SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Original
Article
Ultrasound
evaluation
of
the
rotator
cuff
after
osteosynthesis
of
proximal
humeral
fractures
with
locking
intramedullary
nail
夽
Mauro
Emilio
Conforto
Gracitelli,
Eduardo
Angeli
Malavolta,
Jorge
Henrique
Assunc¸ão
∗,
Bruno
Akio
Matsumura,
Kodi
Edson
Kojima,
Arnaldo
Amado
Ferreira
Neto
UniversidadedeSãoPaulo,InstitutodeOrtopediaeTraumatologia,GrupodeOmbroeCotovelo,SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received8September2016 Accepted3October2016 Availableonline23August2017
Keywords: Shoulderfractures
Fractureintramedullaryfixation Rotatorcuff
Ultrasonography
a
b
s
t
r
a
c
t
Objective:Toevaluatesupraspinatustendonintegritywithultrasound(US)inpatients sub-mittedtoproximalhumeralfracture(PHF)fixationwithalockingintramedullarynail. Methods:Thirty-onepatientswithPHFtreatedwithcurvilinearlockingintramedullarynail, agedbetween50and85 years,wereassessed byUSatsixmonthspostoperativelyand clinicallyatsixand12monthspostoperatively.Theprimaryaimwassupraspinatus ten-donintegrity,evaluatedbyUSatsixmonthspostoperatively.Secondaryaimsincludedthe Constant-Murley,DASHscore,andvisualanalogpainscores,aswellascomplicationsand reoperationrates.
Results:Full-thickness rotator cuff ruptures were observed in four patients (13%), supraspinatusrupturesinthreecases(10%),andsubscapularisrupturesinonecase(3%). Partialruptureswerediagnosedin10cases(32%).TheresultsusingtheConstant-Murley score at12monthswere71.3±15.2pointsforthe entireseries, with73.2±16.1points forpatientswithoutrotatorcuffrupturesand68.7±14.1pointsforthosewithpartialor completeruptures,withoutastatisticallysignificantdifference(p=0.336).Complications, exclusivelyforrotatorcuffruptures,wereobservedinninepatients(29%).
Conclusion: Ahighrateofrotatorcuffruptureswasdemonstrated,withpartialrupturesin 32%ofcasesandfull-thicknessrupturesin13%.However,clinicalresultsaresatisfactory, andarenotinfluencedbythepresenceofrotatorcuffruptures.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
夽
PaperdevelopedattheUniversidadedeSãoPaulo,InstitutodeOrtopediaeTraumatologia,GrupodeOmbroeCotovelo,SãoPaulo,SP, Brazil.
∗ Correspondingauthor.
E-mail:drjorgeassuncao@gmail.com(J.H.Assunc¸ão). http://dx.doi.org/10.1016/j.rboe.2016.10.016
Palavras-chave: Fraturasdoombro
Fixac¸ãointramedulardefraturas Manguitorotador
Ultrassonografia
r
e
s
u
m
o
Objetivo: Avaliaraintegridadedotendãodosupraespinalpormeiodaultrassonografia(US) empacientessubmetidosàfixac¸ãodefraturasdaextremidadeproximaldoúmero(FEPU) comhasteintramedularbloqueada.
Métodos: Foramavaliadosporexamedeultrassonografiaaosseismesesdepós-operatório eclinicamenteaosseise12mesesdepós-operatório31pacientescomFEPUentre50e85 anos,tratadoscomhasteintramedularbloqueadainclinada.Oobjetivoprimáriofoiavaliara integridadedotendãosupraespinaleossecundáriosincluíamdescreverosdemaisachados daultrassonografia,asescalasdeConstant-Murley,EVAeDasheataxadecomplicac¸õese compararosresultadosclínicosdospacientescomesemroturadomanguitorotador. Resultados: Roturas transfixantes do manguito rotador foram observadas em quatro pacientes(13%),comroturadosupraespinalemtrêscasos(10%)edosubescapularem umcaso(3%).Roturasparciaisforamdiagnosticadasemdezcasos(32%).Osresultadospela escaladeConstant-Murleyaos12mesesforamde71,3±15,2pontosparatodaaamostra, de73,2±16,1pontosparaospacientessemroturadomanguitorotadorede68,7±14,1 pontosparaaquelescomroturaparcialoucompleta(p=0,336).Complicac¸ões,exclusivea roturadomanguitorotador,foramobservadasemnovepacientes(29%).
