REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Bilateral
greater
occipital
nerve
block
for
treatment
of
post-dural
puncture
headache
after
caesarean
operations
Esra
Uyar
Türkyilmaz
a,∗,
Nuray
Camgöz
Eryilmaz
a,
Nihan
Aydin
Güzey
a,
Özlem
Moralo˘
glu
baZekaiTahirBurakWomens’HealthTrainingandResearchHospital,DepartmentofAnesthesiologyandReanimation,Ankara,
Turkey
bZekaiTahirBurakWomens’HealthTrainingandResearchHospital,DepartmentofObstetricsandGynecology,Ankara,Turkey
Received3December2014;accepted23March2015 Availableonline21January2016
KEYWORDS Post-duralpuncture headache;
Caesarean operations; GONblock
Abstract
Background: Post-duralpunctureheadache(PDPH)isanimportantcomplicationofneuroaxial anesthesiaandmore frequentlynotedinpregnantwomen.Thepain isdescribedassevere, disturbinganditslocationisusuallyfronto-occipital.TheconservativetreatmentofPDPH con-sistsofbedrest,fluidtheraphy,analgesicsandcaffeine.Epiduralbloodpatchisgoldstandard theraphybutitisaninvasivemethod.Thegreateroccipitalnerve(GON)isformedofsensory fibers thatoriginateintheC2andC3segmentsofthespinalcordanditisthemainsensory nerveoftheoccipitalregion.GONblockagehasbeenusedforthetreatmentofmanykindsof headache.TheaimofthisretrospectivestudyistopresenttheresultsofPDPHtreatedwith GONblockover1yearperiodinourinstitute.
Methods:16patientswhohadbeendiagnosedtohavePDPH,andperformedGONblockafter caesarean operations were included inthe study. GON blocks were performed as the first treatmentdirectlyafterdiagnoseofthePDPHwithlevobupivacaineanddexamethasone.
Results:ThemeanVASscoreofthepatientswas8.75(±0.93)beforetheblock;3.87(±1.78) 10minaftertheblock;1.18(±2.04)2haftertheblockand2.13(±1.64)24haftertheblock. Noadverseeffectswereobserved.
Conclusions: TreatmentofPDPH with GONblock seemsto beaminimal invasive,easy and effectivemethodespeciallyaftercaesareanoperations.AGONblockmaybeconsideredbefore theapplicationofabloodpatch.
©2015SociedadeBrasileiradeAnestesiologia.Publishedby ElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
∗Correspondingauthor.
E-mail:esrauyarturkyilmaz@yahoo.com(E.UyarTürkyilmaz). http://dx.doi.org/10.1016/j.bjane.2015.03.004
PALAVRAS-CHAVE Cefaléiapós-punc¸ão dural;
Cesarianas; BloqueiodoNOM
Bloqueiobilateraldonervooccipitalmaiorparatratamentodecefaleiapós-punc¸ão duralapóscesarianas
Resumo
Justificativa:Acefaleiapós-punc¸ãodural(CPPD)éumacomplicac¸ãoimportantedaanestesia neuroaxialemais frequentementeobservadaem mulheresgrávidas. A dorédescrita como intensa,perturbadora,esualocalizac¸ãoégeralmentefronto-occipital.Otratamento conser-vadordaCPPDconsisteemrepousonoleito,fluidoterapia,analgésicos ecafeína. Otampão sanguíneoperiduraléopadrãoourodetratamento,maséummétodoinvasivo.Onervo occip-italmaior(NOM)éformadoporfibrassensoriaiscomorigemnossegmentosC2eC3damedula espinhaleéoprincipalnervosensorialdaregiãooccipital.ObloqueiodoNOMtemsidousado paraotratamentodemuitostiposdedordecabec¸a.Oobjetivodesteestudoretrospectivofoi apresentarosresultadosdeCPPDtratadacombloqueiodoNOMnoperíododeumanoemnosso instituto.
Métodos: 16pacientesqueforamdiagnosticadascomCPPDesubmetidasabloqueiodeNOM após cesariana foram incluídas no estudo. Os bloqueios do NOM foram realizados como o primeirotratamentoimediatamenteapósodiagnósticodeCPPDcomlevobupivacaínae dex-ametasona.
