ORIGINAL
ARTICLE
Epidemiology of HIV/HCV coinfection in patients cared for
at the Tropical Medicine Foundation of Amazonas
Authors
MarilúBarbieriVictoria1 FlamirdaSilvaVictoria1 KátiaLuzTorres2 SimoneKashima4 DimasTadeuCovas4 AdrianaMalheiro2,3
1FundaçãodeMedicina
TropicaldoAmazonas– FMTAM
2FundaçãodeHematologia
eHemoterapiado Amazonas–HEMOAM
3UniversidadeFederaldo
Amazonas–UFAM
4FundaçãoHemocentrode
RibeirãoPreto–Centro RegionaldeHematologia, HCFMRP-USP.
Submittedon:03/31/2009 Approvedon:09/26/2009
Correspondence to: MarilúBarbieriVictoria RuaRioJavari,200/400, Ed.SaintCyr,
NossaSenhoradasGraças Manaus–AM–Brazil CEP:69053-110 Fone:(92)35841424e (92)99820967 E-mail:mariluvictoria@ vivax.com.br
Wedeclarenoconflictof interest.
ABSTRACT
TheassociationofHIVinfectionandhepatitisCvirus(HCV)infectionoftenoccursbecausebothvi-rusessharethesametransmissionroutes,increasingthepossibilityofHIV/HCVcoinfection.World prevalencegreaterthan30%ofcoinfectedcasesisestimated,anditcanreach90%dependingonthe transmissionroute.WiththeaimofdeterminingthefrequencyandprofileofHIV/HCVcoinfected patients,adescriptiveanalysiswascarriedoutwithpatientswithHIV/AIDSwhoseserologywas positiveforhepatitisCvirus(HCV),caredforattheFundaçãodeMedicinaTropicaldoAmazonas from2000to2007.Inthepresentstudy,ofthe2,653AIDScasesnotifiedinSINAN,1,582patients underwentserologytestforhepatitisC,andafrequencyof4.42%(n=70)ofHIV/HCVcoinfected patientswasidentifiedintheperiodstudied.Themostfrequentinfectionroutewassexualtrans-mission(84.3%),68.6%amongheterosexualindividuals.Mostpatientsweremales(72.9%),aged between25and40years(60.1%),oflowincome(50%earninguptooneminimumwage),and loweducationallevel(80%hadcompletedonlymiddleschool).Ahighpercentageofdeathswere observedduringthestudy(34.3%).TheresultsindicatealowseroprevalenceofHIV/HCVcoinfec-tioninthispopulation,inwhichsexualtransmission,characterizedbysexualpromiscuityamong heterosexualindividuals,isthemajortransmissionrouteofthevirusratherthantheuseofinjection drugs,asshowninworldstatistics.
Keywords:coinfection,hepatitisC,HIV,epidemiology,transmission.
[BrazJInfectDis2010;14(2):135-140]©ElsevierEditoraLtda.
INTRODUCTION
Hepatitis C virus (HCV) and human immu-nodeficiencyvirus(HIV)infectionsareamong thetenmajorcausesofdeathduetoinfectious diseasesworldwide.1Nowadays,therearemore than40millionHIV-infectedindividuals,30% of whom are estimated to be also infected by HCV, representing a growing public health problemworldwide.2,3
Coinfection rates range from 4% to 90%, depending on the type of exposure. Studies carriedoutinBrazilhaveshownacoinfection prevalence of 40%, which varies according to region, geographic differences, age, and effi-ciencyofexposure.1,3,4,5
TheHCVandHIVhavesimilartransmis-sion modalities, but the efficacy of the trans-mission of each virus differs, and several fac-torsinfluencethatcoinfection.Forboth,blood exposure and injection drug use are efficient transmission forms. However, the risk of ver-tical and perinatal transmissions is high for
HIVandrelativelylowforHCV,althoughthe risk increases twice when the mother is HIV positive.6,7
The sexual transmission of HCV is inef-ficient, and the exact risk related to different typesofsexualactivityisunknown;neverthe-less,ithasbeenincreasingamongHIV-infected
menwhohavesexwithmen(MSM).8
The introduction of highly active antiret-roviral therapy (HAART) has significantly improvedlifeexpectancyofHIV-infectedpa-tients; however, the consequences of hepatitis Chavebecomemoreapparent,asaresultei- therofdecompensatedcirrhosisorhepatotox-icityduetoHAART.9,10,11
The interaction of those viruses has been the object of great concern, being considered oneofthemostimportantpublichealthprob- lemsfacedbyhealthprofessionalsandauthori-tiesworldwide.12
SINAMdatabaseandcaredforattheFundaçãodeMedicina TropicaldoAmazonas(FMTAM)from2000to2007.Inad- dition,italsoaimedatbetterknowingtheprofileandbe-haviorofthispopulation,sinceepidemiologicalstudieson HIV/HCVcoinfectioninthestateofAmazonasarescarce.
