Clinical
Paper
Orthognathic
Surgery
Does
pterygomaxillary
disjunction
in
surgically
assisted
rapid
maxillary
expansion
influence
upper
airway
volume?
A
prospective
study
using
Dolphin
Imaging
3D
J.RoˆmulodeMedeiros,M.FerraroBezerra,F.W.GurgelCosta,T.PinheiroBezerra, C.R.deArau´joAlencar,E.C.StudartSoares:Doespterygomaxillarydisjunctionin surgicallyassistedrapidmaxillaryexpansioninfluenceupperairwayvolume?A prospectivestudyusingDolphinImaging3D. Int.J.OralMaxillofac.Surg.2017;46: 1094–1101. ã2017InternationalAssociationofOralandMaxillofacialSurgeons.
PublishedbyElsevierLtd.Allrightsreserved.
J.RoˆmulodeMedeiros1,M.Ferraro Bezerra2,F.W.GurgelCosta2, T.PinheiroBezerra3,C.R.deArau´jo Alencar4,E.C.StudartSoares2
1
DivisionofOralandMaxillofacialSurgery, FederalUniversityofCeara´,Universityof Fortaleza,Fortaleza,Brazil;2DivisionofOral andMaxillofacialSurgery,WalterCantı´dio UniversityHospital,FederalUniversityof Ceara´,Fortaleza,Brazil;3DivisionofOraland MaxillofacialSurgery,WalterCantı´dio UniversityHospital,FederalUniversityof Ceara´,UnichristusUniversityCenter, Fortaleza,Brazil;4PrivateOfficeofOraland MaxillofacialRadiology,Fortaleza,Brazil
Abstract. Surgicallyassistedrapidmaxillaryexpansionhasbeenusedforthe
treatmentoftransversemaxillarydeficiency.Thisprospectivestudyaimedto
evaluatetheeffectofthissurgery(withorwithoutpterygomaxillarydisjunction)on
the upperairwayvolume.Thepatientswererandomlydividedintotwogroups:
withoutpterygomaxillarydisjunction(PD)andwithpterygomaxillarydisjunction
(+PD).Elevenpatientspergroupwereestimatedtoobtainarepresentativesample
(90%ofpowerand95%ofconfidencelevel).Volumetricimagesofconebeam
computedtomographyscanswereobtainedpreoperatively,immediatelyafter
Hyraxscrewstabilizationand6monthsafterHyraxscrewstabilization.Volumetric
measurementsofthenasalcavity,maxillarysinuses,nasopharynx,andoropharynx,
andoftheminimumoropharynxcross-sectionalareawereobtainedusingDolphin
3DImaging Software.Thefinalsampleconsistedof25adultindividuals(+PD
group,n=12;PDgroup,n=13).Inthe+PDgroup,weobservedastatistically
significantincreaseimmediatelyafterHyraxscrewstabilizationforthe
nasopharynxvolume(P=0.003),oropharynxvolume(P=0.007)andoropharynx
cross-sectional area(P=0.001).Pterygomaxillarydisjunctionresultedina
significant(P<0.05)increaseinvolumetricmeasurementsofthenasopharynxand
minimum oropharynxcross-sectionalarea6monthsaftertheexpanderdevice
stabilization.
Keywords:palatalexpansiontechnique;nasal cavity;conebeamcomputedtomography.
Acceptedforpublication14April2017 Availableonline15May2017 http://dx.doi.org/10.1016/j.ijom.2017.04.010,availableonlineathttp://www.sciencedirect.com
Dentofacialdeformitiescanleadtochanges restrictedtothemaxilla,mandible,orreach bothjaws.Whentheytakeplace,theycan occurinthevertical,horizontal,and trans-versefacialplanes1.Fromthefacial defor-mities that affect the middle third, the transverse maxillary compression is the mostprevalentone2,anditcanoccuralone orlinkedtootherskeletalchanges3.Sucha conditionischaracterizedbythepresence ofskeletalconstrictionofthepalate,dental crowding,dentalrotations,andunilateralor bilateralposteriorcrossbite,withdeficitin thearcperimeter.Itis usuallyassociated withnasalbreathingdifficulties, hypertro-phyofadenoids,mouthbreathing,and mid-dleeardiseases4,5.
The treatment of this condition was initially described by Angell6, in 1860, and was reintroduced100 yearslater by Hass7. It advocatedtheexpansion ofthe median palatine suture by orthopaedic devices6,7.Theprocedurewascalledrapid maxillaryexpansion(RME)7.
Surgically assisted rapid maxillary expansions (SARMEs) are performed by osteotomies involving the areas of bone strengthofthefacialskeleton,suchasthe medianpalatinesuture,thezygomatic pil-lars andthe piriform aperture.Despitebeing consideredaresistancearea,the pterygo-maxillaries junctionsmayormaynot be separated duringSARME8. Such separa-tion,whenassociatedwiththeother osteo-tomies,allowsagreatermaxillaryposterior expansion9. Sygouros et al.10 concluded thatnon-performingpterygomaxillary dis-junction(PD)canresultingreaterrisksto theperiodontiumandtothemaxillarybone. Laudemann et al.11 recommendedPD in patientsabove20yearsold.
In2016,Bucketal.12conducteda meta-analysistoassesstheinfluenceofSARME intheupperairway.Theauthorsobserved a substantial volumetric increase in the nasalcavityintheshorttermandaweak evidenceofabsenceofeffectonthe oro-pharynx volume.They warnedaboutthe high riskof biasesin manyarticles and statedthatSARMEmustnotbeindicated tobreathinggain.
