REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
Changes
in
retinal
nerve
fiber
layer
thickness
after
spinal
surgery
in
the
prone
position:
a
prospective
study
夽
Baran
Gencer
a,∗,
Murat
Cos
¸ar
b,
Hasan
Ali
Tufan
a,
Selcuk
Kara
a,
Sedat
Arikan
a,
Tarik
Akman
b,
Hasan
Ali
Kiraz
c,
Arzu
Taskiran
Comez
a,
Volkan
Hanci
daDepartmentofOphthalmology,CanakkaleOnsekizMartUniversity,Canakkale,Turkey bDepartmentofNeurosurgery,CanakkaleOnsekizMartUniversity,Canakkale,Turkey
cDepartmentofAnesthesiologyandReanimation,CanakkaleOnsekizMartUniversity,Canakkale,Turkey dDepartmentofAnesthesiologyandReanimation,DokuzEylülUniversity,Izmir,Turkey
Received19August2013;accepted13March2014 Availableonline30April2014
KEYWORDS
Retinalnervefiber layerthickness; Proneposition; Spinalsurgery; Intraocularpressure
Abstract
Backgroundandobjectives: Changesinocularperfusionplayanimportantroleinthe pathogen-esisofischemicopticneuropathy.Ocularperfusionpressureisequaltomeanarterialpressure minusintraocularpressure.Theaimofthisstudywastoevaluatethechangesintheintraocular pressureandtheretinalnervefiberlayerthicknessinpatientsundergoingspinalsurgeryinthe proneposition.
Methods:Thisprospectivestudyincluded30patientsundergoingspinalsurgery.Retinalnerve fiber layerthickness were measured oneday before andafter thesurgery by usingoptical coherencetomography.Intraocularpressurewasmeasuredbytonopensixtimesatdifferent positionandtime-duration:supineposition(baseline);10minafterintubation(Supine1);10 (Prone1),60(Prone2),120(Prone3)minafter proneposition;andjustafterpostoperative supineposition(Supine2).
Results:Ourstudyinvolved10maleand20femalepatientswiththemedianageof57years. Whenpostoperativeretinalnervefiberlayerthicknessmeasurementswerecomparedwith pre-operativevalues,astatisticallysignificantthinningwasobservedininferiorandnasalquadrants (p=0.009andp=0.003,respectively).Weobservedastatisticallysignificantintraocular pres-suredecreaseinSupine1andanincreaseinbothProne2andProne3whencomparedtothe baseline.Meanarterialpressureandocularperfusionpressurewerefoundtobesignificantly lowerinProne1,Prone2andProne3,whencomparedwiththebaseline.
夽
Apartofthisstudywaspresentedatthe46thNationalCongressofTurkishOphthalmologySociety,October2012,Antalya,Turkey.
∗Correspondingauthor.
E-mail:barangencer@gmail.com(B.Gencer).
http://dx.doi.org/10.1016/j.bjane.2014.03.005
Conclusions:Ourstudyhasshownincreaseinintraocularpressureduringspinalsurgeryinprone position.Astatisticallysignificantretinalnervefiberlayerthicknessthinningwasseenininferior andnasalquadrantsonedayafterthespinalsurgery.
©2014SociedadeBrasileiradeAnestesiologia.PublishedbyElsevier EditoraLtda.Allrights reserved.
PALAVRAS-CHAVE
Espessuradacamada defibrasnervosasda retina;
Pronac¸ão;
Cirurgiadacoluna vertebral;
PressãoIntraocular
Alterac¸õesdaespessuradacamadadefibrasnervosasdaretinaapóscirurgiada
colunavertebralempronac¸ão:estudoprospectivo
Resumo
Justificativaeobjetivos: Asalterac¸õesdeperfusãooculardesempenhamumpapelimportante napatogênesedaneuropatiaópticaisquêmica.Apressãodeperfusãoocularéigualàpressão arterialmédiamenosapressãointraocular.Oobjetivodesteestudofoiavaliarasalterac¸ões dapressãointraocularedaespessuradacamadadefibras nervosasdaretinaempacientes submetidosàcirurgiadacolunavertebralempronac¸ão.
