w w w . r b o . o r g . b r
Original
Article
Functional
evaluation
of
arthroscopic
repair
of
rotator
cuff
injuries
in
patients
with
pseudoparalysis
夽
,
夽夽
Alberto
Naoki
Miyazaki,
Marcelo
Fregoneze,
Pedro
Doneux
Santos,
Luciana
Andrade
da
Silva,
Guilherme
do
Val
Sella
∗,
Douglas
Lobato
Lopes
Neto,
Melvis
Muchiuti
Junior,
Sergio
Luiz
Checchia
OrthopedicsandTraumatologyService,FaculdadedeCiênciasMédicasdaSantaCasadeSãoPaulo,SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received18March2013 Accepted16August2013 Availableonline13April2014
Keywords:
Paralysis
Rotatorcuff/injuries Shoulderjoint/surgery
a
b
s
t
r
a
c
t
Objective:toevaluatethefunctionalresultfromarthroscopicrepairofrotatorcuffinjuries inpatientswithpseudoparalysis,definedasincapacitytoactivelyraisethearmabove90◦, whilecompletepassiveelevationwaspossible.
Methods:wereevaluated38patientswithameanfollow-upof51months(minimumof24). Weanalyzedthepseudoparalysisreversionrateandthefunctionalresultobtained.
Results:accordingtotheassessmentcriteriaoftheUniversityofCaliforniainLosAngeles (UCLA),31(82%)patientshadgoodandexcellentresults,two(5%)hadfairresultsandfive (13%)hadpoorresults.Themeanactiveelevationwentfrom39◦beforetheoperationto139◦ aftertheoperation(p<0.05);themeanactivelateralrotationwentfrom30◦to48◦(p<0.05) andthemeanactivemedialrotationwentfromlevelL3toT12(p<0.05).
Conclusion:arthroscopicrepairofrotatorcuffinjuriesproducedgoodandexcellentresults in82%ofthecasesandastatisticallysignificantimprovementofactiverangeofmotion, withreversionofthepseudoparalysisin97.4%ofthecases.Itisthereforeagoodtreatment option.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
Avaliac¸ão
funcional
do
reparo
artroscópico
da
lesão
do
manguito
rotador
em
pacientes
com
pseudoparalisia
Palavras-chave:
Paralisia
Manguitorotador/lesões Articulac¸ãodoombro/cirurgia
r
e
s
u
m
o
Objetivo:avaliaroresultadofuncionaldoreparoartroscópicodaslesõesdomanguitorotador empacientescompseudoparalisia,definidacomoincapacidadedeelevac¸ãoativadobrac¸o acimade90◦,comelevac¸ãopassivacompleta.
Métodos:reavaliamos38pacientescommédiadeseguimentode51meses(mínimode24). Analisamosataxadereversãodapseudoparalisiaeoresultadofuncionalobtido.
夽Pleasecitethisarticleas:MiyazakiAN,FregonezeM,SantosPD,daSilvaLA,doValSellaG,NetoDLL,etal.Avaliac¸ãofuncionaldo
reparoartroscópicodalesãodomanguitorotadorempacientescompseudoparalisia.RevBrasOrtop.2014;49:178–182.
夽夽
WorkperformedintheShoulderandElbowGroup,DepartmentofOrthopedicsandTraumatology,SchoolofMedicalSciences,Santa CasadeSãoPaulo,FernandinhoSimonsenWing.
∗ Correspondingauthor.
E-mail:guilton@ig.com.br(G.doValSella).
2255-4971/$–seefrontmatter©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditoraLtda.Allrightsreserved.
Resultados: peloscritériosdeavaliac¸ãodaUniversidadedaCalifórniaemLosAngeles(Ucla), 31(82%)pacientestiverambonseexcelentesresultados;dois(5%)resultadosregularese cinco(13%)ruins.Amédiadaelevac¸ãoativapassoude39◦nopré-operatóriopara139◦no pós-operatório(p<0,05),amédiadarotac¸ãolateralativapassoude30◦para48◦(p<0,05)e amédiadarotac¸ãomedialativapassoudonívelL3paraoT12(p<0,05).