MATERIAL AND METHODS
Description of the study area
This study was developed at FMTAM, a state reference center for the follow-up of HIV patients in the city of Manaus,hometoapproximately1.71millionpeopleofthe 2.8millioninhabitantsofthestateofAmazonas,71.4%of whomareinurbanareasand28.6%inruralarea.13
The FMTAM is one of the 20 testing and counseling centers of the state of Amazonas. It comprises specialized outpatient clinics, a hospitalization unit, and laboratories equippedfordiagnosinginfectiousdiseases.
ToidentifytheHIVandHCVcoinfectedpopulationcared for at FMTAM from 2000 to 2007, the following databases wereused:theSINAN(SistemadeInformaçõesdeAgravos deNotificação)database;thedatabaseoftheCoordinationof Sexually Transmitted Diseases/AIDS of the state ofAmazo-nas,andthedatabaseoftheVirologyUnitofFMTAM.
Wechosetostartthestudyintheyear2000duetothe lack of available data on viral hepatitis prior to that year. It is worth noting that, over the study period, the institu-tionhasundergonemodernizationofitsoutpatientclinics andlaboratories,suchasdigitalizationofpatients’datafrom 2005,andintegrationwiththeinformationnetworkofthe MinistryofHealthforAIDScases.
Study design
This is a descriptive study of a case series of patients with AIDScoinfectedwithHCVcaredforattheFMTAMduring thestudyperiod.Afterdatabasecross-referencingandpatients’ selection,medicalrecordsweresoughtforinformationreferring topatients’identification,demographicdata,socioeconomic andculturalprofiles,aswellasriskfactorsfortheacquisition of the diseases in question. Those data were registered in a clinical-epidemiologicalformelaboratedforthestudy.
Seventypatientswereincludedinthestudyaccordingto thefollowingcriteria:ageover12years,bothsexes,andposi-tiveserologyforHIV(anti-HIV)andforHCV(anti-HCV). PatientswithapositivemarkerforhepatitisBvirus(HBsAg) and/orhepatitisDvirus(anti-HD)andthosewhodidnot agreetoparticipateinthestudyorsignthewritteninformed consentwereexcluded.
ThisstudyhasbeenapprovedbytheCommitteeon EthicsinResearchwithHumanBeingsofFMTAM,un-derprotocol2857/2007,inaccordancewithResolution CNS196/96oftheNationalHealthCounciloftheMin-istryofHealth.
Statistical analysis
Thesampleusedforanalysiscomprised70HIV/HCVcoin-fectedpatientscaredforatFMTAMfrom2000to2007.
Datawerepresentedusingtablesandgraphsofsimple, absolute,andrelativefrequencies.Intheanalysisofquan-titative variables, mean and standard deviation (SD) were calculated.DataanalysisusedtheEpi-Infosoftware,version 3.5forWindows,developedanddistributedbyCDC(www. cdc.gov/epiinfo). The 95% confidence interval (CI) was adopted.
