REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
Intravenous
lidocaine
for
post-mastectomy
pain
treatment:
randomized,
blind,
placebo
controlled
clinical
trial
Tania
Cursino
de
Menezes
Couceiro
a,∗,
Luciana
Cavalcanti
Lima
a,b,
Léa
Menezes
Couceiro
Burle
a,
Marcelo
Moraes
Valenc
¸a
caInstitutodeMedicinaIntegralProfessorFernandoFigueira(IMIP),Recife,PE,Brazil bFaculdadePernambucanadeSaúde(FBS),Recife,PE,Brazil
cDepartmentofNeurologyandNeurosurgery,UniversidadeFederaldePernambuco,Recife,PE,Brazil
Received28April2014;accepted19May2014 Availableonline30March2015
KEYWORDS
Postoperativepain; Treatment; Localanesthetic; Pain;
Intravenouslidocaine
Abstract
Backgroundandobjective: Postoperativepaintreatmentinmastectomyremainsamajor chal-lengedespitethemultimodalapproach.Theaimofthisstudywastoinvestigatetheanalgesic effectofintravenouslidocaineinpatientsundergoingmastectomy,aswellasthepostoperative consumptionofopioids.
Methods:AfterapprovalbytheHumanResearchEthicsCommitteeoftheInstitutodeMedicina IntegralProf.FernandoFigueirainRecife,Pernambuco,arandomized,blind,controlledtrial wasconductedwithintravenouslidocaineatadoseof3mg/kginfusedover1hin45women undergoingmastectomyundergeneralanesthesia.Onepatientfromplacebogroupwas.
Results:Groupsweresimilarinage,bodymassindex,typeofsurgery,andpostoperativeneed for opioids.Twoof22patientsinlidocainegroupandthreeof22patientsinplacebogroup requestedopioid(p=0.50).Painonawakeningwasidentifiedin4/22oflidocainegroupand5/22 ofplacebogroup(p=0.50);inthepost-anestheticrecoveryroomin14/22and12/22(p=0.37) oflidocaineandplacebogroups,respectively.Painevaluation24haftersurgeryshowedthat 2/22and3/22patients(p=0.50)oflidocaineandplacebogroups,respectively,complainedof pain.
Conclusion: Intravenouslidocaineatadoseof3mg/kgadministeredoveraperiodofanhour duringmastectomydidnotpromoteadditionalanalgesiacomparedtoplacebointhefirst24h, andhasnotdecreasedopioidconsumption.However,abeneficialeffectofintravenouslidocaine inselectedand/orothertherapeuticregimenspatientscannotberuledout.
© 2014SociedadeBrasileirade Anestesiologia.Publishedby ElsevierEditoraLtda.Allrights reserved.
∗Correspondingauthor.
E-mails:taniacouceiro@yahoo.com.br,taniacursinomcouceiro@gmail.com(T.C.d.M.Couceiro).
http://dx.doi.org/10.1016/j.bjane.2014.05.017
PALAVRAS-CHAVE
Dorpós-operatória; Tratamento; Anestésicolocal; Dor;
Lidocaínaintravenosa
Lidocaínaintravenosanotratamentodadorpós-mastectomia:ensaioclínico
aleatórioencobertoplacebocontrolado
Resumo
Justificativaeobjetivo:Otratamentodadorpós-operatóriaemmastectomiacontinuasendo um grandedesafioapesar daabordagemmultimodal. Oobjetivo desteestudofoi investigar oefeitoanalgésicodalidocaínaintravenosaem pacientessubmetidasamastectomia,como também,oconsumodeopioidepós-operatório.
Métodos: Apósaprovac¸ãopelocomitêdeéticaepesquisaemsereshumanosdoInstitutode MedicinaIntegralProf.FernandoFigueiraemRecife-Pernambucofoirealizadoensaioclínico aleatórioencobertoplacebocontroladocomlidocaínaintravenosanadosede3mg/kginfundida emumahora,em45mulheressubmetidasamastectomiasobanestesiageral. Excluídauma pacientedogrupoplacebo.