Resultados: AmédiadosescoresEVAdaspacientesfoide8,75(±0,93)antesdobloqueio;3,87 (±1,78)10minutosapósobloqueio;1,18(±2,04)2horasapósobloqueioe2,13(±1,64)24 horasapósobloqueio.Efeitosadversosnãoforamobservados.
Conclusões:OtratamentodaCPPDcombloqueiodoNOMpareceserummétodominimamente invasivo,fácileeficaz,especialmenteapóscesarianas.ObloqueiodoNOMpodeserconsiderado antesdaaplicac¸ãodeumtampãosanguíneoperidural.
©2015SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigoOpen Accesssobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Post-dural puncture headache (PDPH) is an disturbing complicationof neuroaxial anesthesia and occurs approx-imately in 1.5% of cases ranging from 0.19% to 3.6% in differentunits.1PDPHismorefrequentlynotedinpregnant
womenreceivingneuroaxialanesthesia.2 Thetypical
loca-tionofthe headacheisusually bifrontaland/or occipital. It is described as severe, disturbing and debilitating pain thatisincreasingintheuprightpositionwhiledecreasingor completelydisappearinginthesupineposition.3According
tothe InternationalHeadacheSociety,headachedevelops within5daysaftertheduralpunctureandresolveseither spontaneouslywithin7 daysor within48hafter effective treatmentofthespinalfluidleak.4Theconservative
treat-mentofPDPHusuallyconsistsoffluidtheraphy,analgesics andcaffeine. Epidural blood patch (EBP) is gold standard theraphybutitisaninvasivemethod.
The greateroccipitalnerve(GON)is formedof sensory fibers that originate in the C2 and C3 segments of the spinalcord.5 It isthe main sensorynerve of theoccipital
region. GON blockage has been used successfully for the treatment of cervicogenic headache, occipital neuralgia, cluster headache, and migraine.5,6 Accompanying clinical
symptomsofPDPHareverysimilartothoseofcervicogenic headachethat have been effectivelytreated with occipi-talnerveblockade.7GONblockis reportedtobeusedfor
treatmentofPDPHinindividualcasesandinonecontrolled study.8---10 The aimofthisretrospectivestudyistopresent
the results of PDPH treated with GON block over 1 year periodinourinstitute.
Methods
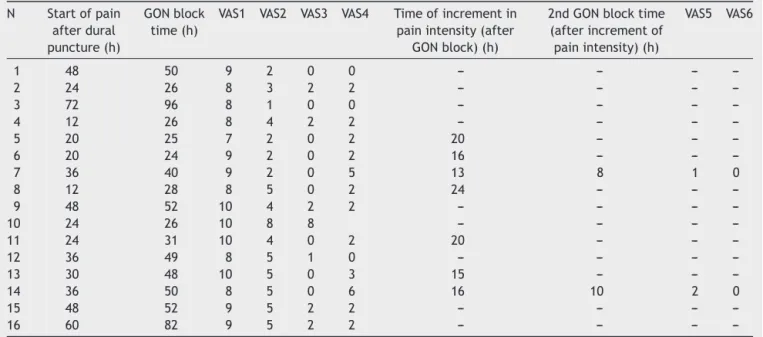
After the improvement of Local Ethics Committee, the patients whohadbeen diagnosedtohave PDPH, and per-formed GON block as the first choice treatment after caesareanoperationsweredeterminedfromtheanesthesia departmentrecordsandincludedinthestudy.Thefollowing parametershadbeenreceivedfromtheanesthesia depart-mentrecords:thetypeanddiameteroftheneedle,thetime when theheadachestarted postoperativelyandwhen the GONblockperformed,thevisualanalog score(VAS)ofthe patientsbeforetheGONblock,10min,2hand24hafterthe GONblock.Ifthereisan incrementinintensity ofpainat theevaluationat24thhour;timeofincrementofpain,VAS aftertheincrementofpain,anyneed forasecond block. Ifasecondblockisperformed;VASofthepatients2hand 24hafterthesecondGONblock
All the headaches occurring after regional anesthesia are firstly evaluated by anesthesia department. For the diagnosisofPDPH,thecriteriaestablishedbyInternational HeadacheSocietyhadbeenused.11Thediagnosticcriteriais
afterduralpuncture;and(4)headacheresolves:(a) spon-taneouslywithin1week(95%ofcases);and(b)within48h afterepiduralbloodpatch(EBP).Allthepatientswhohad beendiagnosedtohavePDPHwereinformedabout conser-vativetheraphy,EBP andGONblock.Patientswhorefused bedrest,demandedearlymobilizationandalsorefusedan EBPasafirstchoice treatmentwereinformedabout GON block and it had been emphasized to thesepatients that thiswasnotaroutinetreatmentforPDPH.Beforetheblock, informedconsentwasobtainedfromthepatients, explain-ingthattheprocedurewasnotroutinetreatment.AsGON block is not a routine treatment for postdural puncture headache,the patients wereobserved closely and during GONblockperiodtherecordswerekeptstrictly.
