SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Original
article
Open
versus
arthroscopic
approach
in
the
treatment
of
femoroacetabular
impingement:
a
case–control
study
with
two-years
follow
up
夽
Bruno
Dutra
Roos
a,∗,
Milton
Valdomiro
Roos
a,
Antero
Camisa
Júnior
a,
Ezequiel
Moreno
Ungaretti
Lima
a,
Maurício
Domingos
Betto
baHospitalOrtopédicodePassoFundo,DepartamentodeOrtopediaeTraumatologia,PassoFundo,RS,Brazil
bHospitalOrtopédicodePassoFundo,GrupodeCirurgiadoQuadril,PassoFundo,RS,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received1December2016 Accepted26January2017 Availableonline9August2017
Keywords: Hipjoint
Femoroacetabularimpingement Hipinjuries
Osteoarthritis
a
b
s
t
r
a
c
t
Objective:To compareclinical andimagingresults andcomplications betweenpatients treated for femoroacetabular impingement (FAI) who underwent either anterior open surgeryoranarthroscopicapproach,withaminimumfollow-upoftwoyears.
Methods:Thisretrospectivecase–controlstudyincludedpatientssubmittedtoFAIsurgical treatment betweenNovember2007andMarch 2012.Patientstreated withopensurgery werecomparedwiththosetreatedwitharthroscopy.Patientswereclinicallyassessedby themodifiedHarrisHipScore,Non-ArthriticHipScore,andinternalhiprotation.Patients wereradiographicallyassessedbythecenter-edgeangle,jointspacewidth,alphaangle, neck-headindex,degreeofarthrosis,andpresenceofheterotopicossificationofthehip. Results:Inthestudyperiod, 56patients(58hips)withFAIwereincluded;16underwent opensurgeryand40underwentarthroscopy.The40patientstreatedbythearthroscopic routehadameanfollow-upof29.1months,and75.6%presentedgoodorexcellentclinical results.Theradiographicevaluationparametersprogressedtonormallevels.The16patients whounderwentopensurgeryhadameanfollow-upof52months,and70.58%presented goodorexcellentclinicalresults.Theradiographicevaluationparametersprogressedto normallevels.Postoperativeclinicalandradiographicresultswereconsideredsimilarin bothgroups.
Conclusions: ArthroscopyandopensurgerytreatmentsforFAIprovidedcomparableclinical andradiographicresults.However,ahigherrateofcomplicationswasobservedintheopen surgerygroup.
©2017PublishedbyElsevierEditoraLtda.onbehalfofSociedadeBrasileiradeOrtopedia eTraumatologia.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
夽
StudyconductedatHospitalOrtopédicodePassoFundo,CentrodeEstudosOrtopédicos,PassoFundo,RS,Brazil. ∗ Correspondingauthor.
E-mail:brunodroos@gmail.com(B.D.Roos).
http://dx.doi.org/10.1016/j.rboe.2017.07.007
Abordagem
anterior
aberta
versus
artroscópica
no
tratamento
do
impacto
femoroacetabular:
estudo
caso-controle
com
seguimento
mínimo
de
dois
anos
Palavras-chave: Articulac¸ãodoquadril Impactofemuroacetabular Lesõesdoquadril Osteoartrite
r
e
s
u
m
o
Objetivos: Compararos resultados clínicose radiográficos,bemcomo as complicac¸ões observadasempacientessubmetidosaotratamentocirúrgico,devidoaimpacto femoroac-etabular,sobabordagemartroscópicaouanterioraberta,comseguimentomínimodedois anos.
Métodos: Estudocaso-controleretrospectivo,compacientesoperadosentrenovembrode 2007emarc¸ode2012equeforamsubmetidosatratamentocirúrgicodeimpacto femoroac-etabular. Pacientes submetidos à abordagem abertaforam comparados compacientes submetidosàabordagemartroscópica.Ospacientesforamavaliadosclinicamentepelos escores clínicosHarris Hipmodificado, NonArthriticHipe quanto à rotac¸ãointerna do quadril.Ospacientesforamavaliadosradiograficamente,aferiram-seoângulocentro-borda, adimensãodoespac¸oarticular,oânguloalfa,oíndicecolo-cabec¸a,ograudeartroseea presenc¸adeossificac¸ãoheterotópicadoquadril.
