J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 43/Oct. 26, 2015 Page 7758
AN ANALYSIS OF CLINICOPATHOLOGICAL AND SURGICAL
OUTCOME IN SALIVARY GLAND TUMORS OF 178 PATIENTS OF
TELANGANA
Boda Kumarswamy1
HOW TO CITE THIS ARTICLE:
Boda Kumarswamy. “An Analysis of Clinicopathological and Surgical Outcome in Salivary Gland Tumors of 178 Patients of Telangana”. Journal of Evidence based Medicine and Healthcare; Volume 2, Issue 43, October 26, 2015; Page: 7758-7767, DOI: 10.18410/jebmh/2015/1047
ABSTRACT: INTRODUCTION: The incidence of tumors of Salivary glands is not uncommon in the surgical practice in Telangana state. In the present study 178 patients with a clinical diagnosis of salivary gland tumors between 2006 and 2014 at Warangal, Telangana were analyzed both retrospectively (2006-2010) and prospectively (2011-2014). Demographic data like age, sex and clinical features like tumor location, FNAC reports, CT scan findings, nature of growth and predisposing factors were recorded. All the patients with benign tumors were managed by surgical excision and malignant lesions with surgery in combination with Radiotherapy. Cervical lymph node metastases were managed by RT and neck dissection. AIM:
This study aims at analyzing the clinical, pathological, Surgical and RT outcome of Salivary gland Tumors in patients attending a large tertiary Hospital at Warangal, rendering services to four districts of Telangana. STUDY DESIGN: 178 patients diagnosed as SGTs retrospectively and prospectively and undergoing surgical treatment were analyzed with respect to their clinical, cytological and surgical outcome. RESULTS: There were 143 patients with benign tumors and 35 patients with malignant tumors. The mean age was 41.3±2.6 years for benign tumors and 65.4±1.8 for the malignant tumors. Parotid gland was commonly involved 75(42.13%) followed minor salivary glands of Hard palate 29(16.29%) and Submandibular gland 23(12.92%). Remaining 51(28.65%) patients presented with tumors involving cheek, lips and floor of the mouth. Among the benign tumors Pleomorphic adenoma accounted for 94(52.80%) and warthin’s tumor for 23(12.92%). Among malignant tumors Mucoepidermoid carcinomas were 12(6.74%), adenocarcinomas 9(5.05%), adenoid cystic carcinomas 6(3.37%) and Acinic cell carcinomas 5(2.80%), EMC 2(1.12%) and Myoepiothelial carcinoma 1(0.56%). CT scan, MRI studies were helpful in deciding the route of approach and risk of involvement of deeper vascular structures with a sensitivity of 63.48%. Facial nerve paralysis was reported in 3.37% and recurrence rate was more with pleomorphic adenomas 6.17%. CONCLUSIONS: The analysis of SGTs from this part of India showed the incidence was higher in females than males. Pleomorphic adenoma was the commonest tumor observed in the present study. Parotid gland was involved in majority of the tumors followed by hard palate involving minor salivary glands. CT scan and MRI proved to be helpful in the diagnosis and determining the approach with a sensitivity of 63.48%. Primary excision of benign tumors resulted in low recurrence rate. Malignant tumors showed better results with surgery and RT combined. Incidence of Facial palsy following SGTs surgery was lowest reported from the center.
KEYWORDS: Parotid, Sub Mandibular, tumors, carcinoma, Mucoepidermoid carcinoma, warthin’s
J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 43/Oct. 26, 2015 Page 7759 INTRODUCTION: Salivary Gland Tumors (SGTs) are a group of heterogeneous disease complexes with variable clinicopathological features. They have a distinct biological nature and account for 3 to 10% of the Head and Neck Neoplasms.1-3 WHO reports quote an annual incidence of 0.4 to 13.5 cases per 100, 000 populations anywhere in the world? The incidence reported in USA is 0.3%4 whereas the reports from other parts of the world are different, indicating variable frequency of these tumors.5,6 These differences can also be due to variation in the cytological reporting by different centers worldwide.7 Usually the tumors remain asymptomatic, appearance of quick growth, pain; facial weakness and ulceration denote malignant transformation. The treatment of salivary gland malignancies remains primarily surgical, although adjunctive radiotherapy may play an important role in those patients with advanced-stage disease.8 Lu and Ly et al concluded that the parotid gland and palate were the most common locations of salivary gland tumors. Pleomorphic adenoma and Mucoepidermoid carcinoma were the most frequent benign and malignant tumors, respectively.9 Studies show that PLGA is a tumor of minor salivary gland distinct from adenoid cystic carcinoma and benign mixed tumor for therapeutic and prognostic considerations. Conservative but complete surgical excision is the treatment of choice for these slow-growing tumors with a low proliferation index; adjuvant therapy does not appear to alter the prognosis.10 The present study analyses the SGTs over a period of 9 years between 2006 and 2014 in terms of predisposing factors, Histopathological and location of tumor and its treatment.
