical
data. Adjusted odds ratios (OR) were estimated by
mul-tivariatelogistic regression analysis(step-forward criteria
includingall relevant likelihood ratio based variables). A
p-value<0.05wasconsideredasstatisticallysignificant.
Results
Baselinecharacteristics
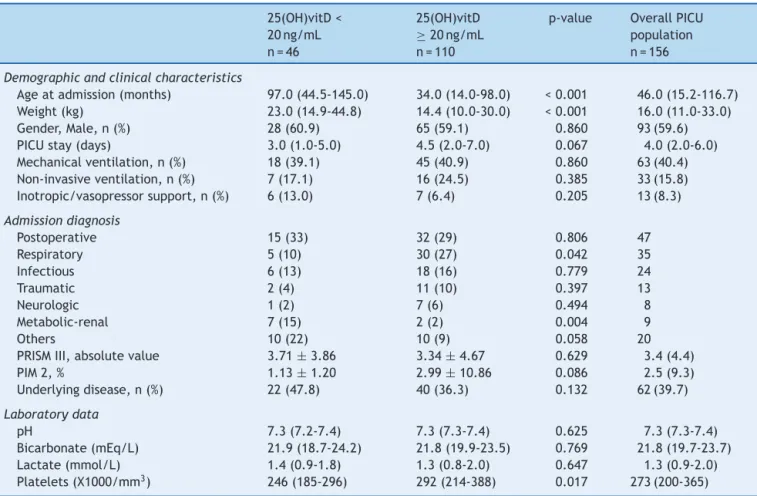
This study comprised 156 PICU patients. Baseline
demo-graphic,clinical,andlaboratorycharacteristicsofthePICU
patientsareshown in Table1. The main reasonsfor PICU
admissionwerepostoperativeandrespiratoryandinfectious disease.Seventy-sixpatients(48.7%) wereyoungerthan4 years.
HypovitaminosisDincidence
DemographicandvitaminDdatainthePICUpopulationand
healthy children arereported in Table 1. 25(OH)vitD
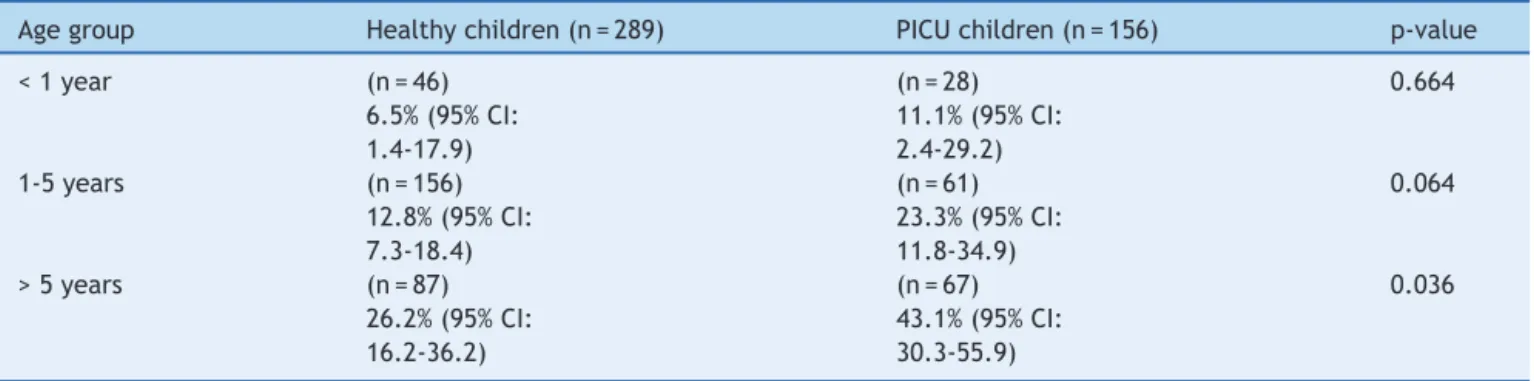
lev-elswerelowerandtheincidenceofhypovitaminosisDwas higher in the PICU population. Vitamin D values in criti-callyillchildren hadanegativecorrelation withpatient’s age(Spearman’scorrelationcoefficient:-0.421;p<0.001). Therefore, vitamin D deficiency was compared between healthyandPICUchildrenindifferentagegroups(Table2). The incidenceof vitamin D deficiency increased withage inboth groups of patients.PICU patients had acrude OR forhypovitaminosisDof2.26(CI95%:1.41-3.61).Theage, weight, and gender-adjusted OR was 1.83 (CI 95%: 1.10-3.06).