Resultados: Foramincluídosnoestudo56pacientes,16submetidosàabordagemabertae 40àartroscópica.Os40pacientestratadosporviaartroscópicaforamseguidospor,em média,29,1meses,75,6%apresentaramresultados clínicosbonsouexcelentes.Quanto àavaliac¸ãoradiográfica,observou-secorrec¸ãoparaíndicesconsideradosnormais.Os16 pacientes operados por via aberta obtiveram seguimento médiode 52 meses, 70,58% apresentaram resultados clínicos bons ou excelentes. Quanto à avaliac¸ão radiográfica, observou-secorrec¸ãoparaíndicesconsideradosnormais.Osresultadosclínicose radio-gráficospós-operatóriosforamconsideradossemelhantesemambososgrupos.
Conclusão: Osresultadosclínicoseradiográficosdotratamentoartroscópicodoimpacto femoroacetabularforamcomparáveisaosresultadosdotratamentoaberto.Observamos ummaiornúmerodecomplicac¸õesnogrupoaberto.
©2017PublicadoporElsevierEditoraLtda.emnomedeSociedadeBrasileirade OrtopediaeTraumatologia.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Femoroacetabularimpingement(FAI)isnowrecognizedasa commoncauseofhippainintheyoungpopulation,with pos-sibledegenerativeconsequences.1,2 Boththeknownimpact mechanisms (cam or inclusion, and pincer or impaction) are associated with pain, restricted range of motion, and decreasedexercisetolerance.3Currently,severalstudieshave suggestedthatsomecasesthatwerepreviouslyconsideredas idiopathichiposteoarthritisaresecondarytoFAI.4–8
Conservativetreatmentcanbeattemptedinitially;it con-sists ofmodifying high-impactphysical activities,avoiding weightedexercisesassociatedwithexcessiveflexionand tor-sionmovementsthatincreasejointdemand,and,finally,the useofanti-inflammatorymedications.Surgicaltreatmentis indicatedincaseswhenconservativetreatmentbringsonly temporary relief.9,10 Some authors claimthat, sinceit is a mechanicalcondition,delayingsurgicaltreatmentoftheFAI maynotbebeneficialtothepatient.However,thereisstillno consensusintheliteratureregardingthissubject.1,2,10,11
Surgical treatment options for FAI include open sur-gical correction with posterior hip dislocation (Ganz approach), anterior hip approaches (Smith-Petersen, Hueter,Sommerville,andanteriorextensible,amongothers),
videoarthroscopicsurgery,andacombinationofarthroscopic techniqueandanteriormini-incision.1–9
Thepresentstudyaimedtocomparetheclinicaland radio-graphicresultsandthecomplicationsrelatedtopatientswho underwent surgical treatmentofFAIperformed bytheHip Surgery Groupof this institutionusing the arthroscopic or anterior open (iliofemoral) approach,witha minimumtwo yearfollow-up.
Material
and
methods
Accordingtotheestablishedcriteria,56patients(58hips) metall the necessaryrequirements forthis study.Patients were divided into two groups: GroupI included casesthat underwent arthroscopic surgery, and Group II, those that underwentopenapproach.
GroupI(arthroscopictreatment)included40patients;36 (87%)weremale,andthemeanagewas36.12years(SD=8.7, range:21–47years).Therighthipwasoperatedonin20cases (48.78%),andthelefthip,in21(51.21%);onecasewasoperated bilaterallyatdifferenttimes.
GroupII(openapproach)included16patients;11(68.75%) weremale,andthemeanagewas35.76years(SD=9.5,range: 19–47years). Therighthip wasoperated onin eightcases (47.05%),andtheleft,innine(52.94%);onecasewasoperated bilaterallyatdifferenttimes.
Regardingtheclinicalaspects,patientswereassessed pre-andpostoperativelythroughtheHarrisHipScore,modifiedby ByrdapudGuimarães13(MHHS);theNon-ArthriticHipScore14 (NAHS);andtherangeofinternalrotation(IR)oftheaffected hip(withgoniometerforgauging).