Métodos: Esteestudoprospectivoincluiu 30pacientessubmetidos àcirurgia dacoluna ver-tebral. A espessurada camadade fibras nervosasdaretina foi medida um dia antese um depoisdacirurgia, como usodatomografia de coerência óptica.A pressão intraocularfoi medidaseisvezescomoTonopeneotempodedurac¸ãoemposic¸õesdiferentes:emsupinac¸ão (basal),10minutosapósaintubac¸ão(Supinac¸ão1);apósapronac¸ãoaos10minutos(Pronac¸ão 1),60minutos(Pronac¸ão2) e120minutos (Pronac¸ão3) e logoapósasupinac¸ão noperíodo pós-operatório(Supinac¸ão2).
Resultados: Nossoestudoenvolveu10pacientesdosexomasculinoe20dofeminino,commédia de57anos.Nopós-operatório,quandoasmedidasdaespessuradacamadadefibrasnervosas daretinaforamcomparadascomosvaloresdopré-operatório,umafinamentoestatisticamente significativodaretinafoiobservadonosquadrantesnasaiseinferiores(p=0,009ep=0,003, respectivamente).Observamos uma diminuic¸ãoda pressãointraocularestatisticamente sig-nificanteemSupinac¸ão1eumaumentoem ambosmomentosPronac¸ão2ePronac¸ão3, em comparac¸ãocomosvaloresbasais.A pressãoarterialmédiae apressãodeperfusão ocular foramsignificativamentemaisbaixasemPronac¸ão1,Pronac¸ão2ePronac¸ão3,emcomparac¸ão comosvaloresbasais.
Conclusões:Nossoestudomostrouaumentodapressãointraocularduranteacirurgiadacoluna vertebralempronac¸ão.Umafinamentoestatisticamentesignificantedaespessuradacamada defibras nervosasdaretinafoiobservadonosquadrantes nasaiseinferioresum diaapósa cirurgiadacolunavertebral.
©2014SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Postoperativevisionloss(POVL)isararebutserious compli-cationthatmaydevelopafternon-ocularsurgeries.1---3POVL
mostcommonlyoccursafterspinalsurgery.Theetiologyof POVLhasbeenidentifiedasposteriorischemicoptic neurop-athy(PION),anteriorischemicopticneuropathy(AION)and central arterial occlusion, respectively.4---6 A multi-center
studydemonstratedthatmalegender,obesity,useofWilson frame,long durationof anesthesia, excess blood lossand low ratio of colloids administration are the independent riskfactorsforperoperative IONdevelopmentafterspinal surgery.7Changesinocularperfusionplayanimportantrole
inthe pathogenesisof ischemicopticneuropathy.8 Ocular
perfusion pressure (OPP) is calculated by the subtraction of intraocular pressure (IOP) from meanarterial pressure
(MAP).8 Several studies have demonstrated that spinal
surgery in the pronepositioncauses an IOP elevation.9---13
Ithasbeen speculatedthatasaresultofIOP elevationin the prone position, OPP reduces (in patients where MAP remainsstableorreduces)andmayleadtoAION.9,10,12
Although IOP changes during spinal surgery in prone position have been well demonstrated, there is no study evaluatingtheeffectofthesechangesontheopticnerve. Retinalnervefiberlayerthickness(RNFLT)is animportant objectivemarkerforearlyperiodchangesduetoopticnerve damage,whichinturniscausedbyischemicoptic neurop-athyandsuddenincreaseinIOP.14---18
Materials
and
methods
The study wasperformed with informedpatient consent, and conducted under a protocol approved by the local Ethics Committee of C¸anakkale Onsekiz Mart University (26.04.2012,050-99-79)andinaccordancewiththeethical standardsstatedinthe1964DeclarationofHelsinki. Partici-pantsforthestudywereenrolledfromconsecutivepatients whounderwentspinalsurgerybetweenMayandNovember 2012,andwhosephysicalstateswereI-IIIinaccordancewith AmericanSocietyofAnesthesiologists(ASA).
