REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
A
prospective,
randomized,
blinded-endpoint,
controlled
study
---
continuous
epidural
infusion
versus
programmed
intermittent
epidural
bolus
in
labor
analgesia
Joana
Nunes
∗,
Sara
Nunes,
Mariano
Veiga,
Mara
Cortez,
Isabel
Seifert
DepartamentodeAnestesiologia,HospitalCentraldoFunchal,Funchal,Portugal
Received15June2014;accepted11December2014 Availableonline19November2015
KEYWORDS Analgesia; Epidural;
Epiduralanalgesic techniques; Infusion;
Obstetricanalgesia; Programmed intermittentbolus
Abstract
Background: Thereisevidencethatadministrationofaprogrammedintermittentepiduralbolus (PIEB)comparedtocontinuousepiduralinfusion(CEI)leadstogreateranalgesiaefficacyand maternalsatisfactionwithdecreasedanestheticinterventions.
Methods:Inthisstudy,166womenwithviablepregnancieswereincluded.Afteranepidural loadingdoseof10mLwithRopivacaine0.16%plusSufentanil10g,parturientwererandomly
assignedtooneofthreeregimens:A---Ropivacaine0.15%plusSufentanil0.2g/mLsolution
as continuousepidural infusion(5mL/h, beginningimmediatelyafter theinitial bolus);B ---Ropivacaine0.1%plusSufentanil0.2g/mLasprogrammedintermittentepiduralbolusandC
--- SamesolutionasgroupAasprogrammedintermittentepiduralbolus.PIEBregimenswere programmedas10mL/hstarting60minaftertheinitialbolus.Rescuebolusesof5mLofthe samesolutionwereadministered,withtheinfusionpump.Weevaluatedmaternalsatisfaction usingaverbalnumericscalefrom0to10.Wealsoevaluatedadverse,maternalandneonatal outcomes.
Results:Weanalyzed130pregnants(A=60;B=33;C=37).Themedianverbalnumericscale formaternalsatisfactionwas8.8ingroupA;8.6ingroupBand8.6ingroupC(p=0.83).We found ahighercaesareandeliveryrateingroupA(56.7%;p=0.02).Nodifferencesinmotor block,instrumentaldeliveryrateandneonataloutcomeswereobserved.
Conclusions: Maintenanceofepiduralanalgesiawithprogrammedintermittentepiduralbolus isassociatedwithareducedincidenceofcaesareandeliverywithequallyhighmaternal satis-factionandnoadverseoutcomes.
©2015SociedadeBrasileiradeAnestesiologia.Publishedby ElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
∗Correspondingauthor.
E-mail:joanacnunes@hotmail.com(J.Nunes). http://dx.doi.org/10.1016/j.bjane.2014.12.006
PALAVRAS-CHAVE Analgesia;
Epidural;
Técnicasdeanalgesia epidural;
Infusão;
Analgesiaobstétrica;
Bolusintermitente
programado
Estudoprospectivo,randômico,controladoedeavaliac¸ãocegadodesfecho---infusão periduralcontínuaversusbolusepiduralintermitenteprogramadoemanalgesia
departo
Resumo
Justificativa:Háevidênciasdequeaadministrac¸ãodeumbolusepiduralintermitente progra-mado(BEIP)comparadaàinfusãoepiduralcontínua(IEC)resultaemmaioreficáciadaanalgesia edasatisfac¸ãomaterna,comreduc¸ãodasintervenc¸õesanestésicas.
Métodos: Nesteestudo,166mulherescomgravidezesviáveisforamincluídas.Apósumadose epiduralde10mLdeRopivacaínaa0,16%eadic¸ãode10gdeSufentanil,asparturientesforam
aleatoriamentedesignadasparaumdostrêsregimes:A-ropivacaínaa0,15%maissoluc¸ãode sufentanil(0,2g/mL)comoinfusãoperiduralcontínua(5mL/h,comec¸andoimediatamente
apósobolusinicial);B-ropivacaínaa0,1%maissufentanil(0,2g/mL)comobolusepidural
intermitenteprogramado;C-soluc¸ãoidênticaàdoGrupoAcombolusepiduralintermitente programado.OsregimesBEIPforamprogramadoscomo10mLporhora,iniciando60minutos apósobolus inicial.Bolus deresgatede 5mLdamesmasoluc¸ãoforamadministradoscom bombadeinfusão.Asatisfac¸ãomaternafoiavaliadautilizandoumaescalanuméricaverbalde 0a10.Tambémavaliamososresultadosadversosmaternaiseneonatais.