According to the Harris Hip Score modified by Byrd,13 resultswerestratifiedaspoor(MHHS<70points),fair(70–79 MHHS),good(MHHS80–89),orexcellent(MHHS90–100).10
All patientswere assessedbyradiographs (anteroposte-rior [AP] view ofthe hip in the orthostatic position, Dunn 45◦, Dunn 90◦, and Lequesne’s false profile),15 as well as magneticresonance imaging forthe diagnosis ofchondral and labralinjuries.Pincer-type FAIwas diagnosedby mea-suring the angle of femoral head coverage and acetabular version on AP radiographs of the hip in the orthostatic positionand in Lequesne’sfalse profile.Cam-typeFAIwas defined as alpha angle greater than 50◦ in Dunn 45◦ radiographs.16
Inthepreoperativeperiod,thefollowingweremeasured: Tönnis17hiparthrosisclassification;center-edgeangle(CE); sizeofthesmallestjointspace,inmillimeters,onAP radio-graphsofthehipintheorthostaticposition;alphaangle,as describedbyMeyer16inDunn45◦ radiographs(␣);and lat-eralviewhead-neckindex(NHI)inDunn90◦ radiographs.15 Inthelatepostoperativeperiod,thesizeofthesmallestjoint spaceinmillimeters,the␣,andtheNHIwereassessedfor comparisonwithpre-operativemeasurements;thepresence ofheterotopic hip ossification was assessedin accordance withBrookeretal.18Toavoidinter-andintra-observererrors, themeasurementsweremadebytwosurgeonsfromthehip group.Incasesofdisagreementofmorethanthreedegreesin theangularmeasurementsorofmorethan1mminthe min-imumjointspace,anewevaluationwasperformedbyathird surgeon,andaconsensuswasthenreached.Themean mag-nificationoftheAPradiographofthehipwas15%,whichwas quantifiedbytheequipment.
TheWilcoxon test(SPSS version18.0,SPSS, Chicago,IL, USA)wasthe statisticalmethod usedtoanalyzethe inter-group paired variables (MHHS,NAHS, IR, alpha angle, and pre- and postoperative NHI). The Mann–Whitney test was applied for the intergroup analysis of the same variables; both tests were considered statistically significant when p<0.05. In order to assess the homogeneity between the groups,thechi-squaredtestwasappliedforthepreoperative measurements.
Results
Accordingtothepreoperativestatisticalanalysis,bothgroups wereconsideredhomogeneous.
In Group I (arthroscopy), the mean follow-up was 29.1 months(24–42).RegardingtheassessmentoftheMHHSscore, the mean preoperativescore was65 points(SD=9.8, range 38–77)andthemeanpostoperative,88(SD=11,range60–100), withameanpostoperativeincreaseof22.1.Accordingtothe establishedcriteria,31(75.60%)casespresentedgoodor excel-lentclinicalresults;eight(19.51%),fair;andthree(7.31%),poor. RegardingtheassessmentoftheMHHSscore,themean pre-operativescorewas68.8points(SD=12.5,range45–80)andthe meanpostoperative,92.5(SD=10,range60–100),withamean postoperative increaseof21.5.Themean pre-operativehip IRwas5◦(SD=10◦,range
−15◦to30◦)andpostoperative,20◦ (SD=12.5◦,range5◦–40◦),withameanpostoperativeincrease of 16.4◦. Statistically significant differences were observed (p<0.001)inthepre-andpostoperativemeasurementsofthe MHHSandNAHSclinicalscores,aswellasinhipIR.
Cam-typeFAIwasobservedin29hips(70.73%)and mixed-typeFAI,in12(28.27%).In20cases(48.78%)isolatedfemoral osteochondroplastywas performedduringthe arthroscopic surgicaltreatment;intheremaining21cases(51.21%),other complementaryprocedureswereperformed,suchas acetabu-larosteochondroplastyinmixed-typeFAIs(12cases[29.26%]), debridementoftheacetabularlabrum(sevencases[17.07%]), acetabular chondral microfracture in Outerbridge grade 4 chondral injuries(four cases[9.75%]) and labrum reattach-mentinaccordancewithFryandDombapudRibasetal.19(five cases[12.19%]).