Periagoetal.13comparedtheaccuracy of cephalometric measurements carried out directly on human skulls withthose obtainedusing3Dvolumetric reconstruc-tionsbyconebeamcomputedtomography
(CBCT), employing Dolphin Imaging
software (version 2.3; Dolphin Imaging Management Solutions,Chatsworth,CA, USA). They concluded that the data obtainedcouldpresentstatistically signif-icant differences in anatomical
dimen-sions, although the software was
accurate for clinical use
(1.131.47%)oncraniofacialanalysis. ElandPalomo14,whenstudyingtheuse of software in 3D measurement of air-ways,concludedthattheDolphinImaging 3D (version 11, Dolphin Imaging Man-agementSolutions)presentedlow accura-cybutahighlevelofconfidenceandhigh correlationofresultswithothersoftware. Abramsonetal.15conductedastudywith theaimofevaluatingtheanatomyofthe upperairwaysthree-dimensionally.Todo so,theycomparedthecephalometric find-ings with data obtained from computed tomography (CT) images,employing 3D Slicersoftware.Thefollowingparameters were considered: volume, surface area, length, average cross-section area, mini-mumretroglossalarea,minimum retropa-latalareaandminimumcross-sectionarea. The authors concludedthatthe measures obtainedbycephalometryandbyusingthe softwarefromimagesobtainedbyCTwere reliable andreproducible.Theyalso con-cluded that the measureof the posterior airwayspacewastheonlyonethatshowed correlationwiththeparametersobtainedby CT.
Giventheabsenceofstudiesthatassess theinfluenceofpterygomaxillary disjunc-tionintheairwaysandbasedonthe hypoth-esis that the changes resulting from SARMEcanresultindimensionalchanges intheupperairways,theaimofthisstudy wastotestthehypothesisthatthe perfor-manceofpterygomaxillarydisjunction
as-sociated with SARME promotes an
increaseinthevolumeoftheupperairways.
Materialsandmethods
Outlineofthestudyandparticipants
Thisisaclinical,prospective,unicentric, randomized and double-blind test, ap-provedbytheResearchEthicsCommittee (Protocol no. 064.06.11), in accordance with the Helsinki Protocol. All patients gavefreeandinformedconsent.Thestudy wasconductedwithpatientsofbothsexes, agedbetween18and45years,with skel-etaltransversemaxillarydeficiency super-iorto5mm,unilateralorbilateralskeletal crossbite,without activeperiodontal dis-easeortoothmobilityintheteeth consid-eredaspillarsforfixingtheHyraxscrew, andneedingSARMEundergeneral anaes-thesia. We excluded patients who were syndromic, smokers, with a history of facialmiddlethirdfractures,withchronic systemic diseases, or using medications with influence on the bone metabolism, aswellaspatientswithtumoursoracute diseases inairwaysviewedby
nasofibro-scopy(J.L.B.,otolaryngologist collabora-tor)andCT.Inaddition,patientswhodid not return for the revaluations were re-movedfromthisstudy.
Interventions
All patients went submitted to SARME undergeneralanaesthesia,andwere oper-atedbythesameteamoforaland maxil-lofacial surgeons (E.C.S.S. and J.R.M.). The operative technique consisted of osteotomy typeLeFortI, usingno. 703 drills,withoutpromotingtheloweringof the maxilla, in addition to the use of osteotomy inmidline withdrill no.701, and a chisel and hammer. One group (+PD)hadsurgicalpterygomaxillary dis-junction but the other group (PD) did not.TheHyraxscrewwasactivatedinthe perioperative period until the maximum openingandemergenceofdiastema;then it was disabled, with a permanent four-quartersofaturn16.
The progressive Hyrax screw activa-tionswereinitiated6daysafterthe surgi-cal procedures, following a value of 0.5mm/day and arate ofone-quarterof aturnofthescrew,twiceaday.Afterthe totaluncrossingofthebitewith overcor-rection,thedeviceswerestabilized for6 monthsusinga0.25-mmligaturewire16.
Assessmentofoutcomes
The primary outcome adopted for this study was the increase inthe upper air-waysvolume,andthesecondaryoutcome wastheincreaseintheoropharynx cross-sectionalarea.
For themeasurement ofoutcomes,all patientsunderwenttestsbyconebeamCT usingani-CATdevice(ImagingSciences International,Hatfield,PA,USA)withthe followingparameters:3–8mA,120kVp, field of view 2216cm, and voxel 0.4mm. The tests had a field of view comprisingtheglabellatothefourth cer-vical vertebra (vertical) and from the acoustic meatus to point A (horizontal). The tomographic tests were performed withthepatientsinanaturalheadposition, with the tongue resting on the palate, avoidingbreathing orswallowingduring the examination.Thepatientsunderwent CTatthreetimes:preoperative(T1),after theactivationperiodpost-SARME,which was verified withthetotaluncrossingof thebitewithovercorrection(T2),andafter 6 months of Hyrax screw stabilization (T3). TheDICOM (Digital Imaging and
Communications in Medicine) files
11.5 (Dolphin Imaging & Management Solutions); measurements were taken blindly,bya dentalsurgeoncollaborator and imaging specialist (C.R.A.A.). Two measurements of each CT were carried out, withan intervalof15days,ofeach volumeandareaofinterest.
We obtained the nasal cavity volume
(NCV), the right (RMSV) and left
(LMSV) maxillarysinusvolume,the na-sopharynxvolume(NPV),theoropharynx volume(OPV),andtheoropharynx mini-mumcross-sectionalarea(OMCSA). Vol-umetric measures were given in cubic millimetres (mm3)and area measures in square millimetres (mm2). Before grey-scale variationwas found intheimages, we adopted a sensitivity (slice airway sensitivity) of 25 for the establishment of the airwayspace. Thelimits (bound-aries) ofeach measurewere definedand standardized according to Table 1. The
process of generating volumes and
OMCSAcanbeseeninFig.1.