Conclusão: Observou-seumaaltataxadealterac¸õesnostendõesdomanguitorotador,com roturasparciaisem32%doscasosetransfixantesem13%.Noentanto,osresultadosclínicos sãosatisfatórios,nãoinfluenciadospelapresenc¸aderoturadomanguitorotador.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Fracturesoftheproximalhumerus(PHF)arethethirdmost commonfractureintheelderly.1Despitethecurrent contro-versyovertheadvantagesofsurgicaltreatment,2,3 deviated fracturesarecommonlytreatedwithfixationorarthroplasty, witha25%increaseinsurgicalindicationsinfiveyears.4
LockedintramedullarynailshavebeenusedforPHFsince beforethedevelopmentoflockedplates5;however,theyhave notachievedthesamepopularity,withthemainreasonsbeing relatedtothe potentialrisksofruptureofthe rotatorcuff, andbecausetheydonothelpinthereductionoffractures.6,7 However,therearebiomechanicaladvantages8–10fortheuse ofnails,and theycan beusedthrough minimally invasive approaches,withlesspotentialdamagetosofttissues.11
Clinical results are similar among patients undergoing osteosynthesiswithlockingplatesornails.6,7,12–15 However, there isdisagreement as to which one generates ahigher rateofcomplications.6,14,16Theriskofruptureorchangesin therotatorcuffafterintramedullarynailshasbeenscarcely studied,7,13,17,18 andnoarticlementionsastandardizedand detailedevaluationoftherotatorcuff.
Theprimaryaimofthestudywastoevaluatetheintegrity ofthe supraspinatus tendon bymeans ofultrasonography (US) in patients submitted to the fixation of PHF with a lockingintramedullarynail.Thesecondary aimwasto cor-relatethe presenceof rupture ofthe rotator cuff withthe Constant-Murley,DASHandVASscores,andtocomparethe
clinical results of patients with and without rotator cuff rupture.
Methods
Studydesign
A prospective study involving 31 patients with fractures deviated from the proximal humeralextremity, underwent surgicaltreatmentwithlockingintramedullarynailthrougha minimallyinvasiveanterolateralapproach.Thepatientswere part ofa previous randomized study19 and were operated betweenMarch2011andDecember2014atthesameCenter. Theoperations wereperformed bythesame surgeon,with thesamemodelofimplant.Theprotocolwasapprovedbythe EthicsCommitteeofourmedicalfacility.
Participants
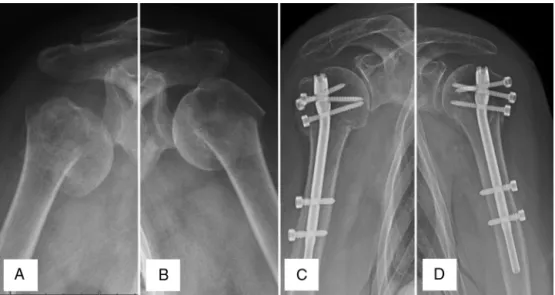
Fig.1–(A)Bilateralfractureofthehumeralproximalextremity,deviatedinvarus,rightshoulder;(B)leftshoulder; (C)radiographs,atthreemonthspostoperativelyoffixationwithintramedullarynail,rightshoulder;(D)leftshoulder.
included.Patientswithirreversibleruptureoftherotatorcuff, thosewhodidnotundergoUS,orthosewithlossoffollow-up beforethefirstclinicalevaluationat3monthswereexcluded.
Surgicaltreatment
The locking intramedullary nail used was Centronail® (Orthofix®,Verona,Italy),madeoftitanium,15cmlongand 7cmthick,andwithaslightlycurvedproximalend.