Resultados: Foramavaliadas 30gestantes(A=60,B=33;C=37)foramavaliados.A mediana naescalanuméricaverbalparaasatisfac¸ãomaternafoide8,8nogrupoA;8,6nogrupoBe 8,6nogrupoC(p=0,83).EncontramosumataxamaiselevadaparapartocesárionogrupoA (56,7%;p=0,02).Nãoobservamosdiferenc¸asnobloqueiomotor,taxadepartoinstrumentale resultadosneonatais.
Conclusões:A manutenc¸ão da analgesia peridural combolus epidural intermitente progra-madoestáassociadaaumareduc¸ãodaincidênciadepartocesarianocomsatisfac¸ãomaterna igualmenteelevadaesemresultadosadversos.
©2015SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigoOpen Accesssobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Childbirth is one of the most painful experiences for woman.1 The degree of painexperienced and the quality
ofpainreliefaffectpatient’ssatisfactionwiththebirthing process,animportantoutcomeofthequalityofcare, con-tributingtolong-termemotionalandpsychologicaleffects.2
Neuraxialanalgesictechniquesoutdidparenteral, inhala-tory andnon-pharmacologicmeasures in laboranalgesia.3
Maintenance technique for epidural labor analgesia has changedfromintermittentmanualbolus---withanincreased riskforcontamination,drugerrorandwidervariationinpain relief4---tocontinuousepiduralinfusion(CEI)withorwithout
patientcontrolledepiduralanalgesia(PCEA).Thelater pro-videsasmootheranalgesicexperiencebutlocalanesthetic consumptionisusuallyhigherandmotorblockmaybemore prominent,5withalikelyincreaseinrates ofdystociaand
instrumentaldeliveries.6
There is evidence that administration of an epidural bolus leads to greater analgesia efficacy7---9 and maternal
satisfactionwithreducedlocalanestheticconsumptionand anestheticinterventions.4,5,10---12Howevernostudy,todate,
hasincluded all women withviable pregnanciesand pro-grammedintermittentepiduralbolus(PIEB)regimentsdiffer significantlyamongstudies.
We hypothesized that, even at lower local anesthetic concentrations,PIEBisassociatedwithsimilarorhigher out-comescomparingtoCEI.Theprimaryoutcomeofthisstudy
is to compare maternal satisfaction, with PIEB at differ-entlocalanestheticconcentrations,tostandardCEIinlabor analgesia.
Methods
We conducted a prospective, randomized, blinded-endpoint, controlledstudy between April and June 2013, approvedbytheClinicalResearchandEthicsCommitteeof Funchal’sCentralHospital.
Women with viable pregnancies who requested labor analgesia,withacervicaldilation>3cmand<5cmandwith abaselinepainscore(assessedatthepeakofthe contrac-tion) from5 to10 in verbal numericscale (VNS)of pain, wereincluded.Writteninformedconsentwasobtainedfrom allsubjectsortheparentsorlegalguardians,forminor sub-jects.Womenwhohadreceivedparenteralopioids,whodid not speakthe languageor were unabletoperform motor blockevaluationtests,wereexcludedfromthestudy.
Assessed for eligibility (n=203) pregnant women who received epidural labor analgesia
Enrolment
Allocation
Follow-up
Analysis
Randomized (n=166)
Even age
Excluded (n=13)*
Allocated to group A (CEI 0,15%) (n=78) Allocated to group B (PIEB 0,1%) (n=41)
Received allocated intervention (n=75) Received allocated intervention (n=40)
Did not received allocated intervention (n=3)
Did not received allocated intervention (n=1)
Allocated to group C (PIEB 0,15%) (n=47)
Received allocated intervention (n=47)
Did not received allocated intervention (n=0)
Discontinued intervention (n=0)
Excluded (n=5)*
Discontinued intervention (n=0)
Excluded (n=7)*
Discontinued intervention (n=0)
Analysed (n=60)
Excluded from analysis (n=2) because maternal satisfaction was missing.