One day before the surgery, the patients underwent a full ophthalmic examination including visual acuity, slit-lampexam,IOPmeasurementusingGoldmannapplanation tonometryandfundusexamination.Patientsunder18year andpatientswithsphericalvalues±5dioptryand/or cylin-dricalvalues±3dioptryrefractoryerror,glaucoma,uveitis, historyofeyesurgery,opticnerveanomaly,historyofallergy totopicalanesthesia, ormeasurement qualitybelow5/10 onopticcoherencetomography(OCT)wereexcluded.
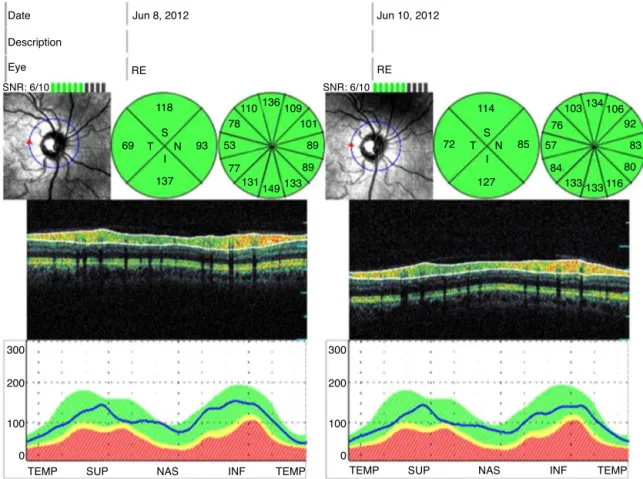
TheRNFLTweremeasuredonedaybeforeandafterthe surgeryby usingOTI SpectralOCT/SLO(Ophthalmic Tech-nologies Inc.(OTI), Toronto, Ontario,Canada). OCT scans were made after placing a 3.4mm diametercircular ring aroundtheopticnerveheadonimageoftheconfocal scan-ninglaserophthalmoscopy.Thepatients’RNFLTmapswere evaluatedtogetherwithnormativeRNFLTratios.The aver-ageRNFLTmeasurementsfortemporal,superior,nasaland inferiorquadrantswerecollected(Fig.1).
No premedication was given before anesthesia. Anes-thesia was induced with2g/kg fentanyl, and 2.5mg/kg propofol.Trachealintubationwasfacilitatedwith0.6mg/kg rocuronium, and the lungs were mechanically ventilated at 0.5 FiO2. Anesthesia wasmaintained withsevoflurane,
and remifentanyl 0.15---0.2g/kg/min. Additional rocuro-niumwasadministeredasrequired.Aftertopicalanesthesia (right eye0.5% proparacaine hydrochloride,0.5% Alcaine, Alcon) IOP measurements were taken for six times with Tono-PenAVIAapplanationtonometer(ReichertInc.,Depew, NY):beforepremedicationinthesupineposition(baseline); 10minafterintubation(Supine1);10min(Prone1),60min (Prone 2), 120min (Prone 3) after being turned to prone positionand10minafterthepatientwasturnedtosupine position(Supine 2).Prone position cushionswere used to stabilizethepatients’headsinproneposition.
Systolic blood pressure (SBP), diastolic blood pressure (DBP),MAP,heart rate(HR),end-tidalcarbondioxide (ET-CO2) and oxygen saturation (SatO2) were also recorded
simultaneouslywithIOPmeasurements.OPPwascalculated using the MAP-IOP formula. The anesthesia, prone posi-tionandsurgerydurationswerealsonoted.Theamountof bloodandliquidsgiventothepatientwasmeasuredagainst bloodlossandurineoutputduringtheoperationtocalculate liquidbalance[liquidbalance=(givenblood+fluids)−(lost blood+urine)].Preoperativeandpostoperativehemoglobin (Hb)andhemocrit(Htc)levelswererecorded.Inthe recov-eryroom, thepatients were asked whetherthey hadany visionlossordiscomfortintheireyes.