J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 43/Oct. 26, 2015 Page 7760 OBSERVATIONS AND RESULTS: 178 patients were included in the present study, out of which 114(64.04%) patient’s data was extracted from past medical records belonging to the period 2006 to 2010. 64(35.95%) patients belonged to the prospective analysis group from the year 2011 to 2014. There were 143(80.33%) patients with benign tumors and 35(19.66%) patients with malignant tumors. The benign to malignant tumors ratio was 4.0:1. The patients with benign tumors belonged to the age groups of 24 to 49 years with a mean age of 41.3±2.6 years. The patients belonged to the age groups between 55 and 69 years for malignant tumors with a mean age of 65.4±1.8 years. The present study showed among 178 patients, 106(62.92%) were females and 72(37.07%) males with a ratio of 1.47:1. The female to male ratio among the patients with benign tumors was 1.42:1 (female 84: male 59), similarly the male to female ratio for the patients with malignant tumors was 1.69:1 (female22 and male 13). 88 patients (49.43%) with benign tumors belonged to the age group between 21 and 50 years. Among the malignant tumors Mucoepidermoid carcinomas were equally distributed in all age groups and the incidence increasing with the age of the patients. (Table 1)
Age group in Years 21-30 31-40 41-50 51-60 61-70
Sex M F M F M F M F M F
Benign Tumors-143
Pleomorphic adenoma-94-52.80% 12 16 14 12 10 08 05 10 03 04
Warthin’s tumor-23-25.87% 03 03 02 03 01 04 01 02 01 03
Canalicular adenoma-12 % 02 01 01 01 01 01 00 02 01 02
Cystadenoma 06-% 01 01 00 02 00 01 00 01 00 00
Myoepithelioma-03- 2.09% 00 00 00 01 00 01 00 01 00 00
Basal cell adenoma-03-8.39% 01 00 00 01 00 00 00 01 00 00
Oncocytoma 2 00 00 00 01 01 00 00 00 00 00
Malignant tumors-35
Mucoepidermoid carcinoma-12 (54.28%) 02 01 01 02 01 01 00 01 01 02
Adenocarcinomas-09(25.71%) 00 02 01 02 00 02 00 01 00 01
Adenoid Cystic carcinoma-06(11.42%) 00 00 01 01 00 00 01 01 01 01 Acinic cell carcinoma-05(8.57%) 01 00 01 01 00 00 00 00 01 01
EMC 2 00 00 00 00 00 01 00 00 00 01
Myoepithelial carcinoma-1(0.56%) 00 00 00 00 00 00 00 01 00 00
Total 22 24 21 27 14 19 07 21 08 15
Table 1: Showing the distribution of SGT according to the age of the patients (n=178)
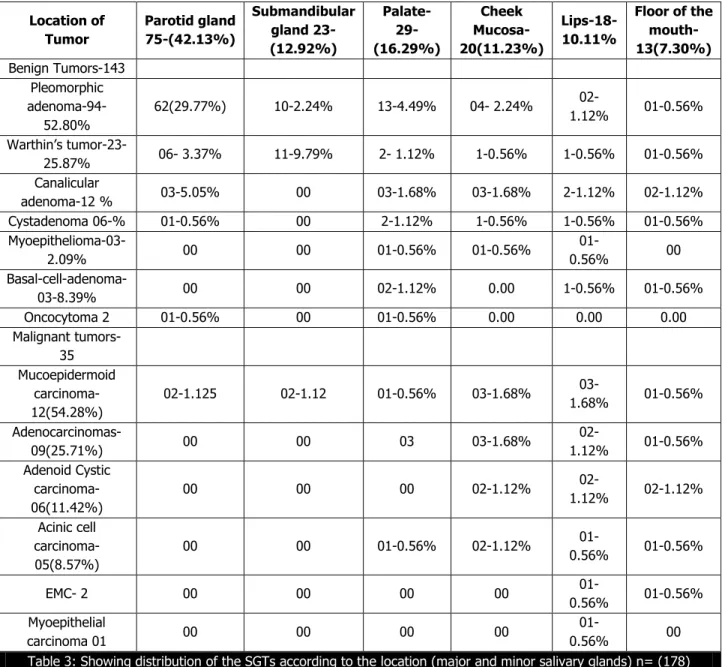
J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 43/Oct. 26, 2015 Page 7761 25.71% of the malignant tumors. Adenoid cystic carcinomas were 6 or 3.37% of the total and 17.1% of the malignant tumors (Table 2). The incidence of Pleomorphic adenoma in males was 44(24.71%) and in females was 50 (30.33%) of the total tumors. Similar sex incidence of other tumors is shown in table 2. Parotid gland was affected in 54(30.33%) of the total patients of 178, followed by hard palate in (16.29%), the