Analysed (n=33)
Excluded from analysis (n=2) because maternal satisfaction was missing.
Analysed (n=37)
Excluded from analysis (n=2) because maternal satisfaction was missing. Odd age
Last number of clinical file between 0-4
Odd age
Last number of clinical file between 5-9 Not meeting inclusion criteria (n=38)
Declined to participate (n=0)
Figure1 CONSORT2010Flowdiagram.CEI,continuousepiduralinfusion;PIEB,programmedintermittentepiduralbolus;*maternal satisfactionscoremissing.
andsecured.Withnotestdose,allparturientsreceivedan initialepiduralfractionedloadingdoseof10mLwith0.16% Ropivacaineplus Sufentanil 10g.If VNSscore was>3 or
ifwomenrequestedanadditionalepiduralbolus,lessthan 30minaftertheepiduralloadingdose,wereexcludedfrom thestudyandsubsequentstatisticalanalysis,ponderingthat theyhadafailedblock.
Parturientwererandomizedtoreceiveoneofthethree followingregimensforthemaintenanceofanalgesia accord-ingtoFig.1.
Forthepurposeofthisworkweusedthesameinfusion pump programmedtodeliverCEIorPIEB accordingtothe protocolofthestudy.Allpump’sinfusiontubingwere con-nectedtothepatient’sepiduralcatheteraftertheloading dose.
The pumpforCEI,groupA,wasprogrammedtodeliver theRopivacaine0.15%plusSufentanil0.2g/mLsolutionat
arateof5mL/h,withPCEAbolusesof5mLwithalockout intervalof20min,andaperhourmaximumvolumeof15mL. Patientswereinstructed,beforeor immediatelyafter the epiduralcatheterplacement,onhowtousethePCEApump andtopushthebuttonwhenevertheyfeltpainful.
The PIEB pump in group Bwasprogrammed to deliver 10mL of0.1%Ropivacaine plusSufentanil0.2g/mL
solu-tioneveryhourbeginning60minaftertheadministrationof theinitialepiduralloadingdose.ThePIEBpumpingroupC, wasprogrammedtodeliver10mLofRopivacaine0.15%plus Sufentanil0.2g/mLsolutioneveryhour beginning60min
aftertheadministrationoftheinitialepiduralloadingdose.
Patientsin the PIEB groups were instructed, to push the nursingbuttonwhenevertheyfeltpainfulandthe anesthe-siologistwascalled toadministeranadditionalbolus with theinfusionpump.
The epiduralanalgesia wascontinuedthroughthe sec-ondstageoflaboruntildeliveryofthefetus.Theadditional bolusinallgroupswasdefinedas5mLofthesolution.
Data noted for each subject included demographic characteristics,co-morbidities, pregnancyandlabordata, adverseeffects,maternalsatisfaction,motorblock evalua-tion,modeofdeliveryandApgarscore.
VNS score for pain and motor function was evaluated everyhourbeginning30minaftertheepiduralloadingdose. The degree of motor block was evaluated in both lower extremitiesusingthe Bromagescore.13 The endpoint was
anydegreeofmotorblockinoneorbothlowerextremities atanytime,duringlabor.
Maternal satisfaction was assessed after labor using a verbalnumericscalefrom0(notsatisfiedatall)to10 (com-pletely satisfied). A blinded nurse assessed this endpoint afterthedelivery.