Regarding the preoperative radiographic evaluation, 13 cases(31.7%)presentedarthrosis classifiedasTönnisgrade 0,21 (51.21%) asTönnis1,andseven(17.07%) asTönnis2; nocaseswereclassifiedasTönnis3.ThemeanCEanglewas 35.78◦(24◦–46◦).NopatientpresentedCEanglelowerthan20◦ (hipdevelopmentaldysplasia).Inthepreoperativeperiod,the meansmallestjointspacewas3.31mm(2–4mm);no statisti-callysignificantdifferencewasobservedincomparisonwith thelatepostoperativeresult(p=1.000).Regarding thealpha angle,themeanpostoperativereductionwas32.9◦;themean preoperativeanglewas76◦(SD=14◦,range60◦–100◦),andthe meanpostoperative,44◦(SD=12.5◦,range32◦–55◦).Regarding theHNI,themeanpostoperativeincreasewas0.10;themean preoperativevaluewas0.10(SD=0,range0.06–0.14),andthe meanpostoperative,0.20(SD=0.1,range0.16–0.32).A statisti-callysignificantdifference(p<0.001)wasobservedforthe pre-and postoperativealphaangleand HNI.Inthelate postop-erativeperiod,36cases(87.80%)didnotpresentheterotopic ossification;infourpatients(9.75%),heterotopicossification wasfoundandclassifiedasBrooker18grade1andonecase (2.43%),asgrade3(Fig.1).
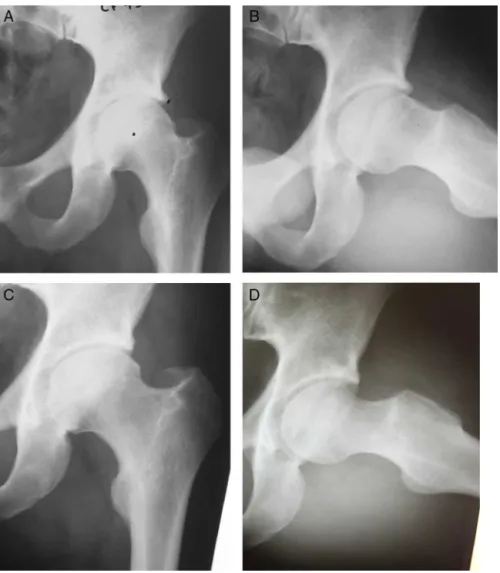
Fig.1–Malepatientaged28years,arthroscopicsurgerygroup.AandB,preoperativeradiographicevidenceofmixed-type FAI,CEangle:39◦;␣angle:64◦.CandD,post-operativeradiographicimaging3yearsand2monthsafterfemoraland acetabularosteochondroplasty,combinedwithlabralre-fixation.CEangle:28◦;␣angle:34◦.
In Group II (open), the mean follow-up was 52 months (43–74). Regarding the assessment ofthe MHHS score, the meanpreoperativescorewas63points(SD=9,range48–70) andthemeanpostoperative,88(SD=22,range58–94),witha meanpostoperativeincreaseof21.7.Accordingtothe estab-lishedcriteria,12(70.58%)casespresentedgoodorexcellent clinical results;two(11.76%), fair; andthree (17.64%),poor. RegardingtheassessmentoftheNAHSscore,themean pre-operativescorewas65points(SD=11.3,range48.75–77.5)and themeanpostoperative,90(SD=20,range60–95),withamean postoperativeincreaseof20.4.Themean pre-operativehip IRwas5◦ (SD=10◦,range
−5◦ to20◦)andpostoperative,25◦ (SD=10◦,range15◦–40◦),withameanpostoperativeincrease of 21.2◦. Statistically significant differences were observed (p<0.001)inthepre-andpostoperativemeasurementsofthe MHHSandNAHSclinicalscores,aswellasinhipIR.