Median (p25-p75) 25(OH)vitD levels during the differ-ent seasons of the year in PICU patients were: spring, 30.1ng/mL (18.2-36.5); summer, 28.1ng/mL (20.5-33.3); fall,24.9ng/mL(19.6-39.0);andwinter,23.0ng/mL (15.4-38.0),p=0.761.
Table1 DemographicandvitaminDdatainhealthychildrenandinPICUpopulation(median,p25-p75).
DemographicandvitaminDdata Healthychildren(n=289) PICUpopulation(n=156) p-value
Ageatadmission(months) 36.0(24.0-84.0) 46.0(15.2-116.7) 0.678
Weight(kg) 16.5(12.0-28.0) 16.0(11.0-33.0) 0.120
Gender,male,n(%) 166(57.4) 93(59.6) 0.836
25(OH)vitD(ng/mL) 30.5(23.2-38.6) 26.0(19.2-35.8) 0.007
25(OH)vitD<20ng/mL(%) 15.6%(95%CI:12.2-20.0) 29.5%(95%CI:22.0-37.0) 0.01
CI,confidenceinterval;PICU,pediatricintensivecareunit;25(OH)vitD,25hydroxivitaminD.
Riskofmortality
Baselinedemographic,clinical,andlaboratory
characteris-ticsofthepatientswithhigherriskofmortality(groupA)vs.
therestofthesampleareshowninTable4.GroupApatients
wereyoungerandlighter.PICUstay,inotropicsupport,and needformechanicalventilationandnon-invasiveventilation werehigheringroupA.Postoperativediagnosisatadmission waslessfrequentingroupA,whereasrespiratorydiagnosis wasmorefrequent.PCT,MR-proADM,andCT-proET-1plasma levelsweresignificantlyhigherinpatientswithhigher pre-dictionofmortalityriskscores,whereasCRPand25OH(vitD) levelswerenodifferentbetweengroupsAandB.
Additionalevaluationusingamultivariatelogistic regres-sion analysis found an adjusted OR by age, season, and underlyingdiseaseof2.42(95%CI:0.86-6.84)forvitaminD deficiencyandpredictionofmortalityriskscores(p=0.09).
Discussion
This studydemonstrated that,in a sample of criticallyill
childrenfromthenorthofSpain,theprevalenceof
hypovi-taminosisDwashighatPICUadmission.Thepresentstudy
supports recent investigations14---16 showing that
hypovita-minosisDiscommonincriticallyillchildren.Itwasobserved that29.5% of thepresent PICU patientshad 25(OH)vitD< 20ng/mL,similartotherateof34.5%fromthestudyby Rip-peletal.14inacohortofcriticallyillAustralianchildren,and lowerthanthe40.1%and69%reportedbyMaddenetal.15 and by McNally et al.16 in North American and Canadian children,respectively.