RESULTS
Origin of the coinfected population
AccordingtoSINAN,from2000to2007,thetotalnumber of AIDS cases accumulated in Brazil corresponded to 209,975 cases.14 In the Northern Region of Brazil, there were8,903cases,andinthestateofAmazonas,2,653cas-es,representing1.3%ofthetotalnumberofcasesinthe country.14
IntermsofAIDSincidence,intheBraziliannorthern region,thestateofAmazonasissecondonlytothestateof Pará.Thatpopulationhasamantowomanratioof2:1,a tendencythathasbeenkeptsince1999inthestateofAma-zonas,whileinBrazilthecurrentratiois1.5:1.14
During the period studied, 2,653 cases of AIDS were notifiedatSINAN.Ofthose,only1,582patientshadun-dergone the serologic test for hepatitis C, 70 of which testedpositive,representingafrequencyof4.42%ofHIV/ HCVcoinfectedpatientscaredforatFMTAMduringthis period.
TheHBV/HCVdoubleinfectionwasidentifiedintwo patients, and the HBV/HCV/HDV triple infection was identified in only one patient. These three patients were excludedfromthestudy.
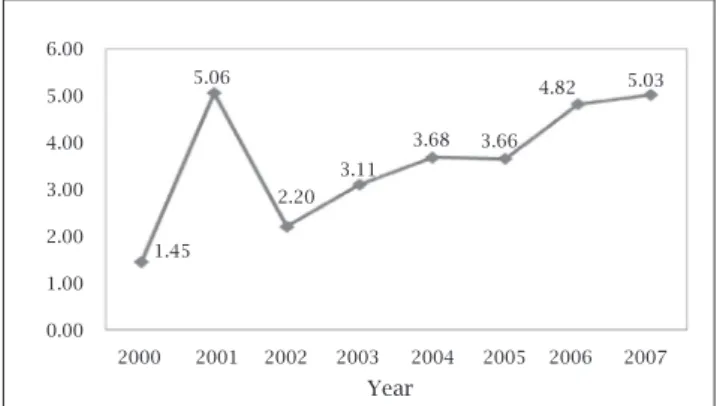
In Figure 1, the annual curve shows an increase in coinfection cases, from 1.45% in the year 2000 to 5.03% in2007.
Figure 1: Annual distribution according to the frequency
of HIV/HCV coinfected patients cared for at FMTAM from 2000 to 2007.
Year
1.45 5.06
2.20 3.11
5.03 4.82
3.66 3.68 6.00
5.00
4.00
3.00
2.00
1.00
0.00
Demographic data
Regarding the gender of HIV/HCV coinfected population (n=70),men(n=51,72.9%)representedthemajority.In thispopulation,agerangedfrom20to67years(meanage, 38.5±10.2years),withtheagebracketof30-35yearsbeing themostpopulous(n=20,28.6%).Regardingthepopula-tioneducationallevel,80%(n=56)hadcompletedmiddle school,and4.2%(n=3)wereilliterate.Regardingmonthly income,50%(n=35)ofthepatientsreceiveduptoonena-tionalminimumwageand20%(n=14)wereunemployed. AmongtheHIV/HCVcoinfectedpatients,theplaceof birthofmostpatients(n=39,55.7%)wasthecityofMan-aus,followedbytheinnerAmazonasstate(n=15,21.4%), andotherstates(n=16,22.9%).Regardingthesiteoforigin, 94.3%(n=66)camefromthecityofManaus,only5.7% (n=4)fromtheinnerAmazonasstate,andnobodycame fromotherstates(Table1).
