w w w . r b o . o r g . b r
Original
Article
Evaluation
of
surgical
treatment
of
Dupuytren’s
disease
by
modified
open
palm
technique
夽
,
夽夽
Thiago
Almeida
Guilhen
∗,
Ana
Beatriz
Macedo
Vieira,
Marcelo
Claudiano
de
Castro,
Helton
Hiroshi
Hirata,
Itibagi
Rocha
Machado
InstitutoJundiaiensedeOrtopediaeTraumatologia,Jundiaí,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received11March2013 Accepted20May2013
Keywords:
Dupuytrencontracture Hand
Surgicalproceduresoperative
a
b
s
t
r
a
c
t
Objective:toassessthesurgicaltechniqueusingthemodifiedpalmopentechniqueforthe treatmentofseverecontractionsofDupuytren’sdisease.
Methods:overaperiodoffouryears,16patientsunderwentsurgicaltreatment,andinits entiretybelongedtostagesIIIandIVoftheclassificationproposedbyTubianaetal.We per-formedmeasurementsoftheextensiondeficitofthemetacarpophalangealjoints,proximal anddistalinterphalangealinpreoperative,postoperative(3months)andlatepostoperative period(5–8years).Anglesgreaterthan30◦metacarpophalangealjointsand15◦proximal
interphalangealtheresultswereconsideredsurgicalrecurrence.
Results:therewasobtainedanaverageof6.3◦atthemetacarpophalangealjoint,13.8◦inthe
proximalinterphalangealanddistalinterphalangealat1.9◦.
Conclusion: themodifiedopenpalmtechniqueisaneffectivemethodinthesurgical treat-mentofseverecontracturesinDupuytren’sdisease.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
Avaliac¸ão
do
tratamento
cirúrgico
da
doenc¸a
de
Dupuytren
pela
técnica
da
palma
aberta
modificada
Palavras-chave:
ContraturadeDupuytren Mãos
Procedimentoscirúrgicos operatórios
r
e
s
u
m
o
Objetivo:avaliarotratamentocirúrgicocomousodatécnicadapalmaabertamodificada paraotratamentodascontraturasgravesdadoenc¸adeDupuytren.
Métodos:emquatroanos,foramsubmetidosaotratamentocirúrgico16pacientes,que per-tenciamaosestágiosIIIeIVdaclassificac¸ãopropostaporTubianaetal.Foramfeitasaferic¸ões dodéficitdeextensãodasarticulac¸õesmetacarpofalangeanaseinferfalangeanaproximale distalnosperíodospré-operatório,pós-operatório(trêsmeses)epós-operatóriotardio(cinco aoitoanos).Angulac¸õesmaioresdoque30◦nasarticulac¸õesmetacarpofalangeanase15◦
nasinterfalangeanasproximaisforamconsideradascomorecidivacirúrgica.
夽
Pleasecitethisarticleas:GuilhenTA,VieiraABM,deCastroMC,HirataHH,MachadoIR.Avaliac¸ãodotratamentocirúrgicodadoenc¸a deDupuytrenpelatécnicadapalmaabertamodificada.RevBrasOrtop.2014;49:31–36.
夽夽
StudyconductedatInstitutoJundiaiensedeOrtopediaeTraumatologia,Jundiaí,SP,Brazil.
∗ Correspondingauthor.
E-mail:tguilhen@hotmail.com(T.A.Guilhen).
2255-4971/$–seefrontmatter©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditoraLtda.Allrightsreserved.
Resultados: obtivemosumamédiadedéficitdeextensãode6,3◦ aoníveldaarticulac¸ão
metacarpofalangeana,13,8◦nainterfalangeanaproximale1,9◦nainterfalangeanadistal.
Conclusão:atécnicadapalmaabertamodificadaéummétodoeficaznotratamentocirúrgico dascontraturasgravesnadoenc¸adeDupuytren.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Todososdireitosreservados.
Introduction
Dupuytren’s disease was named after Baron Guillaume Dupuytren,1 a celebrated French surgeon, whose complete
monographguidedthecurrentknowledgeofthispathology.In 1831,Dupuytrendescribedthediseaseasan anatomopatho-logicalchange,withthickeningandretractionofthepalmar fasciawithflexiondeformityofthefingers.Thismonograph associatedthediseasetolocalchronictraumaonthepalm, usuallyrelatedtoheavyduty.ButDupuytrencautionedthat notallcasescouldbeexplainedthisway.
