REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologia www.sba.com.brSCIENTIFIC
ARTICLE
Comparative
study
between
benzydamine
hydrochloride
gel,
lidocaine
5%
gel
and
lidocaine
10%
spray
on
endotracheal
tube
cuff
as
regards
postoperative
sore
throat
Nashwa
Abdallah
Mekhemar
a,∗,
Ahmed
Samy
El-agwany
b,
Wafaa
Kamel
Radi
a,
Sherif
Mohammed
El-Hady
aaDepartmentofAnaesthesiaandSurgicalIntensiveCare,FacultyofMedicine,UniversityofAlexandria,Alexandria,Egypt
bDepartmentofObstetricsandGynaecology,FacultyofMedicine,UniversityofAlexandria,Alexandria,Egypt
Received18June2014;accepted10September2014 Availableonline26November2014
KEYWORDS Sorethroat; Benzydamin; Lidocaine; Endotrachealtube
Abstract Postoperativesorethroatisacommoncomplicationafterendotrachealintubation. Aftertrachealintubation,theincidenceofsorethroatvariesfrom14.4%to50%.Theaimofthe studywastocomparebetweenbenzydaminehydrochloridegel,lidocaine5%gelandlidocaine 10%spray ontheendotracheal tubecuffasregards postoperative sorethroat.The present studywascarriedouton124patientsadmittedtoAlexandriauniversityhospitalsforlumbar fixationsurgeryrequiringgeneralanesthesia.Patientswererandomlyallocatedinto4groups. Benzydaminehydrochloride gel,5% lidocainehydrochloridegel,10%lidocainehydrochloride spray,ornormalsalinewereappliedonendotrachealtubecuffsbeforeendotracheal intuba-tion.Thepatientswereexaminedfor sorethroat(none,mild,moderate,orsevere)at0,1, 6,12,and24hafterextubation.Theresultswerecollected,analyzedandpresentedintable andfigure.Thehighestincidenceofpostoperativesorethroat occurredat6hafter extuba-tioninallgroups.Therewasasignificantlylowerincidenceofpostoperativesorethroatinthe benzydaminegroupthan5%lidocainegel,10%lidocainespray,andnormalsalinegroups.The benzydaminegrouphadsignificantlydecreasedseverityofpostoperativesorethroatcompared withthe10%lidocaine,5%lidocaine,andnormalsalinegroupsatobservationtimepoint. Com-paredwiththe5%lidocainethe10%lidocainegrouphadsignificantlyincreasedincidenceand severityofpostoperativesorethroatafterextubation.Comparedwithnormalsalinethe10% lidocainegrouphadincreasedincidenceofpostoperativesorethroat.Therewereno signifi-cantdifferencesamonggroupsinlocalorsystemicsideeffects.Soinconclusion,benzydamine hydrochloridegelontheendotrachealtubecuffisasimpleandeffectivemethodtoreducethe incidenceandseverityofpostoperativesorethroat.Applicationof10%lidocainesprayshould beavoidedbecauseofworseningofpostoperativesorethroatwhereincidenceincreasedbut
∗Correspondingauthor.
E-mail:Nashwaabdallah287@gmail.com(N.A.Mekhemar). http://dx.doi.org/10.1016/j.bjane.2014.09.007
nottheseverityinrelationto5%lidocainegel.Applying5%lidocaineontheendotrachealtube cuffdoesnotpreventpostoperativesorethroatbutitsapplicationisbetterthanlidocaine10% sprayorsaline.
© 2014SociedadeBrasileirade Anestesiologia.Publishedby ElsevierEditoraLtda.Allrights reserved.