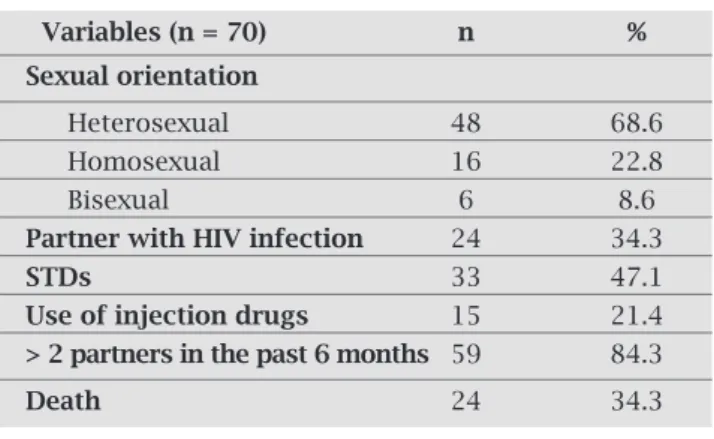
Sexual orientation and risk factors
Accordingtothesexualorientationofthepatientsstudied, 48(68.6%)patientswereheterosexual,16(22.8%)wereho-mosexual,andsix(8.6%)werebisexual.Fifty-nine(84.3%) patientshavereportedsexualpromiscuity,thatis,morethan two partners in six months, and that was the major risk factoranalyzed.Otherriskfactorswereasfollows:acquisi-tionofsexuallytransmitteddiseases(STD),reportedby33 (47.1%)patients;sexpartnerknowntohaveHIVinfection, reportedby24(34.3%)patients;and,inalowerproportion, useofinjectiondrugs,reportedby15patients(21.4%).
Somepatientshadmorethanoneriskfactorassociated atthesametime(Table2).
Evolution of coinfected patients
The coinfected patients detected in the period studied showedahighdeathrate(n=24,34.3%),withmostdeaths occurringbetweentheyears2000and2003,and46(65.7%) patientswerealivebytheendofthestudyinDecember2007 (Table2).
DISCUSSION
The epidemiology of AIDS has changed over the years in Brazil. This epidemic has shown its strength by spreading fromthesoutheasternregiontootherregionsinthecoun-try.InthenorthernregionofBrazil,especiallyinthestate ofAmazonas,theepidemichasshownsocial,cultural,and geographicpeculiarities.15
Almost five years after its discovery,AIDS appeared in thestateofAmazonas,andthefirstnotificationofthedis-easeoccurredinApril1986,whenthenotificationofAIDS cases in Brazil became compulsory.16 From 1986 to 1990, AIDS was restricted to the municipality of Manaus, and, from1991,itspreadtotheinnerstate,butthecityofMan-ausstillhasthegreatestnumberofnotifiedcases.14
Table 2. Distribution of HIV/HCV coinfected patients cared for at FMTAM from 2000 to 2007, according to sexual orientation, risk factors for coinfection, and outcome
Variables (n = 70) n %
Sexual orientation
Heterosexual 48 68.6
Homosexual 16 22.8
Bisexual 6 8.6
Partner with HIV infection 24 34.3
STDs 33 47.1
Use of injection drugs 15 21.4
> 2 partners in the past 6 months 59 84.3
Death 24 34.3
Table 1. Distribution of HIV/HCV coinfected patients cared for at FMTAM from 2000 to 2007, according to demographic, socioeconomic, and cultural data
Variables (n = 70) n %
Gender
Male 51 72.9
Female 19 27.1
Age (years)
20|---25 2 2.8
25|---30 9 12.9
30|---35 20 28.6
35|---40 13 18.6
40|---45 6 8.6
45|---50 8 11.4
50|---55 4 5.7
55|---60 6 8.6
≥65 2 2.8
Mean±SD 38.5±10.2
Range 0-6
Educational level
Illiterate 3 4.3
Completemiddleschool 6 80.0
Completehighschool 9 12.8
Completeuniversity 2 2.9
Income (minimum wages)
Unemployed 14 20.0
≤1 35 50.0
2to3 16 22.9
4to6 5 7.1
Place of birth
CityofManaus 39 55.7
InnerAmazonasstate 15 21.4
Otherstates 16 22.9
Origin
CityofManaus 66 94.3
AccordingtodatafromtheMinistryofHealth,theepi-demicinthestateofAmazonasseemstohavehadatendency toincreasewithaprogressiveincidencerateuntil1999,and stabilization from 2000 to 2003. It began to increase again from2004,whenanimprovementinepidemiologicalsurveil- lancewasobservedwiththerestructurationoftheStateCoor-dinationofSTD/AIDSPrograminthestateofAmazonas.14,15 Nevertheless, the AIDS Epidemiological Surveillance systemstillsuffersfromsub-notificationofcasesanddelay innotifications.17,18 Thismaybeoneoftheplausiblejustifi- cationsforthediscrepancyobservedbetweenthecasesnoti-fiedinthestateofAmazonasandtheactualmagnitudeof theepidemic,ascomparedtotherestofthecountry.