Theconditionisduetometaplasiaofthepalmarfascia fibrous framework, which basically compromise the pre-tendinousband,superficialtransverseligament,spiralband, natatoryligament,lateralsagittalligament,andGrayson’s lig-ament.
TheDupuytren’scontracturefollowsaprogressive evolu-tion,anditsinitialmanifestationsareaninvaginationofthe skinandtheappearanceofnodulesthatuniteamongthem, forminghardconsistencycordsinthe palmandadvancing longitudinallytothefinger.Theconditionisusuallypainless, andafteritsmaturationmaysufferretractions,whichcausea flexiondeformityofthemetacarpophalangeal(MCP)and prox-imalinterphalangeal(PIP)joints.Theconditionaffectsmore menthanwomen(rangingfrom7:1to10:1),fromthefourth tosixth decadeoflife;and the fourthand fifthfingersare themostcommonlyaffected.Additionally,theremaybean associationwiththeformationoffibrousstrandsinthe plan-tarfascia(Lederhose’s disease,5%) andinthepenilefascia (Peyronie’sdisease,3%).2
Itsetiologyisstillunknown,buttheimportanceofheredity was proved,because ofthe high incidence inthe descen-dents of northern Europe. The condition is even known as “disease of the Vikings”. Its inheritance is autosomal dominant with reduced penetrance in women. There is a significant associationwithepilepsy, diabetes,trauma, and alcohol intake, and no evidence that it is an occupational disease.2–4
The anatomopathologic aspect is that of an aggressive lesion,displaying alargenumberofcellsandmitoses. The basiccellpresentisthemyofibroblast(similartofibroblast), usuallyfoundinthepalmarfascia,butwithsignificantability togeneratecontractileforces.Thetransforminggrowthfactor
(TGF-)isanabundantcytokinepresentinthetissue,being largely responsible for the proliferation and differentiation offibroblastsintomyofibroblasts.Moreover,itimprovesthe contractilebehaviorofmyofibroblastsandcausesrapidand strongercontractionsinresponsetomechanicalstimuli.2,5
Otherfactorsinfluencingthedifferentiation,growth,and contractility ofmyofibroblasts includeplatelet-derived pro-tein, fibroblastgrowth factor,epidermal growth factor,and
interleukin-1, as well as cells that synthesize the proteins periostinandtenascin.5
Thediagnosisisclinical,beingestablishedbyinspection andpalpation.Thedifferentialdiagnosisincludes acampto-dactilia,rheumatoidarthritis,retractionofthescarcausedby burnorinjury,palmarcallusofeffort,andulnarnervedeficit.5
Comparedtoconservativetreatment,themostpromising therapyistheapplicationofintrafocalclostridiumcollagenase inthecord,nowinanadvancedclinicaltrialphase.5
Nowadays,thesurgicaloptionisthemostacceptable.In the developmentofthetherapeuticplan,it isimportantto determinethestageatwhichthediseaseis,asthis knowl-edgeinfluencestheintraoperativetechnicaldifficultyandin the post-operativecomplications,aswell astherecurrence ofthedisease.Theneedformoreextensivedissection,the devitalizedskinandtheexcessivetensiononthesutureare predisposingfactorsforpost-operativecomplications,suchas hematomata,skinnecrosis,infectionandpain.5,6
The original surgical treatment was the removalof the contractedfascia;sincethen,varioustechniquesand modi-ficationshavebeendescribed:fasciotomy,dermofasciotomy withskingraft,regionalfasciotomy,radicalfasciotomy,open palmtechnique,partialfasciotomywithpreservationofthe skin,limitedfasciotomy,segmentalaponeurectomy,and per-cutaneousfasciotomy.1,4,6–10
In the open palm technique, originally described by Dupuytren1 and popularized by McCash,7 a regional
fas-ciotomy in the palm of the hand is done, allowing the extensionofthefingers.Thisprocedureresultsinalargeskin defect.Thewoundisleftopentohealbysecondaryintention, toavoidstressand hematomaiformation;this reducesthe incidenceofnecrosisandthepossibilityofinfectionandscar adhesions.6
Objective
Theobjectiveofthisstudyistoevaluatetheresultsofsurgical treatmentofpatientswithDupuytren’sdiseasegradesIIIand IVoperatedinourdepartmentwiththeuseoftheopenpalm technique(McCash)modifiedwiththeassociationof proxi-malanddistallongitudinalincisionalextensionsonthepalm, besidesBrunnerincisionsinthefingers.11
Materials
and
methods
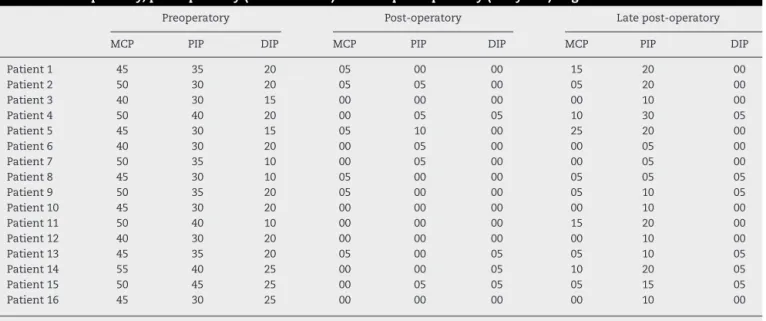
Table1–Preoperatory,post-operatory(threemonths)andlatepost-operatory(5–8years)angulation.