PALAVRAS-CHAVE Dordegarganta; Benzidamina; Lidocaína; Tuboendotraqueal
Estudocomparativoentrecloridratodebenzidaminaemgel,lidocaínaa5%emgele lidocaínaa10%emspraynobalonetedotuboendotraquealemrelac¸ãoàdorde gargantapós-operatória
Resumo Adordegargantapós-operatória(DGPO)éumacomplicac¸ãocomumapósaintubac¸ão traqueal.Emseguidaaesseprocedimento,aincidênciadedordegargantavariade14,4a50%. Oobjetivodoestudofoicompararosefeitosdaaplicac¸ãodecloridratodebenzidaminaem gel,lidocaínaa5%emgel,elidocaínaa10%emspraynobalonetedotuboendotraqueal,no que dizrespeito àdordegargantapós-operatória. Opresenteestudofoi realizado em124 pacientesinternadosemhospitaisuniversitáriosdeAlexandriaparacirurgiadefixac¸ãolombar necessitandodeanestesiageral.Ospacientesforamaleatoriamentealocadosemquatrogrupos. Procedeu-seàaplicac¸ãodecloridratodebenzidaminaemgel,cloridratodelidocaínaa5%em gel,cloridratodelidocaína a10%emspray,ousalinanormalnosbalonetesdoTETantesda intubac¸ãoendotraqueal.Ospacientesforamexaminadosparadordegarganta(nenhuma,leve, moderadaouintensa)a0,1,6,12e24horasapósaextubac¸ão.Osresultadosforamcoletados, analisadoseapresentadosemtabelasefiguras.AmaiorincidênciadeDGPOocorreu6horas apósaextubac¸ãoemtodososgrupos.HouveincidênciasignificativamentemenordeDGPOno grupo debenzidamina versusgrupos delidocaína a5%em gel,lidocaína a10%em spray,e salinanormal.Ogrupotratadocombenzidaminaexibiureduc¸ãosignificativanaintensidade daDGPO,emcomparac¸ãocomosgruposdelidocaína a10%,lidocaínaa5%esalinanormal nopontonotempodeobservac¸ão.Emcomparac¸ãocomlidocaínaa5%,ogrupotratadocom lidocaínaa10%exibiuincidênciaeintensidadesignificativamenteaumentadasnaDGPOapós aextubac¸ão.Emcomparac¸ãocomsalinanormal,ogrupotratadocomlidocaínaa10%exibiu maiorincidênciadeDGPO.Nãoforamobservadasdiferenc¸assignificativasentregruposquantoa efeitoscolateraislocaisousistêmicos.Assim,emconclusão,ousodecloridratodebenzidamina emgelnobalonetedoTETéummétodosimpleseeficazparareduziraincidênciaegravidade daDGPO.Deve-seevitaraaplicac¸ãodelidocaínaa10%emspray,devidoaoagravamentoda DGPO,vistoterocorridoaumentonaincidência,masnãonaseveridade,emrelac¸ãoàlidocaína a5%emgel.Aaplicac¸ãodelidocaínaa5%nobalonetedoTETnãoimpedeaocorrênciada DGPO,masasuaaplicac¸ãooferecemelhoresresultadosdoquelidocaínaa10%emspray,ou soluc¸ãosalina.
©2014SociedadeBrasileira deAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Sorethroatisacommonpostoperativecomplaint.After tra-cheal intubation,theincidenceof sorethroatvaries from 14.4%to50%andafterlaryngealmaskinsertionfrom5.8% to34%.Thehighestincidenceofsorethroatandother air-wayrelatedsymptomstendstooccurinpatientswhohave undergonetrachealintubation.1
Complicationsoftrachealintubationcanbeclassifiedas immediate, early andlate.It iswell recognizedthat pro-longedintubationcanhaveseriousconsequences,butitis lesswellrecognizedthatuneventfulintubationforroutine surgicalprocedurescanalsocausepathologicalchangesthat may provide an organic basis for patients’ postoperative throatsymptoms.2
Several pharmacologicalmethods have been suggested toreducepostoperativesorethroat(POST)including inhal-ingbeclomethasone; applyinglidocainesprayor lidocaine geltothe endotrachealtube (ETT);administeringaspirin, ketamine,orbenzydaminehydrochloride.3
Local anesthetic drugs act by producing a reversible blocktothetransmissionofperipheralnerveimpulses. Lido-caineisusedcommonlyforinfiltrationinconcentrationsof 0.5---1.0%and for peripheral nerveblocksifan intermedi-ateduration is required.Lidocaine 2---4% is usedby many anesthetistsasatopicalsolutionforanesthesiaoftheupper airwaybeforeawakeintubation.3
with a gargle containing a drug such as benzydamine hydrochloride,whichisapprovedforthesymptomatic treat-mentofacutesorethroatpain.4
Benzydamine hydrochloride is a topical non-steroidal anti-inflammatory agent that also has local anesthetic activity.5IthasanalkalinepH,whichmeansthatitbecomes concentratedin inflamed tissueandhas minimalsystemic absorption.5
Ithasbeenreportedthatmoderatetoseveresorethroat maybe resolved withgargling benzamine hydrochloride.6 Preventivetopicalbenzaminehydrochlorideappliedtothe oropharyngeal cavity before endotracheal intubation or before endotracheal intubation and continuously for 48h postoperativelyhasbeenreportedtodecreasetheincidence andseverityofPOSTafterETTinsertionandlaryngealmask airwayinsertion.6
Aim
of
the
work
Theaimofthestudywastocomparebetweenbenzydamine hydrochloridegel,lidocaine5%gelandlidocaine10%spray ontheETTcuffasregardsPOST.