Date
Description
Eye
SNR: 6/10
RE
Jun 8, 2012 Jun 10, 2012
RE
SNR: 6/10
114 103134106
92
83
80 116 133 133 84 57
76 110
118
93
137 69 T
I S
N
136 109
101
89
89 133 149 131 77 53
78
S N 85 72 T
I
127
300
200
100
0
300
200
100
0
TEMP SUP NAS INF TEMP TEMP SUP NAS INF TEMP
Poweranalysis
Themain focusof ourstudy wastodetermine postopera-tiveRNFLT. The samplingsizewasdetermined followinga studybyHongetal.,19whereinferiorquadrantRNFLT
aver-agewasreportedas139.9±11.8m.Thepatientnumber requiredtodetermineanaveragereductionininferior quad-rantRNFLT(with5%ofnormalvalues,0.05˛errorand80% power) wascalculatedas 30.The sample sizewas deter-minedbyapowercalculator.
Statisticalanalyses
Statistical analyses were performed using the Statisti-cal Package for Social Sciences (SPSS), version 15.0, for Windows (SPSS, Chicago, IL). The Shapiro---Wilk normal-ity test was used to examine the compatibility between the measured variables and the normal distribution. The Wilcoxon test was used to compare pre- and postop-erative RNFLT measurements. During the operation the changes in IOP and hemodynamic parameters measured at six different times were later evaluated using the Friedmantest.Pairwisecomparisonswereperformedusing the Wilcoxon and Mann---Whitney U test. The relationship between RNFLT changes and parameters showing signifi-cant changes during the operation were examined using the Spearman correlation test. The data were shown as median(minimum---maximum),andthelevelofsignificance wasacceptedasp<0.05.
Results
Atotalof32patientsunderwentspinalsurgeriesbetween May and November 2012. Among them, 30 patients were included in our study, while two patients were excluded due to tilted disk. There were 10 male and 20 female patients, with an average age of 54.9±13.4 years. The patientcharacteristicsandpropertiesrelatingtothe oper-ationaresummarizedinTable1.
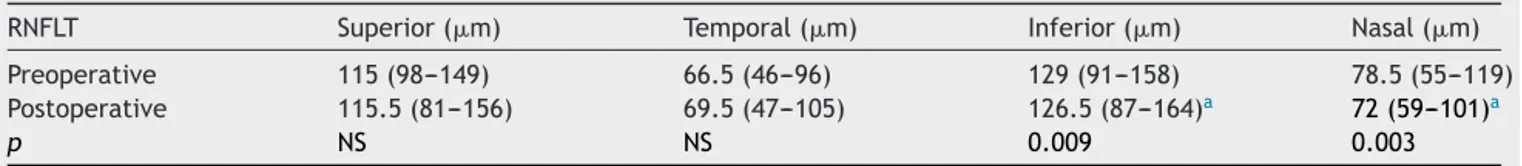
Preoperative and postoperative median values of superior,temporal,inferiorandnasalquadrantRNFLT mea-surements are given in Table 2. There was no significant differencebetween postoperative and preoperative mea-surementsfor superior and temporalquadrants(p>0.05). However,astatisticallysignificantthinningwasobservedin inferior(p=0.009)andnasalquadrants(p=0.003)(Table2). The patients’IOPand hemodynamicmeasurementsare summarized in Table 3. When compared to the base-line, a reductionin IOP wasseen at Supine1 (p<0.001).
Table1 Patientvariables.