Preoperatory Post-operatory Latepost-operatory
MCP PIP DIP MCP PIP DIP MCP PIP DIP
Patient1 45 35 20 05 00 00 15 20 00
Patient2 50 30 20 05 05 00 05 20 00
Patient3 40 30 15 00 00 00 00 10 00
Patient4 50 40 20 00 05 05 10 30 05
Patient5 45 30 15 05 10 00 25 20 00
Patient6 40 30 20 00 05 00 00 05 00
Patient7 50 35 10 00 05 00 00 05 00
Patient8 45 30 10 05 00 00 05 05 05
Patient9 50 35 20 05 00 00 05 10 05
Patient10 45 30 20 00 00 00 00 10 00
Patient11 50 40 10 00 00 00 15 20 00
Patient12 40 30 20 00 00 00 00 10 00
Patient13 45 35 20 05 00 05 05 10 05
Patient14 55 40 25 00 00 05 10 20 05
Patient15 50 45 25 00 05 05 05 15 05
Patient16 45 30 25 00 00 00 00 10 00
MCP,metacarpophalangeal;PIP,proximalinterphalangeal;DIP,distalinterphalangeal.
unilateral,withinvolvementofthefourthandfifthfingers. ThirteenpatientsweremaleCaucasians,includingthethree women.
Inourstudy,weusedtheclassificationproposedbyTubiana etal.,12 whichconsistsofthe sumoftheextensiondeficits
ofthemetacarpophalangeal(MCP),proximalinterphalangeal (PIP),anddistalinterphalangeal(DIP)joints,measuredwith agoniometer.Thisclassificationisdividedintofourstages: gradeI(0–45◦),gradeII(46–90◦),gradeIII(91–135◦),andgradeIV
(>135◦).Inthisstudy,wereincludedonlypatientswithGrades
IIIandIV,anditwastakenintoaccountonlythefingerwith greaterinvolvement.11,12
Inallpatients,thesurgicaltechniqueusedwasthat rec-ommendedbyMcCash,withtransverseincisioninthedistal palmarcrease,associatedwithamodificationwithproximal anddistallongitudinalincisionalextensionsonthepalm.In thefingers,Brunnerincisionsweremade.Wemadeapartial fasciotomy,whichleftopenonlythetransverseincision.4
Post-operativecareconsistedofdailydressingchanges dur-ingthefirst48h,dailychangesinthenext twoweeks,and everythreedaysinsubsequentweeks.Thefingerswere immo-bilizedinextensionforthefirstfivedaysandthepatientwas referredforearlychirotherapyrehabilitation.
Theextensiondeficits forMCP, PIP, and DIPjoints were gaugedinpreoperative,post-operative(threemonths)andlate post-operativeperiods(5–8years).Extensiondeficits exceed-ing30◦inMCP,15◦inPIP,and10◦inDIPjointswereconsidered
assurgicalrecurrences.11,12
Results
Table1lists the measurementsofthe extensiondeficit, in
degrees,ofthethreejoints(MCP,PIP,andDIP)obtainedwitha goniometer.