Samplecalculation
BasedonthestudyofNadaetal.17,who observed a variation of average of 1.901.13,andusingaratioof1.5test patientspercontrol,weestimatedtheneed to assessa sampleof11 individualsper studygroup,toobtainasamplewith90% ofpowerand95%ofconfidence, forthe rejectionofthehypothesisofinvalidityof thisstudy.Beforethepossibilityofsample loss, we added 10% to this value and obtained a minimum of 12 patients per study group, to obtain a representative sample.
Randomization
Theblocked randomizationmethodwith four blocks was generated by Microsoft Excel 2013 (Microsoft, Seattle, WA, USA)usingthe‘‘randbetween’’function, sothateveryfournewpatientswehadthe impressionofanewsequence.Oneofthe co-authors(M.F.B)tookresponsibilityfor generatingtherandomizationsequenceof theenvelopes.Theenvelopeswereopened before each surgical procedure and the patientswereallocatedinoneofthetwo interventiongroups(+PDorPD).
Blinding
Thepatientswereblindedforthesurgical techniqueperformed,butitwas impossi-bletoblindthesurgeonforthetreatment method.Allthemeasurementsweretaken bythesameexaminer(C.R.A.),whodid not participateinthe operationsand did not know to which group the patient belonged(blindexaminer).Theresearcher wasalsoblind.Fortheanalysis,two mea-suresweretakenatanintervalof15days.
Statisticalanalysis
For thestatistical analysis,thedatawere submitted to the Kolmogorov–Smirnov normality test and analysed by one-way or two-way ANOVA tests for repeated measures,bothfollowedbytheBonferroni posthoctest.Theexhibitionofthevalues tookplaceintheformofmeanstandard error of the mean. We used GraphPad Prism 5.0 software for assessments and a95%confidenceintervalwasadoptedfor alltheanalyses.
Results
FromMarch2010toDecember2013,322 patientsvisitedthefacialdeformities out-patientdepartmentatauniversityhospital. Fromthe322individualsassessedduring recruitment of participants for the re-search, the facial deformities outpatient department evaluated 87 patients aged from17to49years old.Eighty patients had no transverse maxillary deficiency. One hundred and twenty-seven patients had this condition (<5mm), associated
or not with crossbite. Moreover, many ofthemfitinmorethanoneofthe exclu-sion criteria adopted. Twenty-eight patients wereinitially selectedin accor-dance withthe eligibilitycriteria of this study (Fig. 2). From these, three were excludedbecause tomographic examina-tionshadnotbeencarriedoutatanyofthe follow-upperiodspreviously established. Thesamplewascomposedof25patients, 19women(76%)andsixmen(24%).The agesrangedfrom17to49years,withan averageof 26.92years (2.919)for the +PDgroup(13patients)and27.50years (1.361)forthePDgroup(12patients). Theaverageagedidnotdifferbetweenthe groups(P=0.856).Inaddition,regarding the sample calculation proposed during theoutlineofthisstudy,weobservedthat inthe+PDgroupthevariationoftheright maxillarysinusvolumefromT1toT3was 5,204.8mm33,285.5mm3,whichgave thesampleof13patientsapowerof99.7% forrepresentingthealternativehypothesis. Inthegroupwithoutdisjunction,the pow-er was inferior, being 98.3% (n=12), considering the volume variation of 4675.4mm33699.9mm3 at the same
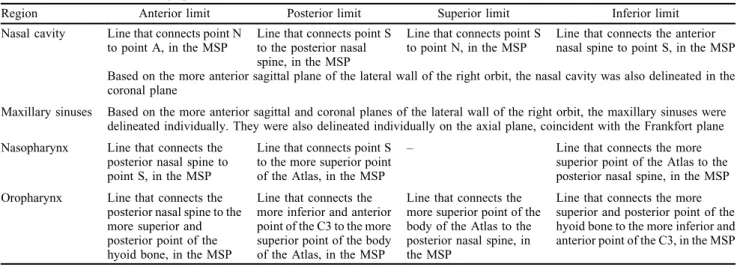
Table1. Definitionofthetomographicanatomicallimits.
Region Anteriorlimit Posteriorlimit Superiorlimit Inferiorlimit
Nasalcavity LinethatconnectspointN
topointA,intheMSP
LinethatconnectspointS
totheposteriornasal
spine,intheMSP
LinethatconnectspointS
topointN,intheMSP
Linethatconnectstheanterior
nasalspinetopointS,intheMSP
Basedonthemoreanteriorsagittalplaneofthelateralwalloftherightorbit,thenasalcavitywasalsodelineatedinthe
coronalplane
Maxillarysinuses Basedonthemoreanteriorsagittalandcoronalplanesofthelateralwalloftherightorbit,themaxillarysinuseswere
delineatedindividually.Theywerealsodelineatedindividuallyontheaxialplane,coincidentwiththeFrankfortplane
Nasopharynx Linethatconnectsthe
posteriornasalspineto
pointS,intheMSP
LinethatconnectspointS
tothemoresuperiorpoint
oftheAtlas,intheMSP
– Linethatconnectsthemore
superiorpointoftheAtlastothe
posteriornasalspine,intheMSP
Oropharynx Linethatconnectsthe
posteriornasalspinetothe
moresuperiorand
posteriorpointofthe
hyoidbone,intheMSP
Linethatconnectsthe
moreinferiorandanterior
pointoftheC3tothemore
superiorpointofthebody
oftheAtlas,intheMSP
Linethatconnectsthe
moresuperiorpointofthe
bodyoftheAtlastothe
posteriornasalspine,in
theMSP
Linethatconnectsthemore
superiorandposteriorpointofthe
hyoidbonetothemoreinferiorand
anteriorpointoftheC3,intheMSP
surgical times. In both cases, the confi-denceadoptedwasof95%.