Methods
Thepresentstudywascarriedouton124patientsadmitted toAlexandriauniversityhospitalsundergoinglumbarfixation surgeryrequiringgeneralanesthesia.
Inclusioncriteria
PatientsofAmericanSocietyofAnesthesiologists(ASA) phys-icalstatusIorII2,Lumbarfixationsurgeryrequiringgeneral anesthesia.
Exclusioncriteria
Historyofpreoperativesorethroat,Morethanoneattempt at intubation, Mallampati grade more than 2, Known allergies to benzydamine hydrochloride or lidocaine and smoking.
Afterapprovalofthelocalethicalcommitteeandhaving aninformedwrittenconsentfromeverypatient,theywere randomlycategorized;byclosedenvelopemethod;intofour groups(31each):
GroupI:wheretheETTcuffswerelubricatedwith benzy-daminehydrochloridegel.
Group II:wheretheETTcuffs werelubricatedwith lido-cainehydrochloride5%gel.
GroupIII:wheretheETTcuffsweresprayedwithlidocaine hydrochloride10%spray.
GroupIV:wherethecuffsweresprayedwithnormalsaline asacontrolgroup.
Anesthesiawasinducedwithfentanyl2---3microgram/kg and propofol 2---2.5mg/kg. Tracheal intubation was facil-itated by rocuronium 0.6mg/kg, and the trachea was intubatedwithalowpressurecuffedsterilepolyvinyl chlo-rideETT.The cuffwasinflated withair andcuffpressure
wasmaintainedat20cmH2Ousingcuffpressuregauge.We
keptthecuffspressureuniformforthe4groupsusingcuff pressuregauge.Anesthesiawasmaintainedusingisoflurane MAC1.2%andincrementsoffentanylandrocuronium.
Monitoringconsistedof5-leadelectrocardiography, non-invasive arterial blood pressure,pulseoximetry, nasopha-ryngeal temperature,andendtidalcarbon dioxide,which waskeptbetween30and35mmHg.Attheendofsurgery, the muscle relaxation was reversed by a combination of neostigmine0.05mg/kgandatropine0.02mg/kg.After gen-tlesuctioningoforalsecretionsbya12Fsuctioncatheter, patients were extubated and transferred to the post-anesthesiacareunit.
Thefollowingwererecorded:
--- Age,sex,weightandheightofthepatients. --- Durationofsurgery.
--- Totalfentanylconsumption. --- Vitalsigns.
--- Postoperativeanalgesia.
--- Potentialsideeffectsassociatedwithtrachealintubation.
POSTwasgradedat (0h)afterfullrecoveryand there-after at 1, 6, 12 and 24h after extubation, ona 4-point scale (0---3)asshown below7:0 ---Nosorethroat; 1---Mild sore throat(complainsof sorethroatonly onasking);2 ---Moderatesorethroat(complainsofsore throatonhis/her own);3---Severesorethroat(changeofvoiceorhoarseness, associatedwiththroatpain).
Results
The age in groupIranged from35.0 to60.0years witha meanof48.74±6.21years;ingroupII;itrangedfrom39.0 to61yearswithameanof49.55±6.81years;ingroupIIIit rangedfrom35.0to60.0yearswithameanof48.39±6.49 yearsandingroupIVitrangedfrom40.0to61.0yearswith ameanof49.84±6.08years.Therewasnosignificant dif-ferencebetweenmeanagesinthefourgroups.
The sex of patients in group I was as follows: 67.7% malesand32.3%females;ingroupII:58.1%malesand41.9% females; in groupIII: 61.3% males and38.7% females and ingroupIV:58.1%malesand41.9%females.Therewasno significantdifferencebetweengroupsasregardssex.
The weightof patients in group I ranged from82.0 to 130.0kgwithameanof97.77±10.57kg;ingroupIIranged from 82.0 to 120.0kg with a mean of 97.32±9.36kg; in group III ranged from 70.0 to 120.0kg with a mean of 93.90±11.30kg; while in group IV ranged from 79.0 to 120.0kgwithameanof95.32±8.87kg.Therewasno sig-nificantdifferencebetweengroupsasregardsweight.