Resultados: Osgruposforamsemelhantesquantoàidade,índicedemassacorpórea,tipode intervenc¸ão cirúrgicaenecessidade deopioide nopós-operatório.Solicitaram opioide2/22 pacientes nos grupos da lidocaína e 3/22 placebo(p=0,50). Identificada a dor ao desper-tarem 4/22nogrupolidocaína e5/22(p=0,50) nogrupoplacebo; nasalade recuperac¸ão pós-anestésicaem14/22e12/22(p=0,37)nosgruposlidocaínaeplaceborespectivamente. Aoavaliarador24horasapósoprocedimentocirúrgico3/22e2/22(p=0,50)daspacientes relataramdoremambososgruposrespectivamente.
Conclusão:Alidocaína intravenosanadosede3mg/kgadministradaemum períododeuma horanotransoperatóriodemastectomianãopromoveuanalgesiaadicionalemrelac¸ãoaogrupo placebonasprimeiras24horasenãodiminuiuoconsumodeopioide.Contudo,umefeito bené-ficodalidocaínaintravenosaempacientesselecionadase/ouemoutrosregimesterapêuticos nãopodeserdescartado.
©2014SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Postoperative pain remains inadequately treated despite its predictability and progress of various analgesic tech-niquesand drugs available for its control.1 Some authors
reportthat, regardless of the typeof surgical procedure, postoperativepainispresentandwithvaryingintensity.2---4
Theincidenceofpostoperativepaininbreastcancerislow whentreatedproperly,5however,itcanresultin
cardiovas-cular and respiratory complications, aswell aspersistent postoperativepain.6Therefore,adequatepaincontrolisof
paramountimportanceinclinicalpractice.
Inthiscontext,themultimodalapproachto postopera-tivepainshouldbeconsidered,giventheanalgesicresults obtainedwitheachparticulardrugandthelowerincidence ofadverseeffects.6,7
Inordertoprovidepostoperativeanalgesia,intravenous lidocaine has been used intra- and post-operatively as partofmultimodalapproach,8withprovenanalgesiceffect
in postoperative abdominal9 and pelvic surgery, such as
colectomy10andprostatectomy,11respectively.
Inadditiontotheanalgesicaction,localanestheticshave anti-inflammatoryaction,11justifyingtheuseofintravenous
lidocainetomodulatetheinflammatoryresponseresulting frompostoperativepain.12 Otherbenefits arethereduced
need for postoperative opioids,8,10 reduced complications
suchasnauseaandvomiting,andreducedpainintensityin thefirst24h.10
Meta-analyses9,13 showconflicting resultsregarding the
analgesic effectof lidocaine onpostoperative pain, high-lighting the need tospecify the realvalue of intravenous lidocaineforpostoperativepainreliefinpatientsundergoing mastectomy.Theobjectiveofthisstudywastoinvestigate theanalgesiceffectofintravenouslidocaineinthefirst24h inwomenundergoingmastectomy,aswellastoassessthe consumptionofopioidspostoperatively.
Methods
After approval by the Human Research Ethics Commit-tee of the Integrative Medicine Institute Prof. Fernando Figueira (IMIP), under number2026 CAAE 0202009917210, andobtainingwritteninformedconsentfromparticipants,a randomized,placebocontrolled,blindclinicaltrialwas per-formedfromJuly2011toAugust2012,attheIMIP,Recife, Pernambuco,Brazil.
donotunderstandthenumericalscale (NS)ofpain assess-mentand/orhaveusedopioidsinthepast24h.
Datawerecollectedusingastandardizedquestionnaire tocharacterizethesample.Dataincluded age,bodymass index (BMI), type of surgery, adjuvant treatment, and pain history, such as headache and surgery breast pain. The variablesstudiedwerepresence andintensityof pain 24h aftersurgeryat threedifferenttimepoints(M1upon awakeningfromanesthesia,M2=1hafteradmissiontothe post-anesthesia care unit (PACU), and M3=24h after the surgicalprocedure)andtheneedforpostoperativeopioids. Painwasassessedatrest,usingaNSpainfrom0to10(0=no painand10=worstpossiblepain).Foranalysis,painseverity wascategorizedasabsent(0),mild(1---3),moderate(4---7), severe(7---9),andverysevere(10).