Usingdatafrompreviousstudies14,15 wecalculatedthat
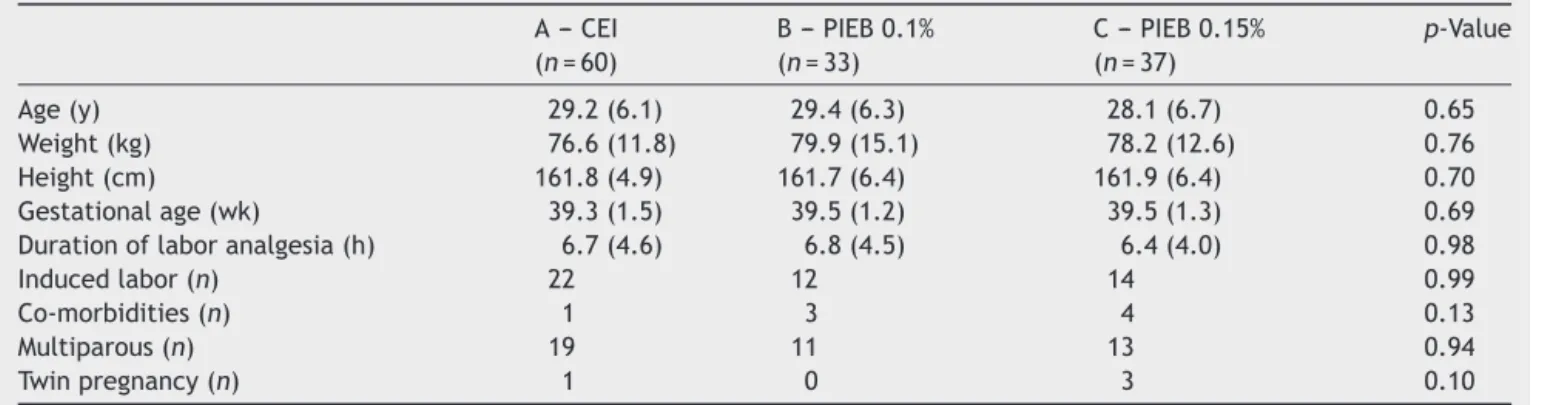
Table1 Subjectandlaborcharacteristicspresentedasmean(SD)ornumber(n).
A---CEI B---PIEB0.1% C---PIEB0.15% p-Value (n=60) (n=33) (n=37)
Age(y) 29.2(6.1) 29.4(6.3) 28.1(6.7) 0.65
Weight(kg) 76.6(11.8) 79.9(15.1) 78.2(12.6) 0.76 Height(cm) 161.8(4.9) 161.7(6.4) 161.9(6.4) 0.70 Gestationalage(wk) 39.3(1.5) 39.5(1.2) 39.5(1.3) 0.69 Durationoflaboranalgesia(h) 6.7(4.6) 6.8(4.5) 6.4(4.0) 0.98
Inducedlabor(n) 22 12 14 0.99
Co-morbidities(n) 1 3 4 0.13
Multiparous(n) 19 11 13 0.94
Twinpregnancy(n) 1 0 3 0.10
CEI,continuousepiduralinfusion;PIEB,programmedintermittentepiduralbolus.
were compared between groups with the Kruskal---Wallis test.Ap-value<0.05wasconsideredstatisticallysignificant.
Results
Onehundredsixty-fivesubjectsrecruitedwererandomized togroupA(CEI0.15%),groupB(PIEB0.1%)orgroupC(PIEB 0.15%).Afterallocationandfollow-upasshownintheflow diagram(Fig.1),130subjectswheresubmittedtodata anal-ysis(A=60;B=33;C=37).Subjectandlaborcharacteristics arereportedinTable1.
ThemedianVNSformaternalsatisfactionwas8.8(95%CI 8.3---9.3)forgroupA(CEI);8.6(95%CI7.9---9.3)forgroupB (PIEB0.1%)and8.6(95%CI7.7---9.4)forgroupC(PIEB0.15%) (p>0.05).
Motorblockoccurredatleastonceduringlaborin6.7% ofcasesintheCEIgroupand2.7%ofcasesinthePIEB0.15% group(p>0.05).NoparturientinPIEB0.1%groupreported motorblock.Theoddsratioforoccurrenceofmotorblock inCEIandPIEB0.15%was2.47(95%CI0.28---21.3).
When we analyze labor outcomes(reported in Fig.2), comparingthethreemaintenancetechniques,we founda
60%
50%
40%
30%
20%
10%
0%
Eutocic* Caesarean* Instrumental
CEI PIEB 0.1% PIEB 0.15% 56.5%
(n=13) 50.6%
(n=39)
26% (n=20)
23.4% (n=18)
34.8% (n=8)
36.6% (n=11)
26.7% (n=8)
36.6% (n=11)
8.7% (n=2)
Figure2 Laboroutcomepresentedaspercentageand num-ber(n). CEI,continuous epiduralinfusion; PIEB,programmed intermittentepiduralbolus;*statisticallysignificantdifference (p<0.05).
significantdifferenceinceasareandelivery(p=0.02)rates, butnodifferenceininstrumentaldeliveryrates(p=0.74).