The25(OH)vitD levels from the present PICU patients
were compared with the 25(OH)vitD levels that were
obtainedaspartofastudyonvitaminDstatusthatis cur-rentlyunderdevelopmentinapopulationofhealthychildren fromthe city of Oviedo(Asturias, Spain).The prevalence of vitamin D deficiency in Oviedo’s population of healthy children wassimilartothereportedprevalence of 18% in Mansbach’spopulation-basedstudyofhealthyNorth Ameri-canchildren,19 butlowerthanthepublishedprevalenceof vitaminDdeficiencyinNorthAmericanandAustralian ado-lescents,whichrangedfrom29%to68%.20,21Theexplanation for these differences is the age. A previously described inversecorrelationbetween25(OH)vitDlevelsandagewas confirmed by the present study. The median age of the presenthealthychildrencohortwas3years,muchyounger thantheadolescentsamplefromtheUnitedStatesand Aus-tralia.TheincidenceofvitaminDdeficiencywascompared betweenhealthyandPICUchildrenindifferentagegroups (Table 2). As expected,incidence of vitamin D deficiency increasedwithageinbothgroupofpatients.PICUpatients haddoubleincidenceofhypovitaminosisDinallagegroups, but thedifferenceswereclearly statisticallysignificant in the older age group, and were almost significant in the medium age group. The probable reasonis that the frag-mentation of thesample produced a smallsample size in the youngerage group.Regarding the seasonof the year, therewerenosignificantdifferencesin25(OH)vitDlevelsin thepresentstudy,althoughvaluestendedtobelowerinfall andwinter,whichagreewithpreviousstudiesperformedin theNorthofSpain18andinothercountries.20Inhealthy chil-dren,factorsconsistentlyassociatedwith25(OH)vitDlevels wereage,seasonoftheyear,anddietarycalciumintake.22
Table2 VitaminDdeficiency(25(OH)vitD<20ng/mL)inhealthyandPICUchildrenindifferentagegroups.
Agegroup Healthychildren(n=289) PICUchildren(n=156) p-value
<1year (n=46)
6.5%(95%CI:
1.4-17.9)
(n=28)
11.1%(95%CI:
2.4-29.2)
0.664
1-5years (n=156)
12.8%(95%CI:
7.3-18.4)
(n=61)
23.3%(95%CI:
11.8-34.9)
0.064
>5years (n=87)
26.2%(95%CI:
16.2-36.2)
(n=67)
43.1%(95%CI:
30.3-55.9)
0.036
Table3 Demographic,clinical,andlaboratorydataintheoverallPICUpopulationandinpatientswithandwithoutvitaminD deficiency.
25(OH)vitD<
20ng/mL
n=46
25(OH)vitD
≥20ng/mL
n=110
p-value OverallPICU
population
n=156
Demographicandclinicalcharacteristics
Ageatadmission(months) 97.0(44.5-145.0) 34.0(14.0-98.0) <0.001 46.0(15.2-116.7)
Weight(kg) 23.0(14.9-44.8) 14.4(10.0-30.0) <0.001 16.0(11.0-33.0)
Gender,Male,n(%) 28(60.9) 65(59.1) 0.860 93(59.6)
PICUstay(days) 3.0(1.0-5.0) 4.5(2.0-7.0) 0.067 4.0(2.0-6.0)
Mechanicalventilation,n(%) 18(39.1) 45(40.9) 0.860 63(40.4)
Non-invasiveventilation,n(%) 7(17.1) 16(24.5) 0.385 33(15.8)
Inotropic/vasopressorsupport,n(%) 6(13.0) 7(6.4) 0.205 13(8.3)
Admissiondiagnosis
Postoperative 15(33) 32(29) 0.806 47
Respiratory 5(10) 30(27) 0.042 35
Infectious 6(13) 18(16) 0.779 24
Traumatic 2(4) 11(10) 0.397 13
Neurologic 1(2) 7(6) 0.494 8
Metabolic-renal 7(15) 2(2) 0.004 9
Others 10(22) 10(9) 0.058 20
PRISMIII,absolutevalue 3.71±3.86 3.34±4.67 0.629 3.4(4.4)
PIM2,% 1.13±1.20 2.99±10.86 0.086 2.5(9.3)
Underlyingdisease,n(%) 22(47.8) 40(36.3) 0.132 62(39.7)
Laboratorydata
pH 7.3(7.2-7.4) 7.3(7.3-7.4) 0.625 7.3(7.3-7.4)
Bicarbonate(mEq/L) 21.9(18.7-24.2) 21.8(19.9-23.5) 0.769 21.8(19.7-23.7)
Lactate(mmol/L) 1.4(0.9-1.8) 1.3(0.8-2.0) 0.647 1.3(0.9-2.0)
Platelets(X1000/mm3) 246(185-296) 292(214-388) 0.017 273(200-365)
CI,confidenceinterval;PICU,pediatricintensivecareunit;PIM2,pediatricindexofmortality2;PRISMIII,pediatricriskofmortalityIII; 25(OH)vitD,25hydroxivitaminD.