Theheight ofpatients in groupIranged from160.0to 189.0cmwithameanof173.13±8.10cm;ingroupIIranged from 160.0to 184.0cm witha mean of 171.94±7.51cm; ingroupIII rangedfrom160.0to183.0cmwithameanof 172.19±6.95cm;while in group IVranged from163.0 to 185.0cmwith a mean of 173.26±6.56cm. There wasno significantdifferencebetweengroupsasregardsheight.
76.29±8.94min;ingroupIIIrangedfrom65.0to110.0min withameanof74.65±8.85min; whilein groupIVranged from 70.0 to 100.0min witha mean of 80.65±9.64min. There was no significant difference between groups as regardsduration.
The totalfentanyldoseingroupIrangedfrom200.0to 350.0gwithameanof245.81±39.73g;ingroupIIranged
from200.0 to300.0gwithamean of245.81±41.78g;
ingroup IIIrangedfrom200.0to300.0gwithameanof
237.10±34.08g;while in groupIVranged from200.0to
350.0g witha meanof 251.61±45.61g.There wasno
significantdifferencebetweengroups.
The heart rateof patients ingroup Iranged from70.0 to80.0beatsperminutewithameanof74.03±4.17beat per minute; in group II ranged from 68.0 to 83.0 beats perminutewithameanof74.90±5.26beatsperminute; in group III ranged from 70.0 to 78.0 beat per minute with a mean of 74.06±3.24 beats per minute; while in group IVranged from70.0 to80.0 beatsper minute with a mean of 76.23±3.29 beats per minute. There was no significant difference between groups as regards heart rate.
ThesystolicbloodpressureingroupIrangedfrom100.0 to 120.0mmHg with a mean of 110.97±8.31mmHg; in group II ranged from 100.0 to 120.0mmHg with a mean of 115.16±5.70mmHg;in group III ranged from 100.0 to 120.0mmHgwitha meanof111.29±7.18mmHg;whilein group IV ranged from 100.0 to 120.0mmHg with a mean of110.32±8.36mmHg.Therewasnosignificantdifference betweengroupsasregardssystolicbloodpressure.
ThediastolicbloodpressureofpatientsingroupIranged from70.0to80.0mmHgwithameanof73.87±4.95mmHg; in group II ranged from 60.0 to 80.0mmHg with a mean of 73.55±6.61mmHg; in group III ranged from 70.0 to 90.0mmHg with a mean of 75.81±5.64mmHg; while in group IV ranged from 70.0 to 84.0mmHg with a mean of76.94±4.81mmHg.Therewasnosignificantdifference betweengroupsasregardsdiastolicbloodpressure.
The temperatureingroupIranged from35.80to36.50 degrees with a mean of 36.15±0.27 degrees; in group II ranged from 35.80 to 36.50 degrees with a mean of 36.18±0.27degrees;ingroupIIIrangedfrom35.90to36.50 degreeswithameanof36.18±0.21degrees;whileingroup IV ranged from 35.70 to 36.50 degrees with a mean of 36.24±0.26 degrees. There was no significant difference betweengroupsasregardstemperature.
The SpO2 of patients in group I ranged from 98.0
to 100.0mm Hg with a mean of 99.03±0.87mmHg; in group II ranged from 98.0 to 100.0mmHg with a mean of 98.97±0.71mmHg; in group III ranged from 98.0 to 100.0mmHg with a mean of 99.19±0.79mmHg; while in group IV ranged from 98.0 to 100.0mmHg with a mean of98.90±0.83mmHg.Therewasnosignificantdifference betweengroupsasregardsSpO2.