Submandibular gland in 23(15.873%) and cheeks in 20(11.23%). Tumors from lips constituted 18(10.11%) and floor of the mouth 13(7.30%). There was no case reported affecting the sublingual gland. Among the benign tumors parotid gland, followed by hard palate and lips were involved in the order of frequency, whereas among the malignant tumors it was Hard palate, parotid gland, sub Mandibular gland and cheek were involved (Table 3). Analyzing the involvement of the Major and Minor salivary glands with SGTs showed that 98(55.05%) tumors were located in parotid and Submandibular glands. The remaining 80(44.94%) of the tumors were arising from the minor salivary glands. The ratio was major: Minor= 1.2:1 (Table 3).
n
178 %
% in the group of benign or
malignant tumors
Gender
Male Female
n % n %
Benign tumors
Pleomorphic adenoma 94 52.80 72.72 44 24.71 50 28.08
Warthin’s tumor 23 12.92 14.30 08 4.49 15 8.42
Canalicular adenoma 12 6.74 4.89 5 2.80 07 3.93
Cystadenoma 06 3.37 2.79 1 0.56 05 2.80
Myoepithelioma 03 1.68 2.09 0 0.0 03 1.68
Basal cell adenoma 03 1.68 2.09 0 0.0 03 1.68
Oncocytoma 02 1.12 1.39 1 0.56 01 0.56
Total 143 80.31 100 59 33.14 84 47.19
Malignant tumors
Mucoepidermoid
carcinoma 12 6.74 31.40 05 2.80 07 03.93
Adenocarcinomas 09 5.05 22.85 04 2.24 05 02.80
Adenoid-cystic carcinoma 06 3.37 20.00 01 3.37 05 02.80
Acinic cell carcinoma 5 2.80 08.57 3 0.6 02 01.12
EMC 2 1.12 08.57 0 0.2 02 01.12
Myoepithelial carcinoma 1 0.56 08.57 0 0.0 01 0.56
Total 35 19.64 100 13 07.30 22 12.35
J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 43/Oct. 26, 2015 Page 7762 Location of Tumor Parotid gland 75-(42.13%) Submandibular gland 23-(12.92%) Palate- 29-(16.29%) Cheek Mucosa-20(11.23%) Lips-18-10.11%
Floor of the mouth-13(7.30%) Benign Tumors-143 Pleomorphic adenoma-94-52.80%
62(29.77%) 10-2.24% 13-4.49% 04- 2.24%
02-1.12% 01-0.56% Warthin’s tumor
-23-25.87% 06- 3.37% 11-9.79% 2- 1.12% 1-0.56% 1-0.56% 01-0.56% Canalicular
adenoma-12 % 03-5.05% 00 03-1.68% 03-1.68% 2-1.12% 02-1.12% Cystadenoma 06-% 01-0.56% 00 2-1.12% 1-0.56% 1-0.56% 01-0.56% Myoepithelioma-03-
2.09% 00 00 01-0.56% 01-0.56%
01-0.56% 00
Basal-cell-adenoma-03-8.39% 00 00 02-1.12% 0.00 1-0.56% 01-0.56%
Oncocytoma 2 01-0.56% 00 01-0.56% 0.00 0.00 0.00
Malignant tumors-35 Mucoepidermoid
carcinoma-12(54.28%)
02-1.125 02-1.12 01-0.56% 03-1.68%
03-1.68% 01-0.56%
Adenocarcinomas-09(25.71%) 00 00 03 03-1.68%
02-1.12% 01-0.56% Adenoid Cystic
carcinoma-06(11.42%)
00 00 00 02-1.12%
02-1.12% 02-1.12% Acinic cell
carcinoma-05(8.57%)
00 00 01-0.56% 02-1.12%
01-0.56% 01-0.56%
EMC- 2 00 00 00 00
01-0.56% 01-0.56% Myoepithelial
carcinoma 01 00 00 00 00
01-0.56% 00
Table 3: Showing distribution of the SGTs according to the location (major and minor salivary glands) n= (178)
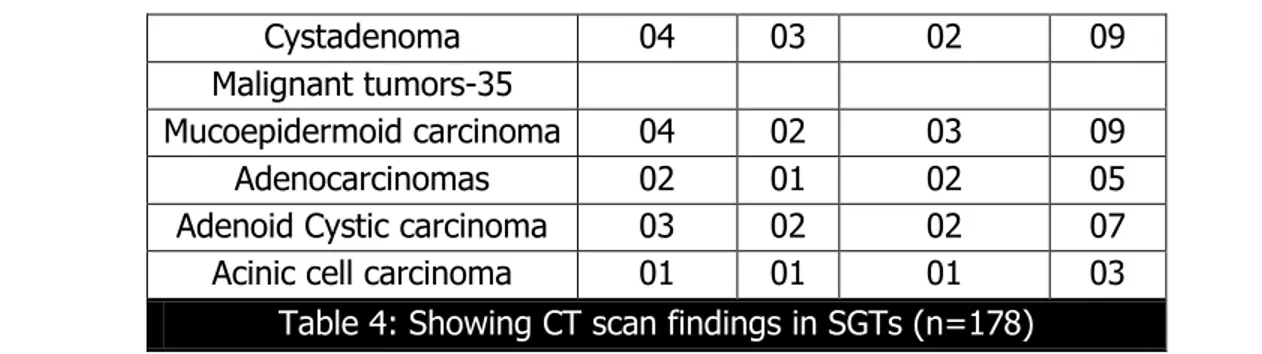