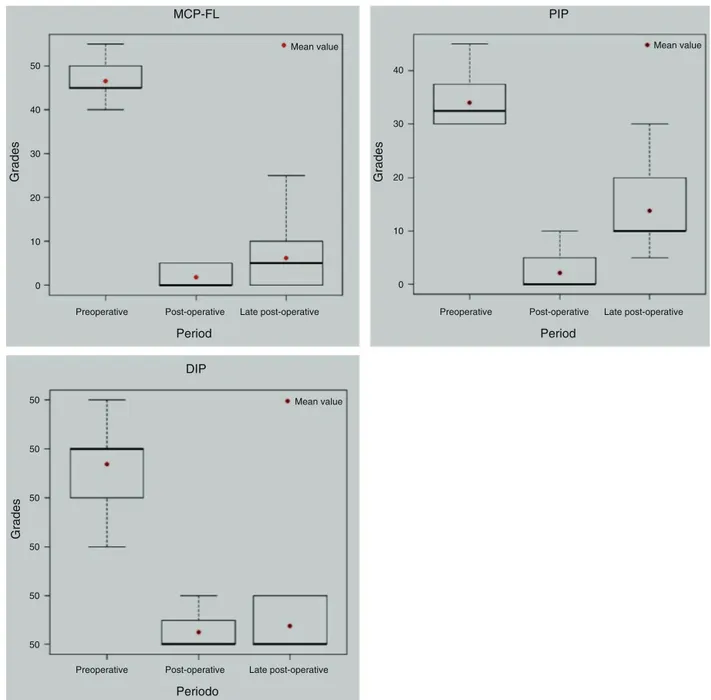
Fig.1displaystheresultsofmeasurementsoftheextension deficitsineachjointinthepre-,post-,andlatepost-operative period.
Tocompare the angleofthe MCP,PIP, andDIP jointsof patients withrespectto preoperative,post-operative(three months)andlatepost-operativeperiod(5–8years),weapplied the non-parametric statistical test of Mann–Whitney for pairedsamples,andthepvalueswerecorrectedbyBonferroni methodformultiplecomparisons.Table2showstheresults ofthetests.
Forthethreejoints,astatisticallysignificantdecreasewas observedfortheaverageangleofthepre-topost-operative period,atthelevelof5%(p<0.05).FortheMCPandDIPjoints, no significantdifference betweenthepost-operativeperiod (threemonths)andlatepost-operativeperiod(5–8years)was noted.However,forthePIPjointasignificantmeanincrease betweenthe post-operativeand latepost-operativeperiods vas noted (p=0.0025), but still ata lower value than that observedpreoperatively.
Fig. 2displays the scatter plotand the Spearman’s cor-relation coefficient among the joints for the angulations measured.Astrongpositivecorrelationamongmeasuresof differentjoints,withcoefficientsbetween0.75and0.85 (all statisticallysignificant,p>0.0001)wasnoted.
Table2–ResultsoftheMann–Whitneytestfor comparisonofmeasurementsofthejointsbetween periods.
Comparisons pa
MCP-FL PIP DIP
Pre×post 0.0012 0.0013 0.0012
Pre-×post-late 0.0012 0.0013 0.0012
Post-×post-late 0.1020 0.0025 1.0000
PIP,proximalinterphalangeal;DIP,distalinterphalangeal.
pvalueslessthan0.05indicatesignificantdifferenceatthe5%level. a pvaluescorrectedbytheBonferronimethodformultiple
PIP MCP-FL
DIP Period Preoperative
50
50
50
50
50
50
50
40
30
20
10
0 40
30
20
10
0
Post-operative Late post-operative
Periodo
Preoperative Post-operative Late post-operative
Period
Preoperative Post-operative Late post-operative Mean value
Mean value
Mean value
Grades
Grades
Grades
Fig.1–Boxesforthejointangulation,accordingtothejointandbyperiod.Inthisfiguretheresultsofmeasurementsofthe extensiondeficitsineachjointinthepreoperative,post-operative,andlatepost-operativeperiodaredepicted.