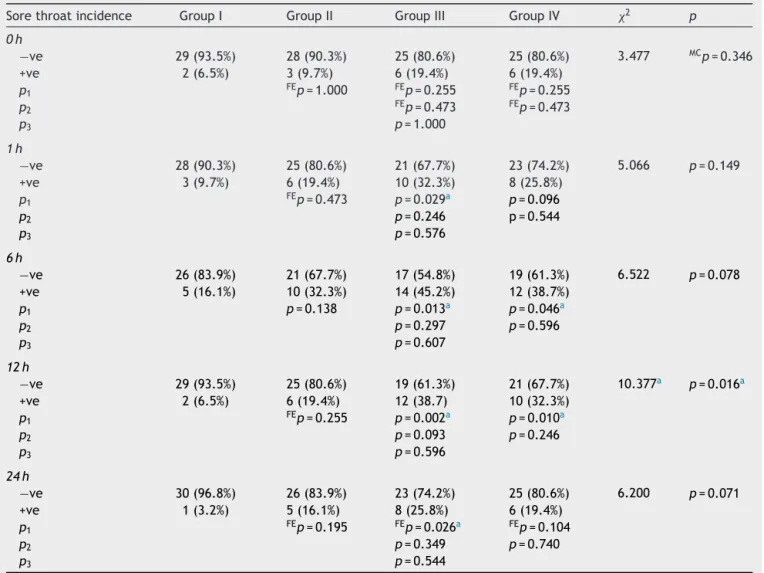
ThesorethroatincidenceingroupIpatientswasas fol-lows:at0h6.5%+ve,at1h9.7%+ve,at6h16.1%+ve,at 12h6.5%+veandat24h3.2%+ve.Allcasesareofgrade1 severity.ThesorethroatincidenceingroupIIpatientswas asfollows:at0h9.7%+ve,at1h19.4%+ve,at6h32.3%+ve, at12h19.4%+veandat24h16.1%+ve.Casesaregrade1 severityexceptat6and12hwhereallcaseswereofgrade 2 severity. The sore throatincidence in groupIII patients
wasasfollows:at 0h 19.4% +ve,at 1h 32.3% +ve,at 6h 45.2%+ve,at12h38.7%+veandat 24h 25.8%+ve.Cases aregrade1severity exceptat 6and 12h where allcases wereofgrade2severity.Thesorethroatincidenceingroup IVpatientswasasfollows:at0h19.4%+ve,at1h25.8%+ve, at6h 38.7%+ve,at12h 32.3%+veandat24h19.4%+ve. Casesaregrade 1severityat 0h andat 1,6, 12and24h wereofgrade2severity.
There wasnosignificant difference betweengroups as regards sore throat incidence at 0h although the rela-tion between groups was groups I<II<III=IV. There was significant difference between groups I and III at 1h but non-significantdifferencebetweentheothersalthoughthe relationbetweengroupswasgroupsII<III>IV.Therewas sig-nificant differencebetween groups I, III andIV at 6,12h wheretherewerelesscasesingroupIbutnon-significant dif-ferencebetweentheothersalthoughtherelationbetween groupswasgroupsII<III>IV.ThehighestincidenceofPOST occurredat6hafterextubationinallgroups.
Therewasnosignificantdifferencebetweengroupsat0h whereallthecaseswereofgrade1.Therewassignificant differenceat1hbetweenthefirstthreegroupsandgroup IVwhereallcasesinthisgroupwereofgrade2andinthe otherswereofgrade1.Therewassignificantdifferenceat 6,12hbetweenthegroupswhereallcasesingroupIwere ofgrade 1 and inthe others were ofgrade 2. There was significantdifferencebetweengroupsat24hwhereallcases ingroupIVwereofgrade2andintheotherswereofgrade 1.
ThePethidinedoseingroupIrangedfrom40.0to60.0mg witha mean of 48.87±6.02mg; in group II ranged from 40.0to60.0mgwithameanof48.23±5.71mg;ingroupIII rangedfrom35.0to60.0mgwithameanof47.26±6.56mg; while in group IV ranged from 40.0 to 60.0mg with a meanof 47.10±4.79mg. There wasno significant differ-encebetweengroupsasregardsPethidineaspostoperative analgesia.
TheadverseeffectsingroupIpatientswereasfollows: 19.4%nauseaandvomiting;9.7% cough;29.5% hoarseness and58.1%dry mouth. Group II:30% nauseaandvomiting; 20%cough;50%hoarsenessand70%drymouth.GroupIII:32% nauseaandvomiting; 25%cough; 55% hoarseness and72% drymouth.GroupIV:33%nauseaandvomiting;26%cough; 57%hoarsenessand73%drymouth.Therewasnosignificant differencebetweengroupsasregardsadverseeffects.
Statisticalanalysisofthedata
Data were fed to the computer and analyzed using IBM SPSSsoftwarepackageversion20.0.8,9Comparisonbetween differentgroupsregardingcategoricalvariableswastested usingChi-squaretest.Whenmorethan20%ofthecellshave expectedcountlessthan 5,correction for chi-squarewas conductedusingFisher’sExacttestor MonteCarlo correc-tion.