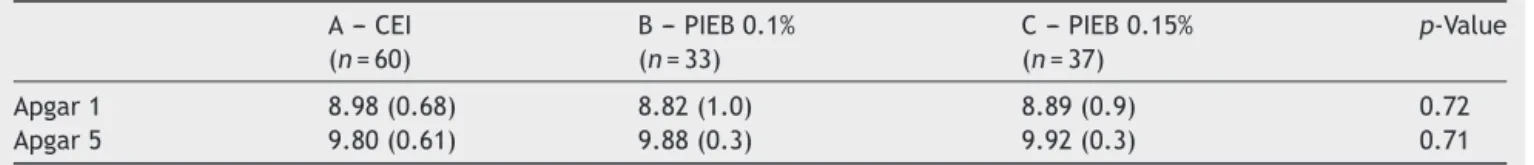
NeonataloutcomesevaluatedbytheApgarscoreat1st and 5thminutes where similarbetween groups (p>0.05). MeanApgarscoresarepresentedinTable2.
There was no significant difference in sensory spread (describedasnumbnessbytheparturient)betweengroups (p=0.59).Cardiovascularchangesandincidenceofnausea andvomiting hada verylowincidence withnosignificant differencesbetweengroups.
Discussion
Maternalsatisfactionisoneofthesecondaryoutcomes indi-catedin theresultsof manystudies,4,14---17 which compare
differentnewtechniquesoflaboranalgesiamaintenance. Analgesiaandsatisfactionwithanalgesiaarenot equiv-alent concepts. Continuousand stableanalgesia,sense of control,painlessuterinecontractionfeeling,abilitytowalk, absenceof numbnessandmotor blockand abilitytopush arealsoimportanttodeterminematernalsatisfactionwith laboranalgesia.14
Otherauthorsfoundagreatersatisfactionratingin sub-jectswhoreceivedPIEB.4TheycomparedPIEBandCEI,both
withPCEA,inwomenundergoinginductionoflabor,hence withhigherpainscoresandinwhichtheanalgesiaefficacyof PIEBmayhaveoverstatedthisdifference.4Alsomost
stud-iestodatearehighlycontrolledandtheirresultsmaynot bereadilyapplicable inthe contextofday-to-dayclinical practice.
Wefoundnostatisticaldifferenceinneonataloradverse outcomesasnumbnessandmotorblock.Nevertheless,there wasalowerincidenceofmotorblockadeinPIEB0.1%group. Thisislikelyexplainedbytheuseofalessconcentratedlocal anestheticsolutionasshowninpreviousstudies.4,18Because
motorblockadeisconsideredundesirableduringlabor anal-gesia,thepotentialdose-sparingeffectofanintermittent bolustechniquemaybemoreclinicallyrelevantwhenlower concentrationoflocalanestheticsolutionsareused.4
Table2 MeanApgarscoresat1stand5thminutespresentedasmean(SD).
A---CEI B---PIEB0.1% C---PIEB0.15% p-Value (n=60) (n=33) (n=37)
Apgar1 8.98(0.68) 8.82(1.0) 8.89(0.9) 0.72
Apgar5 9.80(0.61) 9.88(0.3) 9.92(0.3) 0.71
CEI,continuousepiduralinfusion;PIEB,programmedintermittentepiduralbolus.
thatwedoubledthevolumeinPIEBgroups. Thisfindingis probablyrelatedtothereducedincidenceof motorblock from the combinedbenefits of Ropivacaine, the use of a lowerlocalanestheticconcentration18andmainlythePIEB
technique.
The incidence of instrumental delivery in PIEB groups washigherthanweexpectedandhigherthanotherstudies results,12howeversimilartoourusualstatistics.One
possi-ble explanationis theinfluence of obstetric performance and other obstetric factors in labor outcome. Further-moretheprogrammedintermittentbolus mayoverlapthe expulsionperiodandhencemake theparturientunableto accomplishaneffective expulsiveeffort.Inthe futurewe intendtoclarify theseand other factorsthat canhelp us improve labor analgesia protocols. Although instrumental delivery was higherthan we expected, therewasno sta-tistically significant difference between groups, as other studieshaveshown.4,10Weemphasizethatthereductionof
caesarean delivery,which has higher risksto mother and newborn, is a crucial clinical finding, however larger tri-als aimedatevaluatinglaboroutcomesareneededin the future.