Regarding the measurements carried out,weobservedastatisticallysignificant differencebetweentheperiodsof
assess-ment of this study only for NPV
(P=0.003), OPV (P=0.007), and OMCSA (P=0.001) in the +PD group. ConsideringtheNPVandOMCSAofthis group,weobservedstatisticallysignificant differencebetweenT2andT1(P<0.05),
aswellasbetweenT3andT1(P<0.05).
RegardingtheOPV,weobserved signifi-cantdifferencebetweenT2andT1when thepterygomaxillarydisjunctionwas car-riedout(P<0.05).Besides, bothinthe PDgroupandintheintergroup compar-isons,wedidnotfindstatistically signifi-cantdifferences.Theaccumulatedvolume oftheairways,whichrepresentsthetotal volume, calculated usingthe sumofthe
NCV, RMSV, LMSV, NPV, and OPV,
also did not differ significantly
(P=0.983) at the three times when we comparedthegroupswithandwithoutPD (Table2).
Discussion
In a recent systematic review, a great diversity ofmethodologies forthe volu-metricevaluationoftheupperairwayswas observed, whichgenerates some difficul-ties comparing the results ofsuch stud-ies12.Sincethereisnostandardizationof theanatomicalreferencesused instudies performing volumetric measurements of upperairways usingCBCT andDolphin Imaging3Dsoftware,thisresearch estab-lishedthelimitsofeachregionbasedon previouslypublishedstudies18–20.Despite thedifficultiesfoundintheuseofDolphin Imaging3Dforthispurpose,weconsider that the methodology used in this study was easy to standardize and implement, allowing acquisition ofreproducible and comparable measures between the times studied,aswellaswithotherstudies. Gui-jarro-Martinezetal.21,inasystematic re-view conducted in 2011,highlighted the followingadvantagesofthistypeof meth-odology: speed, absence ofinvasiveness, lowdoseofradiation,andeasyaccessibility
totheminimumcross-sectionalareaandthe volumetricmeasuresoftheupperairways. Ina study witha sample of 27 adult patients in which acoustic rhinometry, rhinomanometry, orthodontic measures, andavisualanaloguescalewereused,a statisticallysignificantincreaseinthe na-salcavitycross-sectionalareaandvolume after SARMEwithpterygomaxillary dis-junction was observed22. Such findings were not observed inthis study, despite theslightvariation foundintheNCVof the+PDgroupandthelargeincreasesin NCV observed in some patients ofboth groups. Buck etal.12, in2016, in agree-ment withthis study, stated thatthe PD doesnotseemtoinfluencetheNCV.
Magnusson et al.23 assessed cases of SARMEbyacousticrhinometryand con-cluded that the effects produced by SARME without PDonthe nasal cavity ofadult patientswere representedbyan increase in the posterior cross-sectional area. Tsolakis et al.24, when comparing CBCT and acoustic reflection (acoustic rhinometryandacousticpharyngometry),
Fig.1. ObtainmentoftheOMCSAvolumesbyDolphinImaging3D.(A,B)Definitionofthenasalcavitylimitsinthemidsagittalandcoronal
planes;(C)volumetricreconstructionofthenasalcavity;(D)definitionofthemaxillarysinuslimitsintheaxialplane;(E,F)definitionoftheright
maxillarysinuslimitsinthecoronalplane,withvolumedefinitionandvolumetricreconstruction;(G,H)definitionofthenasopharynxlimits,with
volumedefinitionandvolumetricreconstruction;(I)definitionoftheoropharynxlimitsandvolume;and(J)OMCSAvolumetricreconstruction
concludedthatCBCTisanaccurate meth-od for measuringthe anterior nasal vol-ume, nasal minimal cross-sectional area, pharyngealvolume,andpharyngeal mini-mal cross-sectional area. Nada et al.17 stated that, because of the nasal cavity anatomy, largerdimensionalchanges oc-cur in the posterior region than in the anterior region.Thus,asmallamountof posteriorexpansionleadstoalargechange involume.ThestatementofNadaetal.17 helps explain the significant increase of NPV foundinthisstudy,sincethespace createdbySARMEbetweenthe
horizon-tal blades of the palatine bones could cause a posterior volumetric increase and, consequently, a greater NPV. Al-thoughnasaldecongestionpriortoCBCT
examinations was not adopted, we
obtainedtheapproximatedrealnasal cav-ityvolumeusingastandardizedslice air-way sensitivity aiming to compare the airway space volume before and after theSARME.Theuseofanasal deconges-tanthasnotbeenperformedasobservedin similar studies evaluating the upper
air-way through a CBCT
methodolo-gy18,20,21,25. In a CBCT study by
Alsufyanietal.26 withoutpriornasal de-congestion,althoughitwasobservedthat thickening and/or a pathological condi-tion-relatedmucosalabnormality can af-fect the imaging segmentation method, this does not render significant clinical repercussionsinallcases.