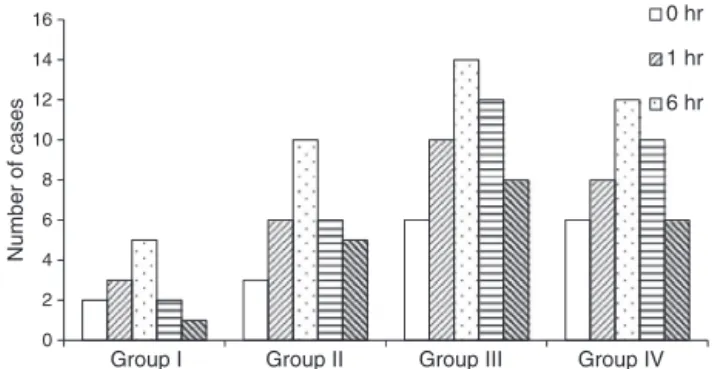
0 2 4 6 8 10 12 14 16 Group IV Group III Group II Group I
Number of cases
0 hr
1 hr
6 hr
Figure1 Comparisonbetween thedifferentstudiedgroups accordingtosorethroatincidenceatintervals0,1,6,12and 24h.
Fornormallydistributeddata,comparisonbetween dif-ferentgroupswereanalyzedusingF-test(ANOVA)andPost Hoctest(Scheffe)forpairwisecomparison,whilefor abnor-mally distributed data, Kruskal---Wallis test was used to comparebetween different groups and PostHoc test was assessedusingMann---WhitneyTest.
Significancetestresultsarequotedastwo-tailed proba-bilities.Significanceoftheobtainedresultswasjudgedat the5%level.
Discussion
Accordingtotheresultsofthisstudy,thehighestincidence of POST occurred at the sixth hour after extubation, but notthefirst hour.Sore throatat thefirst fewhoursafter extubationmight be masked by residualanalgesic effects aftergeneralanesthesiaorpostoperativepaincontrol.
There wasnosignificant difference between groups as regardssore throatincidenceat0h.Therewassignificant differencebetweengroupIandIIIat1h.Therewas signifi-cantdifferencebetweengroupsI,IIIandIVat6,12h.The highestincidenceofPOSToccurredat6hafterextubation inallgroups(Fig.1andTable1).
Thereweremorecaseswithseveredegreeofsorethroat inourstudyingroupIIIthangroupIIintheotheronethat mightbeattributedtooursmallersamplesize.Also,there weremorecaseswithseveredegreeofsorethroatingroup IIIinourstudythangroupII intheother onewhichmight berelatedtooursmallersamplesizeanddifferentmodeof applicationoflidocainewithmucosairritationwithethanol andothers.10,11
There wasnosignificant difference between groups as regardsseverityat0hwhereallthecaseswereofgrade1. Therewassignificant differenceat 1,6,12,24hbetween groups where there were less severity with benzydamine andhighestseveritywithlidocaine10%.Otherworkers find-ings showed significant difference between benzydamine andother3groupsinallthestudiedhours.Therewas sig-nificantbetweenlidocaine10%andlidocaine5%.Also,there wassignificantdifferencebetweenlidocaine10%andsaline. TherewasmorecaseswithseveregradeinourgroupsIIIand IVinrelationtotheotherstudywhere.10,11
Thesideeffectsoftopicaluseofbenzydamine hydrochlo-rideincludelocalnumbnessorburning,stingingsensation, nauseaorvomiting, cough,dry mouth, throatdiscomfort,
drowsiness, and headache, which may be evident before inductionofanesthesia.Toavoidtheseadverseeffects,we appliedbenzydaminehydrochlorideontheETTcuffinstead ofperioperativetopicalapplicationtotheoral pharyngeal cavity.Wefoundthatthismaneuverprovidedexcellent pre-ventionofPOSTandreduceditsincidencefromsalinegroup or10%lidocainesprayby50%.12
Therefore, the application of benzydamine hydrochlo-ride ontheETT cuffs mayprovide asimple andeffective method to attenuate the incidence and severity of POST after tracheal intubation. Application of lidocaine spray to the oral pharyngeal cavity before intubation seems to increase the incidence of sore throat.13,14 In this study, wealsofound thatspraying10% lidocaineontheETTcuff alsoincreasedtheseverityofPOSTcomparedwith5% lido-cainegelorsaline.Tenpercentlidocainesolutioncontains ethanol, polyethylene glycol 400, menthol and saccharin asadditivesinthesolvent,whereasthe5%lidocaine solu-tionwe