Conclusão: oreparoartroscópicodaslesõesdomanguitorotadorproporcionoubonse exce-lentes resultados em82% doscasos eumamelhoria, estatisticamentesignificativa,da amplitudedemovimento(ADM)ativa,comreversãodapseudoparalisiaem97,4%doscasos. É,portanto,umaboaopc¸ãodetratamento.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Todososdireitosreservados.
Introduction
Thefunctionsoftherotatorcuffaretostabilizethehumeral headinsidetheglenoidcavityandrotatethehumerusin rela-tiontothescapula.1Thesupraspinatusmuscleisresponsible forthefirst10◦to15◦ofshoulderelevationrangeofmotion and,together withtheinfraspinatus,teres minorand sub-scapularismuscles,opposestheforceofthedeltoidmuscle, whichtendstomovethehumeralheadupwardsduring ele-vationmovements.2,3Rotatorcuffinjuriesmayleadtolossof thesefunctionsandconsequentlytochronicpain,weakness andfunctionalincapacity.4
Pseudoparalysisduetorotatorcuffinjury(PRCI)hasbeen definedbysomeauthors5–7 asincapacitytoperformactive elevationofthearmabove90◦,withnormalpassivemobility oftheshoulder.Thisdeficitofactiveelevationisassociated withrotatorcuffinjuriesthatareusuallylargeorextensive.8,9 The results from repairing large or extensive rotator cuff injuries have generally been reported in the literature as satisfactory.10–12However,thefunctionalrecoveryofpatients withPRCI who undergo arthroscopic surgical repairisstill knownonlyalittle.
Theobjective ofthe present study was to evaluatethe resultsfromarthroscopicrepairofrotatorcuffinjuriesinPRCI patients.
Sample
and
methods
Between January1996and October2011, the Shoulderand ElbowGroupoftheDepartmentofOrthopedicsand Trauma-tology,SchoolofMedicalSciences,SantaCasadeSãoPaulo, performedarthroscopicoperationson38patientswithPRCI.
Allcaseswiththesecharacteristicswereincludedinthis study.Patientswithrotatorcuffinjurieswithoutparalysisand caseswithfollow-upsshorterthan24monthswereexcluded. Therewere21malepatients(55%);theagerangewasfrom 49to81years(meanof68years);andthedominantlimbwas operatedin30cases.Allthepatientsexceptforonereported havinghadawell-defineepisodeoftraumatothejointor trau-maticmuscleeffortthatledtolossofactiveelevationofthe affectedlimb.Thetimethathadelapsedbetweentheinjury andthesurgicaltreatmentrangedfromtwoto740days,with ameanof83days.Noneofthepatientshadundergoneany previoussurgeryontheaffectedshoulder(Table1).
Therangeofactivemotionbeforetheoperation,as mea-suredusingthestandardizationoftheAmericanAcademyof
OrthopaedicSurgeons(AAOS),13wasfrom0◦to90◦ofelevation (meanof39◦);therangeoflateralrotationwasfrom0◦to80◦ (meanof30◦);andtherangeofmedialrotationwasbetween thegreatertrochanterandT7(meanatL3)(Table2).