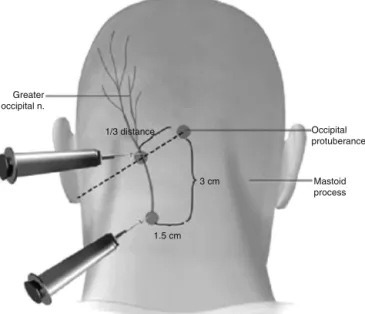
GON blocks were performed as the first treatment directlyafterdiagnoseofthePDPH.Alltheblockswere per-formedbythesametwoanesthesiologistwhohadtenyears experienceinanesthesia.Followingroutinemonitorization (bloodpressure,pulseoximetry,3-leadelectrocardiogram), anivaccesswassecured.BilateralblockadeoftheGONwas performed bythemethodwhich isbased onthe anatomi-callandmarks.TheGONislocatedapproximatelytwothirds of the distance on a line drawn from the center of the mastoidtotheexternaloccipitalprotuberance(Fig.1).12,13
External occipital protuberance (EOP) was palpated and a needle wasinserted between 15mm and 25mm lateral tothe EOPparallel tothe superiornuchal line. 2.5mLof treatmentsolutionwasinjectedeach side.Thetreatment solution consisted of levobupivacaine 2.5mgmL−1
(Chiro-caine 50mg/10mL ampoule, Abbott) and dexamethasone 1mgmL−1 (Onadron 8mg/2mL ampoules, ˙I.E. Ulagay ˙Ilac¸
Sanayii Türk A.S¸.). A second block was performed if the VAS score is higher than 3. Ifsecond block is performed, onlylevobupivacaine2.5mgmL−1(Chirocaine50mg/10mL
ampoule,Abbott) without dexamethasone wasused. Sen-sory changes such as numbness or sensory loss of the dermatomewascheckedaftertheGONblock.Iftherewere
Greater occipital n.
1.5 cm
3 cm Mastoid
process Occipital protuberance 1/3 distance
Figure1 TheGON locatedapproximatelytwothirdsofthe distanceonalinedrawnfromthecenterofthemastoidtothe externaloccipitalprotuberance.
Table1 Demographiccharacteristicsofthepatients.
Mean±SD
Age(years) 29.87(±3.84)
Height(cm) 163.87(±4.19)
Weight(kg) 74.34(±3.40)
BMI(kgm−2) 27.73(±1.36)
no sensory changes, it was decided that the block was failed.TogetherwithGONblockade,oralhydrationhadbeen commenced.Vasovagalsyncopalattack,transientdizziness followingtheinjection,intravascularinjectionofthelocal anestheticsolutionarereportedasadverseaffectsofGON block.14,15 Any adverse effects during and afterthe block
wererecorded. Patients wereexamined onthe third and seventhdayaftertheblock.
Results
In our institution 7864 patients had underwent spinal anesthesiafor caesareanoperationsbetween Januaryand December 2013. 289 patients had been evaluated for headache.213patientshadbeendiagnosedtohavePDPH. Conservativetheraphyhadbeenusedfor188patients,EBP had been used for 9 patients and GON block had been usedfor 16 patientsasthefirst choicetreatment. Among the patients who had been threatened with conservative theraphy;92patientshadadequateanalgesia,73patients hadinadequateanalgesiabutrefusedanyothertherapeutic optionsandEBPwasusedfor23patients.
All of our patients received spinal anesthesia for cae-sareanoperation.Thedemographicalcharacteristicsofthe patientsaredetailedinTable1.None ofourpatientshad preeclampsia,historyofheadacheoranyneurological dis-order.Spinalblocksareperformed using26gaugeneedles withan atraumaticbevel (Atraucan®,B-Braun,Germany).