usedcontainedsodiumchlorideasan additive.In fact,bothmentholandethanolcanirritatetrachealmucosa, potentiallycausingtrachealmucosadamage,thusleadingto increasedseverityofPOST.However,Soltani15reportedthat usingintra-cuff lidocaine(ETTcuffs prefilledwith7---8mL of 2% lidocaine for 90min before intubation and refilled withenough2%lidocaineafterintubation)wassuperiorto sprayingtopical10%lidocaineonlaryngo-pharyngeal struc-tures or on the distal end of the ETT for decreasing the incidence of POST. Lidocaineas lubricating agentcausing increase adverseeffects onanesthesiawake up.Even the cuff rupture sometimes. Localanesthetic cuff injected is atechniqueforlesspainonswallowing.Thealkalinization ofLAbyaddingNAHCO3increaseLAdiffusionthroughcuff
wall.15
Theoretically,chemicalirritationfromtheadditivesmay beavoidedbyusingintra-cufflidocaine.Wealsofoundthat 5%lidocainegeldidnotattenuatetheincidenceandseverity ofPOSTcomparedwithnormalsaline.Thedurationofthe analgesic effectoflidocainesprayappliedtooral mucosa is 15min.16 Inthis study,at the endof surgery(averaging 180minaftertracheal intubation),theanalgesic effectof lidocainespraymighthavealreadydisappeared.This prob-ably explains why we found the incidence of POSTto be no different between the 5% lidocaine and normal saline groups.
Onelimitationofourstudyisthattherewasnorecordof coughingatthetimeofextubation.Althoughtheextubation protocolwasthesameinallgroups,wedidnotevaluatethe correlationbetweenthefrequencyofcoughingatthetime ofextubationandtheincidenceofPOST.The second limi-tationisthattheadditivesto5%and10%lidocainesolution aredifferent,whichmayhaveinfluencedtheresult.
This study demonstrated that applying benzydamine hydrochlorideonanETTcuffmayreducetheincidenceand severityofPOSTcomparedwithapplying10%lidocaine,5% lidocaine,and normalsaline.Application of10% lidocaine sprayshouldbeavoidedbecauseofworseningofPOSTwhere incidenceandseveritywereincreasedinrelationto5% lido-caineorsaline.Applying5%lidocaineontheETTcuffdoes notpreventPOSTbutbetterthansaline.
Table1 Comparisonbetweenthedifferentstudiedgroupsaccordingtosorethroatincidence.
Sorethroatincidence GroupI GroupII GroupIII GroupIV 2 p
0h
−ve 29(93.5%) 28(90.3%) 25(80.6%) 25(80.6%) 3.477 MCp=0.346
+ve 2(6.5%) 3(9.7%) 6(19.4%) 6(19.4%)
p1 FEp=1.000 FEp=0.255 FEp=0.255
p2 FEp=0.473 FEp=0.473
p3 p=1.000
1h
−ve 28(90.3%) 25(80.6%) 21(67.7%) 23(74.2%) 5.066 p=0.149
+ve 3(9.7%) 6(19.4%) 10(32.3%) 8(25.8%)
p1 FEp=0.473 p=0.029a p=0.096
p2 p=0.246 p=0.544
p3 p=0.576
6h
−ve 26(83.9%) 21(67.7%) 17(54.8%) 19(61.3%) 6.522 p=0.078 +ve 5(16.1%) 10(32.3%) 14(45.2%) 12(38.7%)
p1 p=0.138 p=0.013a p=0.046a
p2 p=0.297 p=0.596
p3 p=0.607
12h
−ve 29(93.5%) 25(80.6%) 19(61.3%) 21(67.7%) 10.377a p=0.016a
+ve 2(6.5%) 6(19.4%) 12(38.7) 10(32.3%)
p1 FEp=0.255 p=0.002a p=0.010a
p2 p=0.093 p=0.246
p3 p=0.596
24h
−ve 30(96.8%) 26(83.9%) 23(74.2%) 25(80.6%) 6.200 p=0.071 +ve 1(3.2%) 5(16.1%) 8(25.8%) 6(19.4%)
p1 FEp=0.195 FEp=0.026a FEp=0.104
p2 p=0.349 p=0.740
p3 p=0.544
2,valueofChisquareforcomparingbetweenthedifferentstudiedgroups;p1,pvalueforcomparingbetweengroupIandeachother
group;p2,pvalueforcomparingbetweengroupIIwithgroupsIIIandIV;p3,pvalueforcomparingbetweengroupsIIIandIV;MC,Monte
Carlotest;FE,FisherExacttest.