Cam-typeFAIwasobservedin12hips(70.58%)and mixed-type FAI, in five (29.42%). In 12 cases (70.58%), during the arthroscopicsurgicaltreatment,isolatedfemoral osteochon-droplastywasperformed;intheremainingfivecases(29.42%, mixed-typeFAIs),acetabularosteochondroplastywithlabral re-fixationwasalsoperformed.
Regarding thepreoperativeradiographicevaluation,nine cases(52.9%)presentedarthrosisclassifiedasTönnisgrade0, six(35.29%)asTönnis1,andtwo(11.76%)asTönnis2;nocases were classifiedasTönnis3.ThemeanCE anglewas32.82◦ (23◦–44◦).NopatientpresentedCEanglelowerthan20◦.Inthe preoperativeperiod,themeansmallestjointspacewas3mm (2–4mm);nostatisticallysignificantdifferencewasobserved in comparison with the late postoperative result (p=0.58). Regardingthealphaangle,themeanpostoperativereduction was 32.5◦;the meanpreoperativeanglewas72◦ (SD=12.5◦, range60◦–90◦),andthemeanpostoperative,40◦(SD=9◦,range 32◦–52◦).RegardingtheHNI,themeanpostoperativeincrease was0.12;themeanpreoperativevaluewas0.11(SD=0,range 0.08–0.15),andthe meanpostoperativevalue,0.22(SD=0.1, range0.2–0.3).Astatisticallysignificantdifference(p<0.001) wasobservedforthepre-andpostoperativealphaangleand HNI.Inthelatepostoperativeperiod,12cases(70.58%)didnot presentheterotopicossification;infivepatients(29.41%),the heterotopicossificationwasfoundandclassifiedasBrooker18 grade1(Fig.2).
Fig.2–Malepatientaged37years,opensurgerygroup.AandB,preoperativeradiographicevidenceofmixed-type,CE angle:32◦;␣angle:62◦.CandD,post-operativeradiographicimaging4yearsand4monthsafterfemoralandacetabular osteochondroplasty,combinedwithlabralre-fixation.CEangle:28◦;␣angle:32◦.
werefourcases(23.5%)ofpersistentpain;twocases(bothwith Tönnis2arthrosis)presentedprogressionofthejoint degen-erationandtotalhiparthroplastywasindicated.
No major complications, such as avascular necrosis of the femoralhead, femoralneck fracture, or infection were observed.
Accordingtothestatisticalanalysis,bothgroupspresented similarpostoperativeresultsregardingtheclinicaland radio-graphicevaluation(Tables1–3).
Discussion
Table1–Resultsofthehiparthrosisassessmentinpatientssubmittedtosurgicaltreatmentoffemoroacetabular impingement.
Groups Evaluation Time Median IQR p
Opensurgery Tönnisgrade0 Pre 9(52.9%)
Post Notassessed
Tönnisgrade1 Pre 6(35.29%)
Post Notassessed
Tönnisgrade2 Pre 2(11.76%)
Post Notassessed
Tönnisgrade3 Pre 0
Post Notassessed
Smallestjointspace(mm) Pre 3(SD1,range2to4) 1 0.58 Post 2.85(SD1.3,range1.5to4) 1.3
Arthroscopicsurgery Tönnisgrade0 Pre 13(31.7%) Post Notassessed Tönnisgrade1 Pre 21(51.21%)
Post Notassessed
Tönnisgrade2 Pre 7(17.07%)
Post Notassessed
Tönnisgrade3 Pre 0
Post Notassessed
Smallestjointspace(mm) Pre 3.31(SD1,range2to4) 1 1.000 Post 3.31(SD1,range2to4) 1
IQR,interquartilerange.
Table2–Resultsoftheradiographicmeasurementsofpatientssubmittedtosurgicaltreatmentoffemoroacetabular impingement.