Alongitudinalanterolateraltransdeltoidapproachof5cm was made, beginning atthe anterolateral extremity ofthe acromion. The deltoid muscle was dissected between the anteriorandmiddleportionsupto5cmdistaltotheacromion, withnoreleasefromitsorigin,anduptotheidentificationof thesubacromialbursaandtherotatorcuff.Thesupraspinatus andinfraspinatustendonswereidentifiedandsuturedwith polyesternon-absorbablesurgicalthread.Thehumeralhead wasreduced and provisionallysecured withtwoKirschner wirespercutaneouslyfromtheanteriorfaceofthediaphysis towardtheposterosuperiorportionofthehumeralhead.In caseswithlargertuberclefractures,transosseoussutureswith polyestersurgical threadwere made, andthe fracture was reducedbeforepassingtheintramedullarynail.
Followingfracturereductionandtemporaryfixationofthe humeralheadtothediaphysis,accesswasmadeforinsertion oftheintramedullarynail.Afterpalpationofthesmall tuber-cleand tendonofthelong headofthebiceps, aguidewire waspositioned1cmposteriortothe intertuberculargroove and1cmmedialtothetransitionbetweenthehumerushead andthegreater tubercle,thatwasconfirmedbyradioscopy withtheshoulderat30degreesofexternalrotation.After con-firmationofthecorrectpositioning ofthewire,the 1.5-cm longitudinalopeningofthe supraspinatustendon was per-formedwithascalpel,nearthemedialborderofthegreater tubercle,withoutdamagingitsattachment.
Theguidewirewastheninserted,anditscorrect position-ingcheckedwithradioscopy.A2-cmdeepresurfacingofthe humeralheadwasperformed.Therewasnoneedtoreamthe
humeralmetaphysisanddiaphysis.Thenailwasintroduced andwesoughttomaintainitsupperportion5mmbelowthe surfaceofthehumeralhead.Thenailwasproximallylocked withthreescrewsanddistallywithtwoscrews.Achannelplug wastheninserted.Tensionbandsuturesweremadearound theproximalscrews,withthenon-absorbablesurgicalthreads passedinthesupraspinatusandinfraspinatustendons.The openingofthesupraspinatustendonwassuturedwithatleast threesimplesutureswithpolyester#2non-absorbable surgi-calthread,followedbydeltoidmuscle,subcutaneousandskin sutures.
Theslingwasusedforfourweeksandphysicaltherapy startedafter14days,withpassiveandactiveassisted exer-cisesforthegainofrangeofmotion.Activeexerciseswere startedafter30days,andactiveresistanceexercisesaftertwo months.
Outcome
The primary outcome adopted was the evaluation of the integrityofthesupraspinatustendonthroughanultrasound (US)examinationperformedatthesixthpostoperativemonth. Secondary outcomes were:the Constant-Murley20 and EVA scoresandtheDASHquestionnaire,21andotherUSfindings, as well as complications and reoperations. The Constant-Murleyscorewasassessedat6and12monthspostoperatively andtheotherscoresat12months.Theclinicalscoringwas appliedbyanevaluatorwhodidnotparticipateinthe rehabil-itationorclinicalfollow-upofthepatient.
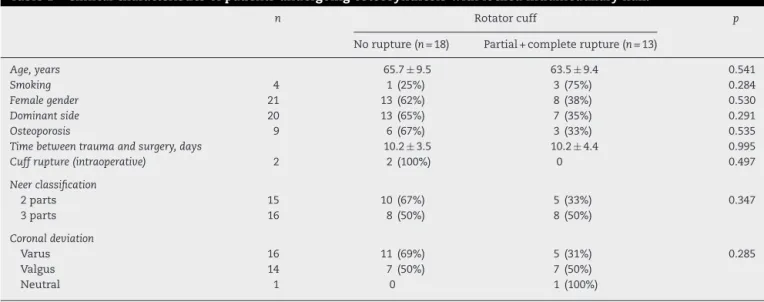
Norupture(n=18) Partial+completerupture(n=13)
Age,years 65.7±9.5 63.5±9.4 0.541
Smoking 4 1(25%) 3(75%) 0.284
Femalegender 21 13(62%) 8(38%) 0.530
Dominantside 20 13(65%) 7(35%) 0.291
Osteoporosis 9 6(67%) 3(33%) 0.535
Timebetweentraumaandsurgery,days 10.2±3.5 10.2±4.4 0.995
Cuffrupture(intraoperative) 2 2(100%) 0 0.497
Neerclassification
2parts 15 10(67%) 5(33%) 0.347
3parts 16 8(50%) 8(50%)
Coronaldeviation
Varus 16 11(69%) 5(31%) 0.285
Valgus 14 7(50%) 7(50%)
Neutral 1 0 1(100%)
andtransfixingrupture.Inthepresenceofalesion,the retrac-tionandextensionoftherupturewasobserved.Alltendons oftherotatorcuffwereevaluated.Thelongheadofthebiceps tendonwasevaluatedforintegrity,tendinopathyandstability. Complicationswerewrittendownaccordingtotheir occur-rence and the total number recorded separately for each patient. The reoperations and type of surgery were also recorded.