Smith etal.18 carriedouta study that usedamethodologysimilartoours.They assessed 20 patients with ages ranging between8 and 15years oldwho under-went non-surgical treatment by RME, withafollow-upof3months,andfound a statistically significant increase in the nasal cavity and nasopharynx volumes. Another study that employed the same age range and postoperative follow-up interval, using acoustic rhinometry, showed an increase in the nasal cavity inareaandvolume27.Thus,itis impres-sivethataconservativetreatmentsuchas RMEcan causea significantincrease in thesevolumes,sinceeventhePDgroup of this study did not show significant increase.It is possible to assigntosuch eventthefactthatallthepatientsincluded inthisstudywereadults,withno interfer-encefromthephysiologicalfacialgrowth inthevolumetricchangesfound.Langer et al.28 concluded, usingacoustic
rhino-metryandrhinomanometry,thattheRME did not affect the nasopharynx area or nasalairwayresistanceinthelongterm, andstressedtheinfluenceoffacialgrowth intheirfindings.
Asnotedbyotherauthors18,therewas notasignificantincreaseinthemaxillary sinusesvolumeafterthemaxillary expan-sions.Thispossiblyoccursbecauseofthe rotationalmovementpatternofthe hemi-maxillas29.Thus,therewouldbeachange ontheformofthemaxillarysinuswithout significantinvolvementofthe sinus vol-ume.Inthiscontext,thereisascarcityof studiesonthechangesthatmayoccurin themaxillarysinusesafterSARME with orwithoutPD.Inthisstudy,weobserveda decreaseinthemaxillarysinusesvolume intheassessmentperiodT2,withreturnto theinitialvolume6monthsafterthe pro-cedure. In addition, although itwas not statistically significant, some patients showedhyperdenseimages involving al-mosttheentiretyofbothmaxillarysinuses inthepostoperativeperiod T2.Thiswas probablyaresultofthehemosinusfound asconsequenceofthesurgicalprocedures. Thisphenomenondirectlyinfluencedthe reduction of accumulated volume in T2 andrecoveryinT3.Thus,studiesonthe maxillary sinuses relating RME and SARMEmustconsiderthisfinding.
Thisstudyshowedasignificantincrease intheOPVofthe+PDgroupintheperiods
between T1 and T2. However, although stabilityhasoccurredinsomepatientsin thisgroup,therewasamarkedrelapseat theinitiallevelsinT3.Thus,thisis con-sistent with the studies of Pereira-Filho etal.19,whoalsodidnotfindastatistically significantincreaseintheOPV6months afterSARME+PD.Itisimportanttonote thatessentialstudiesinpatients undergo-ing growth also pointto the absence of gainintheOPV30.Anon-significant de-creaseintheOPVwasalsoobserved.The authorsattributedthistoapossibleinferior repositioningofthepalatalplane18.
Instudies basedontheuse ofimages obtainedbyCBCT,theOMCSAis influ-encedbythemaxillaryexpansions25. De-spite thefact thatthe OMCSAvariation intensitydidnotdifferinthetwogroupsof this study, we observed a significant in-crease(P<0.05)ofOMCSAinthe+PD
group between T1 and T2, aswell asa relapsetendencybetweenT2andT3.The samewasshowedbythestudyof Pereira-Filhoetal.19,whoalsoobservedan infe-rior dislocation of the OMCSA. In this study, thefound data diverged fromthe findings of the authors previously men-tioned,becauseweobservedasignificant increase(P<0.05)oftheOMCSAinthe
+PDgroupalsobetweenthepostoperative assessmentsT1andT3.
AlthoughthestudyofAkayetal.31has found asignificantgainofthe minimum distancefromtheposteriororopharynxto thetongueafterSARMEwithoutPDin16 adultpatients,inthisstudytherewas no significantincreaseoftheOMCSAinthe PDgroup.Itisplausibletoconsiderthat thisdivergencecanbeattributedto meth-odologicaldifference,sincetheyused lat-eralcephalometricradiographies.
TheincreaseofNPVandOMCSAafter SARME withPDobserved inthis study might have occurred because of three possibleconditions:
(1) Possible inferiorrepositioningofthe palatineplane18,whichisrepresented bytheline(boundary)thatdefinesthe limit between the nasopharynx and oropharynx, with a consequent ten-dency toincrease NPV anddecrease OPV proportionally,asnotedin this study. Thisfindingcouldbealso as-sociatedwithananteriordisplacement ofthemaxilla,inaccordancewiththe resultsfoundbyGu¨nbayetal32. Nev-ertheless, theseauthorsused a bone-bornedeviceanddidnotperformPD. (2) Cross-sectional increase of the hard palate31, considering that SARME +PDimplyamoreuniformposterior expansion33, with possible anterior repositioning and tensionofthe soft tissuesrelated.Abdullatifetal.34 per-formedameta-analysisandsuggested the same musculareffect. They also highlightedthepossiblerelationwith a decreaseinthe apnoea–hypopnoea index(AHI)andlowestoxygen satu-ration(LSAT)inpatientswithOSAS, mentioning the palatoglossus and palatopharyngeal muscles. We be-lieve that the other palate muscles mayreactinthesameway,sincethey alsohaveanintimateanatomical rela-tionshipwithupperairways. Accord-ing to Hickey35, the uvula muscle originates from the posterior nasal spine and from theuppersurface of the palatine aponeurosis, with inser-tionintheuvulamucosa,the palato-glossus muscle originates from the palatine aponeurosisandinsertion in thetongue;thepalatopharyngeal mus-cle originatesfromthe palatine apo-neurosisandfromtheposteriorborder ofthehardpalate,withinsertioninthe posterior border ofthe thyroid carti-lageandinthepharynx;thetensorveli palatini muscle originates from the scaphoid fossa and in the spine of sphenoid bone, with insertion in the palatine aponeurosis andinthe hard palate,andthelevatorvelipalatinihas origininthepetrouspartofthe tem-poralboneandinsertionintheupper surfaceofthepalatineaponeurosis. (3) Changeintongueposition31.Thisfact
was not observed after the RME18, possiblybecauseofthelower expan-sionintheposteriorregionofthepalate resultingfromthisnon-surgical modal-ity16,36, incontrastwith theSARME
+PD,whichseemstopromoteamore Table2. Descriptionofthevolumetricandareameasuresforeachgroup.