Nocomplicationsoccurredduringtheoperations.Themean durationforthestartofthecomplaintsofthetypical symp-tomsof PDPH was 34.37 (±17.11)h afterdural puncture. The mean duration for performing GON block was 44.06 (±20.01)hafterduralpuncture.
Table2 Theonsettime,GONblocktime,painlessdurationandtheintensityofpain.
N Startofpain afterdural puncture(h)
GONblock time(h)
VAS1 VAS2 VAS3 VAS4 Timeofincrementin painintensity(after
GONblock)(h)
2ndGONblocktime (afterincrementof painintensity)(h)
VAS5 VAS6
1 48 50 9 2 0 0 --- --- ---
---2 24 26 8 3 2 2 --- --- ---
---3 72 96 8 1 0 0 --- --- ---
---4 12 26 8 4 2 2 --- --- ---
---5 20 25 7 2 0 2 20 --- ---
---6 20 24 9 2 0 2 16 --- ---
---7 36 40 9 2 0 5 13 8 1 0
8 12 28 8 5 0 2 24 --- ---
---9 48 52 10 4 2 2 --- --- ---
---10 24 26 10 8 8 --- --- ---
---11 24 31 10 4 0 2 20 --- ---
---12 36 49 8 5 1 0 --- --- ---
---13 30 48 10 5 0 3 15 --- ---
---14 36 50 8 5 0 6 16 10 2 0
15 48 52 9 5 2 2 --- --- ---
---16 60 82 9 5 2 2 --- --- ---
---VAS1,VASbeforeGONblock;VAS2,VAS10minutesafterGONblock;VAS3,VAS2hoursafterGONblock;VAS4,VAS24hoursafterGON block;VAS5,VAS2hoursafterthesecondGONblock;VAS6,VAS24hoursaftersecondGONblock.
Discussion
Lossofcerebrospinalfluid(CSF)throughduralholeresults in a decrease in CSF volume and pressure. This CSF vol-ume and pressure loss may cause downward traction on thepain-sensitiveintracranialveinsandmeninges, aswell asthe cranialnerves.3,8 Itis notpossibletoexplainPDPH
only with traction theory. The bimodal theory suggests thatthereis a combination ofboth low CSFpressureand resultantcerebralvasodilatationinreactiontothe stretch-ingof vessels.2 Pregnant womenareparticularly proneto
PDPH.16,17 Additionally, the intensity of PDPH in obstetric
patientsisreportedtobesignificantlyhighercomparedwith theotherpatients.18
TheconservativetreatmentofPDPHconsistsofbedrest, non-steroidal anti-inflammatory drugs (NSAIDs), caffeine andweakopioidanalgesics.Adecreaseinthedurationand severityofheadache,needforanyothertherapeuticoption (e.g.EBP),improvementofdailyactivityisexpectedfrom thetreatment modality. Whereas, Sprigge etal. reported thatbedrestandmildanalgesicsdidnotgiveeffectivepain reliefformorethan14%ofpatientssufferedfromPDPH.19
Studiescomparingtheeffectsofconventionalmedical treat-ment and EBP, report that results did not evidence any reductionof painduring the 24 hoursof follow upin the conventionalmedicaltreatmentgroup18andmorepatients
intheEBPgroupfeltbetterat24hcomparedwiththe con-servativegroup(89% vs.19%).20 Bed restdoes not appear
toaffectthecourseofPDPH.21,22Onerecentmetaanalysis
showedthattheefficacyoforalandIVcaffeine administra-tionwasofnobenefit.23
The most effective treatment for PDPH is EBP, which involvestheinjectionofautologousbloodintotheepidural space.EBPisaninvasivemethodandhasmanysideeffects. Itmaycontributetodevelopmentofbackpain,lumbar ver-tebralsyndrome,transientbradycardia,andanincreasein
bodytemperature.24Longertermcomplicationsarerarebut
examplesincludemeningitis,arachnoiditis,lumbovertebral syndromeandradicularpain.25
Therapeuticepiduralbloodpatchreportedtodecrease PDPHandseverePDPHoverconservativetreatment.26The
cumulativeprobabilityofcompleterecoverywas84%after 1 week in patients allocated to EBP and 14% in patients allocatedtoconservativetreatment.20
Althoughanepiduralbloodpatchremainsthedefinitive treatmentforPDPH,surveysaboutthemanagementofPDPH in differentunitsandcountriespresent thatmost respon-dents first treated the patients conservatively. In surveys aboutUK,GermanandTurkishpractice;71%,94.5%and64% ofrespondersarereportedtoperformEBPafterthefailure ofconservativemeasuresrespectively.27---29National
Obstet-ric Anesthetic Database showed that EBP was performed within two daysof delivery in only 42% women.30 In this