Statisticalanalysis
We evaluated the normality of the data through the Shapiro–WilktestandequalitythroughtheLevenetest.We disclosethecontinuousvariablesinmeanandstandard devi-ationsandthecategoricalvariablesinabsoluteandpercentage values.
Fortheanalysisoftheoutcome,thepatientsweredivided into two groups, according to the absence or presence of cuffrupture.Patientswithcompleterupturewerecompared tothosewithout rupture.Thosewithpartialruptureswere groupedwithfullrupture forcomparisonwiththose with-outrupture.Thecorrelationbetweentheindependentvariable (integrityofthesupraspinatustendonevaluatedbythe US) andthedependentvariables(Constant-MurleyandEVAscores andDASHquestionnaire)wasdoneusingtheAnovatest (para-metricdata)ortheFriedmantest(non-parametricdata).
ThesoftwareSPSSversion20.0(SPSSInc®,Chicago,IL,USA) wasusedfordataanalysis,andthelevelofsignificanceof5% wasadopted.
Results
Thirty-six patients were operated on with a locked intramedullary nails. Of these, five were excluded, four due toloss offollow-up and onebecause the US was not performed. The general data of the series can be seen in
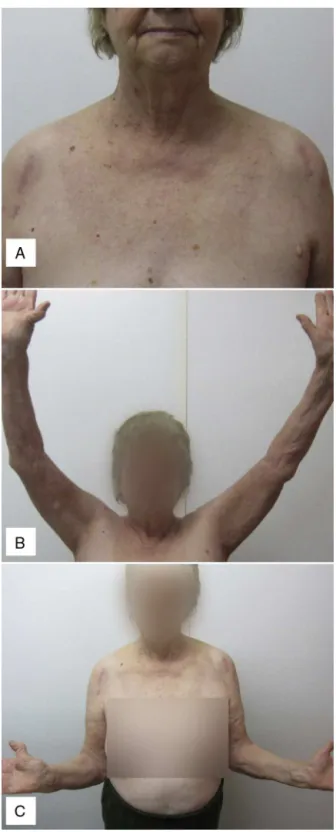
Table1.Follow-upwas12monthsforallpatients.Figs.1and2 showtheclinicalandradiographicresults.
TheUSexaminationwasperformedon31patients.Fig.3 showsanevaluation.Thisexaminationshowedatransfixing
Table2–Resultsofultrasoundexaminationfor evaluationofrotatorcufftendonsandthelongheadof thebicepstendon.
Tendon n(%)
Supraspinatus
Completerupture 3(10%)
Partialjointrupture
<50% 6(20%)
>50% 1(3%)
Interstitialrupture 3(10%)
Tendinopathy 16(52%)
Normal 2(6%)
Subscapular
Complete1/3proximal 1(3%)
Tendinopathy 19(61%)
Normal 11(35%)
Infraspinatus
Tendinopathy 13(42%)
Normal 18(58%)
Longheadofthebiceps
Rupture 3(10%)
Tendinopathy 14(45%)
Normal 14(45%)
ruptureoftherotatorcuffinfourcases(13%),with involve-mentofthesupraspinatustendoninthreepatients,andof thesubscapularisinonecase.Themeanextensionof transfix-ingsupraspinatusruptureswas8mmandthemeanretraction was9mm.Partialruptureswerediagnosedin10cases(32%), withall ofthemaffectingthe supraspinatus tendonatthe jointsurface.Twopatientsrevealedruptureoftherotatorcuff intraoperativelyandweresubmittedtorepair.Norecurrence oftendonrupturewasdetectedinthesepatients,andhadan averageof92pointsontheConstant-Murleyscore.USdata canbeobservedinTable2.