We conducted this study due tothe growing evidence of the efficacyof epidural bolus injection.Several mech-anisms have been suggested toexplainthe benefitsof an epiduralboluscomparedwithacontinuousinfusionof solu-tion.Invitroandlaboratorystudieshavedemonstratedthat an epidural bolus results in a further uniform spread of the solutions in the epidural spaceas opposedto contin-uous administration.7,8 Indeed, analgesiaand motorblock
are produced by the movement of local anesthetic from the extraneural to the intraneural space by a diffusion gradient.9Nerveblockadeisachievedwhentheintraneural
concentrationishigherthantheextraneuralconcentration. If we use low concentrations of local anesthetic in inter-mittent boluses, the total amount of solution inside the nerveisinsufficienttoresultinmotorblockade.Ifweusea continuousinfusion,theextraneuralconcentrationoflocal anesthetic is persistently higher allowing the intraneural concentrationtoreachthethresholdformotorfiberblock.9
Despite these scientific proves, there is still lacking consistency in studies comparing CEI and PIEB. We can hypothesizethat the variationfromour results andother studies results may conceivablybe associatedto the fact thatweanalyzed asamplethatrepresentstheday-to-day women encountered in our clinical practice, as opposed to other conducted controlled studies. Additionally, the localanestheticconcentrations,totalanestheticdose,bolus volumesandtimeintervalsweused,differfromother inves-tigations.
Arecentsystematicreview,12revealedthatmorestudies
shouldbecarriedouttodeterminetheidealPIEBregimen
(pump settings and local anesthetic concentration/opioid dose),thatshowsaconsistentimprovementinlabor analge-siawithafavorableeffectonobstetricoutcomes.However itisclearthatintermittentepiduralbolustechniqueallows theuseoflessconcentratedlocalanestheticsolutionswith clinicallyrelevanteffects.
To findtheoptimumsettings for thebolus volumeand timeintervalinthemaintenanceofepidurallaboranalgesia, astudiedconductedwithnulliparouswomen,manipulating bolustimeintervalandbolus volume.19 Extendingthe
pro-grammed intermittentbolus intervaland volume from15 to60min resulted in lower local anesthetic consumption withsimilaranalgesia.Therewerealsolessadditionalbolus requestsforbreakthrough pain,anincreaseinthetimeto thesedoses and, consequently, earlier feelingof comfort andhighersatisfaction.
Thereareseverallimitationstothegeneralizationofour study conclusions. Firstthe difference in localanesthetic dose perhour between CEI andPIEB groups is an obvious methodologicallimitationthatwecouldnotcontroldueto hospitalpolicies.InsubjectsrandomizedtoCEIgroup,PCEA wasusedasarescuemodality,whichmayhaveattenuated thedifferenceinsatisfactionbetweengroups.PCEAwithout a background infusion is also an intermittent bolus tech-niquebutwhetherthePIEBissuperiortoPCEAremains to bedetermined.
Weusedone-dimensionalscaletoevaluatematernal sat-isfaction because it was simpler but these scales do not reflectthemultipledimensionsofmaternalsatisfaction.
Anotherobvious limitationwasthe lack of controland potentialimpactofmultipleconfoundingfactorsknownto influencethematernalsatisfactionandoutcomes,including theperformance fromanesthesiaandobstetricproviders, labor management, social level and schooling. Another such confounding factor is the density of neuraxial anal-gesia during the second stage of labor. Relaxation of the abdominalwallmusculaturesecondarytoepiduralanalgesia couldresultindecreasedeffectivenessofmaternal expul-sive efforts and ability to coordinate these with uterine contractions.20 Additionally, higher amounts and
concen-trations of neuraxial local anesthetic might relax pelvic floormusculature andinterfere withfetalrotationduring descent.Alsoobstetriciansmightbemorelikelytoperform instrumentalvaginaldeliveriesinparturientswitheffective second-stageanalgesiathaninparturientswithout analge-sia.