Group Evaluation Time Value IQR p
Opensurgery Alphaangle(degree,median) Pre 72◦(SD12.5◦,range52◦to87◦) 12.5 <0.001
Post 40◦(SD9◦,range32◦to48◦) 9
NHI(median) Pre 0.11(SD0,range0.08to0.15) 0 <0.001 Post 0.22(SD0.1,range0.2to0.3) 0.1
CE(mean,degree) Pre 32.82◦(23◦to44◦)
Post Notassessed
Arthroscopicsurgery Alphaangle(degree,median) Pre 76◦(SD11◦,range60◦to88◦) 14 <0.001
Post 44◦(SD12.5◦,range32◦to55◦) 12.5
NHI(median) Pre 0.10(SD0,range0.06to0.14) 0 <0.001 Post 0.20(SD0.1,range0.16to0.32) 0.1
CE(mean,degree) Pre 35.78◦(27◦to46◦)
Post Notassessed
IQR,interquartilerange.
Table3–Resultsofthefunctionalclinicalevaluationofpatientssubmittedtosurgicaltreatmentoffemoroacetabular impingement.
Group Evaluation Time Median,SD,andrange IQR p
Opensurgery MHHS Pre 63(SD9,range48to70) 9 <0.001
Post 88(SD22,range58to94) 22
NAHS Pre 65(SD11.3,range48.75to77.5) 11.3 <0.001 Post 90(SD20,range60to95) 20
Internalrotation Pre 5(SD10◦,range
−5◦to20◦) 10 <0.001 Post 25(SD10◦,range15◦to40◦) 10
Arthroscopicsurgery MHHS Pre 65(SD9.8,range38to77) 9.8 <0.001 Post 88(SD11,range60to100) 11
NAHS Pre 68.8(SD12.5,range45to80) 12.5 <0.001 Post 92.5(SD10,range60to100) 10
Internalrotation Pre 5(SD10◦,range
−15◦to30◦) 10 <0.001 Post 20(SD12.5◦,range5◦to40◦) 12.5
Inthe literature,several authors have presentedresults ofthesurgicaltreatmentofFAI,whetherusingGanz’sopen approach,anteriorapproaches(Smith-Petersen,Hueter,etc.), arthroscopic technique,or thecombination ofarthroscopic technique and anterior mini-approach. To date, the Ganz approachisconsidered the gold standard FAItreatment.2,6 Theresultsare generallypositiveregardingsymptomrelief andimprovementofhipmobilityandlevelofphysicalactivity; theyalsosuggestjointpreservationinthelongterm.1–9
Moststudiesthatcomparetheopenandarthroscopic tech-niquesare comparative meta-analyses. Matsudaet al.,1 in a comparative systematicreview, assessed 18 articles that presentedresultsofsurgicalhipdislocationtechniquesand anteriorandarthroscopicminiapproach;theyconcludedthat all ofthese techniques are capable ofimproving pain and functioninthemediumterm.However,opentechniques pre-sentedagreaternumber ofcomplicationsrelatedtolateral cutaneous-femoralnerveinjuryintheanteriorminiapproach; in surgical hip dislocation, they presenteda greater num-berofcomplicationsrelatedtothesiteofgreatertrochanter osteotomy (pseudoarthrosisand localpain). Botser et al.20 foundsimilarresultsina meta-analysisof26articles, and concludedthatthereisevidencethatthearthroscopic tech-niquepresentsfewercomplicationsandfasterrehabilitation. Recently, Domb et al.21 prospectively paired ten patients undergoingsurgicaltreatment forFAIbyGanzsurgical dis-locationtechnique(meanfollow-upof24.8months)with20 patientsundergoingtreatmentthroughthearthroscopic tech-nique(meanfollow-upof25.5months).Theyconcludedthat patientssubmittedtothearthroscopictreatmentpresenteda significantlygreaterimprovementintheclinicalscores eval-uated.
The iliofemoral anterior approach described by Smith-Petersen22isalsousedinthetreatmentofFAI,allowingdirect accessto the hip joint. However,it does notprovide good accesstotheacetabulumanddoesnotallowthecorrection ofalterations infemoral orientation.1 Injury of the lateral femoral cutaneous nerve is the most prevalent complica-tion,whichinmostcasespresentsspontaneousresolution. Afterone year of follow-up, Ribas et al.19 reported signifi-cantimprovementinaseriesof35FAIhipssurgicallytreated throughtheanteriorapproach.A23◦ increaseinhipIRwas observed,aswellasasignificantimprovementintheclinical parametersevaluated.Regardingcomplications,femoral lat-eralcutaneousnervedysfunctionwasobservedinsixcases (17.1%),beingtransientinfive.Laudeet al.23evaluated100 hipsoperatedwithanteriorapproachcombinedwith arthro-scopic assistance (mean follow-up of 4.9 years); a mean increaseof29.1 pointswasobservedforNAHS,and 11%of patientshadundergonearthroplastyattheendoffollow-up.