Inthepopulationstudied,apredominanceofthemale gender(72.9%)isobserved,andthissignificantdifference betweenmenandwomenisinaccordancewiththefindings ofotherstudiescarriedoutinBrazil,4,12,17,19 despitetheten-dencyofAIDStoincreaseamongwomen.14,20
The population affected is young, at productive age, 60.1%agedbetween25and40years,butalreadyshowing anincreaseintheagebracketascomparedwiththecasesat thebeginningoftheAIDSepidemic.14 Ourdataareinac-cordancewiththestudybyPotteset al.(2007),17whohave also reported a large number of individuals (89.2%) with AIDSatthatagebracket.
Theeducationallevelexpressesdifferencesbetweenin- dividualsintermsofaccesstoinformation,andsomepa- rameterstoreachbetterqualityinpreventionandhealthas-sistanceareundeniablydirectlylinkedtothesocioeconomic levelofthepopulation,whosebetterindicatorsareeduca-tionallevel,income,andoccupation.17
InBrazil,therewasatendencytowardsAIDSpatientshav-ingahighereducationallevel.In1982,almostallcaseswere among individuals with university level or complete high schoollevel,whileonly24%ofthecaseswereamongilliterate individuals.Aninversioninthistrendhasbeenobservedsince 2000,with74%ofthecasesinformingtheeducationallevel wereilliterateorhadcompletedonlymiddleschool.21
These data are consistent with those presented in our study,inwhich80%ofthepatientsincludedhaveonlycom-pleted middle school, representing a low-income popula-tion,50%ofwhomreceiveuptooneminimumwage,20% areunemployed,andhavealoweducationallevel.
Inourstudy,mostofthepatientswerebornandcame from the capital of the state of Amazonas, the city of Manaus,wherethequalityoflifeandaccesstoinformation regardingdiseasepreventionisdirectlyrelatedtotheedu-cationalandsocioeconomiclevel,essentialfactorsinvolved inreducingtheratesofthediseasesinquestion,especially HIVinfection.
TheHIV/HCVcoinfectionrateofpatientscaredforat FMTAM was 2.6% (n = 70), and the world estimates, ac- cordingtosomeauthors,haverangedfrom4%to90%,de-pendingontransmissionroute.22
InBrazil,theNationalProgramofControlandPreven-tion ofViral Hepatitis has estimated, based on studies al-readycarriedoutinthecountrythattheprevalenceofHIV/ HCVcoinfectionrangesfrom17%to36%ofthecases,var-yingindifferentregions.23
Monteiroet al.(2004),24 studying406HIV-infectedindi-vidualsinthecityofBelém,inthestateofPará,havereported a16%prevalenceofHCVinfection.Carvalhoetal.(2009)25 inthecityofRecife,inthestateofPernambuco,studying the HIV/HCV coinfection have reported a low prevalence (4.1%)ascomparedwithotherstudiesintheliterature,pos-siblyduetodifferencesinriskfactorsforacquiringHCV.
The high variability depends not only on the risk fac-torstowhichthepopulationareexposedto,butalsoonthe methodsofHCVdetection.26
In the present study, the major risk factor found was sexual transmission, characterized by sexual promiscu- ity(84.3%),andSTDacquisition(47.1%)betweenhetero-sexual patients. This is in accordance with the studies by Szwarcwald (2000)27and Amaralet al. (2007),4 who have alsoshownthepredominanceofcoinfectionamongpatients havingheterosexualintercourse(68.6%)ascomparedwith menhavingsexwithmen(MSM)(22.8%).