a Statisticallysignificantatp≤0.05.
evaluatethecorrelationbetweenthefrequencyofcoughing orbucking atthetimeofextubationandthe incidenceof POST.Thesecondlimitationisthatbenzydamine hydrochlo-ride is available under differenttrade names in different countries,itsformulationsarequitedifferentineach coun-try,andtheadditivesmightalsovary.Moreover,thesafety and dosage of benzydamine hydrochloride applied to the tracheaneedfurtherinvestigation,eventhoughwedidnot findanyadverseeffectsinourpatients.Thethirdlimitation is that theadditives to5% and 10%lidocaine solutionare different,whichmayhaveinfluencedtheresult.
Conclusions
BenzydaminehydrochloridegelontheETTcuffisasimple andeffectivemethodtoreducetheincidenceandseverity ofPOST inrelation tolidocaineandsaline.Applicationof 10%lidocainesprayshouldbeavoidedbecauseofworsening ofPOSTwhereincidenceandseverityisincreased.Applying
5%lidocainegelontheETTcuffdoesnotpreventPOSTbut betterthanlidocaine10%sprayorsaline.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.StridePC. Postoperative sore throat:topicalhydrocortisone. Anaesthesia.1990;45:968---71.
2.StanleyTH,LoeserEA.Minimizingsorethroat[letter;reply]. Anesthesiology.1979;51:488---9.
3.JensenPJ,HommelgaardP,Sondergaard P.Sore throat after operation:influenceoftrachealintubation,intracuffpressure andtypeofcuff.BrJAnaesth.1982;54:453---7.
4.KeaneWM,RoweLD,DennenyJC.Complicationsofintubation. AnnOtolRhinolLaryngol.1982;91:584---7.
postoperativesorethroat:aprospective,randomized, single-blindstudy.AnesthAnalg.2006;103:1001---3.
6.OgataJ,MinamiK,HorishitaT.Garglingwithsodiumazulene sulfonatereducesthepostoperativesorethroatafterintubation ofthetrachea.AnesthAnalg.2005;101:290---3.
7.Mecca RS. Postoperative recovery. In: Barash PG, Cullen BF, Stoelting RF, editors. Clinical Anaesthesia Philadelphia, PA: Lippincott-Raven;1997.p.1279---303.
8.LeslieE,GeoffreyJ.In:JamesM,editor.Statisticalanalysis. Interpretationand usesofmedical statistics,4thed.Oxford ScientificPublications;1991.p.411---6.
9.KirkpatrickLA,FeeneyBC.AsimpleguidetoIBMSPSSstatistics forversion20.Studented.Belmont,CA:Wadsworth,Cengage Learning;2013.p.115.
10.Huang Yuan-Shiou, Hung Nan-Kai, Lee Meei-Shyuan. The effectiveness of benzydamine hydrochloridespraying onthe endotrachealtubecuffororalmucosaforpostoperativesore throat.IntAnesthResSoc.2010;111:882---6.
11.Hung Nan-Kai, Wu Ching-Tang, Chan Shun-Ming. Effect on postoperative sore throat of spraying the endotra-cheal tube cuff with benzydamine hydrochloride, 10%
lidocaine,and2%lidocaine.SocAmbulAnesthesiol.2010;111: 887---92.
12.PassaliD,VolonteM,PassaliGC.Efficacyandsafetyof ketopro-fenlysinesalt mouthwashversusbenzydaminehydrochloride mouthwashinacutepharyngealinflammation:arandomized, single-blindstudy.ClinTher.2001;23:1508---18.
13.Maruyama K,Sakai H,Miyazawa H. Laryngotracheal applica-tionoflidocainesprayincreasestheincidenceofpostoperative sore throat after total intravenous anesthesia. J Anesth. 2004;18:237---40.
14.Hara K, Maruyama K. Effect of additives in lidocainespray on postoperative sore throat, hoarseness and dysphagia aftertotalintravenousanaesthesia.ActaAnaesthesiolScand. 2005;49:463---7.
15.SoltaniHA,AghadavoudiO.Theeffectofdifferentlidocaine applicationmethodsonpostoperativecoughandsorethroat.J ClinAnesth.2002;14:15---8.