Variable Data
Age(years) 57(28---80)
Gender(male/female) 10/20
BMI(kg/m2) 28.3(18.7---45)
Anesthesiatime(min) 140(82---260) Pronetime(min) 130(70---255) Operationtime(min) 120(60---242) Bloodloss(mL) 350(100---1200) Colloidinfusion(mL) 400(0---1200)
Variablesareshownasthemedian(range). BMI,Bodymassindex;min,minutes;mL,mililitres
AstatisticallysignificantIOPelevationwasobservedinProne 2(p<0.001)andProne3(p=0.01)whencomparedto base-linevalues.HemodynamicchangesshowedthatSBP,DBPand MAPweresignificantlyloweratProne1(p=0.02,p=0.03, p=0.01),Prone 2(p<0.001 forall) andProne3 (p=0.001 for all) when compared to baseline. Average OPP values weresignificantlylowerthanbaselineatProne1(p=0.01), Prone 2 (p<0.001) and Prone 3 (p=0.004). Heart rates were significantly lowerat Prone 2 (p=0.01)and Prone 3 (p=0.01) when compared tobaseline. At all times, SpO2 values were significantly higher when compared to base-line (Supine 1and Prone 2;p<0.001, Prone 1and Supine 2;p=0.001, Prone3;p=0.005).Calculated liquidbalance forallpatientswaspositive,andaveragevalueswere1325 (550---3000)mL.PreoperativeandpostoperativeaverageHb valueswere13.2(11---16.3)g/dLand11.1(8.1---14.1)g/dL, respectively; while Htcvalueswere 39.3(33.8---48.7)g/dL and 34.2 (25---43.1)g/dL. The reductions in postoperative HbandHtcvalueswerestatisticallysignificant(p<0.001for both).
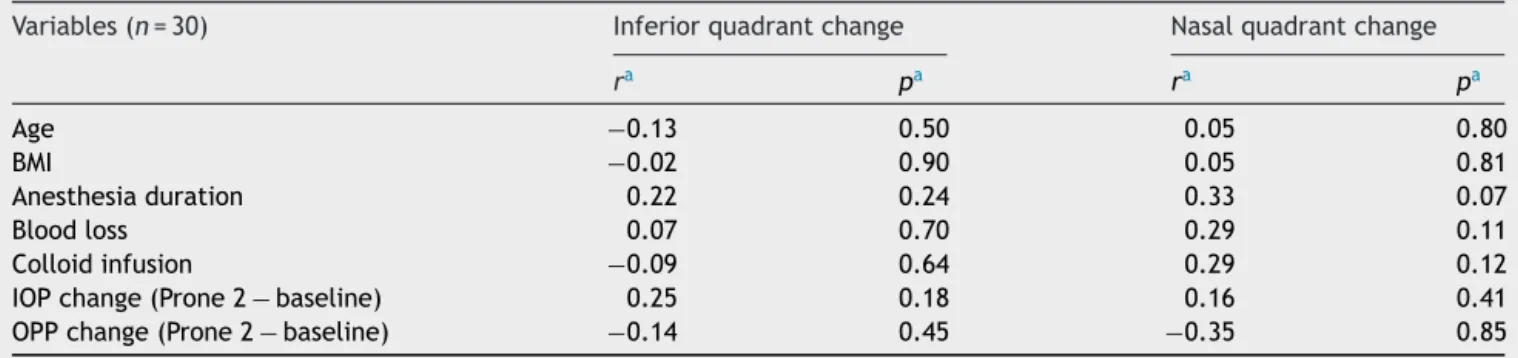
Nosignificantcorrelationwasfoundbetweentheamount of RNFLTthinningandpatients age,BMI,anesthesia dura-tion,bloodloss,andadministeredcolloidamount,changes ofIOPandOPPduringtheoperation(p>0.05)(Table4).
Discussion
ThisprospectivestudyaimedtoexaminechangesinRNFLT andfactorsaffectingthosechangesinpatientswho under-went spinal surgery in the prone position. When we evaluatedthe changes in RNFLTmeasured bySD-OCT, we observed a thinning in the inferior and nasal quadrants on the first postoperative day compared to preoperative
Table2 Preoperativeandpostoperativemeasurementsofretinalnervefiberlayerthicknessatfourquadrants.
RNFLT Superior(m) Temporal(m) Inferior(m) Nasal(m)
Preoperative 115(98---149) 66.5(46---96) 129(91---158) 78.5(55---119) Postoperative 115.5(81---156) 69.5(47---105) 126.5(87---164)a 72(59---101)a
p NS NS 0.009 0.003
Variablesareshownasthemedian(range).