Patientswererandomlyallocatedintotwogroups (lido-caineor placebo)ona1:1ratiobydrawingblocksoffour patients, asin theevent of suspension or discontinuation of study, the number of patients would remain similarin bothgroups. Toensure thatthestudywasblind,the lido-caineandplaceboampouleswerepreparedinsimilarvials andnumberedsequentially.Allpatientsunderwentgeneral anesthesiawithfentanyl(5gkg−1),propofol(1.0mgkg−1),
and rocuronium (0.3mgkg−1) and maintained with 1.5%
sevofluranein 50%fractionof inspiredoxygen.Bolusdose of lidocainewasnotadministeredand,after incision, the 1hinfusionofsalinesolution(100mL)containingthetotal doseoflidocaine(3mgkg−1)orplacebowasstarted.
All patients received intravenous dipyrone (2g) and ketoprofen(100mg)duringsurgeryasprophylaxisof postop-erativepain.The chestwallwasinfiltratedwithasolution containing0.025%bupivacaineandepinephrine1:400,000, accordingtotheMastologyServiceconduct.For postoper-ative analgesia 1g dipyrone was prescribed every 6h. In caseofpain,codeine(30mg)associatedwithparacetamol (200mg) was prescribed to be administered according to patients’request.
The sample sizecalculation wasbased onthe assump-tionofa5%alpha-error,10%beta-error,and90%powerand consideringthatlidocainegrouphada70%reductionin opi-oidconsumption,whiletheplacebogroupwouldhavea30% reduction.13 A loss of 10% was presumed, resulting in 44
subjectsdividedintotwogroupsof22patientseach. Fordataanalysis,EPI-INFOTMsoftwareversion3.5.1for
WindowsTMwasused.Datawerepresentedasabsoluteand
relative frequency distribution and presented in tables. Numericalvariableswererepresentedasmeasuresof cen-tral tendency (mean) and dispersion (standard deviation and range). Chi-square test with Yates’ correction appli-cation and Fisher’s exact test were used to verify the existenceof anassociationbetween categoricalvariables. Ap-value<0.05wasconsideredsignificant.
Results
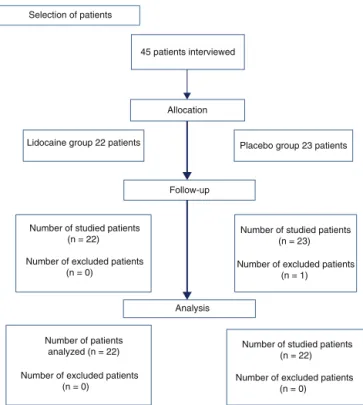
Forty-fourpatientswhounderwentmastectomywere eval-uated,22fromlidocainegroupand22fromplacebogroup (Fig. 1, flowchart). One patient from placebo group was excluded because, although she has shown tounderstand howtousetheproposedratingscaleofpain(NS)and there-forehavebeenincludedinthestudy,shecouldnotevaluate
Selection of patients
45 patients interviewed
Lidocaine group 22 patients Placebo group 23 patients
Follow-up
Number of studied patients (n = 22)
Number of excluded patients (n = 0)
Number of studied patients (n = 23)
Number of excluded patients (n = 1)
Analysis
Number of patients analyzed (n = 22)
Number of excluded patients (n = 0)
Number of studied patients (n = 22)
Number of excluded patients (n = 0) Allocation
Figure1 CONSORTflowchart.n,numberofpatients.
the pain using the NS postoperatively. The groups were similar in age, body mass index, adjuvant chemotherapy treatmentbeforemastectomy,andhistoryofpain(Table1). Regarding the type of surgery, two-thirds of patients in bothgroupsunderwentMadden’smastectomyandtheother one-thirdunderwentmastectomywithsentinellymphnode removal(Table1).