Fig.2–Postoperativeclinicalevaluationatthreemonths demonstratesanterolateralincision(A),elevation(B)and externalrotation(C).
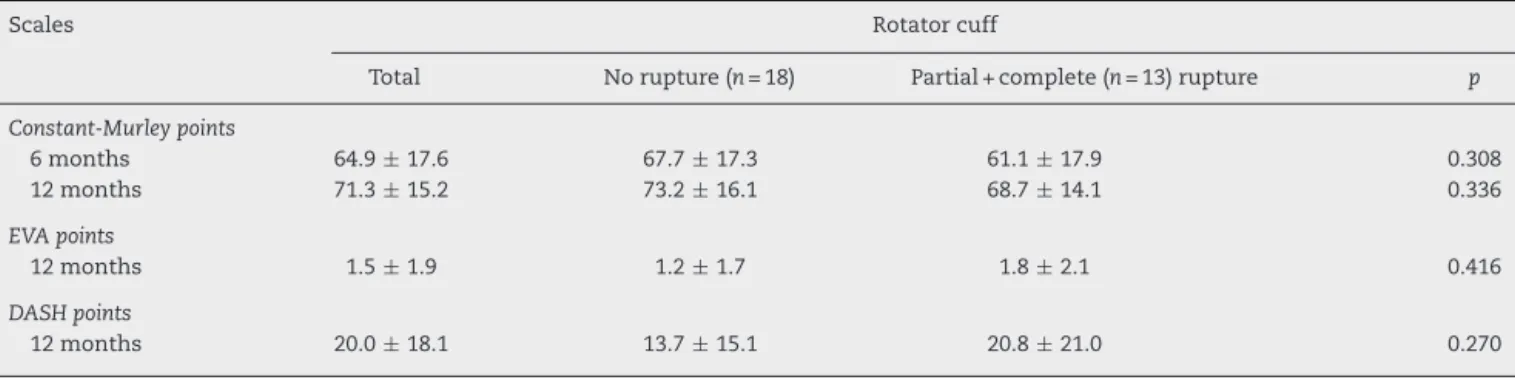
averageofthewholeserieswas64.9±17.6points,inthegroup withoutruptureoftherotatorcuffitwas67.7±17.3pointsand inthegroupwithruptureitwas61,1±17.9points,also with-outstatisticallysignificantdifference(p=0.308).Patientswith rotatorcufftransfixationshowedaConstant-Murleyscoreof 62.0±21.7pointsat12months,withnostatisticallysignificant differenceinrelationtothegroupwithoutruptures(p=0.138).
Intheevaluationoftheabductionforceat6and12months, wealsodidnotobservedifferencesbetweenthegroups.
Theresultsfromthe12-monthDASHquestionnairewere 20.0±18.1pointsfortheentireseries,betterinthegroup with-outruptureoftherotatorcuff(13.7±15.1versus20.8 ±21.0), but without statisticallysignificantdifference (p=0.270). By theEVAscoreat12months,thewholeserieshadameanof 1.5±11.9pointsandthegroupspresentedmeandifferences belowonepoint.ClinicaloutcomescanbeseeninTable3.
Complications,otherthanruptureoftherotatorcuff,were observedinninepatients(29%).Themostcommon compli-cationswereshoulderstiffnessinfourpatients(13%),lossof humeralheadreductiongreaterthan10degreesofthe head-shaftangleinthreecases(9%),jointprotrusionoftheproximal screwsinthreepatients(9%),andosteonecrosisintwocases (6%). Innocasedidthenailremaininaninadequate posi-tion,thatis,abovethegreatertubercle.Ofthefourpatients with transfixing rupture ofthe rotator cuff, twohad other complications,with43.5±6.4pointsontheConstant-Murley scoreat12months.Thetwocaseswithisolatedruptureofthe cuffhad80.5±0.7points.Therotatorcuffrupturerate (par-tialorcomplete)inpatientswithsomecomplicationwas33%, with no statistically significant difference when compared tocaseswithoutothercomplications(p=0.535).Sixpatients (19%)underwentreoperations.