All the patients were not subjected to the uniform investigations due to the time period of one decade and non-availability of sophisticated CT scan and MRI in the earlier years when compared to the later years of the study. CT scan and MRI and Scintiscan were useful in diagnosing and helpful in decision making of the type of surgery in 63.48% of the patients (Table 4).
CT scan MRI Scinti scan Total
Benign Tumors-143 113
Pleomorphic adenoma 33 16 04 53
Warthin’s tumor 14 04 01 19
J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 43/Oct. 26, 2015 Page 7763
Cystadenoma 04 03 02 09
Malignant tumors-35
Mucoepidermoid carcinoma 04 02 03 09
Adenocarcinomas 02 01 02 05
Adenoid Cystic carcinoma 03 02 02 07
Acinic cell carcinoma 01 01 01 03
Table 4: Showing CT scan findings in SGTs (n=178)
All the benign tumor patients were taken up for primary excision of their tumors with an incidence of facial palsy in 4(2.24%), recurrence rate of 5.05%.(9) Inoperable status was encountered due to close proximity to large vessels was encountered in 11(6.17%) of the patients. These patients were managed by leaving tumor mass attached to the vessels. Facial nerve infiltration was found in 47(26.40%) of the patients. By far this study has shown the largest incidence of such a situation due to tumor being adherent to the nerve. Capsular infiltration by the tumor was found in 25 (14.04%) of the patients (Table 5).
Benign Tumors-143
Primary Excision
Facial nerve paralysis
Recurrence Not operable
Neck dissection
for Secondaries
Facial nerve infiltration
Capsule infiltration-with tumor
Radiotherapy
PA
-94-52.80% 94 03 03 04 00 32 21 00
WT-23-25.87% 23 01 02 04 00 09 03 00
CA-12
% 12 00 03 03 00 04 01 00
Cyst A
06-% 06 00 01 00 00 02 00 00
Myo E-03- 2.09%
03 00 00 00 00 00 00 00
BCA-03-8.39% 03 00 00 00 00 00 00 00
O C- 2 02 00 00 00 00 00 00 00
Total 143 04 09 11 00 47 25 00
Table 5: Showing Intra operative findings and Surgical and RT management of Benign SGTs (n=178)
J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 43/Oct. 26, 2015 Page 7764 Malignant
tumors-35
Primary Excision
Facial nerve paralysis
Recurrence Not operable
Neck dissection
for Secondaries
Facial nerve infiltration
Capsule infiltration-with tumor
Radio-therapy
Mucoepidermoid carcinoma-12(54.28%)
10 01 01 02 04 05 03 08
Adenocarcinomas-09 (25.71%) 07 01 00 01 02 03 02 08
Adenoid Cystic carcinoma-06(11.42%)
06 00 00 01 01 01 01 05
Acinic cell carcinoma-05(8.57%)
05 00 01 01 01 00 00 05
EMC- 2 01 00 00 00 01 00 00 01
Myoepithelial
carcinoma 01 01 00 00 00 01 00 00 01
Total 30
02-1.12% 2-1.12%
5-2.80% 10-5.61% 9-5.05% 6-3.37% 28 Table 6: Showing Intra operative findings and Surgical
and RT management of Malignant SGTs (n=178)
The disease-free survival rate and loco-regional control rate at 5 years were 87% and 90%, respectively.