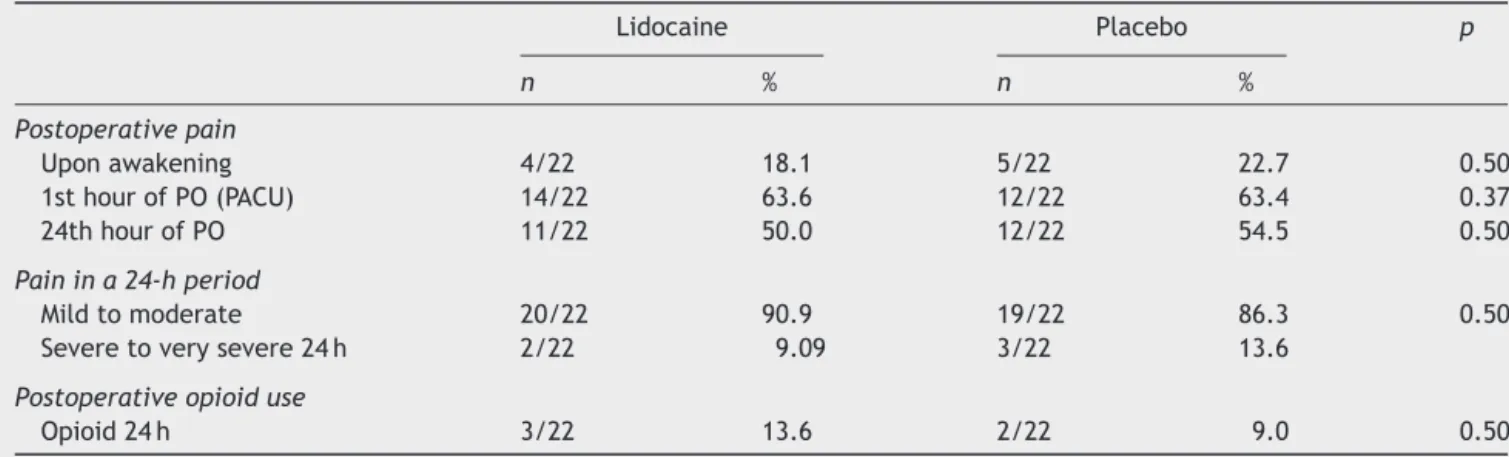
Therewasnodifferencebetweengroupsregarding post-operativepain at restin any ofthe timepointsassessed: uponawakeningfromanesthesia(M1),1hafterPACU admis-sion (M2), and 24h after the surgical procedure (M3) (Table2).
Opioid consumption in the first 24h after surgery was similarinthelidocaineandplacebogroups(Table2).
Discussion
Thisstudydemonstratedthatintravenousadministrationof lidocaineduringsurgeryatadoseof3mgkg−1in1hwasnot
superiortoplaceboforpostoperativeanalgesiainpatients undergoingmastectomy.
Other authors10 reportedbenefitwiththeuse of
intra-venouslidocaineforpostoperativepainrelief.Theauthors found improved analgesia in patients undergoing laparo-scopiccolectomywhenusinganinitialdose of1.5mgkg−1
followed by continuous infusion of 2.0mgkg−1g, which
lastedfor24hpostoperatively.
DeOliveiraetal.14 evaluatingpain inwomen
undergo-ing,ambulatorylaparoscopicsurgerywhoreceivedlidocaine (1.5mgkg−1)20minpriortosurgicalincision,followedbyan
infusionof2mgkg−1h−1uptotheendofsurgicalprocedure,
observepainreliefinthelidocainegroup.
Table1 Samplecharacterizationaccordingtogroups.
Characteristic Lidocaine Placebo p
Age(years)a 52.4±12.4 47.0±11.0 0.10b
BMIa 28.1
±8.1 28.2±3.9 0.89b
PriorQT 11/22(50%) 10/22(45.4%) 0.38c
Headache 6/22(30%) 9/22(40.9%) 0.34c
Breastpain 10/22(45.5%) 8/22(36.3%) 0.37c
Madden’smastectomy 17/22(77.2%) 17/22(77.2%)
---QT,chemotherapy;BMI,bodymassindex.
aMean
±standarddeviation.
b Chi-squaretest.
c Yates’correctionandFisher’sexacttest.
Table2 Occurrenceandintensityofpainatthreedifferenttimesandpostoperativeopioidrequirementin24h.
Lidocaine Placebo p
n % n %
Postoperativepain
Uponawakening 4/22 18.1 5/22 22.7 0.50
1sthourofPO(PACU) 14/22 63.6 12/22 63.4 0.37
24thhourofPO 11/22 50.0 12/22 54.5 0.50
Painina24-hperiod
Mildtomoderate 20/22 90.9 19/22 86.3 0.50
Severetoverysevere24h 2/22 9.09 3/22 13.6
Postoperativeopioiduse
Opioid24h 3/22 13.6 2/22 9.0 0.50
n,sample;Opioid24h,opioidrequirementinthefirst24haftersurgery;PACU,post-anesthesiacareunit;PO,postoperative.
oflidocainefor 24hpostoperativelymayhave resulted in suppressionofcentralsensitization15 andthus contributed
toobtaingoodanalgesiceffectincomparisonwithourstudy. Theuse ofbolus beforesurgery mayleadustothinkthat theadministrationoflidocainebeforesurgicalincisioncan promotebetterpostoperativepainresultsbyreducingthe releaseofinflammatorysubstances.