situation,asmentionedabovemanypatients arelefttoa relativelyloweffectivetreatmentperiod.Anyother treat-ment modality which is more effective than conservative treatmentandlessinvasivethanEBPisseemstobeneeded. ApossibletreatmentmethodforPDPHisGONblockade. Therationaleforusinggreateroccipitalnerveblockcomes fromtheproximityofsensoryneuronsintheuppercervical spinal cord tothe trigeminal nucleus caudalis (TNC) neu-ronsandtheconvergenceofsensoryinputtoTNC neurons frombothcervicalandtrigeminalfibres.31Theconvergence
withinthetrigeminocervicalnucleusallowsthebidirectional exchange of sensory information between the trigeminal andtheuppercervicalspinalnerves.32Sincethebranchof
greateroccipitalnervearisingfromC2rootisresponsiblefor theinnervationofdeepparaspinalmusclesandsuboccipital configurations,greateroccipitalnerveblockadeinhibitsthe stimulations arisingfrom these regions innervated by the greateroccipital nerve.33 Thisblockadeensures the
componentnerveroots organglia.The analgesiaobtained aftertheblockmaybeexplainedbythecentral neuromod-ulatory effectthat causes decreased central sensitization asaresultofthetemporaryinterruptionofafferentinput tothedorsalrootsandtrigeminalnucleus.34 Itisnotclear
why,consideringtheetiology,theheadachestopped defini-tively. Reducing nociceptive traffic through a temporary neuralblockadeinasensitizedsystemmayallow ‘‘winding-down’’ofcentralsensitization.Ongoingpainonthebasisof peripheralsensitizationcouldalsobeenhancedthroughthe sameprocess.12Neurologicalexaminationsandradiological
investigations should be considered in persistent post-spinalcasessothatneurologicalcomplicationscanberuled out.
We observed that the GON blockade was effective in stopping PDPHafter caesareanoperations. The mean VAS score of the patients was 8.75 (±0.93) before the block; 3.87(±1.78)10minaftertheblock;1.18(±2.04)2hafter theblock and2.13(±1.64) 24h aftertheblock.Only one ofourpatientshadneithersensorylossofthedermatome noradecreaseatVASscore10minand2hafterblock,this wasevaluatedfailureoftheblockandthepatientwas con-vincedforEBP.ThepainofthispatientstoppedafterEBP. Ourresultsareconsistentwiththepreviouslyreportedcases andastudycomparingtheeffectsofGONblockwith con-ventionaltheraphy.
Matuteetal.8reportedtheeffectofbilateralGON
block-ageonPDPHwith2cases.Neitherpatienthadrespondedto conservativetreatmentthenablockwasperformedusinga mixtureof4mL0.25%bupivacaineand20mgtriamcinalone. Thepainresolvedwithin1---2minandthepatientswere dis-charged48hlater.Takmazetal.9reportedacaseinwhicha
PDPHdidnotrespondtoconservativetherapyandresolved within2minwithaGONblockperformedwith2mLof0.5% bupivacaine.12haftertheblock,hereportedmildpainthat didnotrestricthisdailyactivity.Theblockswererepeated, whereuponhispaincompletelydisappeared.Najaetal.10
comparedtheeffectofbilateralGONblockageonPDPHwith conventionaltreatmentandreportedthatthepainresolved completely using 1 or 2 injections in 68% of the patients whiletheremaining32%required3or4injections.Weused a mixture of levobupivacaine 0.25% and dexamethasone 1mgmL−1 and injected 2.5mL each side. It is mentioned
thatlocalanestheticswithsteroidwasmoreeffectivethan localanestheticaloneforsuboccipitalinjection.35
It isimportanttostop PDPHespeciallyaftercaesarean operationsbecauseitofteninterfareswithmaternal-infant interaction.The patientsaremostcomfortablewhenthey areinsupinepositionbutmuchobstetricpatientisunable to do this because of the newborn baby. It is reported in a study designed toinvestigate the patientexperience following accidental dural puncture complicating obstet-ric epiduralanalgesia that, afterheadache, bed rest was amajorcomplaintofthepatients;manypatientscouldonly getrelieffromtheirheadachewhensupinebutfound nurs-ingandfeedingababyextremelydifficultwhenprostrate; 47% patients complained that being confined to bed was theworstaspect.36 Inourstudygroupafterapplicationof
GONblock, patientswere mobilizedandcouldbe ableto nurse andbreastfeed their babies easily. Forthis reason, GONblockadeisseemstobemoreuseful aftercaeserean operationscomparedwithothersurgerytypes.