+PDgroup
(meanstandarderror)
PDgroup
(meanstandarderror) Py
NCV(mm3)
T1 28089.32095.4 28030.32419.8 0.321
T2 27096.41413.4 30382.52481.7
T3 27913.92073.4 28523.63164.5
P* 0.174 0.432
RMSV(mm3)
T1 18779.14769.4 18209.15089.6 0.996
T2 12574.91540.9 11520.21253.2
T3 14394.91510.9 13533.71389.7
P* 0.280 0.289
LMSV(mm3)
T1 13594.81048.6 12653.11384.2 0.811
T2 11654.21511.8 11486.61080.6
T3 13539.51306.3 12911.61341.0
P* 0.104 0.123
NPV(mm3)
T1 5245.1664.5 5825.1532.0 0.351
T2 6043.2666.8* 6105.4501.2
T3 5863.9784.5* 6176.7390.1
P* 0.003 0.415
OPV(mm3)
T1 14021.51504.0 12544.21289.8 0.423
T2 18178.72540.7* 14815.32071.8
T3 15568.72340.6 14269.91567.8
P* 0.007 0.181
Accumulatedvolume(mm3)
T1 79729.85992.2 77261.77396.6 0.983
T2 75547.45607.9 74309.95292.4
T3 77280.75486.3 75415.44671.8
P* 0.715 0.788
OMCSA(mm2)
T1 143.522.0 123.316.4 0.134
T2 210.531.9* 166.527.8
T3 159.226.1* 178.724.6
P* 0.001 0.105
NCV,nasalcavityvolume;RMSV,rightmaxillarysinusvolume;LMSV,leftmaxillarysinus
volume;NPV,nasopharynxvolume;OPV,oropharynxvolume;OMCSA,oropharynxminimum
cross-sectionalarea.
*
P<0.05versusT1,one-wayANOVAforrepeatedmeasuresaftertheBonferroniposttest.
y
P<0.05, two-way ANOVA for the repeated measures after the Bonferroni post test
uniformpalate expansion37. Changes
inthepositionofthehyoidbonethat influencethetongueposturewerealso suggestedafterRMEinadolescents38. Vinhaetal.39haveevidencedthatafter SARME+PDtherewasanincreaseof thetransversalsectionofthemedium regionofthepharynx(P=0.107)and inthe inferiorregion (P=0.0003).This effectmaybeattributedtoanincrease in the perimeter ofthedentalarchandin thebonebasestransversally, generat-ing an anterior displacement of the tongue in the oral cavity40,41. These findings corroborate the increase in theOMCSAfoundinourstudy.
Thisstudysuggeststhatsome improve-ments happened in thenasopharynx and oropharynx. Althoughthis studyhadnot aimed toassesspatientswithOSAS,the resultsofourresearchrelatedtoSARME +PDindicatethatafunctionalgainmay happen aspart of the treatmentfor this syndromeand inpatientswithmaxillary transverse compression, especially when theobstructionoccursinthelowerregion ofthepharynx.However,consideringthe methodologicaldesignofourstudy,itwas not possible to have evidences that SARME with pterygomaxillary disjunc-tion+PDmaybeanalternativeindicated for all patients with respiratory difficul-ties. This study agrees with the one by Bucketal.12,whoconcludedthatSARME should not be prescribed for respiratory issues.Thesix-monthfollow-upafter Hy-raxscrewstabilizationusedinthisstudy must also beconsidered, once Marchetti et al.42 reported 20–30% relapse after 2
years following SARME+PD. This
wouldeliminateallthegainachievedby expansioninthelongterm.Otherstudies with more follow-uptime must be con-ductedforabetterassessmentofthe pos-sible alterationsinthe palateandtongue musculatureafterSARME,withor with-outDP,inadditiontotheimpactofthison breathingandontheOSAStreatment.
The conduction of pterygomaxillary disjunction in association with SARME didnotprovidesignificantvolumetric in-crease in the nasal cavity, maxillary sinuses and oropharynx, as well as in the total volume of the upper airways. However, it resulted in significant volu-metricexpansionofthenasopharynxand oftheminimumcross-sectionalareaofthe oropharynx.Onthebasisofthefindingsof thisstudy,futureresearchesareimportant tocorrelatethequantitativedataof tomo-graphic trials concerning the volume of airwayswiththequalitativedataobtained byclinicalandfunctionalparameters.
Funding
None.
CompetingInterests
None.
Ethicalapproval
Thisisaclinical,prospective,unicentric, randomized and double-blind test, ap-provedbytheResearchEthicsCommittee (WalterCantidioUniversityHospital, Pro-tocol no.064.06.11), inaccordance with theHelsinkiProtocol.
Patientconsent
All patients signed a free and informed consentform.
Acknowledgements. We want to express our gratitude to Henrique Clasen Scar-paro,DDS,MSc,PhD,forhissupport.
References
1. AnttilaA,FinneK,Keske-NisulaK,Somppi M,PanulaK,Peltoma¨kiT.Feasibilityand long-termstabilityofsurgicallyassisted rap-id maxillaryexpansionwithlateral osteot-omy.EurJOrthod2004;26:391–5.
