RevBrasAnestesiol.2017;67(4):435---438
REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologia www.sba.com.brCLINICAL
INFORMATION
Post
operative
visual
loss
after
cervical
laminectomy
in
prone
position
Kumar
Naren
Chandra
∗,
Meghraj
Kundan
VardhmanMahavirMedicalCollege&SafdarjangHospital,NewDelhi,India
Received16August2016;accepted25November2016
Availableonline16December2016
KEYWORDS
Spinesurgery; Postoperativevisual loss;
Proneposition; Centralretinalartery occlusion
Abstract Postoperativevisuallossisarareanddevastatingcomplication.Theestimated inci-denceis0.01---1%afternonocularsurgery.Ithasbeenreportedafterspine,cardiacandhead andnecksurgeries.Wereportapatientwhowasoperatedforcervicallaminectomyinprone positionandcomplainedoflossofvisioninoneeyepostoperatively.Hewasthoroughly investi-gatedaftervisualloss.Thecasewasdiagnosedascentralretinalarteryocclusion(CRAO)ofthe lefteye.Hereweconsiderthepotentialetiologicalfactorscausingthisunilaterallossofvision andtrytosuggeststrategiestoreducetheincidenceofthecomplicationinspinalsurgery. ©2016SociedadeBrasileiradeAnestesiologia.Publishedby ElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
PALAVRAS-CHAVE
Cirurgiadacoluna; Perdavisual pós-operatória; Posic¸ãoprona; Oclusãodaartéria centraldaretina
Perdavisualnopós-operatóriodelaminectomiacervicalempronac¸ão
Resumo Aperdavisualpós-operatóriaéumacomplicac¸ãoraraedevastadora.Aincidência estimadaéde0,01---1%apóscirurgianãooftalmológica.Hárelatosdesuaocorrênciaapós cirur-giasdacoluna,cardíacaedecabec¸aepescoc¸o.Relatamosocasodeumpacientesubmetido àlaminectomiacervicalempronac¸ãoquesequeixoudeperdadevisãoemum dosolhos no pós-operatório.Opacientefoiprofundamenteinvestigadoapósaperdavisual.Ocasofoi diag-nosticadocomooclusãodaartériacentraldaretina(CRAO)doolhoesquerdo.Aquiconsideramos ospotenciaisfatoresetiológicosquecausamessaperdaunilateraldavisãoetentamossugerir estratégiasparareduziraincidênciadessacomplicac¸ãoemcirurgiadecolunavertebral. ©2016SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigo OpenAccess sobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
∗Correspondingauthor.
E-mail:kncjsr@rediffmail.com(K.N.Chandra).
http://dx.doi.org/10.1016/j.bjane.2016.11.003
436 K.N.Chandra,M.Kundan
Introduction
Postoperativevisuallossisanunexpectedandrare compli-cationandestimatedincidenceis0.01---1%afternonocular surgery.1---4 Review of literature reveals suchcases as
iso-lated case reports. Patil et al.5 found an overall rate of
0.094%in spine surgerydischargesin USNationwide Inpa-tientSamples(NIS).Mostcommoncausesofpostoperative vision loss are ischaemic optic neuropathy, central reti-nalarterythrombosisandcorticalblindness.Amongthese ischaemicopticneuropathyisfrequentlyobservedcauseof postoperativevisuallossfollowinggeneralanesthesia.1The
secondmostprevalentcauseofpostoperativevisuallossin patientsoperated in the pronepositionfor spinalsurgery iscentralretinalarteryocclusion(CRAO).Therearesome recognizedpreoperativeriskfactorswhichincludediabetes mellitus,hypertension,smoking,renalfailure,narrowangle glaucoma, polycythemia, atherosclerotic vascular disease andcollagenvasculardisorders.6
Case
report
A56yearoldman(170cm,88kg,BMI30.45kg.m−2)cameto
ourhospitalintheNeurosurgerydepartmentwiththe pre-sentingcomplainofpaininleftshoulderradiatingtoleftarm for2years.He hadtinglingsensation inleftarm andpain intherightarmforlast2years.Patienthadhistoryof dia-betesmellitussince4years.Hisbloodsugarwasderanged becausehehadnottakenoralhypoglycemicagentforlast fifteendays.Hewasputonadiabeticdietandantidiabetic drugwasstarted. There washistory of smokingsinceten years.Thepatienthadnoothersignificantdisease.