PRISMIIIandPIM2areexpressedasmean±standarddeviation,admissiondiagnosisasabsolutevalueand%,andtheremainingvariables asmedian(P25-P75).
Unfortunately,dataregardingchildren’scalciumintakewas
notavailable.
Regardingadmissiondiagnosis,alowerrespiratory
diag-nosisratewasobservedinpatientswithvitaminDdeficiency.
Inthefewpublishedpediatricstudies,23anassociationwas
found betweenvitamin Ddeficiency andlung function,as wellaswiththeriskforupperrespiratorytractinfections. Ahighermetabolic-renaldiagnosisrateinpatientswith vita-minDdeficiencywasalsoobserved.Metabolic-renaldiseases cannegativelyinfluencethevitaminDmetabolicpathways, affecting25(OH)vitDlevels.17
Inthepresentsample,patientswithunderlyingdisease had lower levels of 25(OH)vitD. These patients are at a higherrisk forreducedvitamin Dlevelsthroughabnormal diets,alteredmetabolism,orreducedenvironmental expo-sure.
Riskofmortality
Vitamin D deficiency has recently been shown to be
associated with mortality in critically ill adults.11---13,24,25
Other recent investigations have not observed this
relationship.26,27 Considering that the present study was notsufficientlypoweredtoobservedifferencesinsurvival,
othersurrogatemarkersofPICUoutcomewereused,such asmortalityscores.InaccordancewithRippeletal.,14 no associationswere observedbetween vitamin D statusand predictedPRISM IIIand PIM2mortality. However,Madden etal.15 and McNally etal.16 demonstrated that 25(OH)vit DlevelsatadmissionwereinverselyassociatedwithPRISM III in North American children. Furthermore, duration of mechanicalor non-invasiveventilation andlength ofPICU stay did not show differences between low and normal 25(OH)vitDgroupsinthepresentsample,inagreementwith the data observed by Rippel et al.14 in Australian chil-dren. However, McNally et al.16 found an association of vitaminDdeficiencywithlongerlengthofstay.Geographic andethnicdifferences,aswellasdifferentcausesofPICU admissions,couldexplainthesimilarresultsinthepresent studyandintheAustralianstudy,andthedifferenceswith bothNorthAmericanstudies.Variationsinpatientresponses to acute stress and critical illness may depend on the degree of vitamin D insufficiency and thepatient’s tissue requirements.17
Table4 Demographic,clinical,laboratorydata,andmarkerlevelsinpatientswithhighervs.lowerpredictionofriskmortality scores.