Regarding the dose, in a recent study16 using
intra-venous lidocaine in patients who underwent mastectomy, theauthorsevaluated36patientsdividedintotwogroups, with19womenintheplacebogroupand17inthelidocaine group.Lidocainewasadministeredatadoseof1.5mgkg−1
beforesurgical incision, followedby the samedose every hour, which lastedup to60min after closing the surgical incision.The perioperativeconductfor postoperativepain managementwasthe useof ketorolacat a singledose of 30mg. The authors found that lidocainewasable to pro-videsuperior analgesiatoplaceboonly inthefourth hour aftersurgery.Theseauthors16foundadecreaseinthe
cen-tralhyperalgesiaandadecreasedincidenceandseverityof persistentpostoperativepaininthelidocainegroup.
Inourstudy,theabsenceofadditionalanalgesic effect in the early postoperative period (first 4h after surgery) inthelidocainegroupmayhave beenmasked bythe effi-ciencyofthepreconizedpostoperativepainprophylaxis,as wetheadministrationofketoprofen(100mg)anddipyrone (2g)followedbydipyrone(1g)every6hfor24hwas system-atized.Associatedwiththesedrugs,infiltrationofthechest
wallipsilateraltothemastectomywithlocalanestheticand vasoconstrictorwasperformedinallpatients.
Currently,thereisnoconsensusaboutthebestlidocaine administrationmethod.Severalinfusionregimenshavebeen used:exclusivelyduringsurgery,8intraoperativelyand
con-tinued for 1h16 or 24h10, and evenas patient-controlled
analgesia.17 However,in ourstudy thechoiceof lidocaine
administrationfor a periodof 1h without usingan initial dose(bolus)wasbasedonareportofanotherstudybythis investigator,18whichshowedbenefitwhenusingintravenous
lidocaineforashortperiodoftime,andbecausethesurgical procedureintheinstitutionusuallyhasanaverageduration of1h.
Thechoiceofthe3mgkg−1dosewasbasedonthe
anal-gesicsresultsoftherapeuticdosesusedinclinicalpractice (2---5mgmL−1), whichachieved serumlevelsof 2
gmL−1.
Becausethe mild adverse effects beginwithserumlevels above3gmL−1,thisdoseresultsinasafetypharmacology
windowfortheuseofintravenouslidocaine.19,20
Therefore,studiesthatstipulatethebeginningofIL infu-sion in relation to the surgical incision time,duration of infusioninthepostoperativeperiod,andthetotaldose of intravenous lidocaine tobe administered are required to define itsactual roleinpostoperativeanalgesiain women undergoingmastectomy.
properlytotheinfusionregimenused,asthepainresulting fromcholecystectomieshasvisceralorigin,whilethe post-mastectomypainhassomaticorigin.Ontheotherhand,it shouldbeconsideredthattheseverityofpaininthe postop-erativeperiodofthissurgeryvariesfrommildtomoderate andtheuseofsimpleanalgesicssuchasdipyroneassociated withanti-inflammatorydrugsresultsinadequateanalgesia. In this study, opioid requirement was equal in both groups. Thesedataaresimilartothosereportedbyother authorswhoevaluatedopioidconsumptioninwomen under-going mastectomy.16 This result differs from studies with
outpatientsundergoinglaparoscopicsurgery,14laparoscopic
colectomy,10 andcholecystectomies,21inwhichtheauthors
observed a decrease of about 50% in opioid consumption duringthefirst24h.