On examination there was mild upper limb weakness more on left then right. Sensory component was intact. There was no restriction of movement in upper limb. A Magnetic Resonance Imaging (MRI) scan of cervical spine wasperformedwhichrevealedadvancedcervical spondylo-siswithdisco---degenerativenerverootcompressionatC3---4 toC6---7levelwithsecondarycentralcanalstenosis.Hisall preoperativeroutineinvestigationswerewithinnormallimit exceptbloodsugarwhichwas216mg.dL−1.Hisblood
pres-surewas126/78mmHgandhisheartratewas82beats/min. Considering the neurological involvement the surgeon decidedtoperform Endoscopiclaminectomy at C5---6 and C6---7level.Generalanesthesiawasplannedforthepatient. Two 16gauge peripheral intravenous cannulae wasput in both the hands. Anesthesia was induced with midazolam 1mg, propofol 150mg and a bolus of fentanyl 150mcg. Trachealintubation with a size of 8.5mm reinforced oral endotracheal tube was facilitated with vecuronium 6mg. Urinarycatheter wasinserted and patientwas positioned prone. The eyes were protected with chloramphenicol ointmentbeforebeingtapedandpadded.Patientwas sub-sequentlyputontheoperatingtableintheproneposition. His neck was maintained in the midline position using a horse-shoeheadholderwithslightflexion,sothathisback would remain in neutral position with the head remain-ing slightly dependent. Anesthesia was maintained with isoflurane0.8---1.4%. Totalduration of surgerywas around 170minandadditional70minwererequiredforthe induc-tion and cessation of anesthesia. Systolic blood pressure
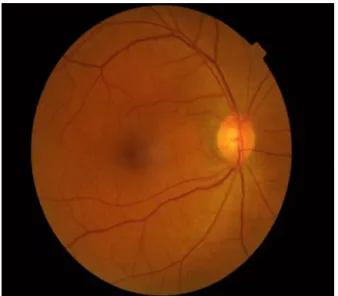
Figure1 Funduspicture ofleft eyeshowing pallor.Retinal
pallorwithattenuatedarteries.
ofthepatientwasmaintainedbetween90and120mmHg throughout theprocedure. Therewas400mLofblood loss duringthesurgerywhichwasreplacedwith1500ofnormal salineandmaintainthebloodpressureonacceptablelevel. At the end of operation, the patient was turned into supine position and transported to the critical care unit with endotracheal tube in place for elective ventilation. There was mild facial swelling and bilateral conjunctival congestion. During overnight elective ventilation patient maintainedhisvitalparameters.Afterreevaluationhewas extubated in the morning. On the first postoperative day following extubation, hecomplained of reduced vision in the lefteye. Immediate opthalmologicalexamination was conductedbyanophthalmologist.
Onexaminationvisualacuitywasfoundtobereducedto perception of light in the left eye while in the right eye it was normal (6/6). Left eye had puffiness of lids, mild proptosis and conjunctival congestion. Extraocular move-mentshowedrestrictedadductionandalsoinelevationand depressioninleftlateralgaze.Intraocularpressureofboth eyeswerenormal.Leftpupilwasmoderatelydilatedwith Relative Afferent Pupillary Defect (RAPD). Fundus exami-nation revealed pallor withoedemaof central retina and adullfovealreflex(Fig.1).Retinalarterieswerethinwith alteredAVratio.Fundusexaminationofrighteyewasnormal (Fig.2).PatientwasgivenacourseofmethylprednisoloneIV 1gdailyfor3days.Despitethis,thevisiondeterioratedto noperceptionoflight.OnfifthdayMRIofrighteyewas nor-malbutleftorbitshoweddiffuseswellingofbellyofmedial rectusmuscle.Casewasdiagnosedacentralretinalartery occlusion(CRAO)oflefteye.