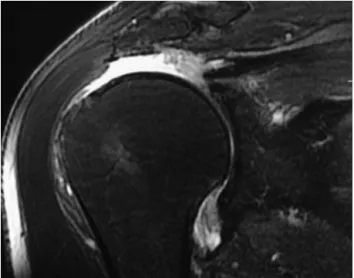
Thepresenceofarotatorcuffinjurywasconfirmedinall thepatientsbymeansofmagneticresonanceimaging(Fig.1). Allthepatientsunderwentthesurgicalprocedureinthe “deckchair” position, under general anesthesia combined withanesthetic blockofthebrachialplexus. Thejoint was arthroscopicallyinspectedbeforetherotatorcuffrepairwas performed. Next, the subacromial spacewas entered, with debridement ofthebursa,mobilizationofthe tendonsand openingofthebonebedofthefemoralhead,followedbyrepair oftherotatorcuffinjury(Fig.2).Tenlargelesionsand28 exten-sivelesionswerefound,inaccordancewiththeclassification proposedbyCofield8(Fig.3).Regardingthetendonsaffected, 26patientshadinjuriestothesupraspinatusand infraspina-tus and12 hadinjuriestothe supraspinatus,infraspinatus andsubscapularis.Noneofthepatientshadinjuriestojust onetendonalone(Table1).Inrelationtothetendonofthe long head ofthe biceps brachiimuscle, 12 patients under-went tenotomy, sevenunderwent tenotomyplus tenodesis andsevendidnotundergotheseprocedures.Acromioplasty wasperformedon32ofthe38patients.Resectionofthe lat-eralportionoftheclaviclewasperformedineightofthe38 patients.Arthrex®materialwasusedonallourpatients.
Duringthepostoperativeperiod,thepatientswere immo-bilizedforsixweeks,inaslingwiththearmabductedand
Table1–Dataonthepatients.
No. Sex Age (years)
Dominance T(days) Follow-up (months)
Pre-opactive ROM:EL,LR,MR
Tendon Size Post-opactive ROM:EL,LR,MR
UCLA
1 F 75 + 21 24 50,45,T7 SS+IS L 130,45,T7 16 2 F 61 − 7 24 80,40,T7 SS+IS L 140,45,T12 31 3 M 68 + 2 35 30,45,L2 SS+IS EXT 140,30,T12 32 4 F 71 + 4 74 0,30,L5 SS+IS EXT 140,30,T10 18 5 M 72 + 30 116 80,45,L3 SS+IS EXT 150,45,L1 32 6 F 78 − 7 65 0,0,L3 SS+IS EXT 150,60,L1 34 7 F 81 + 30 26 60,30,T7 SS+IS EXT 140,40,T7 34 8 F 73 + 20 49 0,30,TR SS+IS+SUB EXT 150,60,L3 34 9 F 76 + 3 48 0,10,L5 SS+IS+SUB EXT 130,60,L1 34 10 F 75 + 20 38 80,30,L1 SS+IS+SUB EXT 120,40,L1 10 11 M 72 + 4 72 30,60,GL SS+IS EXT 160,60,T8 34 12 M 60 + 14 94 45,30,L3 SS+IS EXT 150,45,T10 34 13 M 67 − 14 45 30,10,T7 SS+IS+SUB EXT 150,60,T8 34 14 M 64 + 7 87 0,30,L3 SS+IS+SUB EXT 150,45,L1 32 15 F 67 + 30 74 60,0,T8 SS+IS EXT 140,45,L1 34 16 F 81 + 3 26 45,20,T7 SS+IS+SUB EXT 45,30,T7 15 17 F 79 + 10 25 80,0,T10 SS+IS EXT 150,60,L1 29 18 F 79 − 4 24 30,30,L1 SS+IS EXT 150,45,L1 32 19 M 62 + 45 75 90,60,L1 SS+IS L 150,60,L1 34 20 M 66 + 60 73 30,60,L5 SS+IS L 140,60,L1 34 21 M 74 + 1 29 30,0,T7 SS+IS EXT 120,20,L1 33 22 M 49 + 740 26 80,50,GL SS+IS+SUB EXT 140,60,L3 33 23 M 74 − 14 56 0,0,T7 SS+IS L 150,50,T7 34 24 M 68 + 15 51 60,0,L1 SS+IS L 150,45,L5 34 25 M 56 + 15 25 70,20,L1 SS+IS+SUB EXT 150,50,T7 34 26 F 79 + 30 53 80,60,T7 SS+IS EXT 120,45,L2 29 27 F 69 + 4 50 30,80,T12 SS+IS EXT 120,80,T12 34 28 M 65 + 32 24 60,45,L3 SS+IS EXT 150,45,L1 34 29 M 71 + 30 33 20,70,L3 SS+IS+SUB EXT 150,60,T8 32 30 M 70 − 20 37 0,60,T10 SS+IS EXT 120,60,L1 34 31 M 81 + 15 24 0,0,T8 SS+IS+SUB EXT 150,45,L1 32 32 M 55 + 10 24 0,0,T7 SS+IS L 150,45,T7 32 33 M 74 + 60 25 30,0,T10 SS+IS EXT 150,0,T8 32 34 M 74 + 60 26 80,80,L5 SS+IS+SUB EXT 150,60,T10 34 35 M 53 − 2 24 0,80,T10 SS+IS L 160,60,T10 34 36 F 72 + 150 45 70,45,T7 SS+IS L 120,45,T7 27 37 F 57 − 600 26 90,35,T10 SS+IS+SUB EXT 120,45,T9 19 38 F 62 + 330 48 90,20,GL SS+IS L 140,50,T9 22
Source:hospitalmedicalfiles.