The transmission modalities of HCV and HIV are knowntobesimilar,butthetransmissionefficiencyofeach virus differs. HCV transmission is more efficient through exposure to contaminated blood or blood products, espe-ciallythroughtheuseofinjectiondrugs.28Incertainhigh riskpopulations,suchasusersofinjectiondrugs,coinfec-tionispresentin72%to95%ofthem.6,29,30
Similarlytothenortheasternregionofthecountry,in thenorthernregion,themajordrugsknowntobeusedare cannabisandcocaine.12,17TheUnitedNationshasreported Brazil as the second country with the highest number of individuals with HIV among drug users in Latin Ameri-ca, in addition to being one of the major cocaine traffic routes.31
A recent study carried out in the state of Pernam-buco,inthenortheasternregionofBrazil,confirmsour study, also showing a low prevalence of coinfected in-dividualsinthisstate.25Theauthorshavereportedthat only8.4%ofthepatientsacquireHIVinfectionthrough the use of injection drugs, differently from the south-easternandsouthernregions,whoseratesare25.8%and 30.7%,respectively.Theyhavenotfoundapositiverela-tionbetweencoinfectionandtheuseofinjectiondrugs, inaccordancewithourstudy,inwhichthedrug-injec-tionuseratewasonly21.4%.25
DespitethesmallnumberofHIV/HCVcoinfectedpa- tients(4.42%)inourstudy,theannualdistributionaccord-ing to the frequency showed an ascendtients(4.42%)inourstudy,theannualdistributionaccord-ing curve, rangtients(4.42%)inourstudy,theannualdistributionaccord-ing from1.45%intheyear2000to5.03%in2007.
cases,fromtheinvestigationofhepatitiscasesinthosepa-tientsovertheyears,andfromthelongersurvivalofAIDS patientsduetotheuseoftheHAARTregimenintroduced in1996.
Itisworthnotingthatthedeathsinourstudy(34.3%)oc-curredmainlybetweentheyears2000and2003,whenthecause ofdeathcouldnotbeattributedtothepresenceofHCV.
Ourstudycanhaveunderestimatedtheactualprevalence ofcoinfectioninthepopulationstudiedduetotheexistence offloatationintheserologicstatusandevenseroconversion (the anti-HCV turns negative), which are 2.5 times more frequentamongHIV/HCVcoinfectedpatientsascompared withHCVmono-infectedpatients.32
Inanti-HCVpositiveimmunosuppressedpatients,HCV RNAshouldbeinvestigated,anditspresenceconfirmsthe diagnosis;however,anegativeresultdoesnotexcludeHCV infection,and,wheneversuspicionishigh,anewinvestiga-tionshouldbeperformedinsixmonths.33,34
However, in some active HCV infections, HCV RNA cannot be detected. This can occur in individuals whose anti-HCVantibodylevelsarehigh,andRNAlevelsarelow.35 Thus,HCVRNAcannotbedetectedincertainindividuals intheacutephaseofhepatitisC,butsuchfindingsaretran-sientandachronicinfectioncandevelop.36
The low HIV/HCV coinfection rate (4.42%) found in ourstudyascomparedtothatofotherregionscanbeat-tributednotonlytothesmallsizeofthesample,butalsoto thefactthatHCVinfectionanddiagnosisarestillincreasing intheregion.
Ontheotherhand,serologicaltestsareknowntohave lower sensitivity in the immunodeficiency scenario, and polymerasechainreaction(PCR)isrequiredforconfirming thediagnosis.
The present study suggests that larger studies are re-quired for better assessing the profile of this population and the prevalence of HIV/HCV coinfection in the state ofAmazonas.Thepresentstudyalsostressestheneedfor earlyinvestigationofhepatitisCinHIVpatientsbyusing bothserologicandmolecularmethods,becausethelitera-tureemphasizestheimpactofHIVinpatientswithHCV, regardingtherapidliverdiseaseprogressionandevolution todeath.