2. BettsN,VanarsdallRL, BarberHD, Hig-gins-Barber K,FonsecaRJ.Diagnosisand treatmentoftransversemaxillarydeficiency.
Int J Adult Orthod Orthognath Surg
1995;10:75–96.
3. AloiseAC,PereiraMD,HinoCT,Gragnani FilhoA,FerreiraLD.Stabilityofthe trans-versedimensionofthemaxillaafter surgi-callyassistedrapidexpansion.JCraniofac Surg2007;18:860–5.
4. Piccini A,GiorgettiR,Fiorelli G.Stenosi respiratoria nasaleedipoplasiamascellare. Modificazionidopotrattamentoortodoˆntico comespasionera´pidapalatale.Acta Otorhi-nolItal1989;9:375–80.
5. CoreyJP,HouserSM,NgBA.Nasal con-gestion:areviewofitsetiology,evaluation,
and treatment. Ear Nose Throat J
2000;79:690–8.
6. Angell EH. Treatment of irregularities of permanent or adult teeth. Dent Cosmos
1860;1.540–544,599–600.
7. HassAJ.Rapidexpansionofthemaxillary dentalarchandnasalcavitybyopeningthe
midpalatal suture. Angell Orthod
1961;31:73–90.
8. KoudstallMJ,PoortLJ,vanderWallKGB, Wolvius EB, Prahl-Andersen B, Schulten AJM. Surgically assisted rapid maxillary expansion(SARME):areviewofthe
liter-ature. Int J Oral Maxillofac Surg
2005;34:709–14.
9.Bays RA, Greco JM. Surgically assisted rapidpalatalexpansion:anoutpatient tech-niquewithlongtermstability.JOral Max-illofacSurg1992;50:110–3.
10.SygourosA,MotroM,UgurluF,AcaraA. Surgically assisted rapid maxillary expan-sion: Cone-beam computed tomography evaluation ofdifferent surgical techniques andtheireffectsonthemaxillary dentoske-letal complex. Am J Orthod Dentofacial Orthop2014;146:748–57.
11.LaudemannK,SantoG,RevillaC,HarthM, KoppS,SaderRA,LandesCA.Assessment ofsurgicallyassistedrapidmaxillary expan-sionregardingpterygomaxillarydisjunction using thinvolume-rendering technique:in varianceanalysisandinreliability,accuracy, and validity. J Oral Maxillofac Surg
2011;69:2631–43.
12.BuckLM,DalciO,DarendelilerMA, Papa-dopoulouAK.Effectofsurgicallyassisted rapidmaxillaryexpansiononupperairway volume: asystematicreview. JOral Max-illofacSurg2016;74:1025–43.
13.PeriagoDR,ScarfeWC,MoshiriM,Scheetz JP,SilveiraAM,FarmanAG.Linear accu-racyandreliabilityofconebeamCTderived 3-dimensionalimagesconstructedusingan orthodontic volumetricrenderingprogram.
AngleOrthod2008;78:387–95.
14.ElH,PalomoJM.Measuringtheairwayin3 dimensions:Areliabilityandaccuracystudy.
Am J Orthod Dentofacial Orthop
2010;137:50–2.
15.AbramsonZR,SusarlaS,TagoniJR,Kaban L.Three-dimensionalcomputed tomograph-icanalysisofairwayanatomy.JOral Max-illofacSurg2010;68:363–71.
16.GoldenbergDC,AlonsoN,GoldenbergFC, GebrinES,AmaralTS,ScanaviniMA, Fer-reira MC.Usingcomputedtomographyto evaluatemaxillarychangesaftersurgically assistedrapidpalatalexpansion.JCraniofac Surg2007;18:302–11.
17.NadaRM,vanLoonB,ScholJGJH,Maal TJJ,deKoningMJ,MostafaYA, Kuijpers-Jagtman AM. Volumetric changes of the nose andnasal airway2years aftertooth borne and bone-borne surgically assisted rapidmaxillaryexpansion.EurJ OralSci
2013;121:450–6.
18.Smith T, GhoneimaA,Stewart K,LiuS, EckertG,HalumS,KulaK. Three-dimen-sional computed tomography analysis of airwayvolumechangesafterrapidmaxillary expansion.AmJOrthodDentofacialOrthop
2012;141:618–26.
19.Pereira-Filho VA,Monnazzi MS, Gabrielli MAC,Spin-NetoR,WatanabeER,Gimenez CMM,Santos-PintoA,GabrielliMFR. Volu-metric upperairway assessmentinpatients withtransversemaxillarydeficiencyafter sur-gicallyassistedrapidmaxillaryexpansion.Int JOralMaxillofacSurg2014;43:581–6.
oftheupperairway:avalidationstudy.IntJ OralMaxillofacSurg2013;42:1140–9.
21. Guijarro-Martı´nezR,SwennenGRJ. Cone-beam computerized tomography imaging andanalysisoftheupperairway:a system-aticreviewoftheliterature.IntJOral Max-illofacSurg2011;40:1227–37.
22. ZambonCE,CecchetiMM,UtumiER, Pin-naFR,MachadoGG,PeresMPSM,Voegels RL. Orthodontic measurements and nasal respiratoryfunctionaftersurgicallyassisted rapidmaxillaryexpansion:anacoustic rhi-nometry and rhinomanometrystudy. Int J OralMaxillofacSurg2012;41:1120–6.
23. MagnussonA,BjerklinK,NilssonP, Jo¨ns-sonF,MarcussonA.Nasalcavitysize, air-way resistance, and subjective sensation aftersurgicallyassistedrapidmaxillary ex-pansion:A prospectivelongitudinalstudy.