RNFLT,retinalnervefiberlayerthickness;m,micrometer;NS,nonsignificant.
Table3 Intraocularpressure,bloodpressure(systolic,diastolic,mean),ocularperfusionpressureandheartratemeasurements duringoperation.
IOP(mmHg) SBP(mmHg) DBP(mmHg) MAP(mmHg) OPP(mmHg) HR(beats/min)
Baseline(n=30) 15(7---20) 130(91---202) 77(60---111) 95(69---149) 79.5(53---134) 75(55---100) Supine1(n=30) 10(5---24)a 120(86---190) 75(54---112) 86(63---133) 75.5(47---119) 78.5(55---100)
Prone1(n=30) 14.5(6---31) 117(78---156)a 76(44---99)a 92(54---122)a 71(38---109)a 76(57---109)
Prone2(n=30) 19(10---37)a 107.5(81---148)a 71(53---94)a 82(68---104)a 62.5(35---92)a 69.5(54---93)a
Prone3(n=18) 15(11---35)a 109(90---132)a 70(58---85)a 81.5(72---105)a 64(46---90)a 69(62---98)a
Supine2(n=30) 15.5(9---32) 128(81---170) 77.5(62---99) 98(70---127) 80(46---115) 78.5(55---99)
Variablesareshownasthemedian(range).
IOP,intraocularpressure;SBP,systolicbloodpressure;DBP,diastolicbloodpressure;MAP,meanarterialpressure;OPP,ocularperfusion pressure;HR,heartrate.
a p<0.05,comparedwithbaselinevalue,Wilcoxonsignedrankstest.
measurements.WeobservedasignificantincreaseinIOPin thepronepositionwhiletherewasasignificantdecreasein hemodynamicfactors.However,wedidnotfindany corre-lationbetween the changingof all parametersduring the operationandtheRNFLTthinning.
POVL,occurringafterspinalsurgeryintheproneposition is a serious complicationwhich has been linked,in order ofdecreasingfrequency,toposteriorION,anteriorIONand central artery occlusion, but its etiology is still not well understood.1---3,6IthasbeenproposedthatIOPelevationin
the pronepositionreduces ocular perfusion, especiallyin caseswhoseMAP remainsstable,therebycausing anterior IONorcentralretinalarterialocclusion.12
ThefirststudyinvestigatingIOPchangesinspinalsurgery in the prone position was carried out by Cheng et al.10
Theyobservedasignificant IOPelevationat thebeginning (27±2mmHg) andat the end (40±2mmHg) of the oper-ation in theprone positionwhen compared withbaseline values(19±1mmHg)measuredinthesupineposition. How-ever, theydidnot investigateintraoperative IOP changes. Inanotherstudyevaluatingpatientswhounderwentspinal surgery, it was found that the average IOP values in the supinepositionafteranesthesiainductionwere11.5mmHg, while in the prone position at the beginning and at the endofsurgeryIOPvalueswere23.5mmHgand30.5mmHg, respectively.10 Theydeterminedthatintheproneposition,
these values were significantly higher than in the supine
position. In various studies using healthy volunteers, IOP valuesinthepronepositionwerefoundtobesignificantly higherthaninthesittingposition.20,21
Tothebestofourknowledge,thisstudyisthemost com-prehensivestudytilldate investigatingIOPchangesinthe proneposition.IOPwasmeasured inthepronepositionat the10th,60thand 120thminutesof operation.We found that IOP was highest at the 60th minute, and it reduced slightly at the 120th minute, which wasstill significantly higherthanbaselinevalues.WhileourstudyonIOPchanges duringtheoperationhasavariationcurvesimilartoother studies, any differences may be linked toerroneous high measurementsduetoexcessiveeyelidopeningorpressure ontheglobe.