GONblockisusedfor differenttypesofheadaches, its adverse effects are previously evaluated.14 The adverse
effects of GON block are reported as vasovagal syncopal attack, transient dizzinessfollowing the injection, alope-ciaaroundtheinjectionsiteandexaggeratedheadache.15
Greateroccipitalnerve hassuperficial locationleading to lessercomplications;however,thereisintravascular injec-tionrisk,whichcanbereducedbycarefulaspiration.None oftheseoccurred inour16 patients.Alopecia aroundthe injectionsideisalongertimecomplication;wemade expla-nationaboutthis complicationtoourpatients, nopatient appealedwiththecomplaintofalopecia.
One of the limitations of our study is lack of control group.The effectivenessofGONblockcouldbecompared with the conservative therapy but in our institution the recordsofthepatientswhohadbeenthreatenedwith con-servativetherapyhadnotbeenkeptasstrictasthepatients whohadbeenthreatenedwithGONblock.Acontrolled ran-domizedstudyisneededforcomparingtheefficiencyofthe methods.Anotherlimitationofourstudyisthepossibilityof investigatorbias.
Inconclusion,treatmentofPDPHwithGONblockisseems tobeaminimalinvasive,easy andeffectivemethod espe-ciallyfor patients likenew mothers AGON block maybe consideredbeforethe application ofa blood patch. Well-designedcontrolledstudiesareneededtoassesstheroleof GONblockinthetreatmentofPDPH.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.ChoiPT,GalinskiSE,TakeuchiL,etal.PDPHisacommon compli-cationofneuroaxialblockadeinparturients:ameta-analysisof obstetricalstudies.CanJAnaesth.2003;50:460---9.
2.CandidoKD,StevensRA.Post-duralpunctureheadache: patho-physiology, prevention and treatment. Best Pract Res Clin Anaesthesiol.2003;17:451---69.
3.Turnbull DK, Shepherd DB. Post-dural puncture headache: pathogenesis, prevention and treatment. Br J Anaesth. 2003;91:718---29.
4.AmorimJA,GomesdeBarrosMV,ValencMM.Post-dural (post-lumbar)punctureheadache:riskfactorsandclinicalfeatures. Cephalalgia.2012;32:916---23.
5.AnthonyM.Cervicogenicheadache:prevalenceandresponseto localsteroidtherapy.ClinExpRheumatol.2000;18:59---64. 6.PeresMFP,StilesMA,SiowHC,etal. Greateroccipitalnerve
blockadeforclusterheadache.Cephalalgia.2002;22:520---2. 7.Naja ZM, El-Rajab M, Al-Tannir MA, et al. Occipital nerve
blockadeforcervicogenicheadache:adouble-blindrandomized controlledclinicaltrial.PainPract.2006;6:89---95.
8.MatuteE,BonillaS,GironesA,etal.Bilateralgreater occipi-talnerveblockforpost-duralpunctureheadache.Anaesthesia. 2008;63:551---60.
9.TakmazS,ÜnalKC¸,KaymakC¸,etal.Treatmentofpost-dural punctureheadachewithbilateralgreateroccipitalnerveblock. Headache.2010;50:869---81.
11.Headache Classification Subcommittee of the International HeadacheSociety.TheInternationalClassificationofHeadache Disorders:2ndedition.Cephalalgia.2004;24:9---160.
12.LevinM.Nerveblocksinthetreatmentofheadache. Neurother-apeutics.2010;7:197---203.
13.YoungWB, MarmuraM,AshkenaziA, et al.Greater occipital nerve and otheranesthetic injections for primary headache disorders.Headache.2008;48:1122---5.
14.TobinJ,FlitmanS.Occipitalnerveblocks:whenandwhatto inject?Headache.2009;49:1521---33.