Discussion
Cervicallaminectomyinpronepositioncause’svisualloss 437
Figure2 Normalfunduspictureofrighteye.
commonlyreportedcausesofpostoperativevisuallossare central retinal artery occlusion (CRAO)or vein occlusion, ischaemic optic neuropathy and cerebral ischaemia.7,8
Diabetesmellitus,smoking,chronichypertension,vascular disease and coagulopathy are the potential risk factors for this complication.6 The role of these factors in the
pathogenesisof visualloss inthe setting ofspinal surgery stillremainsunknown.Ourpatientwasaknownsmokerand wasalsosufferingfromdiabetesmellitus.
Externalcompressionovertheorbit,retrobulbar haem-orrhage,ortoosmallorbitalspacecanalsoadverselyaffect retinal circulationleading toCRAOandretinal ischaemia. Leibovitchetal.9intheircasereporthavementionedabout
ischaemicorbitalcompartmentsyndromeinproneposition. Itwasconsideredthatinpronepatienta10◦reverse
Trende-lenbergpositionnormalizedtheintraocularpressure.10Our
patient washeavy built andobese (BMI 30.45kg.m−2), so orbitalspacecouldalreadyhavebeencompromiseddueto abundantorbitalfat,andtheslightestinsultfromprolonged pronepositionmayhaveprecipitatedretinalischaemiadue to central retinal artery occlusion. Moreover diabetes is knowntocausevascularchangeswhichwouldhave precipi-tatedtheeventinourcase.Jampolandcollegues11hasalso
reportedischaemiaof the ciliaryarterial circulation from ocular compression. Retinal embolus is another potential cause for artery occlusion but this generally occurs after acardiacsurgery.
InreviewofpublishedcasesofCRAOafterspinesurgery, Kumarandcolleagues12 describedsignsandsymptomsthat
included unilateral vision loss, nolight perception, affer-ent pupillary defect, periorbital, eyelid oedema or both, chemosis, proptosis, ptosis, paraesthesia of the supraor-bitalregion,hazyorcloudycornea,lossofeyemovements, ecchymosis or other trauma near the eye. Proptosis and extraocularmuscleswellinghasbeenseeninsomecasesin earlyorbitalComputedTomography(CT)orMagnetic Reso-nanceImaging(MRI).Macularorretinaloedema,cherryred spotorattenuatedretinalvesselsweretypical.Ourpatient’s clinicalpresentationresembledthecasereportedbyKumar etal.
Ischaemic optic neuropathy (ION) has been reported in wide variety of surgical procedures like cardiothoracic
surgery,13instrumentedspinalfusionoperations,14headand
necksurgery,15nasalandsinussurgery.16Anteriorischaemic
opticneuropathytypicallyappearsasopticdiscoedemaand peripapillayhaemorrhageandoccursduetoabnormaloptic nervebloodflowfromhypotension,anaemiaoranemboli. Prolongedpronepositionalsoincreasestheintraocular pres-sure causing acute angle closure glaucoma. It is found thatraisedIOPsignificantlydecreasesretinalandchoroidal blood flow anddamages the retinal ganglion cells. But in thisconditiontheeyesbecomepainfulandredalong with cornealoedema.Theconditionisbilateralandaccompanied byheadache,nauseaandvomiting.Vision canbepartially salvagedinboththeseconditionswiththeuseofhighdose steroidsandwithimmediateuseof IOPloweringdrugs.In ourpatient,bloodpressurewasmaintainedthroughoutthe operation and blood loss was also not significantly high. Visual loss waspainless and unilateral. Unfortunatelyour patient had no features of either ION or glaucoma but showedaclearpictureofaCRAOwithnorecoveryofvision. Sometreatmentstrategiescanbeattemptedincasesof CRAO,likeocularmassagetolowerintraocularpressureand improveblood flow in arteries, or todislodge any embo-lus.5% CO2 in oxygencan be inhaled toenhance dilation of arteriesand improve O2 delivery.Intravenous acetazo-lamidemaybegiventoincreaseretinalbloodflow.Allthis attemptmayonlybebeneficialifgivenwithin60---100minof occurrenceofCRAO,otherwisepermanentdamageensues. HayrehandWeingastfoundthatirreversibleretinaldamage followed100minofischaemiawheretheirstudiessurgically occludedthecentralretinalartery.