Spectral domain OCT provides reliable and repeatable measuresofthenervefiberlayeroftheopticnerveatthe levelof7---15m.22Thesepropertieshaveledittobecoming themostimportantdiagnostictoolforearly diagnosisand follow-upfordisordersinvolvingthefrontpartofthevisual pathway.23Inapreviousstudy,interoperator(intraclass
cor-relationcoefficient(ICC),0.87;CV,2.89%)andintraoperator (ICC,0.94and0.95;CV,1.28%and1.26%,respectively,for operatorAandoperatorB)agreementhavebeenfoundfor averageRNFLTmeasurementsusingOTISpectralOCT/SLO.24
ThisstudyisthefirstintheliteraturetoevaluateRNFLT changes following spinal surgery in the prone position. On the first postoperative day, a significant thinning was
Table4 The correlations between inferiorand nasal quadrants’ retinal nerve fiber layer thickness changes and patients variables.
Variables(n=30) Inferiorquadrantchange Nasalquadrantchange
ra pa ra pa
Age −0.13 0.50 0.05 0.80
BMI −0.02 0.90 0.05 0.81
Anesthesiaduration 0.22 0.24 0.33 0.07
Bloodloss 0.07 0.70 0.29 0.11
Colloidinfusion −0.09 0.64 0.29 0.12
IOPchange(Prone2−baseline) 0.25 0.18 0.16 0.41
OPPchange(Prone2−baseline) −0.14 0.45 −0.35 0.85
a Spearman’srankcorrelation.
observedin the inferiorand nasalquadrants.While there wasa significant rise in IOP in the prone position, there wasa significant decrease in hemodynamic factors. How-ever,nosignificantcorrelationwasfoundbetweenpatients’ age,BMI,anesthesiaduration,bloodlossorgivencolloids, IOPorOPPchangesandthinninginRNFL.Similarly,Fortune etal.16showedthatacuteIOPincreasecausedRNFLthinning
in rat eyes, and this thinning returned to normal values afteramonth.Pietteetal.14 foundthatacuteIOPincrease
causedbysuctioninLASIKpatients,whichresultedina sta-tisticallysignificant thinning ofRNFLT, andeven afterIOP valuesreturnedtonormalthisthinningremained.Inanother study,allGDxparametersexceptforsymmetryshowed sta-tisticallysignificantreductiononthefirstpostoperativeday in patients who underwent coronary artery bypass oper-ation. By the 5th postoperative day, superior/nasal ratio parameters returned to normal values, however, by the firstpostoperativemonththeinferiorratiovalueswerestill undernormalvalues.25Thisstudysupportsourresults
show-ingthattheinferiorquadrantretinalnervefibersaremore sensitive.
Althoughthenumberofpatientsinourstudyis compa-rable to similar studies, low patient number is the most important limitation. Another limitation was the lack of long-term follow-ups.The progress of RNFLTchanges was notevaluatedinthisstudy.
Inconclusion,spinalsurgicalinterventionsintheprone positionleadasignificantinferiorandnasalquadrants thin-ninginRNFLattheearlypostoperativeperiodeventhough patientsdonot sufferfromvision loss. Buttherewasnot found any significant correlation between the amount of RNFLTthinningandchangesofIOP duringtheoperationin thisstudy.Largercontrolled studieswithlongerfollow-up willberequiredtofullydeterminetheroleofproneposition onRNFLTchanges.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.PatilCG,LadEM,LadSP,etal.Visuallossafterspinesurgery: apopulation-basedstudy.Spine.2008;33:1491---6.
2.Stevens WR, Glazer PA, Kelley SD, et al. Ophthalmic complicationsafterspinalsurgery.Spine.1997;22:1319---24.
3.Chang SH, Miller NR. The incidence of vision loss due to perioperative ischemic optic neuropathy associated with spinesurgery: theJohnsHopkinsHospitalExperience. Spine. 2005;30:1299---302.
4.AlexandrakisG,LamBL.Bilateralposteriorischemicoptic neu-ropathyafterspinalsurgery.AmJOphthalmol.1999;127:354---5.
5.Ho VT, Newman NJ, Song S, et al. Ischemic optic neurop-athyfollowingspinesurgery.JNeurosurgAnesthesiol.2005;17: 38---44.