Ahumanstudy22showsthatthereisanexcitatoryaction
of the local anesthetic in the intestine smooth muscle andthusadecreasedcolonicdistensionandpostoperative discomfort.Thisactionjustifiesthelidocaineabilityto alle-viate visceralpain,asdemonstrated inanimal models23,24
andprovenfromthereportedresultsinabdominalsurgery. Thispositiveanalgesicresponseinabdominalsurgerycan probablybeexplainedbytheinhibitoryactionofintravenous lidocainein visceromotor reflexes secondary to colon and rectum distention, which contributesto the relief of vis-ceralpain.9,10,13Itisnoteworthythatinthepaincausedby
hiparthroplasty25andmastectomy,16 intravenouslidocaine
didnotpromoteanalgesia,probablybecausethesesurgical proceduresresultin somaticpainthat is lessinhibitedby lidocaine.26
This finding helps to emphasize the hypothesis that intravenous lidocaine has a preferred analgesic effect on visceral9,10,13 and neuropathic26,27 pain. However, recent
studies have demonstrated thatintravenous lidocaine has analgesic13 andantihyperalgesic28,29 actionsresultingfrom
peripheralblockadeofectopicimpulsesinvolvedin nocicep-tionandalsofromitsactiononpotassiumchannels,calcium channels,andG-proteincoupledreceptors.Italsohas anti-inflammatoryaction30,31,aneffectresultingfromthelower
neutrophil accumulationat thesiteof injury andreduced releaseofinflammatorymediators.29,30Theseactionsjustify
itsuseinmultimodalapproachtopostoperativeanalgesia. Somelimitationsofthisstudyshouldbeconsidered.Pain wasassessedonlyatrest.Itisknownthatpaincanariseor worsenwithlimbmovementontheoperatedside,andpain assessmentatthispointcouldbringadditionalinformation. Pain on movement was not assessed because not moving the operated side member in the first24h after the sur-gicalprocedureistheMastologyServiceprotocol.Thepain symptomevaluationwasperformedforashortperiodafter surgery(24h).However,Grigoraetal.16foundnodifference
between pain scores when evaluated patients undergoing mastectomyuptotheseventhpostoperativeday.
Regarding persistent postoperative pain after mastec-tomy,thebenefitoflidocainehasbeenobserved.16However,
thistypeofpainwasnotassessedinourstudy.
Therefore,additionalstudiesareneededtoidentifythe lowestdoseabletopromoteanalgesia,‘‘Whatisthemost appropriateregimeforinfusion?’’,andfinally,identifythe value of lidocaine in the multimodal treatment of acute andchronic postoperativepain. Thus,inthis study, intra-venouslidocaineatadoseof3mgkg−1administeredovera
1hperiodperioperativelyduring mastectomydidnot pro-moteadditionalanalgesiacomparedtoplacebowithinthe first24h and didnot decrease opioid consumption. How-ever,abeneficialeffectofintravenouslidocaineinselected patientsand/orothertherapeuticregimenscannotberuled out.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
WethanktheCristáliaProdutosQuímicose Farmacêuticos LTDAfortheethicalandcarefulpreparationofdrugsforthe study(lidocaineandplacebo).
References
1.WhitePF.Painmanagementafterambulatorysurgery:whereis disconnect?CanJAnaesth.2008;55:201---7.
2.VadiveluN,MitraS,NarayanD.Recentadvancesin postopera-tivepainmanagement.YaleJBiolMed.2010;83:11---25.
3.MaierC,NestlerN,RichterH.Thequalityofpainmanagement inGermanhospitals.DutschArzteblInt.2010;107:607---14.
4.Couceiro TCM, Valenc¸a MM, Lima LC, et al. Prevalência e influência do sexo, idade e tipo de operac¸ão na dor pós-operatória.RevBrasAnestesiol.2009;59:314---20.
5.Couceiro TCM, Valenc¸a MM, Raposo MCF, et al. Prevalence ofpostmastectomypainsyndromand associatedriskfactors: a cross-sectional cohort study. Pain Manag Nurs’. 2014;15: 731---7.
6.Elvir-Lorenzo OL, White PF. Postoperative pain management afterambulatorysurgery:roleofmultimodalanalgesia. Anes-thesiolClin.2010;28:217---24.
7.White P, Kehlet H. Improving postoperative pain mana-gement what are the unresolved issues? Anesthesiology. 2010;112:220---5.
8.LauwickS,KimDJ, MichelagnoliG, etal.Functionalwalking capacity as an outcome measure of laparoscopic prostatec-tomy:theeffectoflidocaineinfusion.BrJAnaesth.2009;103: 213---9.