T,timeelapsedbetweendiagnosisandoperation;ROM,rangeofmotionmeasuredindegrees;Pre-op,beforeoperation;EL,elevation;LR,lateral rotation;MR,medialrotation;Tendon,tendonsaffected,asseenduringoperation;Post-op,afteroperation;SS,supraspinatus;IS,infraspinatus, SUB,subscapularis;EXT,extensive;L,large;T,measurementaccordingtoheightofthethoracicvertebra;L,measurementaccordingtoheight ofthelumbarvertebra;GL,measurementaccordingtoheightofthegluteus;UCLA,scoreonthescaleoftheUniversityofCaliforniainLos Angeles.
Table2–Patients’preoperativeandpostoperativemobility.
Pre-opactiveROM(mean) Post-opactiveROM(mean) mobility
EL 39 139 100
LR 30 48 18
MR L3 T12 3levels
Source:hospitalmedicalfiles.
ROM,rangeofmotion;Pre-op,beforeoperation;Post-op,afteroperation;mobility,differenceinactiveROMfrombeforeoperationtoafter operation.
in neutral rotation. After this period, the sling was with-drawn and elevation, lateral rotation and medial rotation wereallowed,bothpassivelyandactively.Fourmonthsafter theoperation,musclestrengtheningwasstarted(Fig.4).The resultswereevaluatedinaccordancewiththeUCLAmethod14
andtherangeofmotionwasmeasuredinaccordancewiththe standardizationoftheAAOS.13
Fig.2–Arthroscopicsurgicalimage(subacromialview) showingcompleteclosureofanextensiverotatorcuff injury.
theoperationwereanalyzed,takingthesignificancelevelto be5%(p<0.05).
Thelengthoffollow-upforthesepatientsrangedfrom24 to116months(meanof51).
Results
Themeanactiveelevationaftertheoperationwas139◦(range: 45◦to160◦)(p<0.05),themeanlateralrotationwas48◦(range: 0◦ to80◦)(p<0.05)andthemeanmedialrotationwasatthe levelofthe12ththoracicvertebra(range:fromthesacrumto T7)(p<0.05)(Table2).
ThemeanscoreusingtheUCLAmethodinthefinal evalu-ationwas27points(range:10to34).Nineteenpatients(50%) wereclassifiedashavingexcellentresults,12(32%)good,two (5%)fairandfive(13%)poor.Amongthefivecasesthatwere consideredtohavepoorresults,onlyoneneededtobe reop-erated.
Discussion
PRCIisassociatedwithinabilitytoperformsimplearm move-ments of day-to-day life, such as raising the hand to the
Fig.3–Arthroscopicsurgicalimage(subacromialview) showinganextensiverotatorcuffinjury.