J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 43/Oct. 26, 2015 Page 7765 studies. Chidzonga MM, Lopez Perez VM et al reported parotid gland as the commonest site for both benign and malignant tumors. By reviewing the studies from two distant centers, Bello et al commented that most of the malignant tumors occur in the parotid glands in the Finnish population whereas in Israelis they occur in minor salivary glands.18,15 In contrast to the present study Submandibular gland was found to be the second most affected gland with tumors.19 In the present study. Were benign and were malignant tumors which are in confirmation with previous studies.19,20 Pleomorphic Adenoma (PA) was the commonest benign salivary gland tumor affecting both major and minor salivary glands reported in majority of the studies. In this study also PA is by far the commonest tumor with an incidence of 52.80 % of all tumors and 98/72 (73.46%) of the major and 26/98 (26.53%) of the minor salivary glands and affecting the men in 2nd to 5th decades of life. The second commonest tumor was Warthin’s tumor with an incidence of 25.87% of all tumors and 16.08% of benign tumors. As Warthin’s tumor occurs exclusively in parotid gland it is rarely reported in literature reporting tumors of minor salivary glands. Hence canalicular adenoma may be named as the second most common tumor after PA.15 In majority of literature Mucoepidermoid carcinoma (MEC) was reported as the most common malignant tumor of salivary glands; similarly present study showed MEC as 12/178 (6.74%) of all tumors 4/98 (4.08%) of major and 8/80 (10%) of minor salivary glands. It was mainly diagnosed in females in fifth decade.21 Adenocarcinomas were reported to be second commonest in the present series of patients accounting for 5.05% of all tumors and 25.71% of malignant tumors. This reporting is similar to a report from Ellis GL, Auclair PL et al.22 The third commonest malignant tumor observed in the present study was adenoid cystic carcinoma affecting the Submandibular and palatal minor glands with almost equal sex distribution. But in the literature it is reported as the second most common malignant tumor of salivary glands.23
CONCLUSIONS: The incidence of Salivary gland Tumors is worldwide, epidemiological evidence available in the literature when compared to the present study reveals the incidence is commoner in women. In the absence of definite etiology like tobacco and industrial toxins in women but higher occurrence in them, needs further scientific study. Pleomorphic adenoma is the single largest lesion in this group of tumors with parotid gland commonly affected. Tumors arising from the major glands are benign and those from minor glands are malignant. The incidence of benign tumors is almost equal in all age groups. Surgery remains the main stay of treatment with RT for malignant tumors and for recurrences. Early diagnosis and meticulous surgical dissection avoids complications like facial weakness and recurrences as found in the present study.
REFERENCES:
1. Ansari MH. Salivary gland tumors in an Iranian population: a retrospective study of 130 cases. J Oral Maxillofac Surg 2007; 65: 2187-94.
2. Vargas PA, Gerhard R, Araújo Filho VJF, Castro IV. Salivary gland tumors in a Brazilian population: a retrospective study of 124 cases. Rev Hosp Clín Fac Med S Paulo 2002; 57: 271-6.
J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 43/Oct. 26, 2015 Page 7766 4. Barnes L, Eveson JW, Reichart PA, Sidranskiy D. World Health Organization classification of
tumours. Pathology and genetics of head and neck tumours. Lyon, France: IARC; 2005. p. 211-81.