GroupA(PRISMIII
orPIM2>p75)
(n=33)
GroupB(PRISMIII
andPIM2≤p75)
(n=123)
p-value
Demographicandclinicalcharacteristics
Ageatadmission(months) 21.0(8.2-56.0) 58.5(23.2-123.5) 0.007
Weight(kg) 11.1(8.8-20.2) 17.2(12.0-35.4) 0.012
Gender,male,n(%) 22(66.7) 71(57.7) 0.426
PICUstay(days) 5.0(3,0-9.5) 3.0(2.0-6.0) 0.008
Mechanicalventilation,n(%) 25(75.8) 38(30.9) <0.001
Non-invasiveventilation,n(%) 15(45.5) 18(22.4) 0.001
Inotropic/vasopressorsupport,n(%) 9(27.3) 4(3.3) <0.001
Admissiondiagnosis
Postoperative 1(3) 46(37) <0.001
Respiratory 12(36) 23(19) 0.054
Infectious 6(18) 18(15) 0.818
Traumatic 3(9) 10(8) 0.859
Neurologic 3(9) 5(4) 0.473
Metabolic-renal 4(12) 5(4) 0.179
Others 4(12) 16(13) 0.875
PRISMIII,absolutevalue 8.0±6.7 2.2±2.3 <0.001
PIM2,% 8.6±18.4 0.68±0.46 0.019
Laboratorydata
pH 7.3(7.2-7.4) 7.4(7.3-7.4) 0.012
Bicarbonate(mEq/L) 21.8(16.6-24.1) 21.8(19.9-23.7) 0.898
Lactate(mmol/L) 1.4(0.97-2.1) 1.2(0.80-2.0) 0.319
Platelets(x1,000/mm3) 244(163-409) 281(214-364) 0.277
Markers
CRP(mg/dL) 2.58(0.50-14.9) 1.05(0.10-8.4) 0.123
PCT(ng/mL) 1.4(0.3-10.4) 0.18(0.07-1.3) <0.001
MR-proADM(nmol/L) 0.79(0.49-1.5) 0.46(0.33-0.60) <0.001
CT-proET-1(pmol/L) 80.7(57.6-115.9) 50.7(35.8-75.7) <0.001
25(OH)vitD(ng/mL) 25.40(15.5-36.0) 26.6(19.3-35.5) 0.800
25(OH)vitD<20ng/mL,n(%) 11(33.3%) 37(30.1%) 0.832
CRP,C-reactiveprotein;CT-proET-1,carboxy-terminalpro-endothelin-1;MR-proADM,mid-regionalpro-adrenomedullin;PCT, procalci-tonin;PICU,pediatricintensivecareunits;PIM2,pediatricindexofmortality2;PRISMIII,pediatricriskofmortalityIII;25(OH)vitD,25 hydroxivitaminD.
PRISMIIIandPIM2 wereexpressedasmean ±standarddeviation, admissiondiagnosisasabsolutevalue;theothervariableswere expressedasmedian(P75-P25).
By regulating the expression of more than 200
genes, including those influencing cell growth,
1,25-dihydroxyvitamin D3 plays an important role in the
proliferation, maturation, anddeath of cells. The
identi-ficationofmodifiable riskfactorscouldhelptoguidenew
preventativeortherapeuticstrategiesforpediatriccritical
illness.However,recentevidence17suggeststhatthe
inter-pretationofvitaminDstatusbasedon25(OH)vitDlevelsin acuteillnessshouldbeperformed withcaution.Significant variationin25(OH)vitDlevelsmayoccurfromhourtohour inacutely illpatients,andsinglepointassessmentmaybe inaccurateincertaincases.Moreover,vitaminDdeficiency wouldnotonlybedependentontheseverityofvitaminD depletion,butwouldalsoberelatedtotissuerequirement.28 Thereforenewstudiesarenecessaryinordertodetermine reliablemarkersofvitaminDstatusintheacutecare set-ting, as well as strategies to confirm whether vitamin D
supplementationisusefulforhypovitaminosisDincritically illchildren.
The present study has limitations. Firstly,
parathy-roid hormone (PTH) was not measured. The diagnosis
of vitamin D deficiency usually requires the association
of serum 25(OH)vitD levels lower than 20ng/mL and
elevated serum PTH concentrations.29 Secondly, the rel-atively small sample size and the low mortality limited the capacity to analyze specific subgroup of patients. Thirdly, the original study was not intended to esti-mate the prevalence of vitamin D deficiency; therefore, a specific questionnaire about dietary habits, vitamin D
supplementation, or sun exposure was not performed.