In conclusion, we found that maintenance of epidural analgesiawithprogrammedintermittentbolus was associ-atedwithalowercaesareandeliveryrate,withequallyhigh maternalsatisfactionandnoadverseoutcomes.
choosingthelocalanesthetics, volume,concentrationand timeintervalidealforPIEBregiments.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.MelzackR.Themythofpainlesschildbirth(theJohnJ.Bonica lecture).Pain.1984;19:321---37.
2.Lavand’homme P. Chronic pain after vaginal and caesarean delivery: arealityquestioningourdailypracticeofobstetric anesthesia.IntJObstetAnesth.2010;19:1---2.
3.WongCA,ScavoneB,PeacemanA,etal.Theriskofcaesarean deliverywithneuraxialanalgesiagivenearlyversuslateinlabor. NEnglJMed.2005;352:655---65.
4.Wong CA, Ratliff JT, Sullivan JT, et al. A randomized com-parison of programmed intermittent epidural bolus with continuousepiduralinfusionforlaboranalgesia.AnesthAnalg. 2006;102:904---9.
5.BoutrosA,BlaryS,BronchardR,etal.Comparisonof intermit-tentepiduralbolus,continuousepidural infusionandpatient controlled-epiduralanalgesiaduringlabor.IntJObstetAnesth. 1999;8:236---41.
6.ThorntonJG,CapognaG. Reducinglikelihood ofinstrumental deliverywithepiduralanesthesia.Lancet.2001;358:2. 7.HoganQ.Distributionofsolutionintheepiduralspace:
exam-ination by cryomicrotome section. Reg Anesth Pain Med. 2002;27:150---6.
8.KaynarAM,ShankarKB.Epiduralinfusion:continuousorbolus? AnesthAnalg.1999;89:534---634.
9.Capogna G, Stirparo S. Techniques for the maintenance of epidural labor analgesia. Curr Opin Anesthesiol. 2013;26: 261---7.
10.FettesP,MooreC,WhitesideJ,etal.Intermittentvs. contin-uousadministrationofepidural ropivacainewithfentanylfor analgesiaduringlabour.BrJAnaesth.2006;97:359---64. 11.CapognaG,CamorciaM,StirparoS,etal.Programmed
inter-mittentepiduralbolusversuscontinuousepiduralinfusionfor laboranalgesia:theeffects onmaternal motorfunction and laboroutcome.Arandomizeddouble-blindstudyinnulliparous women.AnesthAnalg.2011;113:826---31.
12.George R, Terrence A, Habib A. Intermittent epidural bolus compared withcontinuous epidural infusions for labor anal-gesia: a systematicreview and meta-analysis.Anesth Analg. 2013;116:133---44.
13.BromagePR.Epiduralanalgesia.1sted.Philadelphia:WB Saun-ders;1978.p.144.
14.Stirparo S, Camorcia M, Capogna G. Maternal satisfaction with different techniques of epidural analgesia: a compari-sonbetweentopups,programmedintermittentepiduralbolus (PIEB)andcontinuousepidural infusion(CEI).EurJAnaesth. 2010;27:164.
15.ClivattiJ,SiddiquiN,GoelA,etal.Qualityoflaborneuraxial analgesiaandmaternal satisfactionata tertiarycare teach-inghospital:aprospectiveobservationalstudy.CanJAnaesth. 2013;60:787---95.
16.LeoS,SiaA.Maintaininglabourepiduralanalgesia:whatisthe bestoption?CurrOpinAnaesthesiol.2008;21:263---9.
17.LoubertC,HinovaA,FernandoR.Updateonmodernneuraxial analgesiainlabour:areviewoftheliteratureofthelast5years. Anaesthesia.2011;66:191---212.
18.GómezFC,SerraJS,GalindoIT,etal.0.2%ropivacainevs.0.1% ropivacaineplusfentanylinobstetricepiduralanalgesia.Rev EspAnestesiolReanim.2000;47:332---6.
19.WongCA,McCarthyRJ,HewlettB.Theeffectofmanipulation oftheprogrammedintermittentbolustimeintervaland injec-tionvolumeontotaldruguseforlaborepidural analgesia:a randomizedcontrolledtrial.AnesthAnalg.2011;112:904---11. 20.CambicRC,WongCA.Labouranalgesiaandobstetricoutcomes.