Discussion
We demonstrated good clinical outcomes for PHF patients treatedwithalockedintramedullarynail,withanaverageof 71pointsontheConstant-Murleyscorethroughouttheseries. OurresultswerelowerthanthoseofZhuetal.6andKonrad etal.,12butsimilartothoseofseveralotherauthors.7,13,16,22,23 However,thecomplicationratewashigh,asitoccurredin29% ofourseries,higherthanthatreportedbyZhuetal.6(4%)but similartoorlowerthaninotherstudies.7,12,24
Weobservedahighrateofrotatorcuffchangeson ultra-sonographic analysis. The most affected tendon was the supraspinatusin94%ofcases,followedbysubscapular(64%) and infraspinal (42%). Thelong head ofthe biceps tendon showed changesin55%ofthepatients. Weobserved com-pleterupturesinfourcases(13%),higherthanthosereported by Gradl et al.7 (3%) and Boudard et al.13 (3.3%), which describe only transfixing supraspinatus ruptures. Fjalestad etal.25describe(partialandcomplete)rupturesin28%of non-surgicallytreatedpatientsevaluatedbymagneticresonance imaging.
ThepresenceofrotatorcuffchangesfollowingPHFoccurs irrespectiveofthetreatmentmethod;aruptureisdescribed in25% ofpatientstreated withnon-locked plates, percuta-neousfixationornon-surgically.26 Theriskofpostoperative supraspinatustendonchangesfollowingfixationwithlocked intramedullarynailisevident.Fortheintroductionof synthe-sismaterial,anincisionisnecessary,anditsmicrocirculation isdiminished,evenafteritbeingsutured.27
Fig.3–Ultrasonographicevaluationoftherotatorcuff.(A)Supraspinatustendonrupture;(B)infraspinatustendon; (C)subscapulartendon;(D)longheadofthebicepstendon.
Table3–Resultsofclinicalscoring,comparedaccordingtothepresenceornotofrotatorcuffrupture.
Scales Rotatorcuff
Total Norupture(n=18) Partial+complete(n=13)rupture p
Constant-Murleypoints
6months 64.9±17.6 67.7±17.3 61.1±17.9 0.308
12months 71.3±15.2 73.2±16.1 68.7±14.1 0.336
EVApoints
12months 1.5±1.9 1.2±1.7 1.8±2.1 0.416
DASHpoints
12months 20.0±18.1 13.7±15.1 20.8±21.0 0.270
asymptomatic.28,29 Ofthepatientsbetween60and70years ofage,25.6%maypresenttransfixingruptureoftherotator cuffandupto16.9%ofasymptomaticindividualsmaypresent completeruptures.30
Aspositivepointsofourstudy,wecanmentionthattheUS wasdoneatthesamemedicalCenter,withthesameteamof musculoskeletalradiologistsandwiththesamedevice,which increasestheinternalvalidityofourmeasurement.Wecan alsomentionthatthisisthefirststudytodetailrotatorcuff analysisafterPHFosteosynthesiswithlockedintramedullary nails,notonlydescribingthepresenceoftransfixingruptures. Inaddition,ourserieswasbasedonaprospectivestudy,with standardizedtiming.
Aslimitations,wecanmentionthattheUSexamination wasnotpreviouslyvalidatedorcomparedtoMRIafter frac-turesoftheproximalendofthehumerus.Althoughrotator cuffinspectionwasperformedinallsurgeries,itisnot pos-sibletoruleoutthepresenceofpartialrupturesatjointlevel throughintraoperativeevaluation.Thepresenceofa previ-ousruptureoftherotator cuffcannotbeconfirmedbyour study,sincethereisno imageanalysisbeforethe fracture. Anotherlimitationisrelatedtosubgroupanalyses.The group-ingofpartialandcompleteruptureswasaimedatreducing thecomparisonbiasamongsmallgroups,butduetothesmall
numberinourseries,thiscomparisonmaybesubjecttofalse negatives.Finally,themodelofthenailused,thatisslightly curved,presentsagreaterriskofpainrelatedtothecuffand greaterriskofreoperations,asdemonstratedbyLopizetal.24 Ourresultsshowthatrotatorcuffdisorderswerepresentin 64.1%oftheseries,41.2%tendinopathy,11.0%partialrupture and12.2%completerupture.