Fig.4–Clinicalimageofapatientafterfunctional rehabilitation.
mouth,brushingteethandcombinghair,becauseofthelossof activeelevationofthearm.Thetreatmentoptionsfor pseu-doparalysisincludestrengtheningoftheanteriorportionof theanteriordeltoid,15reversetotalarthroplastywithor with-out associatedmuscle transfer,6,7 repairofthe rotator cuff injury10,16 andtransferofthelatissimusdorsimuscletothe greatertubercle.17
Levyetal.15prospectivelyevaluated17patientswith exten-siveirreparablerotatorcuffinjuriesthatweretreatedthrough arehabilitationprogramfortheanteriorportionofthedeltoid musclebecausetheywerenotinasuitableclinicalcondition toundergosurgicaltreatment.Theirmeanagewas80years. Theiractiveelevationincreasedfrom40◦to160◦afterthe reha-bilitationprogram,withaminimumfollow-upofninemonths. However,theirmusclestrengthdidnotimprove.
Gerber et al.17 proposed transferofthe latissimusdorsi muscle to the greater tubercle as a treatment option for patientswithextensiveirreparableinjuriestotherotatorcuff. Amongthesepatients,themeanelevationbeforethesurgery was62◦anditbecame150◦afterthemuscletransfer.
arthroplasty together with transferof the latissimus dorsi teresmajormuscles.Theanterioractiveelevationincreased from 70◦ to 148◦, lateral rotation increased from −18◦ to 18◦ and medial rotation decreased from L1 to S3. On the other hand,Mulieri etal.18 reportedacomplication rateof around 20% after reverse arthroplasty, over the course of amean follow-up periodof 52 monthsamong60 patients withpseudoparalysiswithoutarthrosisoftheshoulderjoint. Amongthesepatients, 34had nothadprevioussurgeryon theshoulderand,inthisgroup,theanterioractiveelevation increasedfrom54◦to136◦(p<0.001).
Webelievethatarthroscopicrepairofrotatorcuffinjuries inpatients with PRCI presenteda lower complicationrate than that ofreversetotal arthroplasty ofthe shoulder. We alsoobservedthattherewasasignificantimprovementinall shouldermovementsofelevation,lateralrotationandmedial rotation after the rotator cuff injuries had been repaired (Table2).
Morerecently, Oh et al.10 showed that there was pseu-doparalysisreversionrateof76%among29patients.These authorsdidnotconsiderthatadiminishedintervalbetween the acromion and the humerus or fatty infiltration ofthe tendons ofthe rotator cuff were contraindications against repair. Theyrecommended thatthe first-linetreatment for patientswith PRCIwithout arthropathydue torotator cuff injuryshouldbeprimaryarthroscopicrepair.
Denardetal.16 reportedapseudoparalysisreversionrate of90%amongagroupof39patientswhounderwentprimary arthroscopicrepairofrotatorcuffinjuries.Inanothergroup of14patientswhounderwentrevisionofrenewedtearingof therotatorcuff,the reversionratewas43%.Ourstudy cor-roboratesthedataintheliteratureonarthroscopicrepairof rotatorcuffinjuriesinpatientswithPRCI,withareversionrate of97.4%.
Weonly had one casethat required reoperation (2.6%). Thispatientcontinuedtopresentintensepain, diminished strengthandlittlemovementintheaffectedlimb,andforthis reasonhadtoundergoreversetotalarthroplasty.
Conclusion
Arthroscopic repair of rotator cuff injuries in cases with PRCIprovidedastatisticallysignificantimprovementinactive range of motion, with reversion ofthe pseudoparalysis in 97.4%ofthepatientsthustreated.Goodandexcellentresults wereobservedin82%ofthecasesandthisfunctional improve-mentwasobtainedwithlowcomplicationrates.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. VeadoMAC,CastilhoRS,MaiaPEC,RodriguesAU.Estudo prospectivoecomparativodosresultadosfuncionaisapós
reparoabertoeartroscópicodaslesõesdomanguitorotador. RevBrasOrtop.2011;46(5):546–52.
2.DrakeGN,O’ConnorDP,EdwardsTB.Indicationsforreverse totalshoulderarthroplastyinrotatorcuffdisease.Clin OrthopRelatRes.2010;468(6):1526–33.