15.AfridiSK,ShieldsKG,BholaR,etal. Greateroccipitalnerve injectioninprimaryheadachesyndromes---prolongedeffects fromasingleinjection.Pain.2006;122:126---9.
16.PaechM,BanksS,GurrinL.Anauditofaccidentaldural punc-ture duringepiduralinsertion ofa Tuohyneedleinobstetric patients.IntJObstetAnesth.2001;10:162---7.
17.KuczkowskiKM.Postduralpunctureheadacheintheobstetric patient:anoldproblem.Newsolutions.MinervaAnesthesiol. 2004;70:823---30.
18.Sandesc D,Lupei MI, SirbuC,et al.Conventional treatment orepiduralbloodpatchforthetreatmentofdifferent etiolo-giesofpostduralpunctureheadache.ActaAnaesthesiolBelg. 2005;56:265---9.
19.SpriggeJS,HarperSJ.Accidentalduralpunctureandpostdural punctureheadacheinobstetricanaesthesia:presentationand management:a23-year surveyina districtgeneralhospital. Anaesthesia.2008;63:36---43.
20.vanKootenF,OeditR,BakkerSLM,etal.Epiduralbloodpatch in post dural puncture headache: a randomised, observer-blind,controlledclinicaltrial.JNeurolNeurosurgPsychiatry. 2008;79:553---8.
21.Arevalo-RodriguezI,CiapponiA,MunozL,et al.Postureand fluidsforpreventingpost-duralpunctureheadache.Cochrane DatabaseSystRev.2013;12:7.
22.ChoiPT,Galinski SE,LucasS,et al.Examining theevidence in anesthesia literature: a survey and evaluation of obstet-rical postdural puncture headache reports. Can J Anaesth. 2002;49:49---56.
23.Halker RB, Demaerschalk BM, Wellik KE,et al. Caffeine for thepreventionandtreatmentofpostduralpunctureheadache: debunkingthemyth.Neurologist.2007;13:323---7.
24.OhJ,CamannW.Severe,acutemeningealirritativereaction afterepiduralbloodpatch.AnesthAnalg.1998;87:1139---40. 25.Boyle JAH, Stocks GM. Post-dural puncture headache in
the parturient --- an update. Anaesthesia Intens Care Med. 2010;11:302---4.
26.BoonmakP,BoonmakS.Epiduralbloodpatchingforpreventing andtreatingpost-duralpunctureheadache.CochraneDatabase SystRev.2010.
27.BarazR,CollinsRE.Themanagementofaccidentaldural punc-tureduringlabourepiduralanalgesia:asurveyofUKpractice. Anaesthesia.2005;60:673---9.
28.MarcusHE,FabianA,DagtekinO,etal.Pain,postdural punc-ture headache, nausea and pruritis after cesareandelivery: a survey of prophylaxis and treatment. Minerva Anestesiol. 2011;77:1043---9.
29.Gunaydın B, Camgoz N, Karaca G, et al. Survey of Turkish practice evaluating the management of postdural puncture headacheintheobstetricpopulation.ActaAnaesthesiolBelg. 2008;59:7---14.
30.ChanTML,AhmedE,YentisSM,etal.Postpartumheadaches: summaryreportoftheNationalObstetricAnestheticDatabase (NOAD)1999.IntJObstetAnesth.2003;12:107---12.
31.AshkenaziA,LevinM.Greateroccipitalnerveblockformigraine and other headaches: is it useful? Curr Pain Headache Rep. 2007;11:231---5.
32.BiondiDM.Cervicogenicheadache:areviewofdiagnosticand treatmentstrategies.JAmOsteopathAssoc.2005;105Suppl. 2:16S---22S.
33.AkyolF,BiniciO,C¸akırM.Ultrasound-guidedbilateralgreater occipitalnerveblockforthetreatmentofpostduralpuncture headache.TurkJAnaesthReanim.2014;42:40---2.
34.BartschT,GoadsbyPJ.Stimulationofthegreateroccipitalnerve inducesincreasedcentralexcitabilityofduralafferentinput. Brain.2002;125:1496---509.
35.Ambrosini A, Vandenheede M, Rossi P, et al. Suboccipital injection with a mixture of rapid- and long-acting steroids inclusterheadache:adoubleblindplacebo-controlledstudy. Pain.2005;118:92---6.