Spearman correlation =0,8586
40
25
20
15
10
5
0
25
20
15
10
5
0
0
10 20 30 40 50 0 10 20 30 40 50 0 10 20 30 40
30
20
10
0
MCP-FL
MCP-FL DIP
PIP DIP DIP
Spearman correlation =0,7844 Spearman correlation =0,7558
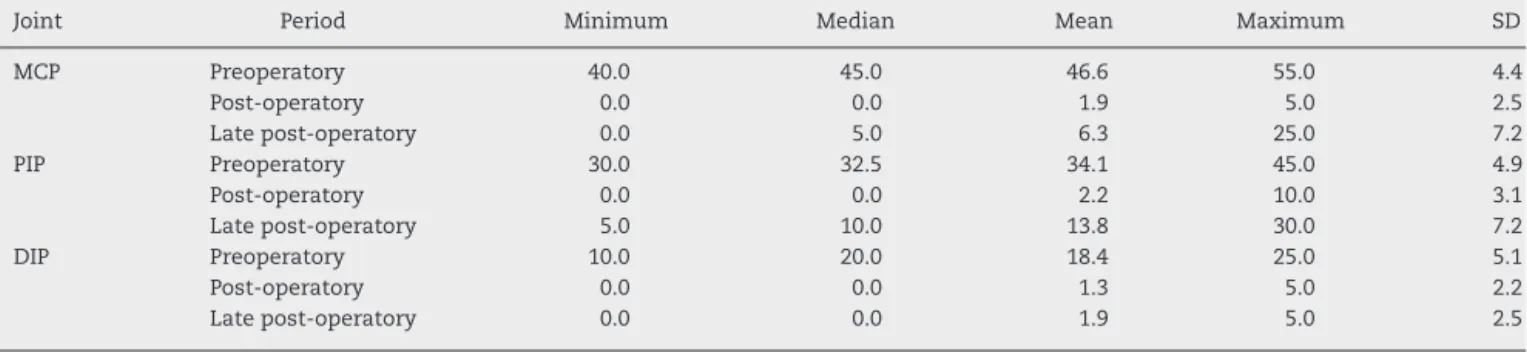
Table3–Valuesofminimum,median,mean,maximumandstandarddeviation(SD)fortheangulationofthejoints, accordingtojointandperiod.
Joint Period Minimum Median Mean Maximum SD
MCP Preoperatory 40.0 45.0 46.6 55.0 4.4
Post-operatory 0.0 0.0 1.9 5.0 2.5
Latepost-operatory 0.0 5.0 6.3 25.0 7.2
PIP Preoperatory 30.0 32.5 34.1 45.0 4.9
Post-operatory 0.0 0.0 2.2 10.0 3.1
Latepost-operatory 5.0 10.0 13.8 30.0 7.2
DIP Preoperatory 10.0 20.0 18.4 25.0 5.1
Post-operatory 0.0 0.0 1.3 5.0 2.2
Latepost-operatory 0.0 0.0 1.9 5.0 2.5
MCP,metacarpophalangeal,PIP,proximalinterphalangeal,DIP,distalinterphalangeal.
Thistablepresentsdescriptivemeasuresofdeficits.Clearlyoccursadecreaseintheangleofthejointsinallpatientsaftersurgery.
Discussion
Theliteratureiscontroversialastotheadvantagesand dis-advantagesofthe openpalm technique,whichdetermines moreskinstretching,besidespreventingcomplicationssuch ashematoma,necrosis,skinischemia,tensionand pain. A disadvantagewouldbeanincreasedriskofinfectionandthe patient discomfort byhaving an “open” injury and by the necessityofmore frequentdressings. Lubahn et al.13
con-ductedacomparativestudybetweenthetwotechniquesand concludedthatpatientsoperatedbytechniquesinwhichthe palmwascompletelyclosedcametosuffergreaterresidual contracture.8,13,14
Inthepresentstudy,13(81.25%)malesandthree(18.75%) females were recruited, all Caucasians, which is consis-tent with the literature, which reports 80% of male and dominance of Caucasians. In this study, the mean age of patientswas65years(range,54–75),similartothatofmost studies.15,16
Inourstudywefound37.5%ofsurgicalrecurrence.These ratesvarywidely(28–50%),regardlessofthetechniqueused. However,toobtaingoodresultsthepatientmusthavean ade-quate post-operativecare,and anstimulus forearly active mobilizationafterremovalofimmobilization,under orienta-tionofachiropractor.McGroutherismostemphaticthat,ina long-termpost-operativeperiod,therecurrenceratereaches 100%forsomedegreeofcontracture.Thisfactoccursbecause thereisaresidualpathologicalfascia,orwhatiscalledthe extentofthedisease,inwhichthereistheformationofnew fasciainaplacenearthesurgicalsite.12,17,18
RecurrenceinMCPjoint isvery low.Ontheother hand, inPIPjointtheincidenceofrecurrenceishigher.Ourstudy describedsixcasesofsurgicalrecurrence,allinthePIPjoint, becauseofanangulation>15◦inthelatepostoperativeperiod
(5–8years),whichagreeswiththeliterature.9,19
Concerning MCP and DIP joints, no significant differ-encesintheangulations betweenthepost-operativeperiod (three months) and late post-operative period (5–8 years) wereobserved.However,forthePIPjointtherewasa signifi-cantmeanincreaseinangulationbetweenthepost-operative (mean,2.2◦) and late post-operative (mean, 13.8◦) periods,