Am J Orthod Dentofacial Orthop
2011;140:641–51.
24. TsolakysIA,VenkatD,HansMG,AlonsoA, Palomo M. When static meets dynamic: Comparingcone-beamcomputed tomogra-phyandacousticreflectionforupperairway analysis.AmJOrthod DentofacialOrthop
2016;150:643–50.
25. ChangY,KoenigLJ,PruszynskiJE,Bradley TG,BosioJA,LiuD.Dimensionalchanges ofupperairwayafterrapidmaxillary expan-sion: A prospective cone-beam computed tomographystudy.AmJOrthodDentofacial Orthop2013;143:462–70.
26. AlsufyaniNA,HessA,NogaM,RayN, Al-SalehMAQ,Lagrave`reMO,MajorPW.New algorithm for semiautomatic segmentation of nasal cavity and pharyngeal airwayin comparisonwithmanualsegmentationusing cone-beam computed tomography. Am J OrthodDentofacialOrthop2016;150:703–
12.
27. PalaisaJ,NganP,MartinC,RazmusdT.Use of conventional tomography to evaluate changesinthenasalcavitywithrapidpalatal expansion.AmJOrthodDentofacialOrthop
2007;132:458–66.
28. LangerMRE,ItikawaCE,ValeraFCP,
Mat-sumoto MAN, Anselmo-Lima WT. Does
rapidmaxillaryexpansionincrease
nasopha-ryngeal space and improve nasal airway resistance? Int J Ped Otorhinolaryng
2011;75:122–5.
29. KilicE,KilicB,KurtG,SakinC,AlkanA. Effectsof surgically assistedrapidpalatal expansion withand without pterygomaxil-larydisjunctionondentalandskeletal struc-tures:aretrospectivereview.OralSurgOral Med Oral Pathol Oral Radiol
2013;115:167–74.
30. ZhaoY,NguyenM,GoldE,MahJK, Same-shimaG,EncisoR.Oropharyngealairway changesafterrapidpalatalexpansion evalu-atedwithcone-beamcomputedtomography.
AmJOrthodDentofacOrthop2010;137:71–
8.
31. AkayMC,ArasI,Gu¨nbayT,ArasA.Does transpalataldistractionaffectpharyngeal air-waydimensionsandrelatedsofttissues?J OralMaxillofacSurg2014;72:1559–64.
32. Gu¨nbayT, AkayMC,Gu¨nbayS,ArasA, KoyuncuBO,SezerB.Transpalatal distrac-tion using bone-borne distractor: clinical observations and dental and skeletal
changes. J Oral Maxillofac Surg
2008;66:2503–14.
33. Mo¨hlhenrichSC,Modabber A,KamalM, FritzU,PrescherA,Ho¨lzleF. Three-dimen-sional effects of pterygomaxillary discon-nection during surgically assisted rapid palatal expansion:acadaveric study.Oral Surg Oral Med Oral Pathol Oral Radiol
2016;121:602–8.
34. Abdullatif J,Certal V,ZaghiS,SongSA, ChangET,GillespieMB,CamachoM. Max-illaryexpansionandmaxillomandibular ex-pansionforadultOSA:asystematicreview and meta-analysis. J Cranio-Maxillofac Surg2016;44:574–8.
35. HickeySA.HeadandNeck.In:StandringS, editor.Gray’sanatomy:theanatomicalbasis ofclinicalpratice.London:Elsevier;2005. p.627–8.
36. GoldenbergDC,GoldenbergFC,AlonsoN, GebrinES,AmaralTS,ScanaviniMA, Fer-reira MC. Hyrax appliance opening and patternofskeletalmaxillaryexpansionafter surgicallyassistedrapidpalatalexpansion:a computedtomographyevaluation.OralSurg
OralMed OralPatholOralRadiolEndod
2008;106:812–9.
37. LoddiPP,PereiraMD,WoloskerAB,Hino CT,KreniskiTM,FerreiraLM.Transverse effectsaftersurgicallyassistedrapid maxil-laryexpansioninthemidpalatalsutureusing computed tomography. J Craniofac Surg
2008;19:433–8.
38. PhoenixA,ValiathanM,NelsonS,Strohl KP,HansM.Changesinhyoidboneposition followingrapidmaxillaryexpansionin ado-lescents.AngleOrthod2011;81:632.
39. VinhaPP,FariaAC,XavierSP,ChristinoM, DeMelo-FilhoFV.Enlargementofthe phar-ynxresultingfromsurgicallyassistedrapid maxillaryexpansion.JOralMaxillofacSurg
2016;74:369–79.
40. Cistulli PA, Palmisano RG, Poole MD. Treatment ofobstructivesleep apnea syn-dromebyrapidmaxillaryexpansion.Sleep
1998;21:831.
41. IwasakiT,SaitohI,TakemotoY,InadaE, KakunoE,KanomiR,HayasakiH, Yama-saki Y. Tongue posture improvement and pharyngealairwayenlargementassecondary effectsofrapidmaxillaryexpansion:A cone-beam computed tomography study. Am J OrthodDentofacialOrthop2013;143:235.
42. MarchettiC,PironiM,BianchhiA,MusciA. Surgically assistedrapidpalatalexpansion vs.segmental Le FortI osteotomy: trans-versestabilityovera2-yearperiod.J Cra-nio-MaxillofacSurg2009;37:74–8.
Address:
Jose´ RoˆmulodeMedeiros FederalUniversityofCeara´ DepartmentofDentalClinic SchoolofDentistry
RuaAlexandreBarauna 949
RodolfoTeofilo 60430-160 Fortaleza Ceara´ Brazil