9.SunY,LiT,WangN,etal.Perioperativesystemiclidocainefor postoperativeanalgesiaandrecoveryafterabdominalsurgery: ameta-analysisofrandomizedcontrolledtrials.DisColon Rec-tum.2012;55:1183---94.
10.Kaba A, Laurent SR, Detroz BJ, et al. Intravenous lido-caineinfusionfacilitatesacuterehabilitationafterlaparoscopic colectomy.Anesthesiology.2007;106:11---8.
11.Beloeil H, Mazoit JX. Effect of local anesthetics on the postoperativeinflammatoryresponse.AnnFrAnesth Reanim. 2009;28:231---7.
12.ClarkeC,McConachieI,BannerR.Lidocaineinfusionasa res-cue analgesic in the perioperative setting. Pain Res Manag. 2008;13:421---3.
13.Marret E,Rolin M,Beaussier M,et al. Meta-análiseof intra-venouslidocaineand postoperativerecovery afterabdominal surgery.BrJSurg.2008;95:1331---8.
14.DeOliveiraGS, FitzgeraldP,StreicherLF.Systemiclidocaine toimprovepostoperativequalityofrecoveryafterambulatory laparoscopicsurgery.AnesthAnalg.2012;115:262---7.
16.GrigorasA,LeeP,SattarF,etal.Perioperativeintravenous lido-cainedecreasestheincidenceofpersistentpainafterbreast surgery.Pain.2012;28:567---72.
17.CepedaMS,DelgadoM,Ponce M,etal.Equivalent outcomes duringpostoperativepatients-controlledintravenousanalgesia withlidocaine plusmorphineversus morphinealone.Anesth Analg.1996;83:102---6.
18.Couceiro TCM, Valenc¸a MM. Lidocaína endovenosa no trata-mento da síndrome SUNCT secundária a tumor de hipófise, Seguimentodeumapacienteporumperíododequatroanos. Relatodecaso.RevDor.2013;14:320---2.
19.LaurettiGR.Mecanismosenvolvidosnaanalgesiadalidocaína venosa.RevBrasAnestesiol.2008;58:280---6.
20.OliveiraCMB,IssyAM,SakataRK.Lidocaínaporviavenosa intra-operatória.RevBrasAnestesiol.2010;60:325---33.
21.SaadawyIM,KakiAM,AbElLatifAA,etal.Lidocainevs. magne-sium:effectonanalgesiaafterlaparoscopiccholecystectomy. ActaAnaesthesiolScand.2010;54:549---56.
22.McKay A, Gottschalk A, Ploppa A, et al. Systemic lidocaine decreasedtheperioperativeopioidanalgesicrequirementsbut failed to reduce discharge time after ambulatory surgery. AnesthAnalg.2009;109:1805---8.
23.Maggi CA,Manzini S,Meli A. contributionofneurogenic and myogenicfactorsintheresponseofratproximalcolonto dis-tention.AmJPhisiol.1987;252:G447---57.
24.Ness TJ. Intravenous lidocaine inhibits visceral nocicep-tive reflexes and spinal neurons in the rat. Anesthesiology. 2000;92:1685---91.
25.Martin F, Cherif K, Gentili ME, et al. Lack of impact of intravenous lidocaine on analgesia, functional recovery, and nociceptivepainthresholdaftertotalhiparthroplasty. Anes-thesiology.2008;109:118---23.
26.KastrupJ,BachFW,PetersenP,etal.Lidocainetreatmentof painfuldiabeticneuropathyandendogenousopioidpeptidesin plasma.ClinJPain.1989;5:239---44.
27.Tremont-LukatsIW, HutsonPR,BackonjaMM. A randomized, double-masked,placebo-controlled pilottrialofextendedIV lidocaineinfusionforreliefofongoingneuropathicpain.ClinJ Pain.2006;22:266---71.
28.NasserR,YadlaS,MaltenfortMG,etal.Complicationsinspine surgery.JNeurosurgSpine.2010;13:144---57.
29.Mitchell SJ, Pellett O, Gorman DF. Cerebral protection bylidocaine during cardiac operations. Ann Thorac Surg. 1999;67:1117---24.
30.MathewJP,MackensenGB,Phillips-ButeB,etal.Randomized, double-blinded, placebocontrolled study ofneuroprotection withlidocaineincardiacsurgery.Stroke.2009;40:880---7.