whichshowsahigherrateofrecurrenceinthePIPjoint–also observedinotherworks.9,19
Anextensiondeficit decreaseforallpatients inthetwo postoperative periodscompared tothe preoperativeperiod was observed, which is shown in the boxes (Fig. 1). This demonstratestheeffectivenessoftheopenpalmtechnique (modified),providedthereisanappropriatetherapeuticplan, whichisconsistentwiththeliterature.5,6
Incomparingthethreejointsinthethreeperiods(Table3), onlythePIPjointshowedsignificantmeanincreasebetween the post-operative and late post-operative periods, which demonstrateahigherrecurrence inPIP,alsoevidentinthe literature.9,19
Conclusion
The modified McCash technique is an effective option for severecases(stagesIIIandIV)ofDupuytren’sdisease.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.DupuytrenG.Delaretractiondesdoigtsparsuite
d’uneaffectiondel’aponeurosepalmaireDescriptiondela
maladie.Operationchirurgicalequiconvientdansdecas.J
UnivHebdMedChirprat.1831;5:352–65.
2.BarrosF,BarrosA,AlmeidaS.EnfermidadedeDupuytren:
avaliac¸ãode100casos.RevBrasOrtop.1997;32(3):
177–83.
3.GalbiattiJA,FioriJM,MansanoRT,DuriganJuniorA.
TratamentodamoléstiadeDupuytrenpelatécnicadeincisão
longitudinalreta,complementadacomz-plastia.RevBras
Ortop.1998;31(4):347–50.
4.SkoogI.Dupuytren’scontracture:pathogenesisandsurgical
treatment.SurgClinNorthAm.1967;47(7):433–44.
5.BlackME,BlazarPE.Dupuytrendiseaseanenvolving
understandingofanage-olddisease.JAmAcadOrthopSurg.
2011;19(2):746–57.
6.BryanAS,GhorbalMS.Longtermresultofclosedpalmar
fasciotomyinthemanagementofDupuytren’scontracture.J
HandSurgBr.1988;13(3):254–7.
7.McCashCR.TheopenpalmtechniqueinDupuytren’s
8. HuestonJI,WolfeI.DigitalgraftsinrecurrentDupuytren’s
contracture.PlastReconstrSurg.1962;29:342–4.
9. McFarlaneRM.Dupuytren’scontracture.In:GreenDP,editor.
Operativehandsurgery.NewYork:ChurchillLivingstone;
1993.
10.HamlinJR.LimitedexcisionofDupuytren’scontracture.Ann
Surg.1952;135:94–7.
11.TubianaR.Theprinciplesofsurgicaltreatmentof
Dupuytren’scontracture.GEMMonography.1974:
123–8.
12.TubianaR,FahrerM,McCulloughMA.Recurrenceandother
complicationsinsurgeryofDupuytren’scontracture.Clin
PlastSurg.1981;8(1):45–9.
13.FreitasAD,PardiniAG,NederAL.ContraturadeDupuytren:
tratamentopelatécnicadapalmaaberta.RevBrasOrtop.
1997;32(4):301–4.
14.LubahnJD,ListerGD,WolfeI.FasciotomyandDupuytren’s
disease:acomparisonbetweentheopenpalmandwound
closure.JHandSurg.1984;9(1):53–8.
15.McFarlaneRM.ThecurrentstatusofDupuytren’sdisease.J
HandSurgAm.1983;85Pt2:703–8.
16.LambDW.Thepracticeofhandsurgery.London:Blackwell
ScientificPublication;1981.
17.HuestonJI.RecurrentDupuytren’scontracture.PlastReconstr
Surg.1962;31:66–9.
18.McFarlaneRM.Patternsofthediseasedfasciainthefingersin
Dupuytren’scontracture.PlastReconstrSurg.
1974;54(1):31–44.
19.TonkinMA,BurkeFD,VarianJP.Surgicaltreatmentof
Dupuytren’scontracture:acomparativestudyoffasciectomy
anddermofasciectomyinonehundredpatients.JHandSurg