Inconclusion,inapopulationofchildrenfromtheNorth of Spain, hypovitaminosis D incidence was high at PICU admission. To the authors’ knowledge, this is the first prospectivestudycomparing25(OH)vitDlevelsincritically illpatientswithhealthychildrenpopulationfromthesame area.HypovitaminosisDwasnotassociatedwithhigher pre-dictionofmortalityriskscores,lengthofstay,andinotropic orrespiratorysupport.Furtherstudiesarerequiredto iden-tifyreliablemarkersof vitaminDstatusinthe acutecare setting,aswellasstrategiestoconfirmwhethervitaminD supplementationcouldbeusefulincriticallyillchildrenwith hypovitaminosisD.
Funding
This study waspartly fundedby agrantfrom‘‘Fundación
ErnestoSánchezVillares’’.PabloMartínez-Camblorwas
sup-portedbytheGrantMTM2011-23204oftheSpanishMinistry
ofScienceandInnovation(FEDERsupportincluded).
Conflicts
of
interest
Corsino Rey had received speakerhonoraria from Brahms
Companytoattendmeetingsrelatedtosepsisbiomarkers.
Theremainingauthorsdeclarenoconflictsofinterest.
Fun-daciónErnestoSánchezVillares,SpanishMinistryofScience
andInnovation,andBrahmsCompanyhadnoparticipationin
thedevelopmentofthemanuscript,includingstudydesign,
collection analysis, interpretation of data, writing of the
report, northe decision to submitthe paper for
publica-tion.
Acknowledgements
Theauthorswouldliketothankthechildrenandparentswho
participatedinthisstudy.Theauthorsalsoacknowledgethe
assistanceofthePICUmedicalandnursingstaffofHospital
UniversitarioCentraldeAsturias.
References
1.PearceSH,CheethamTD.Diagnosisandmanagementofvitamin Ddeficiency.BMJ.2010;340:b5664.
2.FordES,ZhaoG, Tsai J, LiC. VitaminD and all-cause mor-talityamongadultsinUSA:findingsfromtheNationalHealth andNutritionExaminationSurveyLinkedMortalityStudy.IntJ Epidemiol.2011;40:998---1005.
3.Adams JS, Ren S, Liu PT, Chun RF, Lagishetty V, Gom-bart AF, et al. Vitamin D-directed rheostatic regulation of monocyte antibacterial responses. J Immunol. 2009;182: 4289---95.
4.PilzS,TomaschitzA.RoleofvitaminDinarterialhypertension. ExpertRevCardiovascTher.2010;8:1599---608.
5.MitriJ,MuraruMD,PittasAG.VitaminDandtype2diabetes:a systematicreview.EurJClinNutr.2011;65:1005---15.
6.MansonJE, MayneST, Clinton SK. VitaminD and prevention of cancer–ready for prime time? N Engl J Med. 2011;364: 1385---7.
7.KriegelMA,MansonJE,CostenbaderKH.DoesvitaminDaffect risk of developing autoimmune disease? asystematic review. SeminArthritisRheum.2011;40:512---31.e8.
8.Searing DA, Zhang Y, Murphy JR, HaukPJ, Goleva E, Leung DY.DecreasedserumvitaminDlevelsinchildrenwithasthma areassociatedwithincreasedcorticosteroiduse.JAllergyClin Immunol.2010;125:995---1000.
9.MisraM,PacaudD,PetrykA,Collett-SolbergPF,KappyM.Drug and TherapeuticsCommittee oftheLawsonWilkinsPediatric EndocrineSocietyVitaminDdeficiencyinchildrenandits man-agement:reviewofcurrentknowledgeandrecommendations. Pediatrics.2008;122:398---417.
10.HollisBW,WagnerCL,DreznerMK,BinkleyNC.Circulating vita-minD3and25-hydroxyvitaminDinhumans:animportanttoolto defineadequatenutritionalvitaminDstatus.JSteroidBiochem MolBiol.2007;103:631---4.