Conclusions
Our study provides an epidemiological basis for rotator cuff ruptures in patients with fractures of the proximal humerus undergoingfixation witha slightlycurved locked intramedullary nail.We demonstrated ahigh rate of alter-ationsintherotatorcufftendons,withpartialrupturesin32% ofcasesandtransfixingin13%.However,theclinicalresults aresatisfactory,andarenotinfluencedbythepresenceof rup-tureoftherotatorcuff,despitethelimitationsofevaluation duetothesmallnumberinourseries.
Conflicts
of
interest
r
e
f
e
r
e
n
c
e
s
1. PalvanenM,KannusP,NiemiS,ParkkariJ.Updateinthe epidemiologyofproximalhumeralfractures.ClinOrthop RelatRes.2006;442:87–92.
2. RanganA,HandollH,BrealeyS,JeffersonL,KedingA,Martin BC,etal.Surgicalvsnonsurgicaltreatmentofadultswith displacedfracturesoftheproximalhumerus:thePROFHER randomizedclinicaltrial.JAMA.2015;313(10):1037–47. 3. HandollHH,BrorsonS.Interventionsfortreatingproximal
humeralfracturesinadults.CochraneDatabaseSystRev. 2015;11:CD000434.
4. BellJ-E,LeungBC,SprattKF,KovalKJ,WeinsteinJD,Goodman DC,etal.Trendsandvariationinincidence,surgical
treatment,andrepeatsurgeryofproximalhumeralfractures intheelderly.JBoneJointSurgAm.2011;93(2):121–31. 5. LinJ,HouSM,HangYS.Lockednailingfordisplacedsurgical
neckfracturesofthehumerus.JTrauma.1998;45(6):1051–7. 6. ZhuY,LuY,ShenJ,ZhangJ,JiangC.Lockingintramedullary
nailsandlockingplatesinthetreatmentoftwo-part proximalhumeralsurgicalneckfractures:aprospective randomizedtrialwithaminimumofthreeyearsoffollow-up. JBoneJointSurgAm.2011;93(2):159–68.
7. GradlG,DietzeA,KääbM,HopfenmüllerW,MittlmeierT.Is lockingnailingofhumeralheadfracturessuperiortolocking platefixation?ClinOrthopRelatRes.2009;467(11):2986–93. 8. FüchtmeierB,MayR,HenteR,MaghsudiM,VölkM,Hammer
J,etal.Proximalhumerusfractures:acomparative
biomechanicalanalysisofintraandextramedullaryimplants. ArchOrthopTraumaSurg.2007;127(6):441–7.
9. KitsonJ,BoothG,DayR.Abiomechanicalcomparisonof lockingplateandlockingnailimplantsusedforfracturesof theproximalhumerus.JShoulderElbowSurg.
2007;16(3):362–6.
10.YoonRS,DziadoszD,PorterDA,FrankMA,SmithWR, LiporaceFA.Acomprehensiveupdateoncurrentfixation optionsfortwo-partproximalhumerusfractures:a biomechanicalinvestigation.Injury.2014;45(3):510–4. 11.SosefN,vanLeerdamR,OttP,MeylaertsS,RhemrevS.
Minimalinvasivefixationofproximalhumeralfractureswith anintramedullarynail:goodresultsinelderlypatients.Arch OrthopTraumaSurg.2010;130(5):605–11.
12.KonradG,AudigéL,LambertS,HertelR,SüdkampNP.Similar outcomesfornailversusplatefixationofthree-partproximal humeralfractures.ClinOrthopRelatRes.2012;470(2): 602–9.
13.BoudardG,PomaresG,MilinL,LemonnierI,CoudaneH, MainardD,etal.Lockingplatefixationversusantegrade nailingof3-and4-partproximalhumerusfracturesin patientswithoutosteoporosis.Comparativeretrospective studyof63cases.OrthopTraumatolSurgRes.
2014;100(8):917–24.