REFERENCES
1. Alter JM. Epidemiology of viral hepatitis and HIV co-infec-tion.JournalofHepatology2006;44:S6-S9.
2. MohsenAH.HepatitisCandHIV-1Coinfection.GUT2002; 51(4):601-8.
3. CorvinoSM,HenriquesRMS,GrottoRMTet al.Co-infecção
HIV/HCVempacientesdeBotucatueregião.RevBrasEpide-miol2007;10(4).
4. AmaralISA,AlmeidaML,AlvesFTet al
.Epidemiologiadepa-cientesco-infectadosHIV/HCVatendidosnaFundaçãoSanta Casa de Misericórdia do Pará. Revista do Para de Medicina 2007;21(1):15-20.
5. SorianoV,MiróJM,García-SamaniegoJet al .Consensusconfer-enceonchronicviralhepatitisandHIVinfection:updatespanish recommendations.JournalVirologyofHepatology2004;11:2-17. 6. LarsenC,PialouxG,SalmonDet al.Prevalenceofhepatitis
CandhepatitisBinfectioninthehiv-infectedpopulationof France,2004.Eurosurveillance2008;13(22):109-12.
7. Mast EE, Hwang LY, Set DSet al. Risk factors for perinatal transmissionofhepatitisCvirus(HCV)andthenaturalhis-toryofHCVinfectionacquiredininfancy.JournalInfectious Diseases2005;192:1880-9.
8. VandeLaarTJ,VanderBijAK,PrinsMet al.IncreaseinHCV incidenceamongmenwhohavesexwithmeninAmsterdam mostlikelycausedbysexualtransmission.JournalInfectious Diseases2007;196:230-8.
9. Silva ACM, Barone AA. Fatores de risco para infecção pelo HIVempacientescomovírusdahepatiteCRevistadeSaúde Pública2006;40(3):482-8.
10. Rodríguez-RosadoR,García-SamaniegoJ.Hepatotoxicityaf-terintroductionofhighlyactiveanti-retroviraltherapy.AIDS 1998;12:1256.
11. SorianoV,García-SamaniegoJ.Impactoofchronicliverdis-easeduetohepatitisvirusesascauseofhospitaladmissionand deathinHIV-infecteddrugusers.EuropeanJournalEpidemi-ology1999;15:1-4.
12. CarvalhoFHP,SilvaANMR,MeloHRLet al.Prevalênciado
anti-HCVempacientessoropositivosparaoHIV.Revistado ParádeMedicina2006;20(3):11-3.
13. IBGE – Instituto Brasileiro de Geografia e Estatística. Censo demográfico 2008; Disponível em: <http://ibge.gov.br/home/ estatistica/populacao/censo>.Acessoem:18abrilde2009. 14. BRASIL. Ministério da Saúde. Secretaria de Vigilância em
SaúdeProgramaNacionaldeDSTeAIDS.BoletimEpidemi-ológico.AnoVn001-Brasília,2008.Disponívelem:<http:// www.aids.gov.br/>.Acessoem:10abrilde2009.
15. Governo do Estado do Amazonas. Secretaria de Estado da Saúde. Coordenação Estadual do Programa DST/Aids da Fundação de Medicina Tropical do Amazonas. Boletim Epi-demiológicodaAidsnoAmazonas.AnoI–nº1.Brasília,2007. Disponível em: <http://portal.saude.gov.br/>. Acesso em: 10 abril2009.
16. BRASIL. Ministério da Saúde. Governo do Estado do Ama-zonas.SecretariadeEstadodaSaúde.CoordenaçãoEstadual doProgramaDST/AidsdaFundaçãodeMedicinaTropicaldo Amazonas. Boletim Epidemiológico da Aids no Amazonas. AnoII–nº1.Brasília,2007.Disponívelem:<http://portal. saude.gov.br/>.Acessoem:14dezembro2008.
17. PottesFA,BritoAM,GouveiaGCet al.Aidseenvelhecimento: característicadoscasoscomidadeigualoumaiorque50anos em Pernambuco, de 1990 a 2000. Rev Bras Epidemiol 2007; 10(3):338-51.