3.ChecchiaSL,SantosPD,MiyazakiAN,FregonezeM,SilvaLA, LeiteFSF,etal.Avaliac¸ãodosresultadosdaartroplastia parcialdeombroparatratamentodaartropatiaporlesãodo manguitorotador.RevBrasOrtop.2008;43(6):232–9. 4.MoserM,JablonskiMV,HorodyskiM,WrightTW.Functional
outcomeofsurgicallytreatedmassiverotatorcufftears:a comparisonofcompleterepair,partialrepair,and debridement.Orthopedics.2007;30(6):479–82.
5.BerhouetJ,CollinP,BenkalfateT,LeDuC,DuparcF,Courage O,etal.Massiverotatorcufftearsinpatientsyoungerthan65 years.Epidemiologyandcharacteristics.OrthopTraumatol SurgRes.2009;954Suppl.1:S13–8.
6.BoileauP,ChuinardC,RoussanneY,BicknellRT,RochetN, TrojaniC.Reverseshoulderarthroplastycombinedwitha modifiedlatissimusdorsiandteresmajortendontransferfor shoulderpseudoparalysisassociatedwithdroppingarm.Clin OrthopRelatRes.2008;466(3):584–93.
7.WernerCM,SteinmannPA,GilbartM,GerberC.Treatmentof painfulpseudoparesisduetoirreparablerotatorcuff dysfunctionwiththeDeltaIIIreverse-ball-and-sockettotal shoulderprosthesis.JBoneJointSurgAm.2005;87(7):1476–86. 8.CofieldRH.Subscapularmuscletranspositionforrepairof
chronicrotatorcufftears.SurgGynecolObstet. 1982;154(5):667–72.
9.HawkinsRJ,MisamoreGW,HobeikaPE.Surgeryfor full-thicknessrotator-cufftears.JBoneJointSurgAm. 1985;67(9):1349–55.
10.OhJH,KimSH,ShinSH,ChungSW,KimJY,KimSH,etal. Outcomesofrotatorcuffinlarge-to-massivetearwith pseudoparalisis.AmJSportsMed.2011;39(7):1413–20. 11.ChecchiaSL,SantosPD,MiyazakiAN,FregonezeM,SilvaLA,
SalimMussiF,etal.Tratamentocirúrgicodaslesõesextensas domanguitorotadorpelaviadeacessodeltopeitoral.Rev BrasOrtop.2003;38(5):252–60.
12.GerberC,FuchsB,HodlerJ.Theresultsofrepairofmassive tearsoftherotatorcuff.JBoneJointSurgAm.
2000;82(4):505–15.
13.CodsiM,McCarronJ,BremsJJ.Clinicalevaluationofshoulder problems.In:RockwoodJrCA,MatsenIIIFA,WirthMA,etal., editors.Theshoulder.4thed.Philadelphia:SaundersElsevier; 2009.
14.OkuEC,AndradeAP,StadinikySP,CarreraEF,TelliniGG. Traduc¸ãoeadaptac¸ãoculturaldoModifiedUniversityof CaliforniaatLosAngelesShoulderRatingScaleparaalíngua portuguesa.RevBrasReumatol.2006;46(4):246–52.
15.LevyO,MullettH,RobertsS,CopelandS.Theroleofanterior deltoidreeducationinpatientswithmassiveirreparable degenerativerotatorcufftears.JShoulderElbowSurg. 2008;17(6):863–70.
16.DenardPJ,LadermannA,JiwaniAZ,BurkhartSS.Functional outcomeafterarthroscopicrepairofmassiverotatorcuff tearsinindividualswithpseudoparalysis.Arthroscopy. 2012;28(9):1214–9.
17.GerberC,VinhTS,HertelR,HessCW.Latissimusdorsi transferforthetreatmentofmassivetearsofrotatorcuff:a preliminaryreport.ClinOrthopRelatRes.1988;232(1):51–61. 18.MulieriP,DunningP,KleinS,PupelloD,FrankleM.Reverse