Arthroscopyhasbeenwidelydiffusedinthetreatmentof FAIduetoitsshortrehabilitationperiodandgoodaccessto thehipjoint.Complicationsareusuallyrelatedtothetimeof morefrequentinjuriessuchasthoseofthelateralpudendal andlateralfemoralcutaneousnerves,andrarerinjuriessuch astothesciaticnerve(0–12.9%).1,10–12,20Philliponetal.11used thearthroscopictechniqueforFAItreatmentin112patients (meanfollow-upof2.3years)andfoundameanincreaseof24 pointsintheMHHS,withoutcomplications.Inarecent publi-cation,BryrdandJones10evaluated207hips(meanfollow-up
of 16 months) and found a mean increase of20 points in theMHHS;complicationswereobservedin1.5%ofcasesand in0.5%ofcasesprogressedtototalhiparthroplasty. Horis-bergeretal.24 appliedasimilartechniqueto105hipsof88 patients(meanfollow-upof2.3years)andobservedamean postoperativeincreaseof28pointsintheNAHS,witha1.9% complicationratesforsciaticorpudendalnerveneuropraxia and 11% for neuropraxia of the lateral femoral cutaneous nerve.In8.6%ofcases,therewasaneedforconversionto hiparthroplasty.
In the present study, results similar to those in the literature were observed for both groups. A postoperative improvementinthe clinicalevaluationofthe patientswas observed,andtheradiographicparametersprogressedto lev-elsconsiderednormal.Thehighernumberofhiparthroplasty indicationsintheopengroupcanbeexplainedbythelonger follow-upofthesepatients(meanof52months).Inthe arthro-scopicgroup,alowernumberofpostoperativecomplications wasobserved.Alongerfollow-upofthisgroupisnecessaryin ordertodefinewhetherthepostoperativejointpreservation andclinicalresultswillremainsatisfactory.
Thelimitationsofthepresentstudywerethesmallnumber ofpatientsintheopengroup,aswellasthepredominanceof malepatientsandtheshortfollow-uptime(29.1months)in thearthroscopicgroup.
Conclusion
Theclinicalandradiographicresultsofthearthroscopic treat-mentofFAIwere comparabletothoseofthe openanterior approach.Agreaternumberofcomplicationswereobserved intheopengroup.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.MatsudaDK,CarlisleJC,ArthursSC,WiekrsCH,PhilliponMJ. Comparativesystematicreviewoftheopendislocation, mini-open,andarthroscopicsurgeriesforfemuroacetabular impingement.Artroscopy.2011;27(2):252–69.
2.GanzR,ParvizziJ,BeckM,LeuningM,NoltzliH,Siebenrock KA.Femoroacetabularimpingement:acauseforosteoartritis ofthehip.ClinOrthopRelatRes.2003;(417):112–20.
3.SrinivasanSC,HosnyHA,WilliamsMR.Combinedhip arthroscopyandlimitedopenosteochondroplastyfor anteriorfemoroacetabularimpingement:earlypatient reportedoutcomes.HipInt.2013;23(2):218–24.
4.ItoK,MinkaMA,LeuningM,WerlenS,GanzR. Femoroacetabularimpingementandthecam-effect.A MRI-based,quantitativeanatomicalstudyofthefemoral head-neckoffset.JBoneJointSurgBr.2001;83(2):171–6.
5.GoodmanDA,FeighanJE,SmithAD,LatimerB,BulyRL, CoopermanDR.Subclinicalslippedcapitalfemoralepiphysis. Relationshiptoosteoarthrosisofthehip.JBoneJointSurg Am.1997;79(10):1489–97.
accesstothefemoralheadandacetabulumwithouttherisk ofavascularnecrosis.JBoneJointSurgBr.2001;83(8):1119–24.