14.HardemanF,BollarsP,DonnellyM,BellemansJ,NijsS. Predictivefactorsforfunctionaloutcomeandfailurein angularstableosteosynthesisoftheproximalhumerus. Injury.2012;43(2):153–8.
15.VieciliL,TurcoDL,RamalhoJHA,FinelliCA,ToriniAP. Tratamentodasfraturasemduaspartesdocolocirúrgicodo úmerocomousodehasteintramedularmetafisária
bloqueadaproximalmentecomestabilidadeangular.RevBras Ortop.2015;50(1):22–9.
16.WangG,MaoZ,ZhangL,ZhangL,ZhaoY,YinP,etal. Meta-analysisoflockingplateversusintramedullarynailfor treatmentofproximalhumeralfractures.JOrthopSurgRes. 2015;10:122.
17.RochetS,ObertL,SarlieveP,ClappazP,LepageD,GarbuioP, etal.Functionalandsonographicshoulderassessmentafter Seidelnailing:aretrospectivestudyof29cases.RevChir OrthopReparatriceApparMot.2006;92(6):549–55. 18.VerdanoMA,PellegriniA,SchiaviP,SomenziL,ConcariG,
CeccarelliF.Humeralshaftfracturestreatedwithantegrade intramedullarynailing:whataretheconsequencesforthe rotatorcuff?IntOrthop.2013;37(10):2001–7.
19.GracitelliMEC,MalavoltaEA,Assunc¸ãoJH,KojimaKE,dos ReisPR,SilvaJS,etal.Lockingintramedullarynailscompared withlockingplatesfortwo-andthree-partproximalhumeral surgicalneckfractures:arandomizedcontrolledtrial.J ShoulderElbowSurg.2016;25(5):695–703.
20.ConstantCR,MurleyAH.Aclinicalmethodoffunctional assessmentoftheshoulder.ClinOrthopRelatRes. 1987;214:160–4.
21.OrfaleAG,AraújoPMP,FerrazMB,NatourJ.Translationinto BrazilianPortuguese,culturaladaptationandevaluationof thereliabilityoftheDisabilitiesoftheArm,Shoulderand HandQuestionnaire.BrazJMedBiolRes.2005;38(2):293–302. 22.vonRüdenC,TrappO,HierholzerC,ProhaskaS,WurmS,
BührenV.Intramedullarynailingvs.lockingplate osteosynthesisinproximalhumeralfractures:long-term outcome.Unfallchirurg.2014;118(8):686–92.
23.PopescuD,Fernandez-ValenciaJA,RiosM,Cu ˜néJ,DomingoA, PratS.Internalfixationofproximalhumerusfracturesusing theT2-proximalhumeralnail.ArchOrthopTraumaSurg. 2009;129(9):1239–44.
24.LopizY,Garcia-CoiradasJ,Garcia-FernandezC,MarcoF. Proximalhumerusnailing:arandomizedclinicaltrial betweencurvilinearandstraightnails.JShoulderElbowSurg. 2014;23(3):369–76.
25.FjalestadT,HoleMØ,BlücherJ,HovdenIAH,StirisMG, StrømsøeK.Rotatorcufftearsinproximalhumeralfractures: anMRIcohortstudyin76patients.ArchOrthopTraumaSurg. 2010;130(5):575–81.
26.WilmannsC,BonnaireF.Rotatorcuffalterationsresulting fromhumeralheadfractures.Injury.2002;33(9):781–9. 27.GiererP,ScholzM,BeckM,SchaserKD,VollmarB,Mittlmeier
T,etal.Microcirculatorysequelaeoftherotatorcuffafter antegradenailinginproximalhumerusfracture.ArchOrthop TraumaSurg.2010;130(5):687–91.
28.KeenerJD,HsuJE,Steger-MayK,TeefeySA,ChamberlainAM, YamaguchiK.Patternsoftearprogressionforasymptomatic degenerativerotatorcufftears.JShoulderElbowSurg. 2015;24(12):1845–51.
29.KeenerJD,GalatzLM,TeefeySA,MiddletonWD,Steger-May K,Stobbs-CucchiG,etal.Aprospectiveevaluationof survivorshipofasymptomaticdegenerativerotatorcufftears. JBoneJointSurgAm.2015;97(2):89–98.