Conclusion
Reductioninocularbloodflowispossiblebynumerous fac-tors,whichinpresenceofriskfactorcancumulativelylead topostoperativevisualloss.Patientswithpreoperativerisk factors(hypertension,diabetes,smoking,atheroscelorosis, coagulopathy)shouldundergopreoperativeophthalmologic examination.Patientandrelativesshouldalsobeprewarned abouttheunpredictablebutrareriskofperioperativevisual loss.Highriskpatientsshouldbepositionedwiththehead level little higher than the heart when possible. In addi-tionthe head should be maintained in a neutral forward positioni.e.10◦reversetrendelenbergpositioninthe
mid-line, when possible. Perioperative hypotension, anaemia andexcessivehydrationshouldbeavoided.Immediate oph-thalmologic examination should be done for this unusual complication.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.RothS,ThistedRA,EricksonJP,etal.Eyeinjuriesafter non-ocular surgery: a studyof60,965 anaestheticsfrom 1988 to 1992.Anesthesiology.1996;85:1020---7.
438 K.N.Chandra,M.Kundan
3.WilliamsEL,HartWMJr,TempelhoffR.Postoperativeischemic opticneuropathy.AnesthAnalg.1995;80:1018---29.
4.Kumar N, Jivan S, Topping N, et al. Blindness and rectus muscle damage following spinal surgery. Am J Ophthalmol. 2004;138:889---91.
5.PatilCG,LadEM,LadSP,etal.VisualLossafterspinesurgery: apopulationbasedstudy.Spine.2008;33:1491---6.
6.RothS,BarachP.Postoperativevisualloss:stillnoanswersyet. Anesthesiology.2001;95:575---7.
7.Myers MA, HamiltonSR, Bogosian AJ, et al. Visual lossas a complication of spine surgery. A review of37 cases. Spine. 1997;22:1325---9.
8.Stevens WR, Glazer PA, Kelley SD, et al. Ophthalmic complicationsafterspinalsurgery.Spine.1997;12:1319---24. 9.Leibovitch I, Casson R, Laforest C, et al. Ischemic orbital
compartment syndrome as a complication of spinal surgery in the prone position. Ophthalmology. 2000;113: 105---8.
10.OzcanMS,PraetelC,BhattiMT,etal.Theeffectofbody inclina-tionduringpronepositioningonintraocularpressureinawake volunteers:acomparisonoftwooperatingtables.AnesthAnalg. 2004;99:1152---8.
11.JampolLM,GoldbaumM,RosenbergM,etal.Ischemiaofciliary arterialcirculationfromocularcompression.ArchOphthalmol. 1975;93:1311---7.
12.Kumar N, Jivan S, Glenny RW, et al. Blindness and rectus muscle damage following spine surgery. Am J Ophthalmol. 2004;138:889---91.
13.TiceDA.Ischemic opticneuropathyandcardiac surgery.Ann ThoracSurg.1987;44:677.
14.TetzlaffJE,BellJR,KosmorskyG,etal.Ischemicoptic neuropa-thyafterspinalfusion.CanJAnaesth.1998;45:63---6.
15.Marks SC, Jaquers DA,Hirata RM, et al. Blindness following radicalneckdissection.HeadNeck.1990;12:342---5.