6.LeeLA,RothS,PosnerKL,etal.TheAmericanSocietyof Anes-thesiologistsPostoperativeVisualLossRegistry:analysisof93
spinesurgerycaseswithpostoperativevisualloss. Anesthesiol-ogy.2006;105:652---9.
7.ThePostoperativeVisualLossStudyGroup.Riskfactors associ-atedwithischemicopticneuropathyafterspinalfusionsurgery. Anesthesiology.2012;116:15---24.
8.Hayreh SS. Ischemic optic neuropathy. Prog Retin Eye Res. 2009;28:34---62.
9.OzcanMS,PraetelC,BhattiMT,etal.Theeffectofbody inclina-tionduringpronepositioningonintraocularpressureinawake volunteers:acomparisonoftwooperatingtables.AnesthAnalg. 2004;99:1152---8.
10.ChengMA,TodorovA,TempelhoffR,etal.Theeffectofprone positioning on intraocularpressure in anesthetized patients. Anesthesiology.2001;95:1351---5.
11.HuntK,BajekalR,CalderI,etal.Changesinintraocular pres-sureinanesthetizedpronepatients.JNeurosurgAnesthesiol. 2004;16:287---90.
12.RothS.Perioperativevisualloss:whatdoweknow,whatcan wedo?BrJAnaesth.2009;103:31---40.
13.SugataA,HayashiH,KawaguchiM,etal.Changesinintraocular pressureduringpronespinesurgeryunderpropofoland sevoflu-raneanesthesia.JNeurosurgAnesthesiol.2012;24:152---6.
14.PietteS,LiebmannJM,IshikawaH,etal.Acuteconformational changesintheopticnerveheadwithrapidintraocularpressure elevation:implicationsfor LASIKsurgery.OphthalSurgLasers Imaging.2003;34:334---41.
15.FortuneB,YangH,StrouthidisNG,etal.Theeffectofacute intraocular pressure elevationon peripapillary retinal thick-ness,retinalnervefiberlayerthickness,andretardance.Invest OphthalmolVisSci.2009;50:4719---26.
16.Fortune B, Choe TE, Reynaud J, et al. Deformation of the rodentoptic nerve head and peripapillary structures during acuteintraocularpressureelevation.InvestOphthalmolVisSci. 2011;52:6651---61.
17.ContrerasI,RebolledaG,NovalS,etal.Opticdiscevaluationby opticalcoherencetomographyinnonarteriticanteriorischemic opticneuropathy.InvestOphthalmolVisSci.2007;48:4087---92.
18.HoffJM,VarhaugP,MidelfartA, etal.Acutevisuallossafter spinalsurgery.ActaOphthalmol.2010;88:490---2.
19.HongJT,SungKR,ChoJW,etal.Retinalnervefiberlayer mea-surement variability withspectral domain opticalcoherence tomography.KoreanJOphthalmol.2012;26:32---8.
20.LamAK,DouthwaiteWA.Doesthechangeofanteriorchamber depth or/and episcleral venous pressure cause intraocu-lar pressure change in postural variation? Optom Vis Sci. 1997;74:664---7.
21.WalickKS,KraghJrJE,WardJA,etal.Changesinintraocular pressureduetosurgicalpositioning:studyingpotentialriskfor postoperativevisionloss.Spine.2007;32:2591---5.
22.ArefAA,BudenzDL.Spectraldomainopticalcoherence tomo-graphyinthediagnosisandmanagementofglaucoma.Ophthal SurgLasersImaging.2010;41:15---27.
23.Savini G, Carbonelli M, Barboni P. Spectral-domain optical coherencetomographyforthediagnosisandfollow-upof glau-coma.CurrOpinOphthalmol.2011;22:115---23.
24.Pierro L, Gagliardi M, Iuliano L, et al. Retinal nerve fiber layerthicknessreproducibilityusingsevendifferentOCT instru-ments.InvestOphthalmolVisSci.2012;53:5912---20.