7. FitzgeraldRHJr.Acetabularlabrumtears.Diagnosisand treatment.ClinOrthopRelatRes.1995;311:60–8.
8. SeldesRM,TanV,HuntJ,KatzM,WiniarskiR,FitzgeraldRHJr. Anatomy,histologicfeatures,andvascularityoftheadult acetabularlabrum.ClinOrthopRelatRes.2001;382:232–40.
9. GuancheCA,BareA.Artroscopictreatmentof femoroacetabularimpingement.Arthroscopy. 2006;22(1):95–106.
10.ByrdJW,JonesKS.Arthroscopicmanagementof
femoroacetabularimpingement:minimum2-yearfollow-up. Arthroscopy.2011;27(10):1379–88.
11.PhilipponMJ,BriggsKK,YenKM,KuppersmithDA.Outcomes followinghiparthroscophyforfemoroacetabular
impingementwithassociatedcondrolabraldysfunction: minimumtwoyearsfollowup.JBoneJointSurgBr. 2009;91(1):16–23.
12.RoosBD,RoosMV,CamisaJúniorA,LimaEMU,GyboskiDP, MartinsLS.Abordagemextracapsularparatratamentodo impactofemoroacetabular:resultadosclínicos,radiográficos ecomplicac¸ões.RevBrasOrtop.2015;50(4):430–7.
13.GuimarãesRP,AlvesDPL,AzuagaTL,OnoNK,HondaE, PoleselloGC,etal.Traduc¸ãoeadaptac¸ãotransculturaldo HarrisHipScoremodificadoporByrd.ActaOrtopBras. 2010;18(6):339–43.
14.ChristensenCP,AlthausenPL,MittlemanMA,LeeJA, McCarthyJC.Thenonarthritichipscore:reliableand validated.ClinOrthopRelatRes.2003;406:75–83.
15.ClohisyJC,CarlisleJC,BeauléPE,KimY,TrousdaleRT,Sierra RJ,etal.Asystematicapproachtotheplainradiographic evaluationoftheyoungadulthip.JBoneJointSurgAm. 2008;90(4):47–66.
16.MeyerDC,BeckM,EllisT,GanzR,LeunigM.Comparisonof sixradiographicprojectionstoassessfemoralhead/neck asphericity.ClinOrthop.2006;445:181–5.
17.BusseJ,GasteigerW,TönnisD.Anewmethodfor roentgenologicevaluationofthehipjoint–thehipfactor. ArchOrthopUnfallchir.1972;72(1):1–9.
18.BrookerAF,BowermannJW,RobinsonRA,RileyRHJr.Ectopic ossificationfollowingtotalhipreplacement.Incidenceand methodofclassification.JBoneJointSurgAm.
1973;55(8):1629–32.
19.BotserIB,SmithTW,NasserR,DombBG.Opensurgical dislocationversusarthroscopyforfemoroacetabular impingement:acomparisonofclinicaloutcomes. Arthroscopy.2011;27(2):270–8.
20.DombBG,StakeCE,BotserIB,JacksonTJ.Surgicaldislocation ofthehipversusarthroscopictreatmentoffemoroacetabular impingement:aprospectivematched-pairstudywithaverage 2-yearfollow-up.Arthroscopy.2013;29(9):1506–13.
21.Smith-PetersenMN.Treatmentofmalumcoxaesenilis,old slippeduppercapitalfemoralepiphysis,intrapelvic protrusionoftheacetabulum,andcoxaeplanabymeansof acetabuloplasty.JBoneJointSurgAm.1936;18:
869–80.
22.RibasM,Marín-Pe ˜naOR,RegenbrechtB,DeLaTorreB, VillarubiasJM.Hiposteoplastybyananteriorminimally invasiveapproachforactivepatientswithfemoroacetabular impingement.HipInt.2007;17(2):91–8.
23.LaudeF,SarialiE,NogierA.Femoroacetabularimpingement treatmentusingarthroscopyandanteriorapproach.Clin OrthopRelatRes.2009;467(3):747–52.