11.VenkatramS, ChilimuriS,AdrishM,Salako A, PatelM, Diaz-FuentesG.VitaminDdeficiencyisassociatedwithmortalityin themedicalintensivecareunit.CritCare.2011;15:R292.
12.Braun A, Chang D,Mahadevappa K, GibbonsFK, Liu Y, Gio-vannucciE,etal.Associationoflowserum25-hydroxyvitamin D levels and mortality in the critically ill. Crit Care Med. 2011;39:671---7.
13.BraunAB,GibbonsFK,LitonjuaAA,GiovannucciE,Christopher KB. Low serum 25-hydroxyvitamin D at critical care initia-tion is associated with increased mortality. Crit Care Med. 2012;40:63---72.
14.RippelC,SouthM,ButtWW,ShekerdemianLS.VitaminDstatus incriticallyillchildren.IntensiveCareMed.2012;38:2055---62.
15.MaddenK,FeldmanHA,SmithEM,GordonCM,KeislingSM, Sul-livanRM,etal.VitaminDdeficiencyincriticallyillchildren. Pediatrics.2012;130:421---8.
16.McNallyJD,MenonK,ChakrabortyP,FisherL,WilliamsKA, Al-Dirbashi OY, et al. The association of vitamin D status with pediatriccriticalillness.Pediatrics.2012;130:429---36.
17.Quraishi SA, Camargo Jr CA. Vitamin D in acute stress and critical illness. Curr Opin Clin Nutr Metab Care. 2012;15: 625---34.
18.Alonso A, Rodríguez J, Carvajal I, PrietoMA, Rodríguez RM, Pérez AM, et al. Prophylactic vitamin D in healthy infants: assessingtheneed.Metabolism.2011;60:1719---25.
19.Mansbach JM, Ginde AA, Camargo Jr CA. Serum 25-hydroxyvitamin D levels among US children aged 1 to 11 years:dochildrenneedmorevitaminD?Pediatrics.2009;124: 1404---10.
20.Dong Y, Pollock N, Stallmann-Jorgensen IS, Gutin B, Lan L, ChenTC,etal.Low25-hydroxyvitaminDlevelsinadolescents: race,season,adiposity,physicalactivity,andfitness.Pediatrics. 2010;125:1104---11.
21.RovnerAJ,O’BrienKO.HypovitaminosisDamonghealthy chil-drenintheUnitedStates:areviewofthecurrentevidence. ArchPediatrAdolescMed.2008;162:513---9.
22.Gordon CM, Feldman HA, Sinclair L, Williams AL, Kleinman PK,Perez-RosselloJ,etal.PrevalenceofvitaminDdeficiency amonghealthyinfantsandtoddlers.ArchPediatrAdolescMed. 2008;162:505---12.
23.WeissST.Asthmainearlylife:isthehygienehypothesiscorrect? JPediatr(RioJ).2008;84:475---6.
24.LeeP,EismanJA,CenterJR.VitaminDdeficiencyincritically illpatients.NEnglJMed.2009;360:1912---4.
25.LeeP,NairP,EismanJA,CenterJR.VitaminDdeficiencyinthe intensivecare unit:aninvisibleaccomplice tomorbidityand mortality?IntensiveCareMed.2009;35:2028---32.
26.LucidarmeO, Messai E,Mazzoni T,Arcade M,duCheyronD. IncidenceandriskfactorsofvitaminDdeficiencyincriticallyill patients:resultsfromaprospectiveobservationalstudy. Inten-siveCareMed.2010;36:1609---11.
28.Venkatesh B,Davidson B,Robinson K,Pascoe R,Appleton C, JonesM.DorandomestimationsofvitaminD3andparathyroid hormonereflectthe24-hprofileinthecriticallyill?Intensive CareMed.2012;38:177---9.