5. Ito FA, Ito K, Vargas PA, de Almeida OP, Lopes MA. Salivary gland tumors in a Brazilian population: a retrospective study of 496 cases. Int J Oral Maxillofac Surg 2005; 34: 533-6. 6. Luksic I, Virag M, Manoilovic S, Macan D. Salivary gland tumours: 25 years of experience
from a single institution in Croatia. J Craniomaxillofac Surg 2012; 40: e75-81.
7. Kokemueller H, Swennen G, Brueggemann N, Brachvogel P, Eckardt A, Hausamen JE. Epithelial malignancies of the salivary glands: clinical experience of a single institution—a review. Int J Oral Maxillofac Surg 2004; 33: 423-32.
8. Bell RB, Dierks EJ, Homer L, Potter BE. Management and outcome of patients with malignant salivary gland tumors, J Oral Maxillofac Surg. 2005 Jul; 63(7): 917-28.
9. Li LJ, Li Y, Wen YM, Liu H, Zhao HWClinical analysis of salivary gland tumor cases in West China in past 50 years. Oral Oncol. 2008; 44(2): 187-92.
10.Castle JT1, Thompson LD, Frommelt RA, Wenig BM, Kessler HP. Polymorphous low grade adenocarcinoma: a clinicopathologic study of 164 cases.. Cancer. 1999 Jul 15; 86(2): 207-19.
11.Kara MI, Göze F, Ezirganli S¸, Polat S, Muderris S, Elagoz S. Neoplasms of the salivary glands in a Turkish adult population. Med Oral Patol Oral Cir Bucal 2010; 15: e880-5.
12.Al-Khateeb TH, Ababneh KT. Salivary tumors in north Jorda-nians: a descriptive study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 103: 53-9.
13.Lima SS, Soares AF, Amorim RFB, Freitas RA. Epidemiologic profile of salivary gland neoplasms: analysis of 245 cases. Rev Bras Otorrinolaringol 2005; 71.
14.Mejía-Velázquez CP, Durán-Padilla MA, Gómez-Apo E, Quezada-Rivera D, Gaitán-Cepeda LA. Tumors of the salivary gland in Mexicans. A retrospective study of 360 cases. Med Oral Patol Oral Cir Bucal 2012; 17: e183-9.
15.Bello OI, Salo T, Dayan D, Tervahauta E, Almangoush A, Schnaiderman-Shapiro A, et al. Epithelial salivary gland tumors in two distant geographical locations, Finland (Helsinki and Oulu) and Israel (Tel Aviv): a 10-year retrospective comparative study of 2,218 cases. Head Neck Pathol. Epub ahead of print 7 Jan 2012.
16.Subhashraj K. Salivary gland tumors: a single institution expe-rience in India. Br J Oral Maxillofac Surg 2008; 46: 635-8.
17.Satko I, Stanko P, Longauerová I. Salivary gland tumours treated in the stomatological clinics in Bratislava. J Craniomaxillofac Surg 2000; 28: 56-61.
18.Chidzonga MM, Lopez Perez VM, Portilla-Alvarez AL. Salivary gland tumours in Zimbabwe: report of 282 cases. Int J Oral Maxillofac Surg 1995; 24: 293-7.
19.Satko I, Stanko P, Longauerová I. Salivary gland tumours treated in the stomatological clinics in Bratislava. J Craniomaxillofac Surg 2000; 28: 56-61.
J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 43/Oct. 26, 2015 Page 7767 21.Tilakaratne WM, Jayasooriya PR, Tennakoon TM, Saku T. Ep-ithelial salivary tumors in Sri
Lanka: a retrospective study of 713 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 108: 90-8.
22.Ellis GL, Auclair PL. Tumors of the salivary glands. 4th ed. Washington, DC, American Registry of Pathology; 2008.
23.Vuhahula EAM. Salivary gland tumors in Uganda: clinical path-ological study. Afr Health Sci 2004; 4: 15-23.
NAME ADDRESS EMAIL ID OF THE CORRESPONDING AUTHOR: Dr. Boda Kumarswamy,
H. No. 3-16-197/A/1, Near Tata Motors,
Peddammagadda, Hanamkonda, Warangal-506007, Telangana.
E-mail: bodakumarswamy123@gmail.com
Date of Submission: 14/10/2015. Date of Peer Review: 15/10/2015. Date of Acceptance: 19/10/2015. Date of Publishing: 26/10/2015.
AUTHORS:
1. Boda Kumarswamy
PARTICULARS OF CONTRIBUTORS: 1. Assistant Professor, Department of