18. LuizRR,CostaAJL.Sobreacorreçãodanotificaçãodoscasos deAIDSno Brasil. BoletimEpidemiológico–AIDS. Brasília 2001;14(2).
19. Varella RB. Aspectos da epidemia de Aids em município de médioportedoRiodejaneiro,2000-2004.RevBrasEpidemiol 2006;9(4):447-53.
20. Aguiar JI, Uehara SN, Alexandrino POet al. Avaliação
pre-liminardaassociaçãodovírusdaImunodeficiênciaHumana (HIV)comashepatitesviraisdotipoBeCemdoiscentrosde investigação do Brasil. Revista Panamericana de Infectologia 2005;7(2):29-32.
22. Mendes-Corrêia MCJ, Barrone AA, Guastini C. Hepatits C vírusseroprevalenceandriskfactorsamongpatientswithHIV infection.RevSocBrasMedTrop2001;43(1):15-9.
23. SBI–BoletimdeatualizaçãodaSociedadeBrasileiradeInfec-tologia.Hepatitesviraistêmpapeldedestaqueentreagravos depacientesHIVpositivos2006;4,jul/ago/set.
24. MonteiroMC,NascimentoMMP,PassosADCet al.Hepatite C: prevalência e fatores de risco entre portadores do VIH/ SIDAemBelém,Pará,naAmazôniaBrasileira.RevSocBras MedTrop2004;37(2):40-6.
25. Carvalho FHP, Coelho MRC, Vilella TASet al. Co-infecção porHIV/HCVemhospitaluniversitáriodeRecife,Brasil.Rev. SaúdePública2009;43(1):133-9.
26. TovoCV,SantosDE,MattosAZet al.Avaliaçãodaimunidade
celularnospacientesCo-InfectadospelovírusdahepatiteCe vírus da imunodeficiência humana.Arq Gastroenterol 2007; 44(2):113-17,2007.
27. Szwarcwald CL, Bastos FI, Esteves MAPet al.A
dissemi-nação da epidemia da AIDS no Brasil, no período de 1987-1996:Umaanáliseespacial.CadSaudePublica2000; 16(1):S07-19.
28. MontoA,CurrieS,WrightTL.Liverdiseaseininjectiondrug userwithhepatitisC,withandwithoutHIVcoinfection.JAd-dictDis2008;27(2):49-59.
29. ChengDM,NunesD,LibmanHet al.ImpactofHepatitisC onHIVProgressioninAdultsWithAlcoholProblems.Alcohol ClinExpRes2007;31(5):829-36.
30. PolS,SorianoV.ManagementofchronichepatitisCvirusinfection inHIV-infectedpatients.ClinInfectDis2008;47(1):94-101. 31. BRASIL. Ministério da Saúde. Agência Nacional da AIDS,
2005. Disponível em: <http://www.sistemas.aids.gov.br/>. Acessoem:20janeiro2009.
32 Chamot E, Hirschel B, Winstsch Jet al. Loss of antibodies
againsthepatitisCvirusinHIV-seropositiveintravenousdrug users.AIDS1990;4:1275-7.
33. Lakshmi V, Reddy AK, Dakshinamurty KV. Evaluation of commerciallyavailablethird-generationanti-hepatitisCvirus enzyme-linkedimmunosorbentassayinpatientsonhaemodi-alysis.IndianJMedMicrobiol2007;25:140-2.
34. SBI–IConsensodaSociedadeBrasileiradeInfectologiapara oManuseioeTerapiadaHepatiteC2008;35-9.
35. BuschMP,KleinmanSH,JacksonBet al.Nucleicacidtesting
of blood donors for transfusion-transmitted infectious dis-eases:reportofinterorganizationTaskForceonNucleicAcid AmplificationofBlooddonors.Transfusion2000;40:143-59. 36. ThomasDL,AstemborskiJ,RaiRMet al.Naturalhistoryof